Dear Editor,
We read with great interest the article on “Noncardiac pulmonary edema induced by sitagliptin treatment” by Belice et al.[1] published in the fourth issue of 2014. As radiologists, we would like to contribute to the section by listing the points of differentiation between cardiogenic and noncardiogenic pulmonary edema on chest radiograph. These points would be beneficial for the readers involved in primary care.
Pulmonary edema is a broad descriptive term and is usually defined as an abnormal accumulation of fluid in the extravascular compartments of the lungs. The pathophysiologies involved are increased hydrostatic pressure gradient across the capillary wall, diminished osmotic pressure gradient, and increased capillary permeability. Noncardiogenic pulmonary edema is caused by changes in capillary permeability as a result of a direct or an indirect pathologic insult, while cardiogenic pulmonary edema occurs due to increased capillary hydrostatic pressure secondary to elevated pulmonary venous pressure. Major causes of noncardiogenic pulmonary edema are drowning, fluid overload, aspiration, inhalation injury, neurogenic pulmonary edema, acute kidney disease, allergic reaction, and adult respiratory distress syndrome. Cardiogenic edema is caused by factors leading to elevated left atrial pressures, such as atrial outflow obstruction (mitral stenosis, atrial myxoma), left ventricular systolic dysfunction (congestive heart failure), left ventricular diastolic dysfunction, left ventricular volume overload, left ventricular outflow obstruction, dysrhythmias, cardiomyopathies, and myocardial infarction. Clinically, in most instances the history, signs, and symptoms will be sufficient to identify the cause of edema, but in many other instances, especially in a critical care setting, the cause of edema may be difficult to determine. Cardiogenic pulmonary edema shows mediastinal widening in the form of increased vascular pedicle width (>53 mm), pleural effusion, cardiomegaly, peribronchial cuffing, upper lobe pulmonary venous diversion in the form of prominence of bronchovascular markings, Kerley B lines, opacities involving both the central as well as the peripheral lungs, and reduced lung volume.[2] Noncardiogenic pulmonary edema shows the classic “batwing” pattern of pulmonary opacities radiating centrifugally from the hila with air bronchogram. Cardiomegaly, pleural effusion, and mediastinal widening are usually not seen. Lung volume may be normal or increased.[2] The same is illustrated in the chest radiographs in Figure 1, which were taken after obtaining consent from the patients. Differential diagnoses include diffuse pulmonary hemorrhage and diffuse pulmonary infection.
Figure 1.
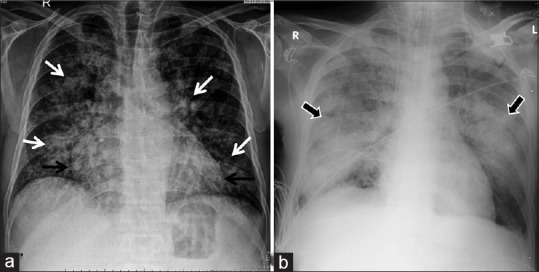
(a) Chest radiograph of a case of cardiogenic pulmonary edema showing cardiomegaly (black arrow) with fluffy air-space opacities in central as well as peripheral lungs (b) Chest radiograph of a case of noncardiogenic pulmonary edema showing batwing opacities (arrowheads) with air bronchogram and absence of cardiomegaly
References
- 1.Belice T, Yuce S, Kizilkaya B, Kurt A, Cure E. Noncardiac pulmonary edema induced by sitagliptin treatment. J Family Med Prim Care. 2014;3:456–7. doi: 10.4103/2249-4863.148149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Milne EN, Pistolesi M, Miniati M, Giuntini C. The radiologic distinction of cardiogenic and noncardiogenic edema. AJR Am J Roentgenol. 1985;144:879–94. doi: 10.2214/ajr.144.5.879. [DOI] [PubMed] [Google Scholar]


