Abstract
Background & Aims
Many patients with cryptogenic cirrhosis (CC) have other conditions associated with nonalcoholic steatohepatitis (NASH) that put them at risk for complications that preclude orthotopic liver transplantation (OLT).
Methods
We followed all patients with NASH and CC who were evaluated for OLT (n=218) at Baylor Regional Transplant Institute between March 2002 and May 2008. Data were compared with those from patients evaluated for OLT because of hepatitis C (HCV)-associated cirrhosis (n=646).
Results
Patients with NASH and CC were older, more likely to be female, had a higher body-mass index, and a greater prevalence of diabetes and hypertension, compared with patients with HCV-associated cirrhosis, but the two groups had similar MELD scores. NASH and CC in patients with MELD scores ≤15 were less likely to progress; these patients were less likely to receive OLT and more likely to die or be taken off the wait list because they were too sick, compared with patients with HCV-associated cirrhosis. The median progression rate among patients with NASH and CC was 1.3 MELD points/year vs. 3.2 MELD points/year for the HCV group (P=0.003). Among patients with MELD scores >15, there were no differences among groups in percentage that received transplants or rate of MELD score progression. Hepatocellular carcinoma occurred in 2.7% of patients with NASH and CC per year, compared with 4.7%/year among those with HCV-associated cirrhosis.
Conclusions
Patients NASH and CC and low MELD score have slower disease progression than patients with HCV-associated cirrhosis and are less likely to receive OLT.
Keywords: Liver Transplantation, NASH, Fatty liver, cirrhosis, Hepatitis C
Introduction
Nonalcoholic fatty liver disease (NAFLD) encompasses a spectrum of clinicopathologic conditions ranging from simple steatosis to NASH, which can progress to cirrhosis, end-stage liver disease and hepatocellular carcinoma.1–3 NASH connotes histologic changes consisting of steatosis, hepatocyte injury, lobular inflammation and/or fibrosis in the absence of alcohol ingestion.4 These histologic findings typically disappear after the development of cirrhosis.5, 6 Therefore, NASH is often inferred as the most likely cause of liver disease in patients with a diagnosis of cryptogenic cirrhosis (CC) and clinical features of the metabolic syndrome.7–9
The prevalence of NAFLD has steadily increased, paralleling the increase in obesity and type 2 diabetes mellitus. NAFLD currently affects approximately 30%–46% of the United States (US) adult population, depending on the population studied.10–15 However, the highest prevalence of NAFLD (90%) and NASH (30%) is seen in the morbidly obese population presenting for bariatric surgery.16–18 The rising prevalence of NASH led to speculation that it would surpass HCV as the leading indication for OLT by 2020.13, 19 However, this is controversial and may not occur as those with NASH are more likely than others to have advanced comorbid conditions such as cardiovascular disease or malignancy that preclude transplantation.20–23
As a result of the increasing prevalence of NASH, more patients are presenting for OLT evaluation with decompensation or HCC.24 To date the course of patients with NASH cirrhosis who are evaluated and listed for OLT has not been defined. Therefore, we aimed to: 1) define the course of patients with cirrhosis due to NASH/CC who are evaluated and/or listed for OLT and 2) to determine the incidence of HCC in NASH/CC patients listed for OLT.
Methods
Institutional review board approval was granted prior to the initiation of this retrospective study. We analyzed all patients >18 years of age who were referred for consideration of primary OLT at Baylor Regional Transplant Institute from March 2002 to May 2008. No living donor liver transplants were performed during this time. Demographic, lab, and imaging data were obtained from patients’ initial OLT evaluation. Non-liver related diagnoses such as diabetes and hypertension are recorded in the Baylor Liver Transplant Research Database if treatment for these conditions was documented in the medical record during their evaluation. NASH required liver biopsy confirmation while cryptogenic cirrhosis connoted absence of serologic evidence of other causes of liver disease or a history of significant alcohol use. All patients denied for OLT during the time period with a diagnosis of NASH/CC were compared to all patients denied for OLT with a diagnosis of HCV cirrhosis. When patients are denied for OLT, they were recorded as excluded for medical comorbidities, psychosocial reasons, adequate hepatic reserve, exceeding tumor criteria, or death. However, the specific comorbidities and psycosocial reasons are not recorded in our database. Thus a competing risk analysis could not be performed. Our center’s listing criteria require that candidates maintain a dry body weight less than 100 pounds over ideal body weight and this is applied to all patients regardless of their liver disease etiology.
All patients listed with a diagnosis of NASH/CC during the time period where compared to all patients listed with a diagnosis of HCV cirrhosis. We chose to include all HCV-infected patients in this group instead of matching them to NASH/CC patients in order to have a large cohort as one comparator group with a single diagnosis.
Patient characteristics were compared using Wilcoxon rank sum. Median values are reported in Tables 1 and 2. Patient survival and risk of development of HCC were evaluated by Kaplan-Meier analysis. Patients were not delisted for advanced liver disease unless it resulted in multiorgan system failure. SAS 9.1 was used for all statistical analyses.
Table 1.
Demographics of patients evaluated and denied for OLT.
| NASH/CC (n=197) |
HCV (n=586) |
P-value | ||
|---|---|---|---|---|
| Age* | 60 | 51 | P<0.001 | |
| Sex | Male | 43% | 65% | P<0.001 |
| Female | 57% | 35% | ||
| Race | White | 75% | 70% | NS |
| Black | 6% | 10% | ||
| Hispanic | 17% | 18% | ||
| Asian | 1% | 1% | ||
| Other | 1% | 1% | ||
| MELD* | 12 | 11 | NS | |
| CTP* | 7 | 7 | NS | |
| ALT* | 32 | 54 | P<0.001 | |
| Platelets* | 97 | 89 | NS | |
| BMI | % >30 | 59% | 40% | P<0.001 |
| GFR mL/min** | 74 | 88 | P<0.004 | |
| Denial Reason | Adequate Hepatic Reserve | 10% | 8% | P<0.001 |
| Comorbid Conditions | 72% | 27% | ||
| Died | 6% | 14% | ||
| Psychosocial Issues | 8% | 39% | ||
| Tumor Criteria | 3% | 9% | ||
| Other | 2% | 3% | ||
NASH= Non-alcoholic steatohepatitis; CC=cryptogenic cirrhosis; HCV = Hepatitis C
Median values are given
Glomerular filtration rate (GFR) was measured by sodium iothalamate clearance (glofil).
Table 2.
Demographics of patients listed for OLT.
| NASH/Cryptogenic (N=217) |
HCV (N=645) |
P-value | ||
|---|---|---|---|---|
| Age* | 56 | 51 | P<0.001 | |
| Sex | Male | 52% | 68% | P<0.001 |
| Female | 48% | 32% | ||
| Race | White | 77% | 74% | P=0.01 |
| Black | 3% | 8% | ||
| Hispanic | 19% | 16% | ||
| Asian | 0% | 1% | ||
| Other | 1% | 1% | ||
| MELD* | 14 | 14 | NS | |
| CTP* | 7 | 7 | NS | |
| ALT* | 37 | 62 | P<0.001 | |
| Platelets* | 86 | 73 | P=0.005 | |
| Diabetes | 55% | 22% | P<0.001 | |
| Hypertension | 46% | 28% | P<0.001 | |
| BMI | % > 30 | 54% | 42% | P=0.004 |
| GFR mL/min** | 82 | 102 | P<0.001 | |
| HCC at any time | 12% | 27% | P<0.001 | |
NASH= Non-alcoholic steatohepatitis; CC=cryptogenic cirrhosis; HCV = Hepatitis C
Median values are given
Glomerular filtration rate (GFR) was measured by sodium iothalamate clearance (glofil).
Results
Evaluated, but not listed patients
During the study period, 415 patients with NASH/CC and 1232 patients with HCV cirrhosis (30% of whom had concominant alcohol consumption) were evaluated for OLT; 48% of each group were not approved for listing for liver transplantation. Table 1a compares the characteristics of the 197 patients denied for listing with a diagnosis of NASH/CC cirrhosis and the 586 patients denied for listing with a diagnosis of HCV cirrhosis. NASH/CC patients who were denied listing were older (median age 60 vs. 51; P<0.001), more likely to be female (57% vs. 35%; P<0.001), heavier (body mass index (BMI) >30: 59% vs. 40%; P<0.001), and had a lower glomerular filtration rate (GFR) (74 mL/min vs. 88 mL/min; P=0.004) when compared to HCV patients who were denied. Despite differences in patient characteristics, liver disease severity at the time of evaluation, as measured by the MELD and Child-Turcotte-Pugh scores, were similar. While all patients in these groups were denied listing for OLT, the reasons for denial were different. NASH/CC patients were most likely to be denied for comorbid conditions (72%), whereas HCV patients were most likely to be denied for psychosocial reasons including ongoing psychological issues, recidivism, and lack of social support (39%; P<0.001).
Listed patients
Table 2 compares the 217 patients listed for OLT with a diagnosis of NASH/CC to the 645 patients listed for OLT with a diagnosis of HCV cirrhosis (27% of whom had concominant alcohol consumption).
Listed patients with NASH/CC were older (56 vs. 51 years; P<0.001) and more likely to be female (48% vs. 32%; P<0.001). They also had a higher percentage of patients with a BMI >30 (54% vs. 42%; P=0.004), diabetes (55% vs. 22%; P<0.001), or hypertension (46% vs. 28%; P<0.001) than HCV patients. GFR (82 vs. 102 mL/min; P<0.001) and alanine aminotransferase (ALT) (37 vs. 62; U/L (P<0.001) were lower in NASH/CC patients than in HCV patients. In addition, HCC was less common in NASH/CC than in HCV patients (12% vs. 27%; P<0.001). Despite these differences, liver disease severity, as measured by median MELD score (14 for both; P=NS) and Child-Turcotte-Pugh point system (7 for both; P=NS), was the same.
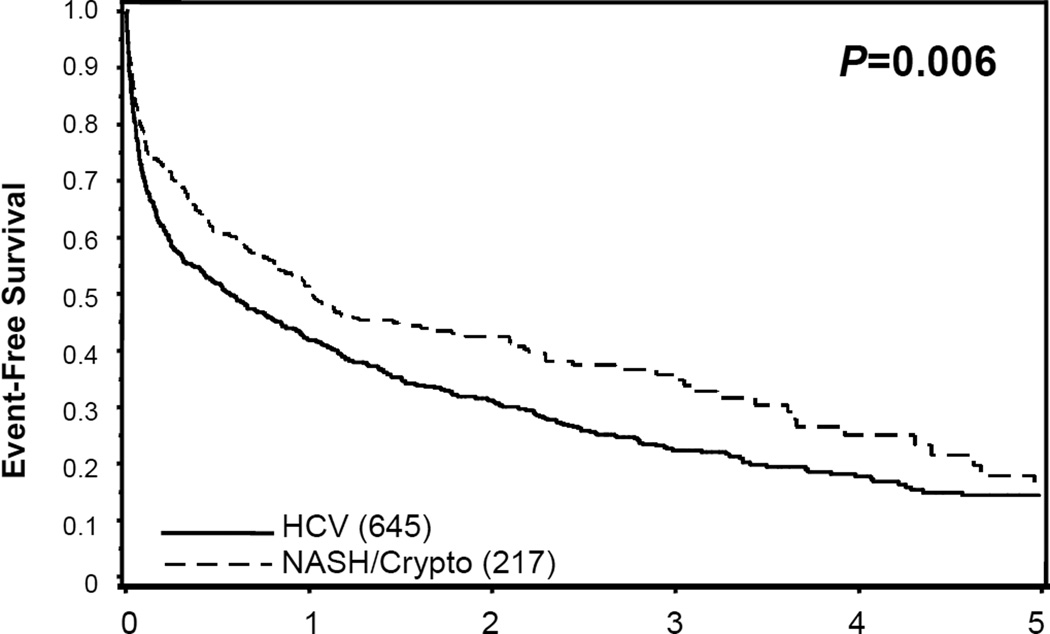
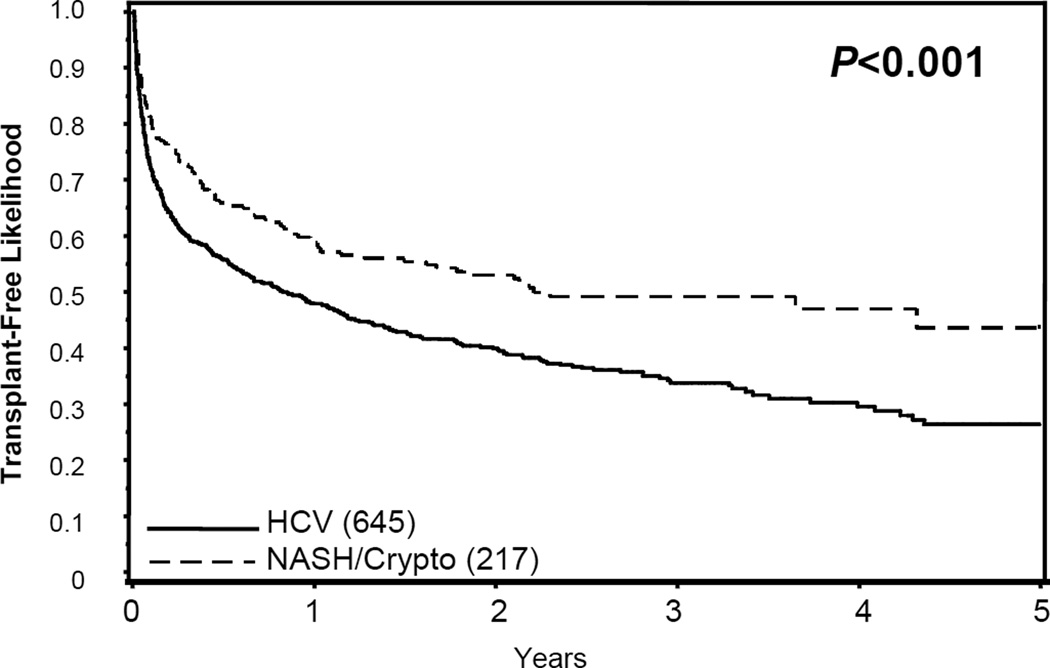
Overall, patients with NASH/CC were less likely to be transplanted than patients with HCV (48% vs. 62%; P<0.001). While listed, 22% of NASH/CC patients and 16% of HCV patients either died on the list or were delisted for being too ill. NASH/CC patients were less likely to reach an endpoint (Figure 1) (death, delisting, or transplantation; P=0.006) after a median of 12.3 months on the transplant waiting list. Liver transplantation was significantly less common in surviving NASH/CC patients who remained on the list (Figure 2) (P<0.001). Thus, NASH/CC patients were not only less likely to be transplanted, but more likely to die or be delisted while waiting compared to HCV patients.
Figure 1.
Event-free survival is shown. An event was defined as liver transplant, death, or delisting for being too sick.
Figure 2.
Transplant-free probability is shown. An event was defined as liver transplant only. Patients were censored who died or were delisted for being too sick.
Among patients listed with an initial MELD score ≤15, NASH/CC patients were less likely to progress and be transplanted than HCV patients (27% vs. 46%; P<0.001). NASH/CC patients with MELD scores ≤15 were also more likely to be delisted or die while waiting (26%), compared to HCV patients (26% vs. 20%; P<0.001). The median time on the waiting list was 382 days for NASH/CC cirrhosis and 355 days for HCV cirrhosis (P=0.06). While listed, the median progression per year based on calculated MELD score for those with a MELD ≤15 was slower for NASH/CC patients than HCV patients (1.3 vs. 3.2 MELD points/year; P=0.003). These trends did not hold for patients listed with MELD scores >15, as the majority of patients, regardless of their type of liver disease, received an OLT. Specifically, 79% of NASH/CC patients, 86% of HCV patients were subsequently transplanted (P=NS), while 16% of NASH/CC patients and 8% of HCV patients were delisted or died while waiting. Patients were transplanted with median calculated MELD scores of 20 vs. 17, in the NASH/CC group, HCV group respectively (patients with HCC exception points were excluded from this analysis; P=0.01). The median MELD progression per year in patients listed with a MELD >15 was similar in the 2 groups (P=NS). Patients listed with a calculated MELD score >15 were generally transplanted within the first year and thus a MELD progression rate could not be calculated (P=NS).
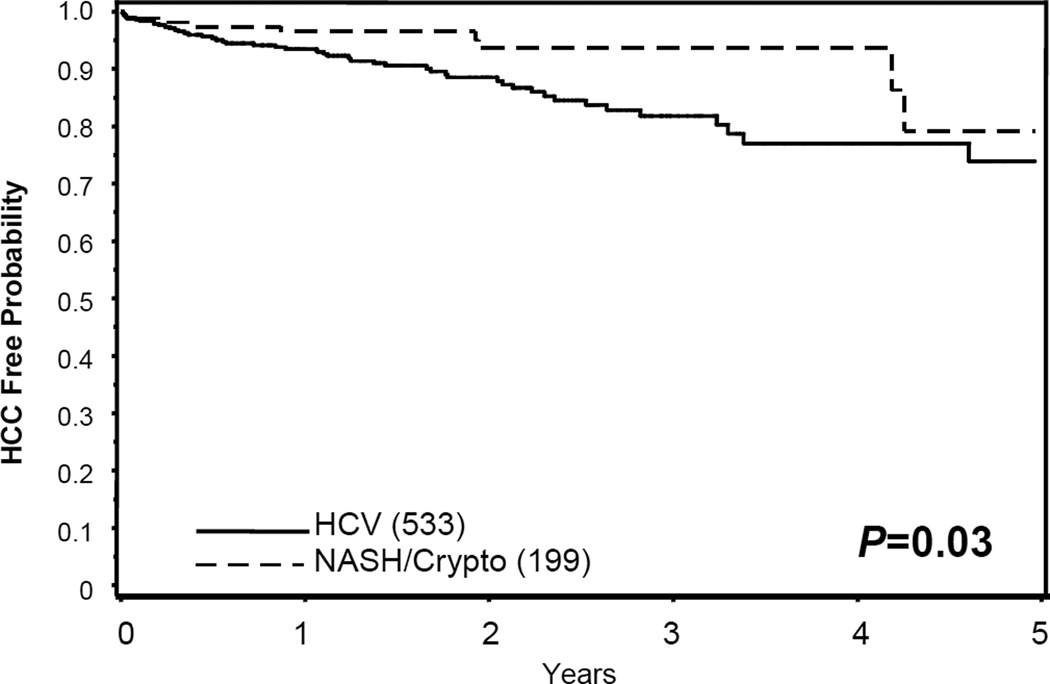
Incidental HCC discovered in explanted livers at the time of transplant were given a diagnosis of HCC on the date of transplant. The likelihood of HCC developing while listed for OLT in NASH/CC and HCV patients is shown in Figure 3 (P=0.03). The average per annum incidence of HCC in listed patients was: 2.7% in NASH/CC patients and 4.7% HCV patients (Table 3).
Figure 3.
Likelihood of remaining free of hepatocellular carcinoma (HCC) while awaiting liver transplantation.
Table 3.
Hepatocellular carcinoma in referred and listed patients.
| NASH/CC | HCV | P-value | ||
|---|---|---|---|---|
| Number | HCC | 26 | 175 | P<0.001 |
| No HCC | 191 | 470 | ||
| Found | Referral diagnosis | 9 | 79 | NS |
| At evaluation | 5 | 36 | ||
| During follow-up | 12 | 60 | ||
| Number HCC/year | 2.7% | 4.7% | P=0.04 | |
NASH= Non-alcoholic steatohepatitis; CC=cryptogenic cirrhosis; HCV= Hepatitis C virus
We next combined all patients evaluated for OLT with NASH/CC and HCV and evaluated factors associated with listing or denial (Supplemental Table 4). Univariate analysis found that older patients without HCC with a lower MELD and GFR, higher BMI, who had diabetes and hypertension were more commonly denied for OLT. Multivariable analysis found that older patients without HCC with a lower MELD and GFR were less likely to be listed.
We also combined all listed patients with NASH/CC and HCV and evaluated factors associated with death or delisting vs. transplant or continued waiting (Supplemental Table 5). Univariate analysis found that older patients without HCC with a lower MELD and GFR, higher BMI, who had diabetes, and hypertension were more likely to die or be delisted. Multivariable analysis found that older patients without HCC with low MELD and high BMI were more likely to die or be delisted.
Discussion
As the obesity epidemic continues, the prevalence of NAFLD has increased. However, since advanced fibrosis in uncommon, the impact of this epidemic on the need for transplantation is unclear.11, 13, 15 The pathologic signs of NASH often disappear when cirrhosis develops, therefore the diagnosis is hard to confirm in retrospect and, as a result, many of these patients are labeled as CC.7–9 Although we acknowledge that a minority of patients with CC may represent other diagnostic entities, we chose to analyze NASH and CC patients together as one group.
The number of liver transplants for NASH/CC nationwide has increased over time, coincident with the increasing prevalence of NAFLD.13, 24, 25 In addition, the number of new referrals to Baylor Regional Transplant Institute for NASH/CC has increased over our study period (data not shown; P=0.04). Although some have suggested that NASH cirrhosis would overtake HCV as the main indication for OLT by 2020, this does not seem likely since coincident comorbid conditions often found in NASH/CC patients may often preclude OLT.13,20–22 In fact, our data confirm this suspicion; NASH/CC patients were almost twice as likely as HCV cirrhosis patients to be denied for listing because of comorbid conditions. Furthermore, NASH/CC patients listed for transplant with a low MELD were less likely to receive a transplant since they progressed slowly and were more likely to die or be delisted, usually due to complications of their comorbid diseases. In contrast, patients with MELD scores >15 were likely to receive an OLT regardless of their diagnosis.
Interestingly, the presence of comorbid conditions does not appear to affect early post-OLT outcomes as compared to those transplanted for other diseases.26, 27 However, over the long-term, NASH/CC transplant recipients are more likely to die of cardiovascular disease while HCV patients are more likely to die of recurrent liver disease.26 While this confirms that the current selection process is adequate to choose patients who benefit from OLT, it likely masks a selection bias in that those with comorbid conditions are not referred for transplant evaluation, not approved for listing, and not transplanted as often as others. This selection appears justified by the observation that NASH/CC patients with diabetes, hypertension, BMI >30 and age >60 years have a 50% one year mortality.27 Thus despite good survival in the currently selected cohort, we should not expand our criteria for OLT to include NASH/CC patients with multiple comorbid conditions. Instead, the primary focus of treatment in NASH/CC patients with a low MELD score needs to be aggressive treatment of their obesity, diabetes, lipid disorders, and hypertension so that they do not develop comorbid conditions that cause death or make them ineligible for transplant.
Hepatocellular carcinoma (HCC) is another well-described complication of cirrhosis. Only one previous study reported a 2.6% per year incidence of HCC in NASH patients.28 However, that study was subject to selection bias, and about a third of their patients had a history of alcohol use. Nonetheless, the incidence of HCC in our study was similar (2.7% per year). This may be related to rigorous surveillance, longer disease duration, and/or more advanced liver disease in our listed patients than in previously reported patient populations.14, 28
In conclusion, although a similar number of NASH/CC and HCV patients were denied OLT, NASH/CC patients are more likely to be denied for transplant because of comorbid conditions and are less likely to be transplanted even if listed compared to HCV cirrhosis patients. This difference is predominantly seen in NASH/CC patients with low MELD scores, who have a slower rate of liver disease progression than those with hepatitis C. Therefore, in an era of increased emphasis on cost-effective medicine, one may consider waiting to evaluate patients with NASH/CC for transplant until their MELD is >15.
Supplementary Material
Acknowledgments
No grant support.
Footnotes
Jacqueline G. O’Leary MD MPH - contributed to the whole content, concept design, acquisition of data, analysis and interpretation of data, drafting the manuscript
Carmen Landaverde MD - contributed to part of the content, drafting part of the manuscript and critical revision.
Linda Jennings – contributed to statistical analysis
Robert M. Goldstein MD – contributed to part of the content, revising of the manuscript.
Gary L. Davis MD - contributed to the whole content, advising of concept design, analysis and interpretation of data, critical revision of the manuscript and statistical analysis.
No conflicts of interest exist for any author.
References
- 1.Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99–S112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 2.Zelman S. The liver in obesity. AMA Arch Intern Med. 1952;90:141–156. doi: 10.1001/archinte.1952.00240080007002. [DOI] [PubMed] [Google Scholar]
- 3.Matteoni CA, Younossi ZM. In diagnosing hepatitis C, which patient needs which test? Cleve Clin J Med. 1999;66:529–530. doi: 10.3949/ccjm.66.9.529. [DOI] [PubMed] [Google Scholar]
- 4.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 5.Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol. 2005;42:132–138. doi: 10.1016/j.jhep.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107:1103–1109. doi: 10.1016/0016-5085(94)90235-6. [DOI] [PubMed] [Google Scholar]
- 7.Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–669. doi: 10.1002/hep.510290347. [DOI] [PubMed] [Google Scholar]
- 8.Ayata G, Gordon FD, Lewis WD, Pomfret E, Pomposelli JJ, Jenkins RL, Khettry U. Cryptogenic cirrhosis: clinicopathologic findings at and after liver transplantation. Hum Pathol. 2002;33:1098–1104. doi: 10.1053/hupa.2002.129419. [DOI] [PubMed] [Google Scholar]
- 9.Clark JM, Diehl AM. Nonalcoholic fatty liver disease: an underrecognized cause of cryptogenic cirrhosis. JAMA. 2003;289:3000–3004. doi: 10.1001/jama.289.22.3000. [DOI] [PubMed] [Google Scholar]
- 10.Fraser A, Longnecker MP, Lawlor DA. Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999–2004. Gastroenterology. 2007;133:1814–1820. doi: 10.1053/j.gastro.2007.08.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 12.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 13.Charlton M. Nonalcoholic fatty liver disease: a review of current understanding and future impact. Clin Gastroenterol Hepatol. 2004;2:1048–1058. doi: 10.1016/s1542-3565(04)00440-9. [DOI] [PubMed] [Google Scholar]
- 14.Page JM, Harrison SA. NASH and HCC. Clin Liver Dis. 2009;13:631–647. doi: 10.1016/j.cld.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, Landt CL, Harrison SA. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 16.Gholam PM, Flancbaum L, Machan JT, Charney DA, Kotler DP. Nonalcoholic fatty liver disease in severely obese subjects. Am J Gastroenterol. 2007;102:399–408. doi: 10.1111/j.1572-0241.2006.01041.x. [DOI] [PubMed] [Google Scholar]
- 17.Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. J Hepatol. 2006;45:600–606. doi: 10.1016/j.jhep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 18.Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: a global perspective. Semin Liver Dis. 2008;28:339–350. doi: 10.1055/s-0028-1091978. [DOI] [PubMed] [Google Scholar]
- 19.Burke A, Lucey MR. Non-alcoholic fatty liver disease, non-alcoholic steatohepatitis and orthotopic liver transplantation. Am J Transplant. 2004;4:686–693. doi: 10.1111/j.1600-6143.2004.00432.x. [DOI] [PubMed] [Google Scholar]
- 20.Yatsuji S, Hashimoto E, Tobari M, Taniai M, Tokushige K, Shiratori K. Clinical features and outcomes of cirrhosis due to non-alcoholic steatohepatitis compared with cirrhosis caused by chronic hepatitis C. J Gastroenterol Hepatol. 2009;24:248–254. doi: 10.1111/j.1440-1746.2008.05640.x. [DOI] [PubMed] [Google Scholar]
- 21.Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 22.Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008;49:608–612. doi: 10.1016/j.jhep.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 23.Rafiq N, Younossi ZM. Nonalcoholic fatty liver disease: a practical approach to evaluation and management. Clin Liver Dis. 2009;13:249–266. doi: 10.1016/j.cld.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Angulo P. Nonalcoholic fatty liver disease and liver transplantation. Liver Transpl. 2006;12:523–534. doi: 10.1002/lt.20738. [DOI] [PubMed] [Google Scholar]
- 25.O'Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008;134:1764–1776. doi: 10.1053/j.gastro.2008.02.028. [DOI] [PubMed] [Google Scholar]
- 26.Yalamanchili K, Saadeh S, Klintmalm GB, Jennings LW, Davis GL. Nonalcoholic fatty liver disease after liver transplantation for cryptogenic cirrhosis or nonalcoholic fatty liver disease. Liver Transpl. 16:431–439. doi: 10.1002/lt.22004. [DOI] [PubMed] [Google Scholar]
- 27.Malik SM, deVera ME, Fontes P, Shaikh O, Ahmad J. Outcome after liver transplantation for NASH cirrhosis. Am J Transplant. 2009;9:782–793. doi: 10.1111/j.1600-6143.2009.02590.x. [DOI] [PubMed] [Google Scholar]
- 28.Ascha MS, Hanouneh IA, Lopez R, Tamimi TA, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972–1978. doi: 10.1002/hep.23527. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.