Abstract
The purpose of this paper is to report a case of chondroblastic osteosarcoma in the region of the maxilla, with 5 months of evolution. The term osteosarcoma refers to a heterogeneous group of malignancies with bone formation or mesenchymal tissue with histopathological evidence of osteogenic differentiation. The pattern of chondroblastic osteosarcoma represents 25% of all reported cases of this neoplasm. Its histopathological diagnosis is based on the predominance of a chondroid matrix formed in the midst of neoplastic cells. A woman patient, 27-year old, melanoderm, presented on extraoral exam with facial asymmetry caused by the a swelling in the premaxillary region with upper lip protrusion. Intraoral exam showed a maxillary tumefaction with involvement of the vestibular and palatine regions. The computerized tomography (CT) analysis exhibited a radiolucent mass with dispersed areas of radiopacity, with poorly defined and indistinct peripheral edges. The patient was subjected to incisional biopsy and histopathological examination showed the presence of a malignant neoplasm of mesenchymal origin characterized by the presence of irregular bone trabeculae dispersed among mildly atypical chondroblastic cells. The World Health Organization (WHO) recognizes several variants that differ in location, clinical behavior and degree of cellular atypia. The conventional or classical osteosarcoma is the most frequent variant, which develops within the medullary bone. This report illustrates the rapid evolution of one of the histological variants of osteosarcoma.
Keywords: Bone tumors, chondroblastic osteosarcoma, jaw, osteogenic sarcoma
INTRODUCTION
The term osteosarcoma refers to a heterogeneous group of malignant neoplasms with bone formation or malignant mesenchymal tissue that presents histopathological evidence of osteogenic differentiation.[1] The exact etiopathogenesis of the disease is still unknown;[2] however, according to Tossato et al.,[3] some risk factors have been associated with the development of osteosarcomas, such as fibrous dysplasia, retinoblastoma, previous exposure to radioactivity, Paget's disease and chronic osteomyelitis. Post-radiation osteogenic sarcoma has been related in bones with preexistent benign diseases, such as fibrous dysplasia and Paget's disease.[4]
The World Health Organization (WHO) recognizes several variants that differ in location, clinical behavior and degree of cellular atypia. The conventional or classical osteosarcoma is the variant that occurs most frequently. This neoplasm develops in the medullary region of bone and may be classified into various histological types,[1] namely: Fibroblastic, chondroblastic, osteoblastic, telangiectasic and mixed.[5]
Osteosarcomas that affect the bones of the cranium are relatively uncommon, with only about 10% occurring in the head and neck.[3 ] Approximately, 5% appear in the maxillary bones and the mandible is the most commonly involved site.[1] The age range of cases appears to be variable in various studies. In a study conducted in Curitiba, Brazil, between 1973 and 2000, based on medical charts of patients with head and neck osteosarcomas, the age range was from 13 to 66 years.[2] The most common symptoms of osteosarcoma include persistent pain, edema and paresthesia/anesthesia. General signs of the disease, such as fever or considerable weight loss, are rare.[6]
In imaging exams, such as radiographs and computerized tomographs, osteosarcoma has been shown as a radiopaque or mixed mass, homogeneous and central, multilocular and with poorly defined limits. There may be destruction of cortical bone and involvement of adjacent soft tissues.[3]
The prognosis for patients with osteosarcoma has improved greatly over the last few decades with the introduction of intensive chemotherapy.[7] The use of chemotherapy before and after surgery for removal of the tumor has been developed to promote local control of the tumor by reducing its size.[8] The parameters of prognostic value include the tumor localization, its size, response to chemotherapy, surgical remission and metastasis.[9,10] The factors for unfavorable prognosis include the presence of metastatic disease at diagnosis, tumor resection with compromised margins, absence of response to chemotherapy, voluminous tumors and elevated serum levels of lactate dehydrogenase (LDH).[11] The treatment of choice in oral osteosarcomas is surgical resection. Obtaining tumor free surgical margin is one of the main factors for local control.[12]
The purpose of this article is to relate a rare case of maxillary chondroblastic osteosarcoma with an emphasis on the clinical and histopathological aspects of the tumor.
CASE REPORT
A 27-year old woman, melanoderm, presented to the Bucco-maxillo-facial Surgery Service of the Dentistry Course, complaining of “a sensation of weight in her face when she ate”. During anamnesis, the patient mentioned an increase in volume in the premaxillary region, with 5 months of evolution, which developed with painful symptomatology and mobility of the maxillary anterior teeth. She reported no paresthesia, episodes of bleeding and/or infections. The patient presented no systemic diseases and her vital signs were shown to be adequate for her age. On extra-oral exam, facial asymmetry caused by a swelling in the premaxillary region with protrusion of the upper lip was observed [Figure 1a and b]. Intraoral exam showed a maxillary tumor with involvement of the vestibular and palatine regions, which extended from tooth 12 to 25 in the vestibular region and from tooth 13 to 24 on the palatine aspect. The swelling involved areas of interdental gingiva, alveolar mucosa and vestibular fornix and presented a normal mucosal color. However, the palatine mucosa in the region of tooth 11 was shown to be ulcerated due to masticatory friction [Figure 2a and b].
Figure 1.
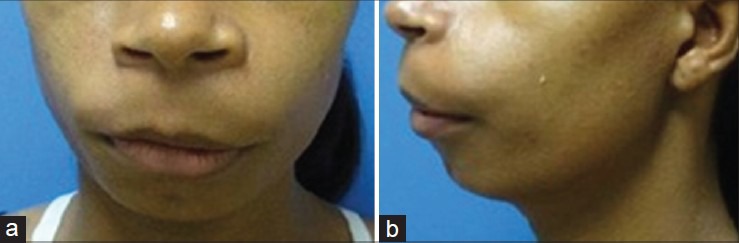
(a and b) Extraoral physical exam. Note facial asymmetry, caused by the swelling in the left premaxillary region, with protrusion of the upper lip
Figure 2.
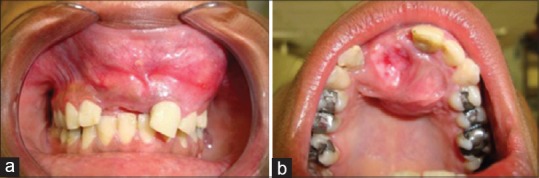
(a and b) Intraoral exam showed a tumor in the anterior maxillary region obliterating the anterior vestibular sulcus. The palatine mucosa in the region of tooth 11 was shown to be ulcerated due to masticatory friction
Complementary imaging diagnostic procedures were requested. Pantomography showed evidence of a poorly delimited lesion, with alterations in the bone trabeculae, causing root displacement in the premaxillary region [Figure 3]. Axial cut of the computerized tomography (CT) revealed a radiolucent mass with dispersed areas of radiopacity, with poorly defined and indistinct peripheral edges, causing complete destruction of the vestibular cortical and partial destruction of the palatine cortical bone [Figure 4a and b]. Possible metastasis had been ruled out, but there was no sign of secondary tumors. The patient was subjected to incisional biopsy and the specimen was sent to the Oral Pathology Service. The sections stained with hematoxylin and eosin showed evidence of a malignant neoplasm of mesenchymal origin, characterized by the presence of irregular bone trabeculae amidst discretely atypical chondroblastic cell proliferation [Figures 5, 6 and 7. At the periphery of mineralized tissue, hyperchromatic and pleomorphic fusiform cells were observed Figure 8. The histopathological diagnosis was chondroblastic osteosarcoma and it was confirmed by two pathologists of different pathology services.
Figure 3.
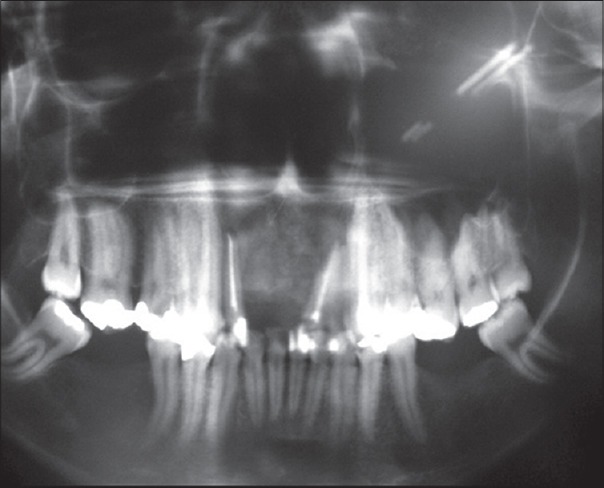
Orthopantomogram shows presence of a poorly delimited lesion, with alterations in the bone trabeculae, causing root displacement in the premaxillary region (arrows)
Figure 4.
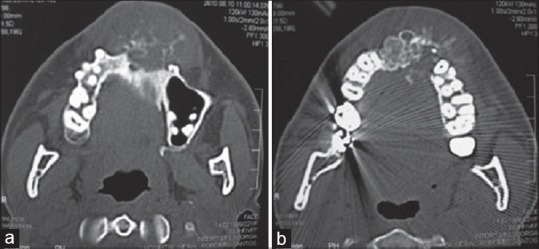
(a and b) Axial CT scan of the maxilla showed expansive lesion with an infiltrative nature, with poorly defined margins, presenting a varied pattern of bone resorption/bone neo formation and causing destruction of the cortical bone
Figure 5.
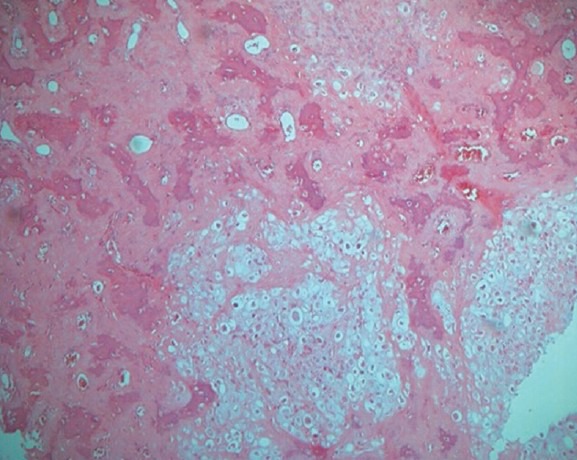
Low-power view of the lesion shows chondroid tissue with areas of osseous differentiation in the form of bone trabeculae. (H&E stain, ×40)
Figure 6.
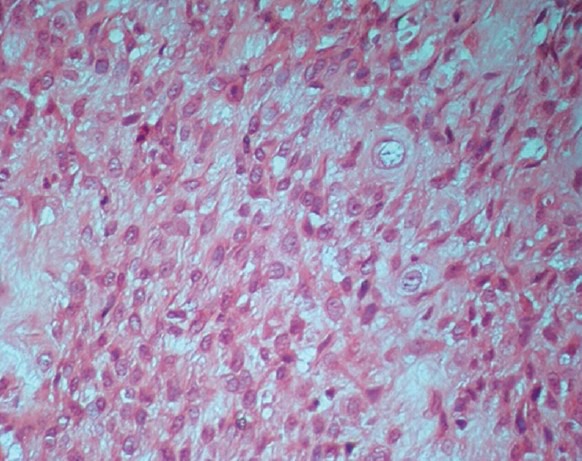
Chondroblastic matrix exhibiting chondrocytes with hyperchromatic and pleomorphic nuclei (H&E stain, ×400)
Figure 7.
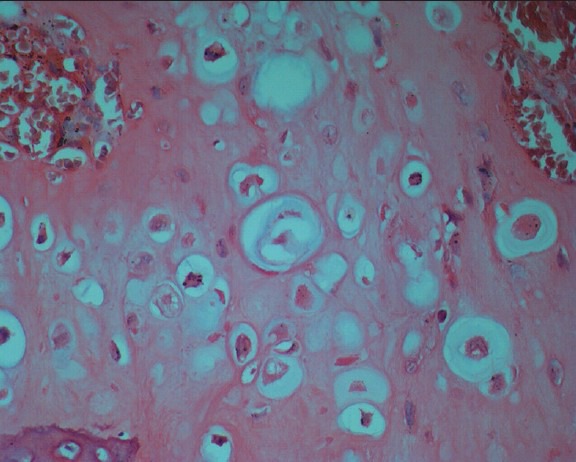
Pleomorphic chondrocytes with hyperchromatic nuclei. (H&E stain, ×400)
Figure 8.
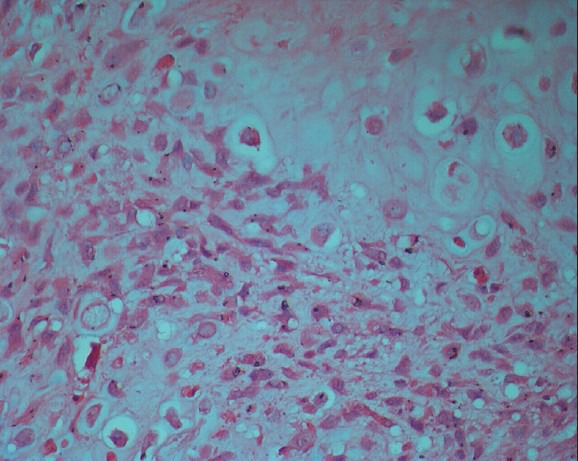
Presence of epitheliod and fusiform neoplastic chondrocytes. (H&E stain, ×400)
The patient was referred to an Oncology Service and is at present undergoing chemotherapy treatment for the purpose of achieving a reduction in volume of the lesion for a future surgical approach. Other additional exams have been requested like serum LDH and alkaline phosphatase levels and magnetic resonance imaging.
DISCUSSION
Osteogenic sarcomas (osteosarcomas) are the most common malignant bone tumors in children and young adults, constituting around 15% of all primary bone tumors;[13] however, according to Chindia (2001),[6] the age range of osteosarcoma cases is variable. In the present case, the mentioned lesion occurred in an adult patient, which corroborates the majority of reports in the literature, which indicate greater prevalence of the lesion in individuals in the 1st and 2nd decade of life. In Brazil, it is difficult to determine the annual incidence due to lack of adequate records. Nevertheless, there are an estimated 350 new cases per year.[14]
Pedruzzi et al.,[2] in 2006, conducted a retrospective analysis of the medical record charts of 13 patients with osteosarcomas of the head and neck, attended by the Head and Neck Service of a reference hospital. They found that this tumor was present in patients from 13 to 66 years of age (mean age of 31.5 years), with slight male predominance , with seven cases (53.8%) being men and six cases (46.2%) women. The tumor was located in the mandible in eight cases (61.5%) and in the maxilla in five cases (38.5%). Although the mandible is mentioned in the literature as the most affected site by the tumor, our patient exhibited an osteosarcoma in the anterior region of the maxilla, which led to elevation of the ala of the nose.
Tooth mobility may be related to osteosarcoma of the mandible and maxilla and in some situations, may be the first sign of the disease. The increase in volume in the facial region could rapidly be perceived due to esthetic and functional problems.[15] In this clinical case report, the patient presented an increase in volume in the region of the premaxilla, with an evolution time of 5 months, that developed with painful symptomatology and mobility of the teeth close to the tumor, ratifying the aspects classically described in the literature.
In addition to an incisional biopsy, diagnostic evaluation should include a detailed clinical history, physical exam, radiographs of the affected site, including CT or magnetic resonance of the area.[6] CT is an excellent auxiliary method in the diagnosis of osteosarcomas, as it provides visualization of tumoral calcifications, involvement of cortical bone and soft tissues and the medullary extension.[3] In the present case, CT of the region was performed, which showed evidence of a mixed mass, radiolucent with dispersed areas of radiopacity, with poorly defined and indistinct peripheral edges, that was not possible to visualize in panthomography. Furthermore, it presented aggressive destruction of the cortical bone involving adjacent soft tissues and bones. These characteristics led to an imaging diagnosis of malignant neoplasia suggestive of osteosarcoma. Nevertheless, other authors have pointed out that osteosarcomas may present as a radiopaque, homogeneous and well-delimited mass.[3]
The WHO recognized four histopathological variants of osteosarcoma. In this sense, the following are examples: The osteoblastic variant, in which osteoid matrix or bone predominates in the midst of stroma; the fibroblastic variant, which is characterized by high degree of fusiform neoplasic cells, with minimal quantities of bone matrix, with or without the presence of cartilage; and the telangiectatic tumor, which contains full or empty blood vessels separated by thin septae simulating aneurysmal bone cysts. Occasionally, the sections at the edges of lesions evidence the permeation of a hemorrhagic area. The quantity of osteoid described is varied. In small samples, the only finding may be a blood clot with some malignant cells. According to the WHO classification, the chondroblastic osteosarcoma is defined as a histological entity characterized by predominant presence of chondroid matrix, which tends to exhibit a high degree of hyaline cartilage and is intimately associated with the non-chondroid element (osteoid or bone matrix).[16] In this case report, it was observed that the tumor presented proliferation of atypical chondroblastic cells, with the presence of irregular bone trabeculae and hyperchromatic discretely pleomorphic fusiform cells at the periphery of mineralized tissue. Possible syndromes like Li–Fraumeni, Rothmund-Thompson and Bloom and Werner; that are risk factors for development of osteosarcoma[17,18] were also considered, but there were no evidence of any such associated syndromes with the present case report.
The treatment of OS demands resection with tumor-free margins and the use of systemic chemotherapy. The therapeutic approach to tumor is based on treatment protocols, such as that established by the European Osteosarcoma Intergroup (EOI), which consists of cycles of cisplatin and doxorubicin and that established by the Brazilian Protocol for Metastatic and No Metastatic Osteosarcoma, with cycles of cisplatin, ifosfamide and doxorubicin.[11] Borba et al.,[16] affirmed that complete surgical excision with negative margins continues to be the main pillar of treatment. Ruνz-Godoyet al.,[19] agree that ample excision is the treatment of choice, although it would be necessary to increase the number of cases in order to determine the behavior of this neoplasia with greater precision. Pedruzzi et al.,[2] related that although surgical resection is the main therapeutic approach, difficulties of obtaining free margins in osteosarcomas of head and neck arise because the anatomy of this region is more complex in comparison with the anatomy of free extremities.
In the present case report, the patient was submitted to incisional biopsy, which provided histopathological diagnosis of chondroblastic osteosarcoma and was afterwards referred to an Oncology Service. At present, the patient is undergoing chemotherapy treatment, in which an adequate therapeutic protocol was adopted and established in accordance with the degree and staging of the tumor.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Soares RC, Soares AF, Souza LB, Santos AL, Pinto LP. Osteosarcoma of the mandible initially resembling lesion of dental periapex: A case report. Braz J Otorhinolaryngol. 2005;71:242–5. doi: 10.1016/S1808-8694(15)31318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pedruzzi PA, Costa PB, Oliveira BV, Ramos GH, Sassi LM, Orlandi D. Osteosarcoma of the head and neck. Rev Bras Cir Cabeç Pescoço. 2006;35:255–9. [Google Scholar]
- 3.Tossato Pdos S, Pereira AC, Cavalcanti MG. Osteosarcoma and chondrosarcoma--radiographic differentiation using computerized tomography. Pesqui Odontol Bras. 2002;16:69–76. doi: 10.1590/s1517-74912002000100012. [DOI] [PubMed] [Google Scholar]
- 4.Prakash O, Varghese BT, Mathews A, Nayak N, Ramchandran K, Pandey M. Radiation induced osteogenic sarcoma of the maxilla. World J Surg Oncol. 2005;3:49. doi: 10.1186/1477-7819-3-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lima JJ, Manzi R, Silva FL, Baptista MZ. Extra-skeletal osteosarcoma in the cervical region - literature review and case report. Radiol Bras. 2002;35:315–9. [Google Scholar]
- 6.Chindia ML. Osteosarcoma of the jaw bones. Oral Oncol. 2001;37:545–7. doi: 10.1016/s1368-8375(00)00129-9. [DOI] [PubMed] [Google Scholar]
- 7.Silva HR, Borges AC, Pizza M, Borsato ML, Castro HC, Luporini SM, et al. Osteosarcoma and acute myeloid leukemia - two cases in children. Rev Bras Hematol Hemoter. 2006;28:76–8. [Google Scholar]
- 8.Guerra RB, Tostes MD, da Costa Miranda L, Pires de Camargo O, Baptista AM, Caiero MT, et al. Comparative analysis between osteosarcoma and Ewing's sarcoma: Evaluation of the time from onset of signs and symptoms until diagnosis. Clinics (Sao Paulo) 2006;61:99–106. doi: 10.1590/s1807-59322006000200003. [DOI] [PubMed] [Google Scholar]
- 9.Alves MT, Miiji LN, Marinho LC, Petrilli AS, Jesus-Garcia R, Tolledo SC, et al. Human osteosarcoma with high immunoreactivity of P 53, erbB-2 and P-glycoprotein, and correlation with anaplasia parameter. Bras Patol Med Lab. 2008;44:107–14. [Google Scholar]
- 10.Castro HC, Ribeiro KC, Bruniera P. Osteosarcoma: Experience of the pediatric oncology service of holy house of mercy in São Paulo. Rev Bras Ortop. 2008;43:108–15. [Google Scholar]
- 11.Rech A, Castro CG, Jr, Mattei J, Gregianin L, Di Leone L, David A, et al. Clinical features in osteosarcoma and prognostic implications. J Pediatr (Rio J) 2004;80:65–70. [PubMed] [Google Scholar]
- 12.Ribeiro AL, Nobre RM, Alves Junior SM, Souza PA, Silva Junior NG, Pinheiro JJ. The importance of early diagnosis and an accurate tumoral evaulation in the treatment of mandibular osteosarcoma. Rev Odonto Ciêc. 2010;25:319–24. [Google Scholar]
- 13.Nanci Neto F, Marchiori E, Vianna AD, Aymoré IL, Almeida AL, Irion KL, et al. Parosteal osteosarcoma: Findings on conventional radiology. Radiol Bras. 2007;40:81–6. [Google Scholar]
- 14.Bispo Junior RZ, Camargo OP. Is there a difference in the prognosis of patients with primary osteosarcoma with poor response to neoadjuvant chemotherapy between grades I and II of Huvos? Rer Bras Ortop. 2011;46:420–3. doi: 10.1016/S2255-4971(15)30256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fletcher CD, Unni KK, Mertens F. 1st edition. France: IARC Press Lyon; 2002. Pathology and genetics of tumours of soft tissue and bone; p. 266. [Google Scholar]
- 16.Borba MA, Farias TP, Sá RM, Dias FL, Freitas EQ, Lima RA, et al. Osteosarcoma of the jaw: Prognosis factors. Rev Bras Cir Cabeç Pescoço. 2004;33:15–9. [Google Scholar]
- 17.Calvert GT, Randall RL, Jones KB, Cannon-Albright L, Lessnick S, Schiffman JD. At-risk populations for osteosarcoma: The syndromes and beyond. Sarcoma 2012. 2012 doi: 10.1155/2012/152382. 152382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hicks MJ, Roth JR, Kozinetz CA, Wang LL. Clinicopathologic features of osteosarcoma in patients with Rothmund-Thomson syndrome. J Clin Oncol. 2007;25:370–5. doi: 10.1200/JCO.2006.08.4558. [DOI] [PubMed] [Google Scholar]
- 19.Ruíz-Godoy RL, Meneses-García A, Mosqueda-Taylor A, De La Garza-Salazar J. Well- differentiated intraosseous osteosarcoma of the jaws: Experience of two cases from the Instituto Nacional de Cancerología, México. Oral Oncol. 1999;35:530–3. doi: 10.1016/s1368-8375(99)00005-6. [DOI] [PubMed] [Google Scholar]


