Abstract
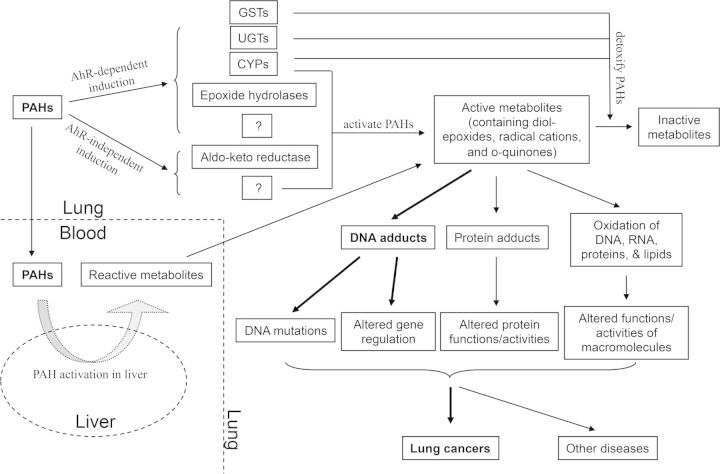
Excessive exposure to polycyclic aromatic hydrocarbons (PAHs) often results in lung cancer, a disease with the highest cancer mortality in the United States. After entry into the lung, PAHs induce phase I metabolic enzymes such as cytochrome P450 (CYP) monooxygenases, i.e. CYP1A1/2 and 1B1, and phase II enzymes such as glutathione S-transferases, UDP glucuronyl transferases, NADPH quinone oxidoreductases (NQOs), aldo-keto reductases (AKRs), and epoxide hydrolases (EHs), via the aryl hydrocarbon receptor (AhR)-dependent and independent pathways. Humans can also be exposed to PAHs through diet, via consumption of charcoal broiled foods. Metabolism of PAHs through the CYP1A1/1B1/EH pathway, CYP peroxidase pathway, and AKR pathway leads to the formation of the active carcinogens diol-epoxides, radical cations, and o-quinones. These reactive metabolites produce DNA adducts, resulting in DNA mutations, alteration of gene expression profiles, and tumorigenesis. Mutations in xenobiotic metabolic enzymes, as well as polymorphisms of tumor suppressor genes (e.g. p53) and/or genes involved in gene expression (e.g. X-ray repair cross-complementing proteins), are associated with lung cancer susceptibility in human populations from different ethnicities, gender, and age groups. Although various metabolic activation/inactivation pathways, AhR signaling, and genetic susceptibilities contribute to lung cancer, the precise points at which PAHs induce tumor initiation remain unknown. The goal of this review is to provide a current state-of-the-science of the mechanisms of human lung carcinogenesis mediated by PAHs, the experimental approaches used to study this complex class of compounds, and future directions for research of these compounds.
Keywords: polycyclic aromatic hydrocarbons, PAH, lung cancer, Ah receptor, carcinogenesis, genetic susceptibility, metabolism, mixtures
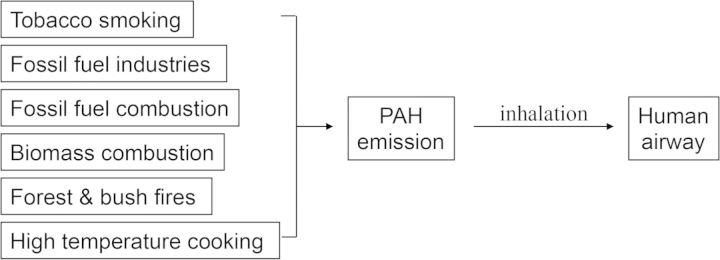
Lung cancer is the leading cause of cancer-related death in both men and women (Horn et al., 2012), responsible for 1.59 million deaths around the world in 2012 (IARC, 2012). Approximately 90% of lung cancer cases are related to tobacco smoking and 1–2% are accounted for by outdoor air pollution and secondhand smoke. Inhalation of incomplete indoor/outdoor combustion of coal and wood may induce lung cancer as well (Reid et al., 2012). Among the many components in tobacco smoke and outdoor and indoor air pollution are polycyclic aromatic hydrocarbons (PAHs), which are defined as a group of chemicals containing 2 or more fused benzene rings but no heteroatoms (Agency for Toxic Substances and Disease Registry (ATSDR) December, 1990). The PAHs are considered to be the most important carcinogens in these complex mixtures (Hecht, 2002, 2011; Rubin, 2001). Although PAHs can exist in hundreds of different combinations, the National Waste Minimization Program defines this group using the Toxic Release Inventory reporting category for PAHs, which include 20 compounds, such as benzo[a]pyrene (BaP), dibenzo[a,h]anthracene, 3-methylcholanthrene, 5-methylchrysene, and 7,12-dimethylbenz[a]anthracene (Agency for Toxic Substances and Disease Registry (ATSDR) December, 1990).
Inhalation exposure to PAH-containing substances increases the risk of lung cancer in humans (DeMarini, 2004; Eom et al., 2013; Osgood et al., 2013; Tsay et al., 2013). It is estimated that there is 100 ng or more of total PAHs per gram of tobacco, regardless of the manufacturers and brands (Grimmer et al., 1988), and smokers inhale ∼0.26 μg of BaP per pack of 20 cigarettes (Piccardo et al., 2010). Domestic wood burning and road traffic are also major sources of PAHs (Bostrom et al., 2002). For example, in Stockholm, Sweden, the sum of 14 different PAHs was 100–200 ng/m3 (taken from road samples), with the most abundant being phenanthrene and BaP, both of which varied between 1 and 2 ng/m3.
In addition to inhalation, it is well established that, in cigarette and cigar smokers, considerably greater amounts of PAHs are swallowed and enter the gastrointestinal tract than those that enter through the lung (Jarup, 2003; Nebert et al., 2013; Rozman and Klaassen, 2007). Significant amounts (0.1–20 µg/kg; up to 100 µg/kg) of PAHs are also detected in grilled, barbecued, or smoked meat products (Hansen et al., 1992; Larsson et al., 1983; Masuda et al., 1966; Mottier et al., 2000; Simko, 2002; Sinha et al., 1994) (Fig. 1). Consumption of fried chicken and smoked dried beef translates to BaP concentrations of 5.4–5.5 μg/kg, and charcoal-broiled steak contains BaP level of ∼9.0 μg/kg. This amounts to an extrapolated environmental dose of ∼40–50 ng/kg/day. However, BaP concentrations have been reported to be as high as 19 μg/kg in smoked meat in Austria (Tiefenbacher et al., 1982) and 69 μg/kg in rape seed oil (Pupin and Toledo, 1996). Ingestion of these foods would increase BaP amounts to 80–380 ng/kg/day (Pupin and Toledo, 1996). Researchers have not found a direct link between dietary PAH exposure and lung cancer incidence, except for one recent study from China (Cai et al., 2012).
FIG. 1.
Major sources through which PAH exposure occurs in humans.
Although much research has been conducted on PAHs and the various components that occur within environmental PAH-containing mixtures, a comprehensive review of the mechanisms by which PAHs contribute to lung cancer has not been written. This review will provide an overview of the current state-of-the-science of the metabolism of PAHs and how these processes contribute to lung cancer, information on mode of action to inform current health assessments, and knowledge gaps to determine the next steps for research on these compounds. Specifically, this review will evaluate the most commonly studied PAHs including BaP and the novel approaches used to study the mechanisms by which these compounds may cause lung cancer. Moreover, a thorough understanding of these mechanisms by which PAHs induce cancer may lead to more targeted treatments for lung cancer, which often has a poor prognosis and results in billions of dollars expended on health care costs associated with this disease.
THE PAHs—A COMPLEX GROUP OF COMPOUNDS
The carcinogenicity of PAHs is associated with the complexity of the molecule (i.e. increasing number of benzenoid rings). According to the United States Environmental Protection Agency, there are at least 11 carcinogenic or mutagenic PAHs. The International Agency for Research on Cancer (IARC) lists the following PAHs as human carcinogens or potential carcinogens: benz[a]anthracene, benzo[b]fluoranthene, benzo[j]fluoranthene, BaP,dibenz[a,h]anthracene, 7H-dibenzo[c,g]carbazole, dibenzo[a,h]pyrene, dibenzo[a,i]pyrene, indeno[1,2,3-cd]pyrene, benzo[k]fluoranthene, dibenzo[a,e]pyrene, dibenzo[a,l]pyrene, and 5-methylchrysene (Fig. 2) (IARC, 2010). The PAHs have been classified as belonging to different groups (IARC, 2010), based on their carcinogenicities. BaP is carcinogenic to humans (Group 1). Cyclopenta[cd]pyrene (Fig. 2), dibenz[a,h]anthracene, and dibenzo[a,l]pyrene are probably carcinogenic to humans (Group 2A). Benz[j]aceanthrylene, benz[a]anthracene, benzo[b]fluoranthene, benzo[j]fluoranthene, benzo[k]fluoranthene, benzo[c]phenanthrene, chrysene, dibenzo[a,h]pyrene, dibenzo[a,i]-pyrene, indeno[1,2,3-cd]pyrene, and 5-methylchrysene are possibly carcinogenic to humans (Group 2B) (Fig. 2).
FIG. 2.
Chemical structure of PAHs.
BaP has often served as a reference for the carcinogenicity of other PAHs (Bostrom et al., 2002) and most studies have been conducted using BaP because of its known carcinogenic effects. It is important to note, however, that other PAHs need to be studied as well, in addition to BaP.
MECHANISMS OF ACTIVATION OF CARCINOGENIC PAHs
In general, PAHs are lipophilic compounds that can easily cross cell membranes through passive diffusion after inhalation. The parental PAH molecules that enter pulmonary cells are considered procarcinogens because they do not directly induce DNA damage (Alexandrov et al., 2010; Miller and Ramos, 2001; Ramos and Moorthy, 2005; Rybicki et al., 2006). Rather, it is the transformation of a single PAH into its carcinogenic metabolites that contribute to cancer etiology. Transformation of these compounds involves multiple metabolic enzymes and 3 known major pathways: the CYP1A1/1B1 and epoxide hydrolase pathway (CYP/EH pathway), CYP peroxidase pathway, and aldo-keto reductases pathway (AKR pathway). In general, PAHs are metabolized by CYPs and other metabolic enzymes into phenols, catechols, and quinones, resulting in the formation of diol-epoxides, radical cations, or reactive and redox-active o-quinones, which may all react with DNA to produce DNA adducts. For example, quinones react with the N-7 of guanine and N-3 of adenine in DNA (Liu et al., 2002). This formation of DNA adducts can cause mismatch in DNA replication, as well as altered promoter methylation and/or promoter binding (Yang et al., 2012), leading to an inheritable DNA mutation or abnormal gene expression, and ultimately tumorigenesis. Although PAHs are not considered liver carcinogens, they do become metabolized to DNA-reactive metabolites in liver following oral exposure (Kondraganti et al., 2003).
The reactive metabolites of PAHs may also induce the formation of protein adducts in cells (Berge et al., 2004; Kafferlein et al., 2010), which may affect the normal activities of these proteins. PAH metabolites may also trigger an elevation in reactive oxygen species (ROS), which can directly affect DNA, lipids (Kwack and Lee, 2000), or proteins and initiate carcinogenesis.
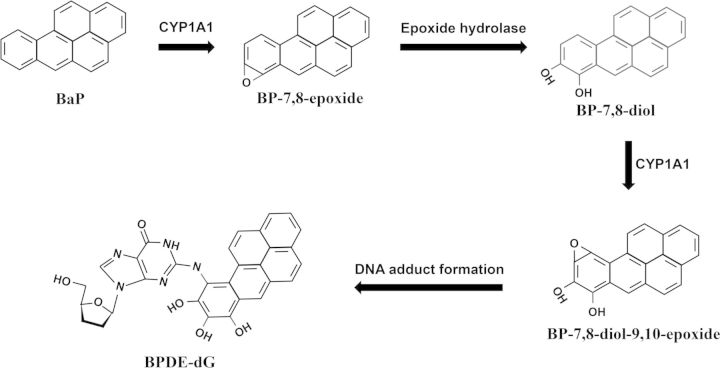
The most commonly studied PAH, BaP, is transformed in vivo into BP-7,8-epoxide by CYP1A1 via the CYP/EH pathway. BP-7,8-epoxide is further oxidized by EH to form BP-7,8-dihydrodiol, followed by the final step of CYP1A1-catalyzed hydroxylation to form BP-7,8-dihydrodiol-9,10-epoxide (BPDE), the ultimate carcinogen (Beresford, 1993) (Fig. 3). BPDE reacts with DNA to produce adducts that have been identified in lung tissues of smokers, and may cause mutations that are observed in p53 tumor suppressor gene and KRAS oncogene (Conney, 1982; Denissenko et al., 1996; Geacintov et al., 1997; Pfeifer and Besaratinia, 2009; Rojas et al., 1998). Denissenko et al. (1996) reported that adduct formation was gene sequence-specific, with adducts being formed at codons 157, 248, and 273. Mutations of these sequences on the p53 gene lead to carcinogenesis and have been linked to human lung cancers (Denissenko et al., 1996). Thus, targeted adduct formation rather than phenotypic selection appears to shape the p53 mutational spectrum in lung cancer. These results provide a direct etiological link between a defined chemical carcinogen and human cancer.
FIG. 3.
Major pathways of metabolic activation of the PAH BaP to DNA-binding metabolites.
CYPs also contain a ‘peroxidase-like’ activity (Hrycay and Bandiera, 2012), which catalyze one-electron oxidation of BaP at the C6 position to produce radical cations (Cavalieri and Rogan, 1985). These PAH-derived radical cations, though short-lived, can react with DNA and cause mutations (Devanesan et al., 1992).
In the AKR pathway, dihydrodiol dehydrogenase, a member of the aldo-keto reductase superfamily, catalyzes dehydrogenation of BP-7,8-diol, a BaP metabolite, to form a BP catechol (Burczynski et al., 1999). Further oxidations of catechols generate o-quinones. Redox cycling of quinones could lead to formation of ROS, which could also lead to carcinogenesis via oxidative DNA damage (Moorthy et al., 2002). In 2004, Lan et al. (2004) reported that AKR1C3-Gln/Gln genotype was associated with a 1.84-fold increased risk of lung cancer in a Chinese population with high coal smoke exposure, indicating a significant role of the AKR pathway in PAH activation in lung carcinogenesis.
Thus, the following pathways operate in the metabolic activation of PAHs (Borza et al., 2008): (i) formation of dihydrodiol epoxides requiring 2 CYP-catalyzed oxidations and epoxide hydrolase; (ii) formation of phenols via radical cations by 1-electron oxidation (Cavalieri and Rogan, 1985); and (iii) formation of o-quinones via catechols by involvement of aldo-keto reductases with formation of ROS (Fig. 4).
FIG. 4.
Multiple mechanisms by which PAHs cause lung cancer.
CURRENT RESEARCH ON PAH-INDUCED AHR ACTIVATION
The mechanism by which PAHs contribute to AhR-dependent induction is well understood (Marlowe and Puga, 2005; Nebert et al., 2004; Ramadoss et al., 2005) (Fig. 4). AhR is expressed in almost all tissues and is highly expressed in liver, adipose tissue, and bronchial epithelial cells (Tsay et al., 2013). AhR is a transcription factor normally wrapped within an inactive protein complex in the cytosol. PAH binding to the receptor releases a key component, hepatitis B virus X-associated protein 2, from the AhR complex, resulting in the translocation of the AhR complex into the nucleus. Once in the nucleus, a dimer of heat shock protein 90 (Hsp90) is released from the complex, allowing dimerization of AhR with the AhR nuclear translocator (ARNT). This AhR/ARNT heterodimer is the active form of the AhR transcription factor. This transcription factor is then able to recognize AhR-responsive elements (AHREs) in promoter regions of AhR responsive genes and regulate their transcription to alter expression levels of a battery of AhR-regulated genes, including CYP1 isoforms.
Carcinogenic PAHs such as BaP or 3-methylcholanthrene are ligands of AhR (Nebert et al., 2004). Activation of the AhR has a variety of other downstream effects that include formation of DNA adducts (via CYP1A/1B1-dependent metabolic activation), tumorigenesis, inflammation, cell proliferation, and loss of cell-cell adhesion (Tsay et al., 2013). Because of its high level of expression in human bronchial epithelial cells, AhR has many physiological consequences in the lung such as its effects on cell proliferation and differentiation, cell-cell adhesion interaction, cytokine expression, mucin production, and xenobiotic metabolism (Chiba et al., 2011). Numerous studies have shown that the AhR also plays an important role in the development of lung cancer. Matsumoto et al. (2007) have shown that urban particulate matter induced lung cancer in wild type (AhR+/+), but not in AhR-null mice, suggesting that AhR plays a mechanistic role in the development of lung tumorigenesis by urban particulate matter, and this occurred through CYP1A1 induction (Matsumoto et al., 2007). Therefore, the AhR plays an important role in lung tumorigenesis mediated by PAHs, and understanding the role of the AhR in lung tumorigenesis may lead to the identification of novel biomarkers for early diagnosis/prognosis and new targets for therapy. For example, tanespimycin (17-Allylamino-17-demethoxygeldanamycin), an Hsp90 inhibitor, is a drug candidate to treat lung cancer. Although tanespimycin decreases AhR levels and AhR-regulated gene expression in multiple lung adenocarcinoma cells, AhR expression is associated with increased anticancer activity of tanespimycin (Chen et al., 2013), thereby suggesting both the significance and complexity of the AhR in regard to PAH activation, metabolism, and lung cancer therapy.
PAH ACTIVATION BY CYTOCHROME P450s
CYPs account for ∼75% of the total metabolic enzymes for the various xenobiotics humans are exposed to everyday (Guengerich, 2008), and they are the major metabolic enzymes that catalyze the oxidation of organic substances such as PAHs. The CYP1 family, including CYP1A1, CYP1A2, and CYP1B1, plays a pivotal role in PAH activation (Bowes et al., 1996; Moorthy, 2008; Shimada et al., 1996, 2001; Walsh et al., 2013). This has been demonstrated by studies from Shimada et al. (2010), in which CYP1A1 catalyzed PAHs faster than other isoforms like CYP1A2, 2C9, 3A4, and 2C19. Other isoforms such as CYP2A6, 2B6, 2C8, 2D6, 2E1, 3A5, 3A7, and 4A11 may not play a significant role in PAH metabolism (Shimada et al., 2001).
CYP1 isoforms are all monooxygenases, which incorporate 1 oxygen atom into a substrate, often generating oxidative epoxides (Nebert et al., 2004). Endogenous CYP1A1, but not CYP1A2, is expressed in lung, and pulmonary CYP1A1 is highly inducible by PAHs (Choudhary et al., 2003; Jiang et al., 2004) (Fig. 4). Such induction may last weeks and months after exposure to PAHs is discontinued (Fazili et al., 2010; Jiang et al., 2009; Moorthy, 2000; Moorthy et al., 1993), a phenomenon that may have important implications for carcinogenesis (Moorthy, 2008).
CYP1B1, which is expressed in lung and other extra-hepatic tissues (Dey et al., 1999), is also known to play an important role in PAH metabolism in relation to carcinogenesis. Human CYP1B1 plays an important role in the activation of diverse pro-carcinogens such as BaP, BaP-7-8-diol, dibenzo[a]pyrene, benz[a]anthracene, 7,12-dimethylbenz[a]anthracene, 7,12-dimethylbenz[a]anthracene-3,4-diol, 5-methylchrysene, 2-nitropyrene, 3-methoxy-4-aminoazobenzene, etc.
CYP1B1 is also over-expressed in various tumor tissues, and therefore could be considered a histopathological tumor marker (Liehr et al., 1995; Murray et al., 1997; Spencer et al., 1999; Spink et al., 1997). Uppstad et al. (2010), using RNA interference studies, compared the individual role(s) of CYP1A1 and CYP1B1 in the metabolic activation of BaP to its carcinogenic metabolites in human lung cells, and showed a major role for CYP1A1 in the formation of carcinogenic BaP diol-epoxides, whereas both CYP1A1 and 1B1 contribute significantly to the formation of BaP-cis and trans-7,8-dihydrodiol isomers. On the other hand, Shimada et al. (1999) showed that CYP1B1, together with epoxide hydrolase, catalyzes the conversion of BaP to BaP-7.8-diol at much higher (∼10-fold) higher than CYP1A1.
DETOXIFICATION OF PAHs
Recent studies also suggest an important role for CYPs in the detoxification of PAHs (Arlt et al., 2012; Joubert et al., 2012). Nebert et al. (2013) showed that CYP1A1 is an absolute requirement for detoxification of oral BaP (Uno et al., 2006). Preliminary studies from one of our laboratories have suggested that CYP1A1 and 1A2 have reciprocal roles in lung cancer, with CYP1A1 playing a role in PAH activation, and 1A2 in their detoxification (Jiang, Zhou, Maturu, Wang, and Moorthy, unpublished data). Phase II enzymes in the liver are also responsible for the clearance of PAHs. Beside UDP glucuronyl transferases (Saengtienchai et al., 2014), glutathione S-transferase Mu 1 (GSTM1) detoxifies PAHs (Fig. 4). Furthermore, the importance of this enzyme for detoxification has been indicated in GSTM null women, who exhibit a higher risk of lung cancer (Bennett et al., 1999).
MODELS AND APPROACHES TO STUDY PAH METABOLISM
Due to the complexity of PAH metabolic pathways and metabolic enzymes (Fig. 4), in vitro cell culture may not seem suitable to simulate the PAH metabolism in human body, nor to study PAH carcinogenesis in the lung. However, the benefit of utilizing cell culture models cannot be ignored. Cell cultures continue to be applied in investigations of single metabolic pathway, cross-talking of signaling pathways, gene regulation such as promoter methylation, and cell biology in PAH carcinogenesis. We have recently identified the significant role of the AHRE974 of CYP1A1 5-flanking sequence in PAH induction of CYP1A1 promoter in pulmonary cell culture systems (Chu, Wang, Basu, Maturu, Couroucli, Jiang, and Moorthy, unpublished data). In fact, because more than 1 cell type is involved in the development of pulmonary carcinogenesis, new 3-dimensional models using multiple cell types would be desirable.
Knock-out mice have emerged as important tools to investigate the role of a particular gene in PAH activation or carcinogenesis (Chavan and Krishnamurthy, 2012; Dragin et al., 2008; Jiang et al., 2009, 2010; Kondraganti et al., 2003; Shimada et al., 2002). For example, studies in AhR knockout mice indicate the existence of an AhR-independent pathway for PAH activation in mouse liver (Kondraganti et al., 2003), and the regulation of hepatic and pulmonary CYP1A1 by PAHs is altered in Cyp1a2-null mice (Jiang et al., 2010). Carcinogenicities of PAHs are also lost in AhR knockout mice (Nakatsuru et al., 2004; Shimizu et al., 2000), thereby suggesting that AhR is involved in pulmonary carcinogenesis. Knock-out animal models will continue to be used to determine many of the mechanisms associated with PAH toxicity; however, 1 potential disadvantage to the use of knock-out animal models is that the various animal genes encoding the metabolic enzymes may not be similar to those in the human.
To better study the roles of CYPs in PAH toxicities to humans, humanized mice have also been developed. To produce these animals, the endogenous rodent genes are replaced with their human homologues or equivalents (Dragin et al., 2007; Gonzalez, 2007; Kazuki et al., 2012; Moriguchi et al., 2003). Corchero et al. (2001) used a BAC clone containing both CYP1A1 and 1A2 genes to generate a transgenic mouse line that was bred into either Cyp1a1-null or Cyp1a2-null background, thereby creating functional humanized CYP1A1 (Cheung et al., 2005) and humanized 1A2 mice (Jiang et al., 2005), respectively. The humanized CYP1A2 mice has shown preferential N2-hydroxylation of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine, a pathway that is predominant in human, based on in vitro studies (Cheung et al., 2005). Dragin et al. (2007) have also developed humanized mice that express both human CYP1A1 and 1A2, but lack their mouse orthologues, making these models ideal for studying human metabolism of PAHs in mice (Uno et al., 2009). Recently, Li et al. (2014) reported the establishment of a humanized CYP1B1 mouse line. The use of humanized mouse models will be essential in the future elucidation of the health effects of PAHs in humans, provide a link between the in vitro and human studies, and assist in addressing many of the data gaps listed in this review.
GENETIC SUSCEPTIBILITY TO PAH-ASSOCIATED LUNG CANCERS
Less than one-fourth of tobacco smokers are diagnosed with lung cancer (Ezzati and Lopez, 2004), and yet, ∼1 out of 10 of lung cancer deaths is among non-smokers (Alberg et al., 2013), indicating that many genes and gene families affect the activation and elimination of PAHs and genetic susceptibility plays a role in lung cancer. Mutations, including single nucleotide polymorphisms (SNPs), of these genes alter their biological functions such as catalytic activities, hence, affect the toxicity of PAHs and have implications for studying the mechanisms of PAHs by adding to their complex mechanism(s) of action. These mutations have been demonstrated in CYPs, GSTs, and p53. For example, polymorphisms of CYP1A1, GSTM1, and GSTT1 affect the susceptibility of lung cancer induced by PAH exposure (Bennett et al., 1999; Ji et al., 2012; Ketterer et al., 1992; Przygodzki et al., 1998).
The discovery of SNPs associated with PAHs and lung cancer susceptibility has also increased due to the fast development of highly efficient and economic gene sequencing technologies. These genes include GSTP1, AKR, microsomal epoxide hydrolase (EPHX1), X-ray repair cross-complementing protein 1, and excision repair cross-complementing protein EERC2 (Ada et al., 2012; Lan et al., 2004; Penning and Drury, 2007; Sun et al., 2010; Timofeeva et al., 2010; Wang et al., 2013; Zhou et al., 2011).
Moreover, a mutation that increases the susceptibility of any human disease should be critically evaluated. Such studies should consider sample size, gender, age, ethnicity, smoking habit, occupational and environmental PAH exposure, and subcategories of lung cancers. For example, Ada et al. (2012) surveyed 213 lung cancer patients and 231 controls in a Turkish population and found that GSTP1 exon 6 variant genotypes exhibited an overall increase in lung cancer risk. However, GSTM1-null, GSTT1-null, and GSTP1 exon 5 variant genotypes were not associated with a significant risk for developing lung cancer. Similar observations were also reported in a study of Caucasians (Timofeeva et al., 2010). Timofeeva et al. (2010) surveyed 17 SNPs and 2 deletion polymorphisms in 638 patients and 1300 controls under the age of 51. They found that the mutations in myeloperoxidase, EPHX1, GSTT1, GSTM1, GSTP1, and NQO1 genes showed no significant overall increase in lung cancer risk. Subgroup analysis revealed gender- and/or smoking-specific effects of EPHX1, GSTT1 deletion, GSTP1, and NQO1 polymorphisms.
Current research also suggests that multiple mutation sites in multiple genes are involved in the PAH-associated lung cancer susceptibilities. A genome-wide association study, which is based on genotyping arrays (Carvalho et al., 2013; Lange et al., 2014), has also found several SNPs that are associated with lung cancer incidences, in different nations and ethnic groups (Dong et al., 2012; Lee et al., 2013; Spitz et al., 2013). Cross-sectional investigation with PAH-induced genetic damage in 1557 Chinese coke oven workers has identified that 13q12.12-rs753955C is associated with elevated urinary 8-hydroxydeoxyguanosine level (Dai et al., 2014), a biomarker of oxidative DNA damage. Future studies of these multiple mutation sites will require increased sample size along with novel genetic analyses from next-generation sequencing to determine the various genetic susceptibilities which contribute to cancer as a result of exposure to PAHs.
IMPLICATIONS FOR HUMAN HEALTH
There is great variability among different PAHs with respect to carcinogenic potency and their dose-response relationships (Deutsch-Wenzel et al., 1983; Grimmer et al., 1988). Moreover, in reality, the environmental PAHs often exist as mixtures. Tarantini et al. (2011) reported that the components in PAH mixtures can affect the carcinogenicity of each PAH, by exhibiting synergistic and antagonistic effects, often simultaneously. This finding complicates the evaluation of cancer risk for PAHs. Recently Cioroiu et al. (2013) assessed PAHs in the lungs of 31 patients with lung cancer in Romania. Fifteen PAHs were detected, of which benz[a]anthracene, anthracene, fluoranthene, BaP, benzo[b]fluoranthrene, benzo[k]fluoranthrene were considered the major components of the mixture (Fig. 2). This study is the first to record PAH concentrations in human lung cancer tissue, and indicates that lung cancer patients present high concentrations of carcinogenic (0.33–31.94 ng/g wet tissue, mean = 6.12 ±7.31 ng/g wet tissue) and noncarcinogenic (2.46–218.19 ng/g wet tissue, mean = 45.57 ± 54.83 ng/g wet tissue) PAHs in lung tissue, thereby providing strong evidence that PAHs are etiologic factors in lung cancer in humans. Further mechanistic studies of the relevant components of these mixtures, as well as the mixtures themselves, are needed to determine which component(s) (and which when combined), play a role in the etiology of lung cancer.
In conjunction with studying mixtures, quantitative cancer risk estimates of PAHs are highly uncertain because of the lack of good-quality data. According to the World Health Organization Air Quality Guidelines for Europe, the unit risk is 9 × 10−5 per ng/m3 of BaP as an indicator of the total PAH content, namely, lifetime exposure to 0.1 ng/m3 would theoretically lead to 1 extra cancer case in 100 000 exposed individuals. This concentration of 0.1 ng/m3 of BaP is suggested as a health-based guideline. Because the carcinogenic potency of fluoranthene has been estimated to be ∼20 times less than that of BaP, a tentative guideline value of 2 ng/m3 is suggested for fluoranthene. Guidelines still need to be determined for other significant PAHs such as phenanthrene, methylated phenanthrenes/anthracenes and pyrene, and large-molecule PAHs such as dibenz[a,h]anthracene, benzo[b]fluoranthene, benzo[k]fluoranthene, and indeno[1,2,3-cd]pyrene. Thus, it is only through careful mechanistic studies that recommendations can be provided in support of these guidelines.
KNOWLEDGE GAPS IN MECHANISTIC RESEARCH OF PAHs
Although there is a great amount of literature on PAHs, there are still several knowledge gaps that need to be fulfilled in order to fully understand the complex nature of these compounds, and the gaps increase exponentially when considering that PAHs often exists in mixtures. For example, most mechanistic studies have been conducted using BaP, suggesting there is need for investigations with other human carcinogenic PAHs and mixtures of these PAHs. Most work has focused on parent PAHs, but alkylated and oxygenated PAHs are also present in the environment. Also, more structure-activity relationship work is needed to predict which PAHs might be lung carcinogens. Other areas of needed research include: AhR versus AhR-independent pathways of PAH-induced carcinogenesis; identification of susceptible individuals and the mechanisms that play a role in susceptibility; immune-related mechanisms of PAH-mediated lung cancer; and the role of epigenetics in PAH-induced lung cancer. For example, Pavanello et al. (2010) recently showed that shorter telomere length in peripheral blood lymphocytes of workers exposed to PAHs is predictive of lung cancer risk. Finally, treatments to prevent or reverse the mechanisms that induce carcinogenesis induced by PAHs are necessary to reduce the incidence of lung cancer.
CONCLUSIONS
In conclusion, this review focuses on the mechanisms of toxicity of PAHs, in relation to pulmonary carcinogenesis in humans. To tease the mechanistic effects of multiple PAHs will require an inter-disciplinary approach with systems biologists, epidemiologists, pathologists, omics researchers, mechanistic researchers, and biostatisticians who can analyze complex data sets. PAHs are a complex mixture, often with over 100 components, making these compounds difficult to study. The most well-known PAH, BaP, is just the beginning of our understanding of the components of these mixtures. Further research is needed on how individual or binary and higher order mixtures of PAHs induce genetic and molecular alterations. To add to the complexity, these mixtures should be investigated in susceptible populations such as those with genetic polymorphisms as well as in sensitive populations such as children. This research will lead to novel strategies for the prevention and/or treatment of human lung carcinogenesis mediated by environmental PAHs.
ACKNOWLEDGMENTS
We thank Dr Cynthia Rider (NIEHS), Dr Heather Henry (NIEHS), Dr William Suk (NIEHS), and Dr Gwen W. Collman for reviewing this manuscript.
FUNDING
National Institute of Health (grants ES-009132, HL-112516, HL-087174, and ES-019689 to B.M.).
References
- Ada A. O., Kunak S. C., Hancer F., Soydas E., Alpar S., Gulhan M., Iscan M. (2012). Association between GSTM1, GSTT1, and GSTP1 polymorphisms and lung cancer risk in a Turkish population. Mol. Biol. Rep. , 39, 5985–5993. [DOI] [PubMed] [Google Scholar]
- Agency for Toxic Substances and Disease Registry (ATSDR), (1990). Polycyclic Aromatic Hydrocarbons, December 1990, in Public Health Statement. U.S. Department of Health and Human Services U.S. Public Health Service, Atlanta, GA. [Google Scholar]
- Alberg A. J., Wallace K., Silvestri G. A., Brock M. V. (2013). Invited commentary: The etiology of lung cancer in men compared with women. Am. J. Epidemiol , 177, 613–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexandrov K., Rojas M., Satarug S. (2010). The critical DNA damage by benzo(a)pyrene in lung tissues of smokers and approaches to preventing its formation. Toxicol. Lett. , 198, 63–68. [DOI] [PubMed] [Google Scholar]
- Arlt V. M., Poirier M. C., Sykes S. E., John K., Moserova M., Stiborova M., Wolf C. R., Henderson C. J., Phillips D. H. (2012). Exposure to benzo[a]pyrene of hepatic cytochrome P450 reductase null (HRN) and P450 reductase conditional null (RCN) mice: detection of benzo[a]pyrene diol epoxide-DNA adducts by immunohistochemistry and 32P-postlabelling. Toxicol. Lett. , 213, 160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett W. P., Alavanja M. C., Blomeke B., Vahakangas K. H., Castren K., Welsh J. A., Bowman E. D., Khan M. A., Flieder D. B., Harris C. C. (1999). Environmental tobacco smoke, genetic susceptibility, and risk of lung cancer in never-smoking women. J. Natl Cancer Inst. , 91, 2009–2014. [DOI] [PubMed] [Google Scholar]
- Beresford A. P. (1993). CYP1A1: friend or foe? Drug Metab. Rev. , 25, 503–517. [DOI] [PubMed] [Google Scholar]
- Berge G., Mollerup S., S O. V., Hewer A., Phillips D. H., Eilertsen E., Haugen A. (2004). Role of estrogen receptor in regulation of polycyclic aromatic hydrocarbon metabolic activation in lung. Lung Cancer , 45, 289–297. [DOI] [PubMed] [Google Scholar]
- Borza A., Plottner S., Wolf A., Behm C., Selinski S., Hengstler J. G., Roos P. H., Bolt H. M., Kuhlmann J., Follmann W. (2008). Synergism of aromatic amines and benzo[a]pyrene in induction of Ah receptor-dependent genes. Arch. Toxicol. , 82, 973–980. [DOI] [PubMed] [Google Scholar]
- Bostrom C. E., Gerde P., Hanberg A., Jernstrom B., Johansson C., Kyrklund T., Rannug A., Tornqvist M., Victorin K., Westerholm R. (2002). Cancer risk assessment, indicators, and guidelines for polycyclic aromatic hydrocarbons in the ambient air. Environ. Health Perspect. , 110(Suppl. 3), 451–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowes R. C., 3rd, Parrish A. R., Steinberg M. A., Willett K. L., Zhao W., Savas U., Jefcoate C. R., Safe S. H., Ramos K. S. (1996). Atypical cytochrome P450 induction profiles in glomerular mesangial cells at the mRNA and enzyme level. Evidence for CYP1A1 and CYP1B1 expression and their involvement in benzo[a]pyrene metabolism. Biochem. Pharmacol. , 52, 587–595. [DOI] [PubMed] [Google Scholar]
- Burczynski M. E., Lin H. K., Penning T. M. (1999). Isoform-specific induction of a human aldo-keto reductase by polycyclic aromatic hydrocarbons (PAHs), electrophiles, and oxidative stress: implications for the alternative pathway of PAH activation catalyzed by human dihydrodiol dehydrogenase. Cancer Res. , 59, 607–614. [PubMed] [Google Scholar]
- Cai Y., Lv J., Zhang W., Zhang L. (2012), ‘Dietary exposure estimates of 16 polycyclic aromatic hydrocarbons (PAHs) in Xuanwei and Fuyuan, counties in a high lung cancer incidence area in China. J. Environ. Monit. , 14, 886–892. [DOI] [PubMed] [Google Scholar]
- Carvalho R. H., Hou J., Haberle V., Aerts J., Grosveld F., Lenhard B., Philipsen S. (2013). Genomewide DNA methylation analysis identifies novel methylated genes in non-small-cell lung carcinomas. J. Thorac. Oncol. , 8, 562–573. [DOI] [PubMed] [Google Scholar]
- Cavalieri E., Rogan E. (1985). Role of radical cations in aromatic hydrocarbon carcinogenesis. Environ. Health Perspect. , 64, 69–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavan H., Krishnamurthy P. (2012). Polycyclic aromatic hydrocarbons (PAHs) mediate transcriptional activation of the ATP binding cassette transporter ABCB6 gene via the aryl hydrocarbon receptor (AhR). J. Biol. Chem. , 287, 32054–32068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P. H., Chang J. T., Li L. A., Tsai H. T., Shen M. Y., Lin P. (2013). Aryl hydrocarbon receptor is a target of 17-Allylamino-17-demethoxygeldanamycin and enhances its anticancer activity in lung adenocarcinoma cells. Mol. Pharmacol. , 83, 605–612. [DOI] [PubMed] [Google Scholar]
- Cheung C., Ma X., Krausz K. W., Kimura S., Feigenbaum L., Dalton T. P., Nebert D. W., Idle J. R., Gonzalez F. J. (2005). Differential metabolism of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in mice humanized for CYP1A1 and CYP1A2. Chem. Res. Toxicol. , 18, 1471–1478. [DOI] [PubMed] [Google Scholar]
- Chiba T., Uchi H., Tsuji G., Gondo H., Moroi Y., Furue M. (2011). Arylhydrocarbon receptor (AhR) activation in airway epithelial cells induces MUC5AC via reactive oxygen species (ROS) production. Pulm. Pharmacol. Ther. , 24, 133–140. [DOI] [PubMed] [Google Scholar]
- Choudhary D., Jansson I., Schenkman J. B., Sarfarazi M., Stoilov I. (2003). Comparative expression profiling of 40 mouse cytochrome P450 genes in embryonic and adult tissues. Arch. Biochem. Biophys. , 414, 91–100. [DOI] [PubMed] [Google Scholar]
- Cioroiu B. I., Tarcau D., Cucu-Man S., Chisalita I., Cioroiu M. (2013). Polycyclic aromatic hydrocarbons in lung tissue of patients with pulmonary cancer from Romania. Influence according as demographic status and ABO phenotypes. Chemosphere , 92, 504–511. [DOI] [PubMed] [Google Scholar]
- Conney A. H. (1982). Induction of microsomal enzymes by foreign chemicals and carcinogenesis by polycyclic aromatic hydrocarbons: G. H. A. Clowes Memorial Lecture. Cancer Res. , 42, 4875–4917. [PubMed] [Google Scholar]
- Corchero J., Pimprale S., Kimura S., Gonzalez F. J. (2001). Organization of the CYP1A cluster on human chromosome 15: implications for gene regulation. Pharmacogenetics , 11, 1–6. [DOI] [PubMed] [Google Scholar]
- Dai X., Deng S., Wang T., Qiu G., Li J., Yang B., Feng W., He X., Deng Q., Ye J., et al. (2014). Associations between 25 lung cancer risk-related SNPs and polycyclic aromatic hydrocarbon-induced genetic damage in coke oven workers. Cancer Epidemiol. Biomarkers Prev. , 23, 986–996. [DOI] [PubMed] [Google Scholar]
- DeMarini D. M. (2004). Genotoxicity of tobacco smoke and tobacco smoke condensate: a review. Mutat. Res. , 567, 447–474. [DOI] [PubMed] [Google Scholar]
- Denissenko M. F., Pao A., Tang M., Pfeifer G. P. (1996). Preferential formation of benzo[a]pyrene adducts at lung cancer mutational hotspots in P53. Science, 274, 430–432. [DOI] [PubMed] [Google Scholar]
- Deutsch-Wenzel R. P., Brune H., Grimmer G., Dettbarn G., Misfeld J. (1983). Experimental studies in rat lungs on the carcinogenicity and dose-response relationships of eight frequently occurring environmental polycyclic aromatic hydrocarbons. J. Natl Cancer Inst. , 71, 539–544. [PubMed] [Google Scholar]
- Devanesan P. D., Pao A., Tang M., Pfeifer G. P. (1992). Identification and quantitation of benzo[a]pyrene-DNA adducts formed by rat liver microsomes in vitro. Chem. Res. Toxicol. , 5, 302–309. [DOI] [PubMed] [Google Scholar]
- Dey A., Jones J. E., Nebert D. W. (1999). Tissue- and cell type-specific expression of cytochrome P450 1A1 and cytochrome P450 1A2 mRNA in the mouse localized in situ hybridization. Biochem. Pharmacol. , 58, 525–537. [DOI] [PubMed] [Google Scholar]
- Dong J., Hu Z., Wu C., Guo H., Zhou B., Lv J., Lu D., Chen K., Shi Y., Chu M., et al. (2012). Association analyses identify multiple new lung cancer susceptibility loci and their interactions with smoking in the Chinese population. Nat. Genet. , 44, 895–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragin N., Uno S., Wang B., Dalton T. P., Nebert D. W. (2007). Generation of ‘humanized’ hCYP1A1_1A2_Cyp1a1/1a2(-/-) mouse line. Biochem. Biophys. Res. Commun. , 359, 635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragin N., Shi Z., Madan R., Karp C. L., Sartor M. A., Chen C., Gonzalez F. J., Nebert D. W. (2008). Phenotype of the Cyp1a1/1a2/1b1-/- triple-knockout mouse. Mol. Pharmacol. , 73, 1844–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eom S. Y., Yim D. H., Moon S. I., Youn J. W., Kwon H. J., Oh H. C., Yang J. J., Park S. K., Yoo K. Y., Kim H. S., et al. (2013). Polycyclic aromatic hydrocarbon-induced oxidative stress, antioxidant capacity, and the risk of lung cancer: a pilot nested case-control study. Anticancer Res. , 33, 3089–3097. [PubMed] [Google Scholar]
- Ezzati M., Lopez A. D. (2004). Regional, disease specific patterns of smoking-attributable mortality in 2000. Tob. Control , 13, 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazili I. S., Jiang W., Wang L., Felix E. A., Khatlani T., Coumoul X., Barouki R., Moorthy B. (2010). Persistent induction of cytochrome P4501A1 in human hepatoma cells by 3-methylcholanthrene: evidence for sustained transcriptional activation of the CYP1A1 promoter. J. Pharmacol. Exp. Ther. , 333, 99–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geacintov N. E., Cosman M., Hingerty B. E., Amin S., Broyde S., Patel D. J. (1997). NMR solution structures of stereoisometric covalent polycyclic aromatic carcinogen-DNA adduct: principles, patterns, and diversity. Chem. Res. Toxicol. , 10, 111–146. [DOI] [PubMed] [Google Scholar]
- Gonzalez F. J. (2007). CYP3A4 and pregnane X receptor humanized mice. J. Biochem. Mol. Toxicol. , 21, 158–162. [DOI] [PubMed] [Google Scholar]
- Grimmer G., Brune H., Dettbarn G., Naujack K. W., Mohr U., Wenzel-Hartung R. (1988). Contribution of polycyclic aromatic compounds to the carcinogenicity of sidestream smoke of cigarettes evaluated by implantation into the lungs of rats. Cancer Lett. , 43, 173–177. [DOI] [PubMed] [Google Scholar]
- Guengerich F. P. (2008). Cytochrome p450 and chemical toxicology. Chem. Res. Toxicol. , 21, 70–83. [DOI] [PubMed] [Google Scholar]
- Hansen A. M., Olsen I. L., Poulsen O. M. (1992). Polycyclic aromatic hydrocarbons in air samples of meat smokehouses. Sci. Total Environ. , 126, 17–26. [DOI] [PubMed] [Google Scholar]
- Hecht S. S. (2002). Cigarette smoking and lung cancer: chemical mechanisms and approaches to prevention. Lancet Oncol. , 3, 461–469. [DOI] [PubMed] [Google Scholar]
- Hecht S. S. (2011). More than 500 trillion molecules of strong carcinogens per cigarette: use in product labelling? Tob. Control , 20, 387. [DOI] [PubMed] [Google Scholar]
- Horn L., Pao W., Johnson D. H. (2012). Harrison’s Principles of Internal Medicine. Neoplasms of the Lung, 18th ed McGraw-Hill New York. [Google Scholar]
- Hrycay E. G., Bandiera S. M. (2012). The monooxygenase, peroxidase, and peroxygenase properties of cytochrome P450. Arch. Biochem. Biophys. , 522, 71–89. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC) (2010). Some non-heterocyclic polycyclic aromatic hydrocarbons and some related exposures. IARC Monographs 92; Lyon, France. [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC) (2012). Globocan 2012: estimated cancer incidence, mortality and prevalence worldwide in 2012, World Health Organization, Lyon, France. [Google Scholar]
- Jarup L. (2003). Hazards of heavy metal contamination. Br. Med. Bullet. , 68, 167–182. [DOI] [PubMed] [Google Scholar]
- Ji Y. N., Wang Q., Suo L. J. (2012). CYP1A1 Ile462Val polymorphism contributes to lung cancer susceptibility among lung squamous carcinoma and smokers: a meta-analysis. PLoS ONE , 7, e43397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W., Welty S. E., Couroucli X. I., Barrios R., Kondraganti S. R., Muthiah K., Yu L., Avery S. E., Moorthy B. (2004). Disruption of the Ah receptor gene alters the susceptibility of mice to oxygen-mediated regulation of pulmonary and hepatic cytochromes P4501A expression and exacerbates hyperoxic lung injury. J. Pharmacol. Exp. Ther. , 310, 512–519. [DOI] [PubMed] [Google Scholar]
- Jiang W., Wang L., Zhang W., Coffee R., Fazili I. S., Moorthy B. (2009). Persistent induction of cytochrome P450 (CYP)1A enzymes by 3-methylcholanthrene in vivo in mice is mediated by sustained transcriptional activation of the corresponding promoters. Biochem. Biophys. Res. Commun. , 390, 1419–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W., Wang L., Kondraganti S. R., Fazili I. S., Couroucli X. I., Felix E. A., Moorthy B. (2010). Disruption of the gene for CYP1A2, which is expressed primarily in liver, leads to differential regulation of hepatic and pulmonary mouse CYP1A1 expression and augmented human CYP1A1 transcriptional activation in response to 3-methylcholanthrene in vivo. J. Pharmacol. Exp. Ther. , 335, 369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Z., Dalton T. P., Jin L., Wang B., Tsuneoka Y., Shertzer H. G., Deka R., Nebert D. W. (2005). Toward the evaluation of function in genetic variability: characterizing human SNP frequencies and establishing BAC-transgenic mice carrying the human CYP1A1_CYP1A2 locus. Hum. Mutat. , 25, 196–206. [DOI] [PubMed] [Google Scholar]
- Joubert B. R., Haberg S. E., Nilsen R. M., Wang X., Vollset S. E., Murphy S. K., Huang Z., Hoyo C., Midttun O., Cupul-Uicab L. A., et al. (2012). 450K epigenome-wide scan identifies differential DNA methylation in newborns related to maternal smoking during pregnancy. Environ. Health Perspect. , 120, 1425–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kafferlein H. U., Marczynski B., Mensing T., Bruning T. (2010). Albumin and hemoglobin adducts of benzo[a]pyrene in humans—analytical methods, exposure assessment, and recommendations for future directions. Crit. Rev. Toxicol. , 40, 126–150. [DOI] [PubMed] [Google Scholar]
- Kazuki Y., Kobayashi K., Aueviriyavit S., Oshima T., Kuroiwa Y., Tsukazaki Y., Senda N., Kawakami H., Ohtsuki S., Abe S., et al. (2012). Trans-chromosomic mice containing a human CYP3A cluster for prediction of xenobiotic metabolism in humans. Hum. Mol. Genet , 22, 578–592. [DOI] [PubMed] [Google Scholar]
- Ketterer B., Harris J. M., Talaska G., Meyer D. J., Pemble S. E., Taylor J. B., Lang N. P., Kadlubar F. F. (1992). The human glutathione S-transferase supergene family, its polymorphism, and its effects on susceptibility to lung cancer. Environ. Health Perspect. , 98, 87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondraganti S. R., Fernandez-Salguero P., Gonzalez F. J., Ramos K. S., Jiang W., Moorthy B. (2003). Polycyclic aromatic hydrocarbon-inducible DNA adducts: evidence by 32P-postlabeling and use of knockout mice for Ah receptor-independent mechanisms of metabolic activation in vivo. Int. J. Cancer , 103, 5–11. [DOI] [PubMed] [Google Scholar]
- Kwack S. J., Lee B. M. (2000). Correlation between DNA or protein adducts and benzo[a]pyrene diol epoxide I-triglyceride adduct detected in vitro and in vivo. Carcinogenesis , 21, 629–632. [DOI] [PubMed] [Google Scholar]
- Lan Q., Mumford J. L., Shen M., Demarini D. M., Bonner M. R., He X., Yeager M., Welch R., Chanock S., Tian L., et al. (2004). Oxidative damage-related genes AKR1C3 and OGG1 modulate risks for lung cancer due to exposure to PAH-rich coal combustion emissions. Carcinogenesis , 25, 2177–2181. [DOI] [PubMed] [Google Scholar]
- Lange L. A., Hu Y., Zhang H., Xue C., Schmidt E. M., Tang Z. Z., Bizon C., Lange E. M., Smith J. D., Turner E. H., et al. (2014). Whole-exome sequencing identifies rare and low-frequency coding variants associated with LDL cholesterol. Am. J. Hum. Genet. , 94, 233–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsson B. K., Sahlberg G. P., Eriksson A. T., Busk L. A. (1983). Polycyclic aromatic hydrocarbons in grilled food. J. Agric. Food Chem. , 31, 867–873. [DOI] [PubMed] [Google Scholar]
- Lee D., Lee G. K., Yoon K. A., Lee J. S. (2013). Pathway-based analysis using genome-wide association data from a Korean non-small cell lung cancer study. PLoS ONE , 8, e65396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F., Jiang C., Larsen M. C., Bushkofsky J., Krausz K. W., Wang T., Jefcoate C. R., Gonzalez F. J. (2014). Lipidomics reveals a link between CYP1B1 and SCD1 in promoting obesity. J. Proteome Res. , 13, 2679–2687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liehr J. G., Ricci M. J., Jefcoate C. R., Hannigan E. V., Hokanson J. A., Zhu B. T. (1995). 4-Hydroxylation of estradiol by human uterine myometrium and myoma microsomes: implications for the mechanism of uterine tumorigenesis. Proc. Natl Acad. Sci. U S A , 92, 9220–9224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Vinje J., Pacifico C., Natile G., Sletten E. (2002). Formation of adenine-N3/guanine-N7 cross-link in the reaction of trans-oriented platinum substrates with dinucleotides. J. Am. Chem. Soc. , 124, 12854–12862. [DOI] [PubMed] [Google Scholar]
- Marlowe J. L., Puga A. (2005). Aryl hydrocarbon receptor, cell cycle regulation, toxicity, and tumorigenesis. J. Cell Biochem. , 96, 1174–1184. [DOI] [PubMed] [Google Scholar]
- Masuda Y., Mori K., Kuratsune M. (1966). Polycyclic aromatic hydrocarbons in common Japanese foods. I. Broiled fish, roasted barley, shoyu, and caramel. Gann , 57, 133–142. [PubMed] [Google Scholar]
- Matsumoto Y., Ide F., Kishi R., Akutagawa T., Sakai S., Nakamura M., Ishikawa T., Fujii-Kuriyama Y., Nakatsuru Y. (2007). Aryl hydrocarbon receptor plays a significant role in mediating airborne particulate-induced carcinogenesis in mice. Environ. Sci. Technol. , 41, 3775–3780. [DOI] [PubMed] [Google Scholar]
- Miller K. P., Ramos K. S. (2001). Impact of cellular metabolism on the biological effects of benzo[a]pyrene and related hydrocarbons. Drug Metab. Rev. , 33, 1–35. [DOI] [PubMed] [Google Scholar]
- Moorthy B., Chen S., Li D., Randerath K. (1993). 3-Methylcholanthrene-inducible liver cytochrome(s) P450 in female Sprague–Dawley rats: possible link between P450 turnover and formation of DNA adducts and I-compounds. Carcinogenesis , 14, 879–886. [DOI] [PubMed] [Google Scholar]
- Moorthy B. (2000). Persistent expression of 3-methylcholanthrene-inducible cytochromes P4501A in rat hepatic and extrahepatic tissues. J. Pharmacol. Exp. Ther. , 294, 313–322. [PubMed] [Google Scholar]
- Moorthy B., Miller K. P., Jiang W., Ramos K. S. (2002). The atherogen 3-methylcholanthrene induces multiple DNA adducts in mouse aortic smooth muscle cells: role of cytochrome P4501B1. Cardiovasc. Res. , 53, 1002–1009. [DOI] [PubMed] [Google Scholar]
- Moorthy B. (2008). The CYP1A subfamily. In Cytochromes P450: Role in the Drug Metabolism and Toxicity of Drugs and other Xenobiotics (Ioannides C., Ed.), pp. 97–135. RSC Publishing, Cambridge, UK. [Google Scholar]
- Moriguchi T., Motohashi H., Hosoya T., Nakajima O., Takahashi S., Ohsako S., Aoki Y., Nishimura N., Tohyama C., Fujii-Kuriyama Y., et al. (2003). Distinct response to dioxin in an arylhydrocarbon receptor (AHR)-humanized mouse. Proc. Natl Acad. Sci. U S A , 100, 5652–5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottier P., Parisod V., Turesky R. J. (2000). Quantitative determination of polycyclic aromatic hydrocarbons in barbecued meat sausages by gas chromatography coupled to mass spectrometry. J. Agric. Food Chem. , 48, 1160–1166. [DOI] [PubMed] [Google Scholar]
- Murray G. I., Taylor M. C., McFadyen M. C., McKay J. A., Greenlee W. F., Burke M. D., Melvin W. T. (1997). Tumor-specific expression of cytochrome P450 CYP1B1. Cancer Res. , 57, 3026–3031. [PubMed] [Google Scholar]
- Nakatsuru Y., Wakabayashi K., Fujii-Kuriyama Y., Ishikawa T., Kusama K., Ide F. (2004). Dibenzo[A,L]pyrene-induced genotoxic and carcinogenic responses are dramatically suppressed in aryl hydrocarbon receptor-deficient mice. Int. J. Cancer , 112, 179–183. [DOI] [PubMed] [Google Scholar]
- Nebert D. W., Dalton T. P., Okey A. B., Gonzalez F. J. (2004). Role of aryl hydrocarbon receptor-mediated induction of the CYP1 enzymes in environmental toxicity and cancer. J. Biol. Chem. , 279, 23847–23850. [DOI] [PubMed] [Google Scholar]
- Nebert D. W., Shi Z., Galvez-Peralta M., Uno S., Dragin N. (2013). Oral benzo[a]pyrene: understanding pharmacokinetics, detoxication and consequences—Cyp1 knockout mouse lines as a paradigm. Mol. Pharmacol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osgood R. S., Upham B. L., Hill T., 3rd, Helms K. L., Velmurugan K., Babica P., Bauer A. K. (2013). Polycyclic aromatic hydrocarbon-induced signaling events relevant to inflammation and tumorigenesis in lung cells are dependent on molecular structure. PLoS ONE , 8, e65150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavanello S., Pesatori A. C., Dioni L., Hoxha M., Bollati V., Siwinska E., Mielzynska D., Bolognesi C., Bertazzi P. A., Baccarelli A. (2010). Shorter telomere length in peripheral blood lymphocytes of workers exposed to polycyclic aromatic hydrocarbons. Carcinogenesis , 31, 216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penning T. M., Drury J. E. (2007). Human aldo-keto reductases: function, gene regulation, and single nucleotide polymorphisms. Arch. Biochem. Biophys. , 464, 241–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeifer G. P., Besaratinia A. (2009). Mutational spectra of human cancer. Hum. Genet. , 125, 493–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccardo M. T., Stella A., Valerio F. (2010). Is the smokers exposure to environmental tobacco smoke negligible? Environ . Health , 9, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Przygodzki R. M., Bennett W. P., Guinee D. G., Jr., Khan M. A., Freedman A., Shields P. G., Travis W. D., Jett J. R., Tazelaar H., Pairolero P., et al. (1998). p53 mutation spectrum in relation to GSTM1, CYP1A1 and CYP2E1 in surgically treated patients with non-small cell lung cancer. Pharmacogenetics , 8, 503–511. [DOI] [PubMed] [Google Scholar]
- Pupin A. M., Toledo M. C. (1996). Benzo(a)pyrene in Brazilian vegetable oils. Food Addit. Contam. , 13, 639–645. [DOI] [PubMed] [Google Scholar]
- Ramadoss P., Marcus C., Perdew G. H. (2005). Role of the aryl hydrocarbon receptor in drug metabolism. Expert Opin. Drug Metab. Toxicol. , 1, 9–21. [DOI] [PubMed] [Google Scholar]
- Ramos K. S., Moorthy B. (2005). Bioactivation of polycyclic aromatic hydrocarbon carcinogens within the vascular wall: implications for human atherogenesis. Drug Metab. Rev. , 37, 595–610. [DOI] [PubMed] [Google Scholar]
- Reid B. C., Ghazarian A. A., DeMarini D. M., Sapkota A., Jack D., Lan Q., Winn D. M., Birnbaum L. S. (2012). Research opportunities for cancer associated with indoor air pollution from solid-fuel combustion. Environ. Health Perspect. , 120, 1495–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas M., Alexandrov K., Cascorbi I., Brockmoller J., Likhachev A., Pozharisski K., Bouvier G., Auburtin G., Mayer L., Kopp-Schneider A., et al. (1998). High benzo[a]pyrene diol-epoxide DNA adduct levels in lung and blood cells from individuals with combined CYP1A1 MspI/Msp-GSTM1*0/*0 genotypes. Pharmacogenetics , 8, 109–118. [PubMed] [Google Scholar]
- Rozman K. K., Klaassen C. D. (2007). Absorption, distribution and excretion of toxicants. In Casarett and Doull´s Toxicology: The Basic Science of Poisons (Klaassen C. D., Ed.), pp. 107–132. McGraw-Hill, New York. [Google Scholar]
- Rubin H. (2001). Synergistic mechanisms in carcinogenesis by polycyclic aromatic hydrocarbons and by tobacco smoke: a bio-historical perspective with updates. Carcinogenesis , 22, 1903–1930. [DOI] [PubMed] [Google Scholar]
- Rybicki B. A., Nock N. L., Savera A. T., Tang D., Rundle A. (2006). Polycyclic aromatic hydrocarbon-DNA adduct formation in prostate carcinogenesis. Cancer Lett. , 239, 157–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saengtienchai A., Ikenaka Y., Nakayama S. M., Mizukawa H., Kakehi M., Bortey-Sam N., Darwish W. S., Tsubota T., Terasaki M., Poapolathep A., et al. (2014). Identification of interspecific differences in phase II reactions: determination of metabolites in the urine of 16 mammalian species exposed to environmental pyrene. Environ. Toxicol. Chem. , 33, 2062–2069. [DOI] [PubMed] [Google Scholar]
- Shimada T., Hayes C. L., Yamazaki H., Amin S., Hecht S. S., Guengerich F. P., Sutter T. R. (1996). Activation of chemically diverse procarcinogens by human cytochrome P-450 1B1. Cancer Res. , 56, 2979–2984. [PubMed] [Google Scholar]
- Shimada T., Gillam E. M., Oda Y., Tsumura F., Sutter T. R., Guengerich F. P., Inoue K. (1999). Metabolism of benzo[a]pyrene to trans-7,8-dihydroxy-7, 8-dihydrobenzo[a]pyrene by recombinant human cytochrome P450 1B1 and purified liver epoxide hydrolase. Chem. Res. Toxicol. , 12, 623–629. [DOI] [PubMed] [Google Scholar]
- Shimada T., Oda Y., Gillam E. M., Guengerich F. P., Inoue K. (2001). Metabolic activation of polycyclic aromatic hydrocarbons and other procarcinogens by cytochromes P450 1A1 and P450 1B1 allelic variants and other human cytochromes P450 in Salmonella typhimurium NM2009. Drug Metab. Dispos. , 29, 1176–1182. [PubMed] [Google Scholar]
- Shimada T., Inoue K., Suzuki Y., Kawai T., Azuma E., Nakajima T., Shindo M., Kurose K., Sugie A., Yamagishi Y., et al. (2002). Arylhydrocarbon receptor-dependent induction of liver and lung cytochromes P450 1A1, 1A2, and 1B1 by polycyclic aromatic hydrocarbons and polychlorinated biphenyls in genetically engineered C57BL/6J mice. Carcinogenesis , 23, 1199–1207. [DOI] [PubMed] [Google Scholar]
- Shimada T., Tanaka K., Takenaka S., Murayama N., Martin M. V., Foroozesh M. K., Yamazaki H., Guengerich F. P., Komori M. (2010). Structure–function relationships of inhibition of human cytochromes P450 1A1, 1A2, 1B1, 2C9, and 3A4 by 33 flavonoid derivatives. Chem. Res. Toxicol. , 23, 1921–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu Y., Nakatsuru Y., Ichinose M., Takahashi Y., Kume H., Mimura J., Fujii-Kuriyama Y., Ishikawa T. (2000). Benzo[a]pyrene carcinogenicity is lost in mice lacking the aryl hydrocarbon receptor. Proc. Natl Acad. Sci. U S A , 97, 779–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simko P. (2002). Determination of polycyclic aromatic hydrocarbons in smoked meat products and smoke flavouring food additives. J. Chromatogr. B , 770, 3–18. [DOI] [PubMed] [Google Scholar]
- Sinha R., Rothman N., Brown E. D., Mark S. D., Hoover R. N., Caporaso N. E., Levander O. A., Knize M. G., Lang N. P., Kadlubar F. F. (1994). Pan-fried meat containing high levels of heterocyclic aromatic amines but low levels of polycyclic aromatic hydrocarbons induces cytochrome P4501A2 activity in humans. Cancer Res. , 54, 6154–6159. [PubMed] [Google Scholar]
- Spencer D. L., Masten S. A., Lanier K. M., Yang X., Grassman J. A., Miller C. R., Sutter T. R., Lucier G. W., Walker N. J. (1999). Quantitative analysis of constitutive and 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced cytochrome P450 1B1 expression in human lymphocytes. Cancer Epidemiol. Biomarkers Prev. , 8, 139–146. [PubMed] [Google Scholar]
- Spink D. C., Spink B. C., Cao J. Q., Gierthy J. F., Hayes C. L., Li Y., Sutter T. R. (1997). Induction of cytochrome P450 1B1 and catechol estrogen metabolism in ACHN human renal adenocarcinoma cells. J. Steroid Biochem. Mol. Biol. , 62, 223–232. [DOI] [PubMed] [Google Scholar]
- Spitz M. R., Amos C. I., Land S., Wu X., Dong Q., Wenzlaff A. S., Schwartz A. G. (2013). Role of selected genetic variants in lung cancer risk in African Americans. J. Thorac. Oncol. , 8,391–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun N., Sun X., Chen B., Cheng H., Feng J., Cheng L., Lu Z. (2010). MRP2 and GSTP1 polymorphisms and chemotherapy response in advanced non-small cell lung cancer. Cancer Chemother. Pharmacol. , 65, 437–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarantini A., Maitre A., Lefebvre E., Marques M., Rajhi A., Douki T. (2011). Polycyclic aromatic hydrocarbons in binary mixtures modulate the efficiency of benzo[a]pyrene to form DNA adducts in human cells. Toxicology , 279, 36–44. [DOI] [PubMed] [Google Scholar]
- Tiefenbacher K., Pfannhauser W., Woidich H. (1982). Investigation on contamination of food by polycyclic aromatic hydrocarbons. In Recent Developments in Food Analysis: Proceedings of the First European Conference on Food Chemistry (Balees W., Czedik-Eysenberg Baltes P. B., Pfannhauser W., Eds.), pp. 76–82. Verlag Chemie, Deerfield Beach, FL. [Google Scholar]
- Timofeeva M., Kropp S., Sauter W., Beckmann L., Rosenberger A., Illig T., Jager B., Mittelstrass K., Dienemann H., Consortium L., et al. (2010). Genetic polymorphisms of MPO, GSTT1, GSTM1, GSTP1, EPHX1 and NQO1 as risk factors of early-onset lung cancer. Int. J. Cancer , 127, 1547–1561. [DOI] [PubMed] [Google Scholar]
- Tsay J. J., Tchou-Wong K. M., Greenberg A. K., Pass H., Rom W. N. (2013). Aryl hydrocarbon receptor and lung cancer. Anticancer Res. , 33, 1247–1256. [PMC free article] [PubMed] [Google Scholar]
- Uno S., Dalton T. P., Dragin N., Curran C. P., Derkenne S., Miller M. L., Shertzer H. G., Gonzalez F. J., Nebert D. W. (2006). Oral benzo[a]pyrene in Cyp1 knockout mouse lines: CYP1A1 important in detoxication, CYP1B1 metabolism required for immune damage independent of total-body burden and clearance rate. Mol. Pharmacol. , 69, 1103–1114. [DOI] [PubMed] [Google Scholar]
- Uno S., Endo K., Ishida Y., Tateno C., Makishima M., Yoshizato K., Nebert D. W. (2009). CYP1A1 and CYP1A2 expression: comparing ‘humanized’ mouse lines and wild-type mice; comparing human and mouse hepatoma-derived cell lines. Toxicol. Appl. Pharmacol. , 237, 119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uppstad H., Ovrebo S., Haugen A., Mollerup S. (2010). Importance of CYP1A1 and CYP1B1 in bioactivation of benzo[a]pyrene in human lung cell lines. Toxicol. Lett. , 192, 221–228. [DOI] [PubMed] [Google Scholar]
- Walsh A. A., Szklarz G. D., Scott E. E. (2013). Human cytochrome P450 1A1 structure and utility in understanding drug and xenobiotic metabolism. J. Biol. Chem. , 288, 12932–12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Zhu J., Zhang R., Wang S., Gu Z. (2013). Association between microsomal epoxide hydrolase 1 T113C polymorphism and susceptibility to lung cancer. Tumour Biol. [DOI] [PubMed] [Google Scholar]
- Yang P., Ma J., Zhang B., Duan H., He Z., Zeng J., Zeng X., Li D., Wang Q., Xiao Y., et al. (2012). CpG site-specific hypermethylation of p16INK4alpha in peripheral blood lymphocytes of PAH-exposed workers. Cancer Epidemiol. Biomarkers Prev. , 21, 182–190. [DOI] [PubMed] [Google Scholar]
- Zhou F., Yu Z., Jiang T., Lv H., Yao R., Liang J. (2011). Genetic polymorphisms of GSTP1 and XRCC1: prediction of clinical outcome of platinum-based chemotherapy in advanced non-small cell lung cancer (NSCLC) patients. Swiss Med. Wkly , 141, w13275. [DOI] [PubMed] [Google Scholar]