Abstract
Objectives
Acupuncture is commonly used as a complimentary treatment for pain management. However, there has been no systematic review summarizing the current evidence concerning the effectiveness of acupuncture for acute postoperative pain after back surgery. This systematic review aimed at evaluating the effectiveness of acupuncture treatment for acute postoperative pain (≤1 week) after back surgery.
Methods
We searched 15 electronic databases without language restrictions. Two reviewers independently assessed studies for eligibility and extracted data, outcomes, and risk of bias. Random effect meta-analyses and subgroup analyses were performed.
Results
Five trials, including 3 of high quality, met our inclusion criteria. The meta-analysis showed positive results for acupuncture treatment of pain after surgery in terms of the visual analogue scale (VAS) for pain intensity 24 hours after surgery, when compared to sham acupuncture (standard mean difference −0.67 (−1.04 to −0.31), P = 0.0003), whereas the other meta-analysis did not show a positive effect of acupuncture on 24-hour opiate demands when compared to sham acupuncture (standard mean difference −0.23 (−0.58 to 0.13), P = 0.21).
Conclusion
Our systematic review finds encouraging but limited evidence for the effectiveness of acupuncture treatment for acute postoperative pain after back surgery. Further rigorously designed clinical trials are required.
Keywords: acupuncture, pain, back surgery, systematic review, meta-analysis
Introduction
Rates of back surgery in the United States are the highest in the world1 and continue to rise steadily.2 Over the last few years, billions of dollars have been spent worldwide on surgery for people with chronic low back pain, and thousands of research articles have been dedicated to the subject.3 The most common reason for back surgery is the persistent low back pain caused by intervertebral disk herniation, spinal stenosis, or spondylolisthesis.4 Unfortunately, acute postoperative pain after back surgery remains a common problem. A high prevalence of moderate or severe pain on the first day following surgery as did 30% to 64% of back or spine surgery patients.5
Pain management after back surgery is a very important element of patient care. Various opioid analgesics have been used for postoperative pain management, including morphine, hydromorphine, meperidine, or fentanyl.6 However, unwanted opioid side effects, such as nausea and vomiting, are frequently observed.7 More importantly, patients with fewer side effects experience more satisfaction. Therefore, the need for safe, effective therapies for pain management after back surgery has become evident.
Acupuncture is commonly used for pain management.8,9 Numerous studies have shown that acupuncture is safe10 and cost-effective11 compared to routine care.12 The primary goal of acupuncture treatment after back surgery is pain reduction. However, there has been no systematic review summarizing the current evidence concerning the effectiveness of acupuncture for acute postoperative pain after back surgery. For this reason, we conducted a systematic review of randomized controlled trials (RCTs) to evaluate critically, whether acupuncture is effective in relieving acute postoperative pain (≤1 week) after back surgery.
Methods
Information Sources and Search Strategy
Using the COSI model,13 the following electronic databases were searched from their inception to December 2012, without restrictions on language: the Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, MEDLINE, PubMed, the Allied and Complementary Medicine Database (AMED), CINAHL, Chinese databases (including the China Knowledge Resource Integrated Database (CNKI), Wanfang Data and VIP), a Japanese database (the Japan Science and Technology Information Aggregator Electronic database), and Korean databases (including DBpia, the Korean traditional knowledge portal, NDSL, OASIS and RISS). We also manually searched gray literature.
The following key search terms were used: “(acupuncture OR acup* OR acupressure OR electroacupuncture OR auricular acupuncture OR laser acupuncture OR scalp acupuncture) AND (spinal surgery OR spine surgery OR back surgery OR lumbar surgery OR lumbar operation OR vertebra surgery OR thoracolumbar surgery OR FBSS OR “failed back surgery syndrome” OR laminectomy OR discectomy OR foraminotomy OR spinal fusion OR vertebroplasty)”. We adjusted search strategies for each of the databases. No restrictions on publication status were imposed.
Study Selection
Types of Studies
RCTs of acupuncture as a treatment option for pain after back surgery were included. Relevant dissertations and abstracts were also included. The titles and abstracts of the searched articles were read by a single primary researcher (YHC) who was trained in search and systematic review for 3 years. If the articles were not written in English, we primarily reviewed them through their English abstracts. They were translated into English prior to screening by a commercial service, if we had troubles with language comprehension. The articles that were then potentially to be included in our review were checked by 2 independent reviewers (YHC, CKK).
Types of Participants
The clinical trials involving back surgery patients were included. There were no restrictions related to the reason for the back surgery, the site of the back surgery, the type of back surgery, age, or gender. We included patients within 1 week that had passed after back surgery regarding as acute postoperative pain.
Types of Interventions/Controls
Acupuncture is defined as a collection of procedures involving penetration of the skin with needles to stimulate certain points on the body, known as acupoints following the meridian theory of traditional Chinese medicine.14,15 Other means of stimulating the acupoints, including lasers, ultrasound, and electricity, may also be used.16 Thus, our study mainly considered the effects of acupuncture with needling at acupoints or other stimulations with non-needling on acupoints (including lasers, ultrasound, electricity, and etc.). We included classical acupuncture, electro-acupuncture, acupoint electronic stimulation, acupressure, auricular acupuncture, auricular acupressure, scalp acupuncture, laser acupuncture, and abdominal acupuncture. We also included trials that compared acupuncture plus a conventional therapy (ie, regular care or routine rehabilitation) with conventional therapy alone. We excluded needling on nonacupuncture sites or acupuncture plus herbal medicine. Controls included sham/placebo acupuncture, (eg, nonpenetrating on acupoints or superficial penetrating on nonacupoints)17–19 no treatment, and conventional therapy for pain after back surgery (eg, drugs, rehabilitation, etc.).
Outcome Measures
We considered any pain-related measures, such as the visual analogue scale (VAS) and opiate demands. We also considered the general safety aspects, that is, adverse events of acupuncture as secondary outcomes.
Data Extraction and Quality Assessment
Data were independently extracted by two reviewers (YHC, BCS) and were blinded to the results of the other reviewer. The reviewers collected data related to the methodologies of the studies, the identification of outcome measurements, the results, and the final conclusions. Through the use of Cochrane's tool for assessment of risk of bias,20 each study's methodological quality was quantitatively evaluated. Cochrane's risk of bias tool consists of seven domains: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other bias. The instructions in the Cochrane handbook were followed. In this study, the 7th other risk of bias was assessed as a low risk, if baseline characteristics were properly reported and not different between treatment and control groups. Any discrepancies were resolved through discussion to reach a consensus or by consulting the third reviewer (MSL). We considered trials high quality if we assessed the risk of bias to be low in more than four of the seven domains. Therefore, this study should be interpreted as a weighted analysis of high-quality trials.
Data Synthesis
Meta-analyses were analyzed using the Cochrane Collaboration software (Review Manager [RevMan] version 5.1; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The 95% confidence interval (CI) and the standard mean difference (SMD) were calculated in the meta-analysis if the data were continuous. The 95% CI and the risk estimate (relative risk; RR) were calculated if the data were dichotomous. The variance of the change was imputed using a correlation factor of 0.4, as suggested by the Cochrane Collaboration.20 We then pooled data from across the studies using random effects models if excessive statistical heterogeneity did not exist. We assessed statistical heterogeneity using the chi-square test and the Higgins I2 test.20 If any kinds of heterogeneity exist, we conducted subgroup analysis or sensitivity analysis additionally for more comprehensive understanding of meta-analysis. Formal funnel plots were planned for assessing the publication bias, if over 10 trials were included in the same meta-analysis. However, we were not able to carry out this assessment, due to the small number of trials included in the meta-analysis.
Results
Study Description
Figure1 shows details of the trial selection process. We identified 1,515 publications. We excluded 1,464 studies after screening the abstracts and titles. Fifty-one articles were fully evaluated. We subsequently excluded 46 additional articles, 29 of which described studies that were uncontrolled and 4 of which described studies that were not randomized. Six RCTs were excluded, four21–24 of which related to anesthesia effects during surgery, one25 of which involved nonacupuncture sites, one26 of which involved acupuncture plus herbal medicine. Whereas 7 RCTs were also excluded, two27,28 of which involved chronic postoperative pain and five29–33 of which involved indistinguishable from acute/chronic postoperative pain. Those studies are summarized in Appendix 1. Consequently, 5 RCTs34–38 met our inclusion criteria. Three trials34,36,38 studied acupuncture versus sham acupuncture, 1 trials35 studied acupuncture versus conventional therapy, and 1 trial37 studied acupuncture plus conventional therapy versus conventional therapy. The key data are summarized in Table 1. There were 3 Taiwanese studies,34,37,38 1 German study,36 and 1 Chinese study.35 Three trials35–37 were 2-parallel-arm group design studies, and 2 trials34,38 were 3-parallel-arm group design studies.
Figure 1.
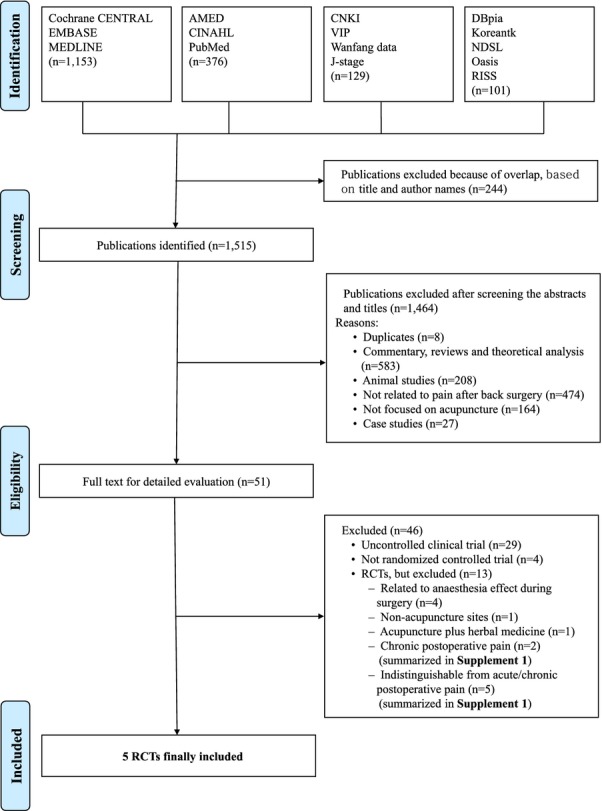
Flow chart of the trial selection process. RCT, randomized controlled trial.
Table 1.
Summary of Randomized Controlled Trials of Acupuncture for Acute Postoperative Pain after Back Surgery
| Authorref (year) Country | Reason for Surgery | Design | Sample Size (A:B:C) | Baseline Characteristics Difference of Treatment and Control Groups | AT Time before/after Surgery | Intervention | Main Outcomes | |
|---|---|---|---|---|---|---|---|---|
| Treatment | Control | |||||||
| Treatment | Control | |||||||
| AT vs. Sham AT | ||||||||
| Yeh38 (2011) Taiwan | Lumbar disk herniation, lumbar spinal stenosis, spondylolisthesis | Patient blind, parallel 3 arms | 90 (30/30/30) | No difference (gender, age, body weight, height, other chronic diseases, admitted diagnosis, number of lumber surgeries, worst preoperative pain, average preoperative pain, operation duration, amount of blood loss) | 3 h after surgery 4 h after surgery | (A) True AES | (B) Sham AES (2 cm away from actual acupoints) (C) No treatment | (1) VAS (pain) 24 h after surgery (2) Opiate demands Postoperative dose during first 24 h |
| Yeh34 (2010a) Taiwan | Lumbar disk herniation, Lumbar spinal stenosis, lumbar vertebra dislocation | Patient blind, parallel 3 arms | 94 (33/30/31) | No difference (gender, age, employment, height, body weight, other chronic diseases, admitted diagnosis, lumber of lumber surgeries, worst preoperative pain, average preoperative pain, preoperative systolic blood pressure, preoperative diastolic blood pressure, type of operation, operation duration, amount of blood loss) | 1 h before surgery 1 h after surgery 2 h after surgery | (A) True AES | (B) Sham AES (2 cm away from actual acupoints) (C) No treatment | (1) VAS(pain) Before surgery 1 h after surgery 2 h after surgery 24 h after surgery (2) Opiate dose Postoperative dose during first 24 h |
| Wang36 (2000) Germany | Lumbar disk herniation | Patient blind, Parallel 2 arms | 132 (66/66) | No mentioned difference between the two groups | AT was conducted before and after corrective surgery for a total of 3-6 days | (A) Classic AT | (B) Placebo AT (2 cm away from actual acupoints) | (1) VAS (pain) Before AT Immediately after AT 0.5 h after AT 1 h after AT 2 h after AT 6 h after AT |
| AT vs. conventional therapy | ||||||||
| Li35 (2008) China | Lumbar disk herniation | Parallel 2 arms | 90 (45/45) | No difference (Gender, age, course of disease(narrative only)) | 6 h after surgery 1–3 days after surgery (twice a day) 4–7 days after surgery (once a day) | (A) Abdominal AT | (B) Drugs (anti-inflammatory and analgesic) | (1) VAS (pain) Before surgery 1 week after surgery 1 month after surgery 3 months after surgery |
| AT plus conventional therapy vs. conventional therapy | ||||||||
| Yeh37 (2010b) Taiwan | Lumbar spine (not reported details) | Parallel 2 arms | 74 (36/38) | No difference (gender, age, smoking, history of postoperative vomiting, history of spinal surgery, hypertension, diabetes, ASA class, operation duration, amount of blood loss, number of postoperative drains) | 1–3 days after surgery (four times) | (A) Auricular AT plus regular care | (B) Regular care alone | (1) VAS (pain) 2 h after surgery 24 h after surgery 48 h after surgery 72 h after surgery (2) Morphine demands Postoperative dose during first 24 h During 24–48 h after surgery During 48–72 h after surgery |
AES, acupoint electrical stimulation (non-penetration); AT, acupuncture; EA, electro-acupuncture; VAS, visual analogue scale; ASA, the American Society of Anaesthesiologists.
Characteristics of Included RCTs
Table 1 shows the differences in the baseline characteristics of the treatment and control groups. Four studies34,35,37,38 reported no differences between the two groups, whereas 1 study36 did not mention baseline imbalance.
All 5 studies34–38 included reported that treatments related to acupuncture were performed within 7 days after back surgery.
In outcome assessments, the VAS, opiate dose, or morphine dosage was used for pain intensity. Table 1 summarizes the details of the studies included.
Study Quality
The methodological quality of the RCTs was variable (Table 2). Two studies37,38 described a proper method of sequence generation. One study38 used a computerized randomization, and 1 other study37 used a randomization list. The other 3 studies34–36 did not clearly report how the allocation sequence was generated. Allocation was concealed in 2 studies.34,38 Participants blinding and personnel blinding were reported in 4 studies,34,36–38 and assessor blinding was reported in 3 studies.34,36,38 The risk of bias for incomplete outcome data was low in 2 studies,37,38 because details about dropouts and withdrawals were reported. In all, the 5 included RCTs34–38 had an unclear risk of bias in terms of selective reporting. Four studies34,35,37,38 were evaluated to be at low risk of bias from other sources because baseline characteristics were properly reported and not different between the treatment and control groups. However, 1 study36 was evaluated to be at high risk of bias from other sources because there were baseline imbalances in VAS without consideration of adjustment between the two groups. In total, 3 studies34,37,38 were considered high in quality (low risk of bias), 1 study36 was considered medium in quality, and the other 1 study35 was considered low in quality.
Table 2.
Cochrane Risk of Bias of Included Randomized Clinical Trials
| First Authorref (Year) | Yeh38 (2011) | Yeh34 (2010a) | Wang36 (2000) | Li35 (2008) | Yeh37 (2010b) |
|---|---|---|---|---|---|
| 1. Random sequence generation (selection bias) | L (computerized randomization) | U | U | U | L (randomization list) |
| 2. Allocation concealment (selection bias) | L (mentioned) | L (mentioned) | U | U | U |
| 3. Blinding of participants and personnel (performance bias) | L (patient blind) | L (patient blind) | L (patient blind) | U | L (mentioned) |
| 4. Blinding of outcome assessment (detection bias) | L (mentioned) | L (mentioned) | L (mentioned) | U | U |
| 5. Incomplete outcome data (attrition bias) | L (mentioned) | U | U | U | L (Mentioned) |
| 6. Selective reporting (reporting bias) | U | U | U | U | U |
| 7. Other bias | L | L | H | L | L |
Risk of bias: H, high risk of bias; L, low risk of bias; U, unclear.
Descriptions of Acupuncture Treatment
All of the RCTs stated that the rationale for acupuncture point selection was drawn from traditional Chinese medicine theory (Table 3). Two studies34,38 used acupoint electrical stimulation with nonpenetration, 1 study36 used classic acupuncture with manual stimulation, 1 study35 used abdominal acupuncture with classic acupuncture, and 1 study37 used acupressure on the ear.
Table 3.
Summary of Acupuncture Treatment Points and other Information Related to Acupuncture Treatment
| First Authorref (Year) | Acupuncture Method | Total Treatment (times) | Acupuncture Points | Deqi | Rationales for Acupuncture Points | Adverse Events |
|---|---|---|---|---|---|---|
| Yeh38 (2011) | AES | 2 | BL40, GB34, HT7, P6 | n.r. | TCM theory | No adverse effect |
| Yeh34 (2010a) | AES | 3 | BL40, GB34, HT7, P6 | n.r | TCM theory | n.r. |
| Wang36 (2000) | Classic AT with MS | 2–3 | BL25, GB31, BL26, GB30, BL62, BL23, BL36, BL40, GB34 | Considered | TCM theory | n.r. |
| Li35 (2008) | Abdominal AT with Classic AT | 10 | Standard points: CV12, CV9, CV6, CV4 Individualized: CV6 0.2 unit of length lateral (L2-3 surgery) CV5 0.2 unit of length lateral (L3-4 surgery) CV4 0.2 unit of length lateral (L4-5 surgery) Additive: KI14, ST25 (back pain) Ab7(CV6 0.5 unit of length lateral), ST26, Ab4, Ab6 (Sciatica) ST28, ST24 (Low back pain) | n.r. | TCM theory | n.r. |
| Yeh37 (2010b) | Auricular acupressure | 12 | TF4, AT3, AH9, CO4, CO3, CO18 | n.r. | TCM theory | n.r. |
AES, acupoint electrical stimulation (nonpenetration); AT, acupuncture; MS, manual stimulation; n.r., not reported; TCM, traditional Chinese medicine.
Outcomes
Acupuncture vs. Sham Acupuncture (3 RCTs)
Two RCTs34,38 evaluated the effect of acupoint electrical stimulation in comparison to sham acupoint electrical stimulation. The other 1 RCT36 reported the results of classic acupuncture versus sham acupuncture in terms of pain intensity as measured by VAS. In one study,36 the times at which the VAS were measured were before acupuncture, immediately after acupuncture, 0.5 hour after acupuncture, 1 hour after acupuncture, 2 hours after acupuncture, and 6 hours after acupuncture. In another study, the times at which pain was evaluated using the VAS scale were before surgery, 1 hour after surgery, 2 hours after surgery, and 24 hours after surgery.34 In the third study,38 pain was evaluated 24 hours after surgery (Table 1).
Two trials34,38 showed favorable effects of acupoint electrical stimulation that were superior to those of sham acupoint electrical stimulation.
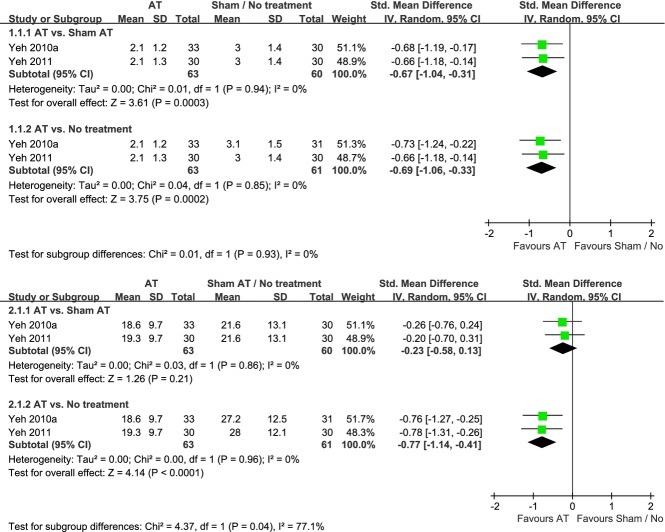
The pooled meta-analysis of data showed significant improvements in pain intensity for VAS 24 hours after surgery (2 studies34,38 n = 123, SMD, −0.67; 95% CI of −1.04 to −0.31, P = 0.0003, heterogeneity: χ2 = 0.01, P = 0.94, and I2 = 0%; Figure2.1).
Figure 2.
Meta-analysis of acupuncture for pain after back surgery. VAS, visual analogue scale; AT, acupuncture.
However, the pooled meta-analysis of data did not show significant improvements in postoperative opiate dose demands during the first 24 hours after surgery (2 studies34,38 n = 123, SMD, −0.23; 95% CI of −0.58 to 0.13, P = 0.21, heterogeneity: χ2 = 0.03, P = 0.86, and I2 = 0%; Figure2.2).
Acupuncture vs. No Treatment (2 RCTs)
Two RCTs34,38 evaluated the effect of acupoint electrical stimulation in comparison to no treatment. The points of time for measuring the VAS were before surgery, 1 hour after surgery, 2 hours after surgery, and 24 hours after surgery (Table 4).
Table 4.
Effect Estimates for Acupuncture for Acute Postoperative Pain after Back Surgery
| Outcome of Subgroup | Number of Studiesref | Number of Patients | Effect Estimate (SMD [95% CI]) |
|---|---|---|---|
| AT vs. sham AT | |||
| VAS (pain) | |||
| Before AT | 136 | 132 | −0.95 [−1.31, −0.59] |
| Immediately after AT | 136 | 132 | −2.91 [−3.40, −2.41] |
| 0.5 h after AT | 136 | 132 | −4.74 [−5.42, −4.07] |
| 1 h after AT | 136 | 132 | −5.68 [−6.45, −4.90] |
| 2 h after AT | 136 | 132 | −6.95 [−7.87, −6.03] |
| 6 h after AT | 136 | 132 | −9.82 [−11.07, −8.57] |
| Before surgery | 134 | 60 | NA |
| 1 h after surgery | 134 | 60 | NA |
| 2 h after surgery | 134 | 60 | NA |
| 24 h after surgery | 234,38 | 124 | −0.67 [−1.04, −0.31] |
| Opiate demands | |||
| Postoperative dose during first 24 h | 234,38 | 124 | −0.23 [−0.58, −0.13] |
| AT vs. no treatment | |||
| VAS (pain) | |||
| Before surgery | 134 | 60 | NA |
| 1 h after surgery | 134 | 60 | NA |
| 2 h after surgery | 134 | 60 | NA |
| 24 h after surgery | 234,38 | 124 | −0.69 [−1.06, −0.33] |
| Opiate demands | |||
| Postoperative dose during first 24 h | 234,38 | 124 | −0.77 [−1.14, −0.41] |
| AT vs. conventional therapy | |||
| VAS (pain) | |||
| Before surgery | 135 | 90 | 0.11 [−0.30, 0.52] |
| 1 week after surgery | 135 | 90 | 0.16 [−0.26, 0.57] |
| 1 month after surgery | 135 | 90 | −0.94 [−1.38, −0.50] |
| 3 months after surgery | 135 | 90 | −0.08 [−0.50, 0.33] |
| AT plus conventional therapy vs. conventional therapy | |||
| VAS (pain) | |||
| 2 h after surgery | 137 | 74 | NA |
| 24 h after surgery | 137 | 74 | NA |
| 48 h after surgery | 137 | 74 | NA |
| 72 h after surgery | 137 | 74 | NA |
| Morphine demands | |||
| Postoperative dose during first 24 h after surgery | 137 | 74 | NA |
| Postoperative dose 24 h–48 h after surgery | 137 | 74 | NA |
| Postoperative dose 48 h–72 h after surgery | 137 | 74 | NA |
AT, acupuncture; CI, confidence interval; NA, not applicable because of the lack of data on standard deviation in the original paper; SMD, standardized mean difference; VAS, visual analogue scale.
The pooled meta-analysis of the data showed significant improvements in pain intensity for VAS 24 hours after surgery (2 studies34,38 n = 124, SMD, −0.69; 95% CI of −1.06 to −0.33, P = 0.0002, heterogeneity: χ2 = 0.04, P = 0.85, and I2 = 0%; Figure2.1). In addition, the pooled meta-analysis of the data showed significant improvements in postoperative opiate dose demands during the first 24 hours after surgery (2 studies34,38 n = 124, SMD, −0.77; 95% CI of −1.14 to −0.41, P < 0.0001, heterogeneity:χ2 = 0.00, P = 0.96, and I2 = 0%; Figure2.2).
Acupuncture vs. Conventional Therapy (1 RCT)
One RCT35 evaluated the effect of acupuncture (abdominal acupuncture) in comparison with conventional therapy (drugs).
The points of time for measuring the VAS were before surgery, 1 week after surgery, 1 month after surgery, and 3 months after surgery.
There were no differences between the acupuncture and conventional therapy in terms of VAS for pain intensity before surgery and 1 week after surgery. However, the RCT showed acupuncture to be superior to conventional therapy in VAS for pain intensity 1 and 3 months after surgery (Table 4).
Acupuncture Plus Conventional Therapy vs. Conventional Therapy (1 RCT)
One RCT37 evaluated the effect of acupuncture plus conventional therapy (auricular acupuncture plus regular care) in comparison with conventional therapy (regular care alone).
The points of time for measuring the VAS were 2 hours after surgery, 24 hours after surgery, 48 hours after surgery, and 72 hours after surgery, whereas the points of time for measuring the morphine demands were during first 24 hours after surgery, during 24 hours to 48 hours after surgery, and during 48 hours to 72 hours after surgery.
However, the RCT37 was not applicable for effect estimates because of the lack of data on standard deviation in the original paper (Table 4).
The Safety of Acupuncture
Only 1 RCT38 reported adverse events associated with acupuncture or acupoint electrical stimulation and stated that there were no adverse events. None of others mentioned adverse events.
Discussion
Strengths and Weaknesses
This is the first systematic review and meta-analysis of RCTs that has critically evaluated the totality of RCTs for testing the effectiveness of acupuncture for acute postoperative pain relief after back surgery. Through rigorous searches without limitations on language, we found 5 RCTs comparing sham, no treatment, and conventional therapy.
Because there has been no systematic review summarizing the current evidence concerning the effectiveness of acupuncture for acute postoperative pain after back surgery, we considered to include all of acupuncture intervention types such as acupuncture with penetrating or nonpenetrating on acupoints stimulation. We also included trials that compared acupuncture plus a conventional therapy (i.e., regular care) with conventional therapy alone. But we excluded at nonacupuncture sites or acupuncture plus herbal medicine, because these methods of acupuncture were not able to evaluate the effects of specific acupuncture treatment.
Clinical merit of this systematic review is that it evaluated the possibility that acupuncture may act as an alternative or complementary modality when conservative therapies present lesser effects on pain or considerable adverse events when managing acute postoperative pain conditions after back surgery. Also, this systematic review was conducted in accord with the QUOROM statement39 and the PRISMA statement.40
Based on the Cochrane risk of bias assessment,20 the methodological quality was generally moderate (3 of the 5 were of high quality, but all of these were by the same author). In addition, 3 high-quality RCTs34,37,38 included in this review performed sample size estimation with appropriate power analysis. Whereas one trial35 included was of poor methodological quality in terms of the method of allocation concealment, blinding of participants and personnel, blinding of outcome assessment, and power analysis.
Most of the RCTs included were high-quality reports with respect to the revised standards for reporting interventions in clinical trials of acupuncture (STRICTA),41 especially for acupuncture techniques such as needle type, the depth of insertion, needle stimulation, and responses elicited.
However, the study designs of the RCTs included had some flaws in terms of several components of internal validity. First, the design for acupuncture compared to no treatments seems insufficient because it is difficult to control for nonspecific effects of acupuncture.42 Second, the design for acupuncture compared to conventional therapy is likely to have performance bias because it is not able to incorporate blinding properly.43 Third, the design for acupuncture compared to sham acupuncture also has questionable validity of using relevant sham control.
One of the most important questions is what methods of sham acupuncture are acceptable. There are various sham control methods which are penetrating minimal or superficial acupuncture, penetrating on nonacupoints, or a blunt tip touching the skin without penetration.44 However, there is still not enough evidence which design is the most appropriate sham control.45,46
Moreover, although sham procedure is methodologically necessary to produce valid results such as reducing the performance bias, ethical issues are apparent. It is possible to effect critical ethic problem by sham control without usual medical care for reducing the patient's pain that goes neglected.
Therefore, those study designs should have adhered more closely to the methodology of comparative effectiveness research (CER). CER is the direct comparison of existing interventions, aiming to determine which treatment works best for whom and under what circumstances.47 Accordingly, CER or pragmatic effectiveness trials that reflect clinical practice could find firm conclusion on effectiveness of acupuncture more clearly. Furthermore, CER could resolve the critical ethical issues.
Clinical Implications
Our meta-analysis of the pooled data on VAS for pain intensity showed superior effects of acupuncture during the first 24 hours after back surgery. In contrast, the meta-analysis of opiate demands did not show a positive effect of acupuncture. Despite the different results for the two pain outcomes, acupuncture seems to reduce acute postoperative pain in patients with back surgery. Yet, we could not find clear evidence on effectiveness of acupuncture for the following reason. First, the total numbers of RCTs and participants involved were too small to draw concrete conclusions on the therapeutic effect of acupuncture. Second, the specific and convictive mechanisms of acupuncture are still being elucidated. Third, the time for measuring the VAS differed between some studies (See Table 1). Further, there was lack of observation as to long-term follow-up.
Nevertheless, acupuncture may be an easy accessible,48 convenient49,50 and economical way11 to control pain after back surgery in clinical field. In addition, acupuncture appears to be a relatively safe treatment.10,51,52 If performed by well-trained practitioners, the adverse events occur rarely when used for neck and lower back pain.53,54 However, occasional serious events continue to be reported in relation to the safety of acupuncture.55,56
In this systematic review, only 1 RCT38 reported no adverse events for acupuncture treatment. Acupuncture did not appear to be associated with serious adverse events, but the evidence is limited. Adverse events associated with the use of acupuncture for controlling acute postoperative pain after back surgery should be reported in future research in more detail and rigorously assessed by standardized monitoring.
Based on this review, our main finding is that acupuncture seems to be effective for pain after back surgery, based on 3 high-quality RCTs34,37,38 and two meta-analyses, but the effect of acupuncture on pain after back surgery is limited due to some methodological flaws.
Conclusions and Future Research
In this systematic review, rigorous searches were performed following PRISMA guidelines. We note here several points that must be addressed in future research. First, future trials should adhere more closely to the methodology of comparative effectiveness research because sham-acupuncture-controlled trials may lead to critical ethic problem and could not reflect clinical practice circumstances. Thus, larger pragmatic effectiveness trials to compare acupuncture with standard treatments should be conducted. Second, the acupuncture points used varied widely and were not consistent across studies. However, this is a key feature of traditional Chinese medicine and its individualized point selection. Nevertheless, clinical heterogeneity (by 6 checklist items) can be an issue of standardization and should be considered by adhering to the revised STRICTA guidelines41 in reporting of acupuncture trial. Third, the RCTs included in this systematic review had various control groups and outcome measures, which made it difficult to draw firm conclusions concerning the effects of acupuncture on outcomes after back surgery. Thus, more consistent and standardized outcome measures should be used in future trials. In addition, future trials should observe CONSORT and STRICTA guidelines41 in their study designs.
Acknowledgments
This study was supported by the Korea Institute of Oriental Medicine (KIOM, Grant # K13273). The authors have no conflict of interests.
Author Contributions
YHC, CKK, KHH, and BCS contributed to the study conception and design. YHC and CKK performed search, determined the inclusion eligibility of trials, extracted data from the trials, and assessed the methodological quality of the trials. BCS provided a third assessment of the methodological quality of all trials. YHC, MSL, and BCS entered and organized the data, conducted the analyses, and drafted the manuscript. YHC, CKK, KHH, MSL, IHH, DWS, BKC, GSS, and BCS all contributed to check the analysis and interpretation of the data. YHC and BCS are the guarantors.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article:
Appendix S1. Summary of 7 RCTs of 2 chronic and 5 unknown the time of acupuncture application trials after back surgery.
References
- 1.Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine (Phila Pa 1976) 1994;19:1201–1206. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES. United States’ trends and regional variations in lumbar spine surgery: 1992-2003. Spine (Phila Pa 1976) 2006;31:2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Don AS, Carragee E. A brief overview of evidence-informed management of chronic low back pain with surgery. Spine J. 2008;8:258–265. doi: 10.1016/j.spinee.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 4.Cummins J, Lurie JD, Tosteson TD, et al. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial's (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine (Phila Pa 1976) 2006;31:806–814. doi: 10.1097/01.brs.0000207473.09030.0d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sommer M, de Rijke JM, van Kleef M, et al. The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur J Anaesthesiol. 2008;25:267–274. doi: 10.1017/S0265021507003031. [DOI] [PubMed] [Google Scholar]
- 6.Hutchison RW, Chon EH, Tucker J, et al. A comparison of a fentanyl, morphine, and hydromorphone patient-controlled intravenous delivery for acute postoperative analgesia: a multicenter study of opioid-induced adverse reactions. Hosp Pharm. 2006;41:659–663. [Google Scholar]
- 7.Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11:S105–S120. [PubMed] [Google Scholar]
- 8.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–1453. doi: 10.1001/archinternmed.2012.3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shin JS, Ha IH, Lee J, et al. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: a multicenter, randomized, controlled, comparative effectiveness trial. Pain. 2013;154:1030–1037. doi: 10.1016/j.pain.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Yamashita H, Tsukayama H, Tanno Y, Nishijo K. Adverse events in acupuncture and moxibustion treatment: a six-year survey at a national clinic in Japan. J Altern Complement Med. 1999;5:229–236. doi: 10.1089/acm.1999.5.229. [DOI] [PubMed] [Google Scholar]
- 11.Lin CW, Haas M, Maher CG, Machado LA, van Tulder MW. Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J. 2011;20:1024–1038. doi: 10.1007/s00586-010-1676-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JH, Choi TY, Lee MS, Lee H, Shin BC. Acupuncture for acute low back pain: a systematic review. Clin J Pain. 2013;29:172–185. doi: 10.1097/AJP.0b013e31824909f9. [DOI] [PubMed] [Google Scholar]
- 13.Bidwell S, Fabricious Jensen M. Etext on Health Technology Assessment (HTA) Information Resources, Chapter 3: Using a Search Protocol to Identify Sources of Information: The COSI Model. Bethesda, MD: National Information Center on Health Services Research and Health Care Technology (NICHSR); 2006. [Google Scholar]
- 14.Wikipedia. s.v. “acupuncture”, last modified October 27, 2013, http://en.wikipedia.org/wiki/Acupuncture.
- 15.Vickers A, Zollman C. ABC of complementary medicine. Acupuncture. BMJ. 1999;319:973–976. doi: 10.1136/bmj.319.7215.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Connor J, Bensky D. Acupuncture, A Comprehensive Text. Chicago: Eastland Press; 1981. [Google Scholar]
- 17.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 18.Vincent C, Lewith G. Placebo controls for acupuncture studies. J R Soc Med. 1995;88:199–202. [PMC free article] [PubMed] [Google Scholar]
- 19.Park J, White A, Stevinson C, Ernst E, James M. Validating a new non-penetrating sham acupuncture device: two randomised controlled trials. Acupunct Med. 2002;20:168–174. doi: 10.1136/aim.20.4.168. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JP, Green S, Collaboration C. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: Wiley Online Library; 2008. [Google Scholar]
- 21.Mo X, Chen Z, Shi H. A clinical study on analgesic effect of acupuncture and acupuncture combined with medicine on postoperative pain of resection of nucleus pulposus of lumbar intervertebral disc. Acupunct Res. 2000;25:296–299. [Google Scholar]
- 22.Martelete M, Fiori A. Comparative study of the analgesic effect of transcutaneous nerve stimulation (TNS); electroacupuncture (EA) and meperidine in the treatment of postoperative pain. Acupunct Electrother Res. 1985;10:183. doi: 10.3727/036012985816714432. [DOI] [PubMed] [Google Scholar]
- 23.Ou JY, Hong H, Wang WL, You YY. Observation on therapeutic effect of compound anesthesia of transcutaneous electrical point stimulation and Remifentanil. Zhongguo Zhen Jiu. 2008;28:826–828. [PubMed] [Google Scholar]
- 24.Li H, Dong M. Observation of combined acupuncture and cervical plexus anaesthesia applied in cervical operation by anterior route [Chinese] Clin Eng. 2012;19:595–596. [Google Scholar]
- 25.Wang C, Ci H, Gao Q, et al. Observation on the effect of silver needle therapy in the treatment of failed back surgery syndrome. Chin J Clin Rehabil. 2004:8. [Google Scholar]
- 26.Liao Z. Comparison analysis of cervical disease treatment by acupuncture and maneuver therapy. Chin J Clin Rehabil. 2003;7:1049. [Google Scholar]
- 27.Zheng SH, Wu YT, Liao JR, Xu MC, Hu CN, Zheng WC. Abdominal acupuncture treatment of failed back surgery syndrome clinical observation [Chinese] J Emerg Trad Chin Med. 2010;19:1497–1498. [Google Scholar]
- 28.Huang H, Zheng S, Feng J, et al. Thin's abdominal acupuncture for treatment of failed back surgery syndrome in 20 cases of clinical observation. Guid J Trad Chin Med Pharm. 2012;18:63–65. [Google Scholar]
- 29.Feng H, Zhang YF, Ding M. Analysis of therapeutic effect of lower limb sensation disorder after lumbar disc herniation operation treated with plum-blossom needle along meridians. Zhongguo Zhen Jiu. 2012;32:129–132. [PubMed] [Google Scholar]
- 30.Zhao BX, Wang KZ, Zhao JX, et al. Clinical effects of acupuncture after surgical operation in patients with prolapse of the lumbar intervertebral disc. J Tradit Chin Med. 2008;28:250–254. doi: 10.1016/s0254-6272(09)60003-0. [DOI] [PubMed] [Google Scholar]
- 31.Xuan P, Luo X, Luo S. Clinical research on acupuncture to treat patients with lower extremity numbness after accepting lumbar spinal stenosis operation. Chin Nurs Res. 2011;25:129–130. [Google Scholar]
- 32.Xin Z, Cao H, He Y, Qiu M, Zheng X, Sao P. Observation of therapeutic effect of electroacupuncture jiaji therapy for failed back surgery syndrome. Liaoning J Trad Chin Med. 2009;36:813–814. [Google Scholar]
- 33.Yu W, Huo S, Cai H, Lee R. A study on electric acupuncture point stimulation for failed back surgery syndrome by pulsed stimulation. Chin J Rehabil Med. 2001;16:161–163. [Google Scholar]
- 34.Yeh ML, Chung YC, Chen KM, Tsou MY, Chen HH. Acupoint electrical stimulation reduces acute postoperative pain in surgical patients with patient-controlled analgesia: a randomized controlled study. Altern Ther Health Med. 2010;16:10–18. [PubMed] [Google Scholar]
- 35.Li Y, Chen B, Lin D. Effect of abdominal acupuncture therapy on postoperative residual symptoms in patients with lumbar intervertebral disc herniation: an observation of 45 cases [J] J New Chin Med. 2008;5:049. [Google Scholar]
- 36.Wang RR, Tronnier V. Effect of acupuncture on pain management in patients before and after lumbar disc protrusion surgery–a randomized control study. Am J Chin Med. 2000;28:25–33. doi: 10.1142/S0192415X00000052. [DOI] [PubMed] [Google Scholar]
- 37.Yeh ML, Tsou MY, Lee BY, Chen HH, Chung YC. Effects of auricular acupressure on pain reduction in patient-controlled analgesia after lumbar spine surgery. Acta Anaesthesiol Taiwan. 2010;48:80–86. doi: 10.1016/S1875-4597(10)60018-5. [DOI] [PubMed] [Google Scholar]
- 38.Yeh ML, Chung YC, Chen KM, Chen HH. Pain reduction of acupoint electrical stimulation for patients with spinal surgery: a placebo-controlled study. Int J Nurs Stud. 2011;48:703–709. doi: 10.1016/j.ijnurstu.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 40.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 41.MacPherson H, Altman DG, Hammerschlag R, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. J Evid-Based Med. 2010;3:140–155. doi: 10.1111/j.1756-5391.2010.01086.x. [DOI] [PubMed] [Google Scholar]
- 42.Birch S. Controlling for non-specific effects of acupuncture in clinical trials. Clin Acupunct Orient Med. 2003;4:59–70. [Google Scholar]
- 43.Lao L, Ezzo J, Berman B, Hammerschlag R. Assessing clinical efficacy of acupuncture: considerations for designing future acupuncture trials. In: Stux G, Hammerschlag R, editors. Clinical Acupuncture. Berlin: Springer; 2001. pp. 187–209. [Google Scholar]
- 44.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med. 2006;24:13–15. doi: 10.1136/aim.24.1.13. [DOI] [PubMed] [Google Scholar]
- 45.He W, Tong Y, Zhao Y, et al. Review of controlled clinical trials on acupuncture versus sham acupuncture in Germany. J Tradit Chin Med. 2013;33:403–407. doi: 10.1016/s0254-6272(13)60187-9. [DOI] [PubMed] [Google Scholar]
- 46.Zhang CS, Yang AW, Zhang AL, May BH, Xue CC. Sham control methods used in ear-acupuncture/ear-acupressure randomized controlled trials: a systematic review. J Altern Complement Med. 2014;20:147–161. doi: 10.1089/acm.2013.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sox HC. Defining comparative effectiveness research: the importance of getting it right. Med Care. 2010;48:S7–S8. doi: 10.1097/MLR.0b013e3181da3709. [DOI] [PubMed] [Google Scholar]
- 48.Freedman LB. Acupuncture. New York: New York Times; 1994. [Google Scholar]
- 49.Chen SC, Lu SN, Lai CT, Jean JY, Hsiao CL, Hsu PT. Aqueous acupuncture for postoperative pain–a matched controlled trial. Gaoxiong Yi Xue Ke Xue Za Zhi. 1991;7:466–470. [PubMed] [Google Scholar]
- 50.Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. J Altern Complement Med. 2006;12:489–495. doi: 10.1089/acm.2006.12.489. [DOI] [PubMed] [Google Scholar]
- 51.MacPherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34 000 treatments by traditional acupuncturists. BMJ. 2001;323:486–487. doi: 10.1136/bmj.323.7311.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.White A, Hayhoe S, Hart A, Ernst E. Survey of adverse events following acupuncture (SAFA): a prospective study of 32,000 consultations. Acupunct Med. 2001;19:84–92. doi: 10.1136/aim.19.2.84. [DOI] [PubMed] [Google Scholar]
- 53.Furlan AD, Yazdi F, Tsertsvadze A, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid based Complement Alternat Med. 2012;2012:953139. doi: 10.1155/2012/953139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lao L, Hamilton GR, Fu J, Berman BM. Is acupuncture safe? A systematic review of case reports. Altern Ther Health Med. 2003;9:72–83. [PubMed] [Google Scholar]
- 55.Ernst E, Lee MS, Choi TY. Acupuncture: does it alleviate pain and are there serious risks? A review of reviews. Pain. 2011;152:755–764. doi: 10.1016/j.pain.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 56.Zhang J, Shang H, Gao X, Ernst E. Acupuncture-related adverse events: a systematic review of the Chinese literature. Bull World Health Organ. 2010;88:915C–921C. doi: 10.2471/BLT.10.076737. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Summary of 7 RCTs of 2 chronic and 5 unknown the time of acupuncture application trials after back surgery.