INTRODUCTION
The past two decades have seen five major and multiple small trials comparing prone and supine position ventilation in acute respiratory distress syndrome (ARDS). This article attempts to review the evidences for prone-positioning in ARDS.
METHODS
A PubMed search was done with keywords prone-position (tagged with major) and ARDS separated by Boolean operator ‘AND’. This returned 128 titles with 28 clinical trials and 25 review articles. Those clinical trials with <30 participants have been excluded. Five clinical trials were finally reviewed [Table 1]. Similarly, six meta-analyses were selected for discussion [Table 2] based on relevance of topic and quality of evidence.
Table 1.
Major trials on prone position ventilation in ARDS
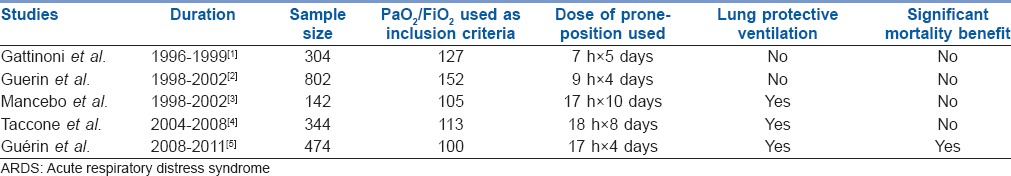
Table 2.
Summary of various meta analyses on prone position ventilation in ARDS

DISCUSSION
Earlier trials could not demonstrate a mortality benefit of prone-position over supine position ventilation [Table 1]. The swing in evidence supporting prone-position ventilation can largely be credited to the PROSEVA (Proning Severe ARDS Patients) trial.[5] This was a multicentre, prospective, randomized controlled trial (RCT) where 466 severe ARDS patients were assigned to undergo either 16 h prone-positioning sessions or to be left in the supine position. The 28-day mortality was 16.0% in the prone group and 32.8% in the supine group (P < 0.001). The 90-day mortality was 23.6% in the prone group versus 41.0% in the supine group (P < 0.001). These results may, however, be confounded by the fact that the supine position group were a sicker group with a slightly higher SOFA score and were receiving more pressors and neuromuscular blockers. Also, the list of exclusion criteria was lengthy suggesting that the beneficial outcome may be restricted to a minority of ARDS patients. Furthermore, the PROSEVA staff was highly trained and experienced in the procedure of prone-positioning, so the same results may not apply to settings with untrained staff.
The earliest of meta-analysis done in 2008 did not show any mortality benefit of prone-positioning, but two meta analyses performed in 2010 by Sud et al. and Gattinoni et al. respectively showed that cases of severe ARDS do benefit from prone-positioning. In December 2013, Lee et al. conducted a meta-analysis of 11 RCTs and concluded that along with severe ARDS, longer durations of prone-positioning is also beneficial. The meta-analysis done in January 2014 by Beitler et al. have shown a survival benefit with low tidal volume and prone-position ventilation.[10] The largest of the meta-meta analyses published in March 2014 by Tonelli et al. where they included 159 RCTs and 29 meta analyses to see the effect of various modalities in cases of ARDS, also suggested that prone-position ventilation has survival benefit in cases of severe ARDS [Table 2].
The mechanics of prone-position ventilation can be explained as follows: In a normal lung, the alveolar density is more posteriorly.[12] In supine position, these posterior alveoli get compressed due to various reasons such as: (1) Action of gravity, (2) shape of the chest wall: The anterior lung parenchyma is more conical than the posterior lung parenchyma. The anterior alveoli thus have a greater volume of intra-thoracic cavity available to expand and are thus more distended than the posterior alveoli and (3) the heart and diaphragm further act under gravity to compress posterior alveoli.
The total recruitment of alveoli is more in prone-position than in supine position because the posterior lung parenchyma comes in non-dependent position and hence their compression due to gravity is prevented and also because the heart and diaphragm no longer act under gravity to compress alveoli.
The ARDS lung is characterized by infiltrates that tend to accumulate in the dependent alveoli. In supine position, the infiltrates accumulate and compromise the posterior alveoli and thus prevent ventilation. The anterior alveoli, which are fewer than posterior alveoli, are only available to maintain ventilation.[8] [Figure 1]
Figure 1.
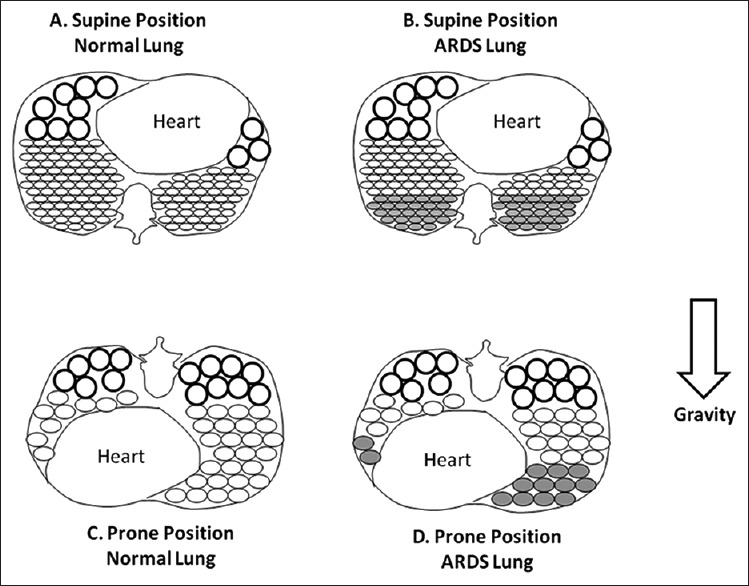
Cross-section of the lungs. (a) Normal lung in supine position. (b) Acute respiratory distress syndrome lung in supine position. (c) Normal lung in prone-position. (d) ARDS lung in prone-position. Circles represent alveoli. Shaded circles indicate alveoli with infiltrates
In prone-position, the infiltrates rapidly shift to accumulate and compromise the anterior alveoli (dependent part). The posterior alveoli (non-dependent), which are far greater in number than anterior alveoli, are thus released to maintain a better perfusion.[8]
The same amount of infiltrates has more posterior alveoli to compromise in the supine position as compared to anterior alveoli in prone-position. This helps in more alveolar recruitment in a homogeneous manner.[8] Apart from this, the perfusion also is maintained homogeneously.[8] The pre-load on the heart decreases and cardiac index improves. The end result is better oxygenation.[13]
Prone-position ventilation is not free from complications. Those related to the mechanics of manoeuvre are a transient desaturation, transient hypotension, accidental extubation, and catheter displacements. Those related to duration of proning are pressure ulcers, vomiting and need for excessive sedation. Harmful complications like compression of nerves and retinal vessels, facial oedema, difficulty in instituting cardiopulmonary resuscitation have also been seen. Most of these can be prevented by an experienced team and use of special devices and beds that facilitate the mechanics of safe proning.
Patient can be turned into prone-position either manually or through automated beds designed for this purpose. Manual method is cheaper than the automated one but requires highly skilled staff and integrated work of the nursing staff with the respiratory therapist. The respiratory therapist ensures the stability of the endotracheal tube, one nurse is needed to secure the vascular lines and at least two or three nurses to turn the patient prone. Automated prone-positioning needs one nurse, minimises risk during turning and provides continuous rotation if required.
CONCLUSION
The recent PROSEVA trial has provided compelling evidence in support of long duration prone-position ventilation for mortality reduction in severe ARDS cases. This is a relatively cheaper method of ARDS management and might be a simple solution to the complicated problem of high burden of ARDS and related mortality.
REFERENCES
- 1.Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345:568–73. doi: 10.1056/NEJMoa010043. [DOI] [PubMed] [Google Scholar]
- 2.Guerin C, Gaillard S, Lemasson S, Ayzac L, Girard R, Beuret P, et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: A randomized controlled trial. JAMA. 2004;292:2379–87. doi: 10.1001/jama.292.19.2379. [DOI] [PubMed] [Google Scholar]
- 3.Mancebo J, Fernández R, Blanch L, Rialp G, Gordo F, Ferrer M, et al. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;173:1233–9. doi: 10.1164/rccm.200503-353OC. [DOI] [PubMed] [Google Scholar]
- 4.Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, Mietto C, et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: A randomized controlled trial. JAMA. 2009;302:1977–84. doi: 10.1001/jama.2009.1614. [DOI] [PubMed] [Google Scholar]
- 5.Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–68. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 6.Sud S, Sud M, Friedrich JO, Adhikari NK. Effect of mechanical ventilation in the prone position on clinical outcomes in patients with acute hypoxemic respiratory failure: A systematic review and meta-analysis. CMAJ. 2008;178:1153–61. doi: 10.1503/cmaj.071802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sud S, Friedrich JO, Taccone P, Polli F, Adhikari NK, Latini R, et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: Systematic review and meta-analysis. Intensive Care Med. 2010;36:585–99. doi: 10.1007/s00134-009-1748-1. [DOI] [PubMed] [Google Scholar]
- 8.Gattinoni L, Carlesso E, Taccone P, Polli F, Guérin C, Mancebo J. Prone positioning improves survival in severe ARDS: A pathophysiologic review and individual patient meta-analysis. Minerva Anestesiol. 2010;76:448–54. [PubMed] [Google Scholar]
- 9.Lee JM, Bae W, Lee YJ, Cho YJ. The efficacy and safety of prone positional ventilation in acute respiratory distress syndrome: Updated study-level meta-analysis of 11 randomized controlled trials. Crit Care Med. 2014;42:1252–62. doi: 10.1097/CCM.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 10.Beitler JR, Shaefi S, Montesi SB, Devlin A, Loring SH, Talmor D, et al. Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: A meta-analysis. Intensive Care Med. 2014;40:332–41. doi: 10.1007/s00134-013-3194-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tonelli AR, Zein J, Adams J, Ioannidis JP. Effects of interventions on survival in acute respiratory distress syndrome: An umbrella review of 159 published randomized trials and 29 meta-analyses. Intensive Care Med. 2014;40:769–87. doi: 10.1007/s00134-014-3272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mackenzie CF. Anatomy, physiology, and pathology of the prone position and postural drainage. Crit Care Med. 2001;29:1084–5. doi: 10.1097/00003246-200105000-00046. [DOI] [PubMed] [Google Scholar]
- 13.Malbouisson LM, Busch CJ, Puybasset L, Lu Q, Cluzel P, Rouby JJ. Role of the heart in the loss of aeration characterizing lower lobes in acute respiratory distress syndrome. CT Scan ARDS Study Group. Am J Respir Crit Care Med. 2000;161:2005–12. doi: 10.1164/ajrccm.161.6.9907067. [DOI] [PubMed] [Google Scholar]


