Background: The mechanism of H5N1 pathogenesis in humans remains unclear.
Results: SAEC-T clones were poorly susceptible to previously circulating avian influenza viruses but were completely susceptible to H5N1.
Conclusion: Infectivity depends on a delicate balance between acid stability of viral hemagglutinin and endosomal pH in infected cells.
Significance: These findings could explain why H5N1 is directly transmitted to humans from birds, resulting in serious illness.
Keywords: Endosome, Epithelial Cell, Membrane Fusion, Viral Protein, Virus Entry, Avian Influenza Virus, Endosomal pH, Hemagglutinin, Tropism
Abstract
The highly pathogenic avian influenza (AI) virus, H5N1, is a serious threat to public health worldwide. Both the currently circulating H5N1 and previously circulating AI viruses recognize avian-type receptors; however, only the H5N1 is highly infectious and virulent in humans. The mechanism(s) underlying this difference in infectivity remains unclear. The aim of this study was to clarify the mechanisms responsible for the difference in infectivity between the current and previously circulating strains. Primary human small airway epithelial cells (SAECs) were transformed with the SV40 large T-antigen to establish a series of clones (SAEC-Ts). These clones were then used to test the infectivity of AI strains. Human SAEC-Ts could be broadly categorized into two different types based on their susceptibility (high or low) to the viruses. SAEC-T clones were poorly susceptible to previously circulating AI but were completely susceptible to the currently circulating H5N1. The hemagglutinin (HA) of the current H5N1 virus showed greater membrane fusion activity at higher pH levels than that of previous AI viruses, resulting in broader cell tropism. Moreover, the endosomal pH was lower in high susceptibility SAEC-T clones than that in low susceptibility SAEC-T clones. Taken together, the results of this study suggest that the infectivity of AI viruses, including H5N1, depends upon a delicate balance between the acid sensitivity of the viral HA and the pH within the endosomes of the target cell. Thus, one of the mechanisms underlying H5N1 pathogenesis in humans relies on its ability to fuse efficiently with the endosomes in human airway epithelial cells.
Introduction
The first case of human infection by the highly pathogenic avian influenza (AI)2 virus H5N1 (HPAIV H5N1) was reported in Hong Kong in 1997. Since then, H5N1 viruses have spread worldwide and are prevalent in Asia, Europe, and Africa (particularly Egypt). To date, more than 648 human H5N1 infections have been officially reported, more than half of which have proven fatal (1).
The surface hemagglutinin (HA) protein of influenza viruses recognizes terminal sialic acid (SA) and galactose residues on sialylglycans. In general, human influenza viruses preferentially recognize receptors expressing terminal α2,6-linked SA (α2,6SA) residues, which are abundantly expressed in the human upper respiratory tract, although AI viruses preferentially bind to receptors expressing terminal α2,3SA residues, which are expressed mainly in the respiratory and enteric tracts of birds (2). The H5N1 virus infects the human lower respiratory tract, including the bronchioles and alveoli, which express both α2,3SA and α2,6SA residues (3, 4). This receptor distribution is thought to be the reason why H5N1 viruses can be transmitted from birds to humans. However, even though all AI subtypes, including H5, H7, and H9, bind α2,3SA, H5N1 is one of the few AI viruses that is highly infectious and virulent in humans (H7N7 and the recently emerged H7N9 can also infect humans in some cases) (5, 6). To date, few studies have examined the mechanism(s) underlying AI infection of humans, other than receptor specificity. Therefore, the mechanism(s) underlying H5N1 infection of human respiratory tissue must be identified if we are to fully understand the pathogenesis of this virus.
MDCK and A549 cells are susceptible to infection by influenza viruses; however, because these cell lines were derived from non-human tissue and carcinoma cells, respectively, they are not suitable for investigating viral infection of human respiratory tissue. Thus, novel cell lines that maintain the phenotype of human airway epithelia are required. To this end, we transformed human bronchiolar epithelial cells (small airway epithelial cells (SAECs)) with the SV40 large T-antigen and isolated several clonal cell lines (SAEC-Ts). A previous study suggests that human bronchial epithelial cells are a better model of influenza virus infectivity and tropism than other cell types (7). Also, cells immortalized with SV40 large T-antigen show both the morphological and functional characteristics of the parental cells (8, 9).
Here, we examined the ability of currently circulating H5N1 and previously circulating AI viruses to infect different SAEC-T clones. The results suggest that post-receptor binding steps, particularly those within the endosomes of the target cells, play a key role in the infectivity of AI viruses and that the high fusogenic activity of H5N1 results in severe pathogenicity in humans.
EXPERIMENTAL PROCEDURES
Viruses and Cells
Influenza virus strains A/crow/Kyoto/53/04 (H5N1) (Cw/Ky (H5N1)) and A/chicken/Egypt/CL6/07 (H5N1) (Ck/Eg (H5N1)) were isolated from embryonated chicken eggs inoculated with tracheal or lung homogenates from dead crows (10) or dead chickens (11), respectively. A/Beijing/262/95 (H1N1) (Beijing (H1N1)), A/Duck/Hong Kong/273/78 (H2N2) (Dk/Hk (H2N2)), A/Panama/2007/99 (H3N2) (Panama (H3N2)), A/Duck/Hong Kong/668/79 (H4N5) (Dk/Hk (H4N5)), A/Duck/Hong Kong/820/80 (H5N3) (Dk/Hk (H5N3)), A/Turkey/Ontario/7732/66 (H5N9) (Tk/Ont (H5N9)), A/Duck/Hong Kong/960/80 (H6N2) (Dk/Hk (H6N2)), A/wigeon/Osaka/1/01 (H7N7) (Wg/Os (H7N7)), A/Turkey/Ontario/6118/67 (H8N4) (Tk/Ont (H8N4)), and A/Duck/Hong Kong/448/78 (H9N2) (Dk/Hk (H9N2)) were kind gifts from Yoshinobu Okuno (Kanonji Institute, the Research Foundation for Microbial Diseases of Osaka University, Kagawa, Japan). These influenza virus strains were grown in 9-day-old embryonated chicken eggs. For subsequent studies, allantoic fluids were pre-cleared by centrifugation at 3,300 × g for 20 min followed by filtration through 0.45-μm filters. The viruses were then purified by centrifugation (112,500 × g for 2 h) through PBS containing 20% sucrose. Virus pellets were resuspended in PBS, and aliquots were stored as working stocks at −80 °C. Virus titers were measured in focus-forming assays in MDCK cells and expressed as focus-forming units/ml (12). All experiments with live avian viruses were performed at Osaka University or at the Kyoto Prefectural University of Medicine under Biosafety Level 3+ conditions (as approved by the Ministry of Agriculture, Forestry and Fisheries, Japan). MDCK cells were purchased from the Riken BioResource Center Cell Bank (Ibaragi, Japan). Human lung epithelial carcinoma (A549) cells were kindly provided by the Cell Resource Center for Biomedical Research (Tohoku University, Sendai, Japan). Human primary SAECs were purchased from Lonza Corp. (Walkersville, MD).
Reagents
MDCK and A549 cells were cultured in minimal essential medium supplemented with 10% fetal bovine serum (FBS) and standard antibiotics. SAECs were cultured in Small Airway Cell Growth Medium (SAGM, Lonza) according to the manufacturer's recommendations. SAEC-Ts were cultured in D/M medium (DMM), which is based on Dulbecco's modified Eagle's medium (DMEM), and MCDB153 (1:1), supplemented with growth factors (bovine pituitary extract (30 μg/ml), hydrocortisone (0.5 μg/ml), epidermal growth factor (0.5 ng/ml), epinephrine (0.5 μg/ml), transferrin (10 μg/ml), insulin (5 μg/ml), triiodothyronine (6.5 ng/ml), retinoic acid (0.1 ng/ml), and cholera toxin (0.1 μg/ml)), 5% FBS, and antibiotics (penicillin (100 units/ml), streptomycin (100 μg/ml), and amphotericin B (250 ng/ml)). Primary SAECs were also cultured in DMM in the virus infection experiment.
Establishment of SAEC-derived Cell Clones
SAECs were immortalized by transformation with the SV40 large T-antigen gene as described previously (13). Briefly, after primary culture, a monolayer of primary SAECs was exposed to a retroviral vector containing a gene encoding the SV40 large T-antigen in medium including Polybrene (8 μg/ml). Five hours later, the medium was replaced with SAGM. The cells were then incubated for 1 week. Immortalized cells were selected by adding G-418 sulfate (500 μg/ml) to the culture medium. Single cell clones were isolated by limiting dilution in a 96-well microplate to establish SAEC-T clones.
Assessment of SA Expression by Flow Cytometry
SAEC-T monolayers were detached by exposure to 0.025% trypsin/EDTA and then fixed with 4% paraformaldehyde for 30 min at 4 °C. After washing twice with PBS containing 10 mm glycine and once with PBS, the cells were blocked with PBS containing 1% bovine serum albumin for 1 h at 4 °C. The cells were then incubated for 1 h at 4 °C with 2.5 μg/ml Sambucus nigra-FITC (Vector Laboratories, Burlingame, CA) to detect SAα2,6 or with Maackia amurensis-FITC (Vector Laboratories) to detect SAα2,3. After washing three times with PBS, 50,000 events were acquired on a FACSCalibur flow cytometer (BD Biosciences) to measure fluorescence intensity. Data were analyzed using CellQuest software (BD Biosciences). MDCK, 1A5, and 21E5 cells were also treated with Arthrobacter ureafaciens sialidase (100 milliunits/ml, Nacalai Tesque, Kyoto, Japan; prepared in PBS (pH 6.8)) for 4 h at 37 °C (or mock-treated) before lectin staining.
Plasmid Construction
Viral RNA was isolated using TRIzol reagent (Invitrogen), and cDNA was synthesized using random hexamers. The full-length HA sequences from Dk/Hk (H2N2), Dk/Hk (H4N5), Cw/Ky (H5N1), Ck/Eg (H5N1), Tk/Ont (H5N9), Dk/Hk (H6N2), Wg/Os (H7N7), and Tk/Ont (H8N4) were constructed by PCR. The HA sequences of A/Thailand/Kan353/04 (H5N1) (Thailand (H5N1)), A/Indonesia/5/05 (H5N1) (Indonesia (H5N1)), and A/Shanghai/1/06 (H5N1) (Shanghai (H5N1)) were constructed by PCR using overlapping deoxyoligonucleotides corresponding to the published sequence of the HA open reading frame. The full-length sequences of both A/duck/Egypt/D1Br/2007 (H5N1) (Dk/Eg (H5N1)) (clade 2.2.1) (PB2, PB1, PA, HA, NP, NA, M, and NS) (11) and Dk/Hk (H5N3) (PB2, PB1, PA, HA, NP, NA, M, and NS) were constructed by PCR. The virulent HA sequence of Dk/Hk (H5N3) was constructed by changing single basic amino acids within the HA cleavage site to multiple basic amino acids (N′-TR-C′ to N′-RRKKR-C′), as described previously (10). The HA genomes of H5N1 (Cw/Ky (H5N1), Ck/Eg (H5N1), Thailand (H5N1), Indonesia (H5N1), or Shanghai (H5N1)) and the eight-segment sequence of Dk/Eg (H5N1) and Dk/HK (H5N3), including the virulent HA sequence, were cloned into the transcription plasmid, pPOLI (14). The HA open reading frame sequences from Dk/Hk (H2N2), Dk/Hk (H4N5), Cw/Ky (H5N1), Ck/Eg (H5N1), Thailand (H5N1), Indonesia (H5N1), Shanghai (H5N1), Dk/HK (H5N3), Tk/Ont (H5N9), Dk/Hk (H6N2), Wg/Os (H7N7), and Tk/Ont (H8N4) were cloned into pCAGGS protein expression plasmids (15).
Generation of Recombinant H5N3 and H5N1 Viruses
Recombinant viruses were generated using a previously described reverse genetics system (14–16), with slight modifications. Briefly, the pPOLI plasmid containing seven genomes of Dk/HK (H5N3) and its virulent HA genome (harboring multiple basic amino acids), or each of the H5N1 HA genomes described above, was transfected together with pCAGGS expression plasmids (15) harboring WSN PA, PB1, PB2, and NP into 293T cells that had been co-cultured with CEFs (at a ratio of 7:3). The pPOLI plasmid containing eight genomes of Dk/Eg (H5N1) was used together with pCAGGS (WSN PA, PB1, PB2, and NP) to generate recombinant Dk/Eg (H5N1). Next, 5 μg/ml of acetylated trypsin (Sigma) was added to the plates at 1 and 4 days post-transfection. At 7 days post-transfection, the culture supernatants were collected and injected into 9-day-old chicken eggs. The allantoic fluid was collected at 3 days post-injection and titrated to measure the number of focus-forming units/ml. All recombinant Dk/HK (H5N3) viruses (including the virulent HA and H5N1 HA genomes) were confirmed by sequencing.
Virus Infection
Primary SAECs, SAEC-Ts, and MDCK cells were cultured in 96-well plates (2.0 × 104 cells/well) or 24-well plates (1.0 × 105 cells/well) and then infected with viruses at an m.o.i. of 1, 3, or 10. The cells were then incubated at 37 °C for 1 h. The medium containing the virus was removed, and the cells were washed twice. MDCK cells were then cultured in minimum essential medium (Sigma) containing 10% FBS, and primary SAECs and SAEC-T cells were cultured in DMM containing 5% FBS. Virus-infected cells were subjected to immunofluorescence analysis to detect viral antigens or used in cell fusion assays.
Immunofluorescence Analysis
Cells were cultured in 96-well plates (2.0 × 104 cells/well). At 16 h post-infection, cells were fixed with PBS containing 4% paraformaldehyde and 0.1% Triton X-100 for 30 min at room temperature and washed with PBS (three times). The cells were then stained with a rabbit polyclonal antibody against A/Duck Hong Kong/342/78 (H5N2) to detect influenza virus antigens. This antibody recognizes influenza virus NP and M1 proteins. Antibody binding to viral proteins was detected with an Alexa Fluor 488-conjugated secondary antibody (Molecular Probes, Carlsbad, CA) diluted 1:500 in PBS containing 1% bovine serum albumin. Cell nuclei were counterstained with Hoechst 33342 (Sigma). To determine the percentage of cells (for each SAEC-T clone) infected with the viruses (the infectivity ratio), the cells were photographed, and the number of antigen-positive cells and cell nuclei visible in the microscope field were counted (more than three independent cell culture experiments were performed). Cell nuclei (in more than 1,000 cells infected with each virus strain) were counted using ImageJ, and antigen-positive cells were counted using a manual counter. The percentage of cells (for each SAEC-T clone) infected by the virus (the infectivity ratio) was calculated by dividing the number of antigen-positive cells by the total number of nuclei in the same field. The results are expressed as the mean ± S.D. of at least three independent cell cultures.
Western Blot Analysis of Virus Binding to SAEC-T Clones
Viruses were allowed to bind to SEAC-T cell clones cultured in 24-well plates (1.0 × 105 cells/well). Briefly, cells were washed twice with PBS, infected with viruses at an m.o.i. of 10, and then incubated at 4 °C for 1 h to avoid endocytosis. The cells were then washed five times with ice-cold PBS and lysed with PBS containing 2% SDS. Lysates (10 μg of protein per lane; measured using the bicinchoninic acid protein quantification kit; Pierce) were subjected to electrophoresis in a 10% SDS-polyacrylamide gel. Lysed free virus particles were used as detection and loading controls. The proteins were then transferred to nitrocellulose membranes and blocked overnight in PBS containing 5% nonfat milk and 0.05% Tween 20 at 4 °C. The membrane was reacted with a rabbit polyclonal antivirus antibody (diluted 1:2,000 in PBS containing 5% nonfat milk and 0.05% Tween 20), followed by a horseradish peroxidase-conjugated donkey anti-rabbit IgG (1:10,000 in PBS containing 0.05% Tween 20; Jackson ImmunoResearch) at room temperature. The membrane was washed with PBS containing 0.05% Tween 20 between steps. The reactive bands were visualized using the enhanced chemiluminescence system (Pierce) and Fuji XR film. The intensity of each band was measured using ImageJ.
Imaging the Internalization of Fluorescently Labeled Virus Particles in Live Cells
Virus particles were labeled with octadecyl rhodamine B (R18; Molecular Probes) as described previously (17), with some modifications. Briefly, purified virions (105 focus-forming units/ml) were suspended in 0.5 ml of PBS containing 1 μm R18. The reaction mixture was gently shaken in the dark for 1 h at room temperature and then passed twice through a filter (0.22-μm pore size; Millipore). Before viral infection, cell monolayers were labeled with the cytoplasmic dye CellTracker Green 5-chloromethylfluorescein diacetate (Molecular Probes), according to the manufacturer's instructions. Nuclei were stained with Hoechst 33342 (Sigma). Dye-labeled cells were washed twice with PBS, infected with viruses at an m.o.i. of 3, and incubated at 4 °C for 15 min. After removing the viruses, cells were washed twice and cultured in DMM containing 5% FBS in a temperature-controlled chamber mounted on the stage of a confocal laser scanning microscope (OLYMPUS, Tokyo, Japan). The chamber was maintained at 37 °C under a humidified 5% CO2 atmosphere. Images were taken with a ×100 oil objective lens (NA = 1.4, OLYMPUS), and data were acquired using FV1000 Viewer software (OLYMPUS).
Cell Fusion Assay
MDCK cells (1.0 × 105 cells/well) were cultured in 24-well plates and infected with viruses at an m.o.i. of 1. At 8 h post-infection, the cells were washed twice with PBS followed by fusion buffers at different pH (150 mm NaCl adjusted to pH 5.0, 5.125, 5.25, 5.375, 5.5, 5.625, 5.75, or 5.875 with 10 mm HEPES). Cells were incubated with each fusion buffer for 5 min and then returned to DMEM/F-12 medium containing trypsin (0.25 μg/ml) and cultured for 2–3 h at 37 °C. Cells were then fixed with 0.5% (v/v) glutaraldehyde and stained with 0.025% (w/v) crystal violet. Micrographs were taken at ×10 magnification. Alternatively, MDCK cells (cultured to 90% confluency in 24-well plates) were transfected with pCAGGS plasmids coding the HA gene sequences of different AI virus strains using Lipofectamine 2000 (Invitrogen) according to the manufacturer's recommendations. At 24 h post-transfection, cells were treated with the different pH buffers, cultured, and fixed as described above.
Polykaryons containing more than five nuclei were counted as described previously (18). The pH threshold was defined as the highest pH value at which polykaryon formation was observed.
Measurement of Endosomal pH
The endosomal pH in the SAEC-T clones was measured by confocal microscopy according to the method of Teichgräber et al. (19), with slight modifications. Briefly, SAEC-T clones were cultured in glass dishes and then loaded with LysoSensor Green DND-189 (1 μm; Molecular Probes; prepared in PBS) for 10 min at 37 °C. Cells were washed twice with PBS and then cultured in DMM containing 5% FBS for at least 0.5 h to allow the dye to accumulate within acidic vesicles. Cells were treated and cultured as described above in a temperature-controlled chamber set on the stage of a confocal laser scanning microscope (OLYMPUS). Images were taken with a ×100 oil objective lens (NA = 1.4, OLYMPUS), and data were acquired using FV1000 Viewer software (OLYMPUS). The fluorescence intensity of the stained vesicles was measured using FV1000 Viewer software (OLYMPUS). Six different micrographs (each including 5–10 1A5 or 21E5 cells) were used for pH analysis. Captured images were recorded at an excitation wavelength of 473 nm and an emission wavelength of 485–545 nm. After subtracting the background signal, the fluorescence intensity of the pixels of all cells in each micrograph was converted to inherent values for each individual cell using ImageJ, and the average value for each micrograph was used to determine the vesicular pH in 1A5 and 21E5 cells. Simultaneously, standard curves of fluorescence intensity were constructed using cells treated with a series of calibration buffers, namely 10 mm NaCl, 130 mm KCl, 1 mm MgSO4, 10 mm Na-MES, 10 μg/ml nigericin, and 20 μg/ml monensin, which had pH values of 4.5, 5.0, 5.5, 6.0, and 6.5. These calibration buffers can equilibrate the intracellular and extracellular pH values (see Thomas et al. (20)). A pH standard curve was generated by washing cells three times with PBS and then allowing them to equilibrate for 10 min at 37 °C in the calibration buffer. After equilibration, cells were incubated for 10 min at 37 °C with calibration buffer containing 1 μm LysoSensor Green DND-189 (Molecular Probes). Cells were then washed twice with calibration buffer and immediately photographed. The fluorescence intensity of the pixels of all cells in each micrograph was converted to the inherent values, which correspond to the pH value of each individual calibration buffer (pH 4.5–6.5). Six different micrographs (each including 5–10 individual 1A5 or 21E5 clones) were used to prepare standard curves for each individual pH calibration buffer. For flow cytometric analysis of endosomal pH values in the different SAEC-T clones, each clone was labeled with LysoSensor Green DND-189 as described above and carefully removed from the culture plates by trypsinization. CEFs were used as a control. The fluorescence intensity of 10,000 events was measured using a FACSCalibur flow cytometer (BD Biosciences). Data were analyzed using CellQuest software (BD Biosciences).
Imaging of pH-sensitive Endosomes after Endocytosis of Fluorescently Labeled Virus Particles
Virus particles were labeled with R18 as described above. Cells were cultured on glass dishes, washed twice with PBS, and then infected with viruses at an m.o.i. of 3, followed by incubation at 4 °C for 15 min. After removing the viruses and washing twice with PBS, the cells were stained with LysoSensor Green DND-189 (1 μm; Molecular Probes), as described above. Cells were then washed twice with PBS and cultured in DMM containing 5% FBS in a temperature-controlled chamber mounted on the stage of a confocal laser scanning microscope (OLYMPUS). Images were taken with a ×100 oil objective lens (NA = 1.4, OLYMPUS) at 1 h post-infection, and data were acquired using FV1000 Viewer software (OLYMPUS).
Measurement of Endosomal pH Using Fluorescein-labeled Virions
The pH in the endosomes was estimated using fluorescein-labeled virions (F-virions) as described previously (21, 22). Briefly, viral particles were labeled with fluorescein octadecyl ester (Molecular Probes) according to the same method used for R18 labeling. Before viral infection, monolayers of cultured cells were labeled with the cytoplasmic dye CellTrace Far Red (Molecular Probes), according to manufacturer's instructions. Cells were then washed twice with PBS, infected with F-virions at an m.o.i. of 3, and incubated at 4 °C for 15 min. After removing the F-virions and washing twice with PBS, the cells were cultured for 45 min in DMM containing 5% FBS in a temperature-controlled chamber mounted on the stage of a confocal laser scanning microscope (OLYMPUS). Images were taken with a ×100 oil objective lens (OLYMPUS), and the fluorescence intensity of the F-virions was measured using FV1000 Viewer software (OLYMPUS). n = 25 micrographs showing 1A5 or 21E5 cells were used to measure endosomal pH. To determine the pH values, the fluorescence intensity of F-virions was measured in an area measuring 0.5 × 0.5 μm. Images were captured at an excitation wavelength of 473 nm and recorded at an emission wavelength of 485–545 nm. The endosomal pH in the SAEC-T clones was read from a standard curve constructed by treating infected cells with calibration buffers (10 μg/ml nigericin and 20 μg/ml monensin) at a range of pH values (pH 5.0, 5.5, 6.0, 6.5, and 7.0). At least eight micrographs showing cells treated with each pH buffer were used to construct the standard curve.
Virus Infection Inhibition Assay
To examine the effect of increasing endosomal pH on virus infection, 1A5 and 21E5 cells were incubated in DMM containing 5% FBS plus bafilomycin A1 (BafA1) (1.56, 3.125, 6.25, 12.5, and 25 nm; Sigma) for 2 h prior to virus infection. The endosomal pH in cells treated with BafA1 was determined using the pH-sensitive dye, LysoSensor Green DND-189, and a confocal laser scanning microscope (OLYMPUS), as described above. Infection assays were also performed using BafA1-treated cells. After two washes with PBS, cells were infected with Cw/Ky (H5N1) or Dk/Hk (H5N3). The percentage of infected 1A5 and 21E5 cells was determined as described above.
Statistical Analysis
All data are expressed as the mean and standard deviation of at least three determinations per experimental condition. Student's t test (assuming unequal variances) was used for statistical analysis. A p value < 0.05 was considered significant.
RESULTS
Establishment of Human SAEC-T Clones
First, we compared the ability of H5N1 and other AI viruses to infect SAECs. Viral antigens were detected in almost all cells infected with Cw/Ky (H5N1 clade 2.5). By contrast, partial cells were infected with identical titers of Dk/Hk (H5N3) (Fig. 1A). These results implied that SAECs are heterogeneous and show differential susceptibility to AI viruses and that H5N1 shows a broad tropism for epithelial cells. Therefore, to examine the cell populations within primary SAECs and the cellular mechanisms underlying the differences in susceptibility to viral infection, we generated SAEC clones by transforming SAECs with the SV40 large T-antigen (13). Twenty one cell clones (SAEC-Ts) were established, and all showed similar proliferation kinetics in culture (Table 1), although there were slight differences in morphology. The SV40 large T-antigen was stably expressed, even after more than 10 passages (data not shown). Similar to primary SAECs, all SAEC-Ts were cytokeratin (an epithelial cell marker)-positive and MUC5AC (a goblet cell marker)/SCGB1A1 (a Clara cell marker)-negative (data not shown).
FIGURE 1.

Expression of viral antigens in primary human SAECs and SAEC-T clones infected with different viruses. A, primary human SAECs were infected with human influenza virus (Beijing (H1N1)) and H5N1 (Cw/Ky (H5N1)) and previously circulating AI viruses (Dk/Hk (H5N3)) at an m.o.i. of 10. Viral antigens were detected by immunostaining (SEE “Experimental Procedures”) at 16 h post-infection (green). Cells nuclei were counterstained with Hoechst 33342 (blue). Scale bars, 100 μm. B, representative SAEC-T clones (1A5 and 21E5) were infected with H5N1 (Cw/Ky (H5N1)) or previously circulating AI viruses (Dk/Hk (H5N3), rDk/Hk-RRKKR-HA) at an m.o.i. of 10. Viral antigens were detected as described in A (green). Cell nuclei were counterstained with Hoechst 33342 (blue). Scale bars, 200 μm.
TABLE 1.
Categorization of human SAEC-T clones according to their susceptibility to infection by influenza viruses
Infectivity is expressed as follows: ++, 100%; +, ≥30 and <100%; ±, >0 and <30%. H, high susceptibility clones; L, low susceptibility clones.
| Clone namea | Beijing (H1N1) | Cw/Ky (H5N1) | Dk/Hk (H5N3) | Type |
|---|---|---|---|---|
| 1A5b | ++ | ++ | + | H |
| 1E7 | ++ | ++ | + | H |
| 6F1 | ++ | ++ | + | H |
| 7E1 | ++ | ++ | + | H |
| 8A11 | ++ | ++ | + | H |
| 18C10 | ++ | ++ | + | H |
| 19B4 | ++ | ++ | + | H |
| 19F1 | ++ | ++ | + | H |
| 24G5 | ++ | ++ | + | H |
| 30E10 | ++ | ++ | + | H |
| 1C4 | ++ | ++ | ± | L |
| 3A8 | ++ | ++ | ± | L |
| 3C12 | ++ | ++ | ± | L |
| 4A8 | ++ | ++ | ± | L |
| 7C11 | ++ | ++ | ± | L |
| 21D5 | ++ | ++ | ± | L |
| 21E5b | ++ | ++ | ± | L |
| 25H4 | ++ | ++ | ± | L |
| 27E7 | ++ | ++ | ± | L |
| 28E10 | ++ | ++ | ± | L |
| 31H2 | ++ | ++ | ± | L |
a These 21 cell clones all showed similar proliferation kinetics in culture.
b 1A5 and 21E5 clones were used for further analysis as examples of high (1A5) and low (21E5) susceptibility clones.
Characterization of SAEC-T Clones According to Susceptibility to Infection by Influenza Viruses
To evaluate the susceptibility of each SAEC-T clone to infection by influenza viruses, we exposed them to H5N1 (Cw/Ky (H5N1)), a low pathogenic AI virus (Dk/Hk (H5N3)), or human influenza virus Beijing (H1N1) (used as the control). All SAEC-Ts were susceptible to infection by Cw/Ky (H5N1) and Beijing (H1N1) (100% infection rate, see Table 1). Dk/Hk (H5N3) showed a moderate infection rate (30–99%) in 10 of the 21 SAEC-T clones and a marginal infection rate (1–29%) in the remainder. Thus, SAEC-T clones were categorized as either high or low susceptibility clones on the basis of their susceptibility to Dk/Hk (H5N3) (high, ≥30% infected; and low, <30% infected) (Table 1). Two clones were selected as examples of high (1A5) and low (21E5) susceptibility clones (Fig. 1B) for further examination.
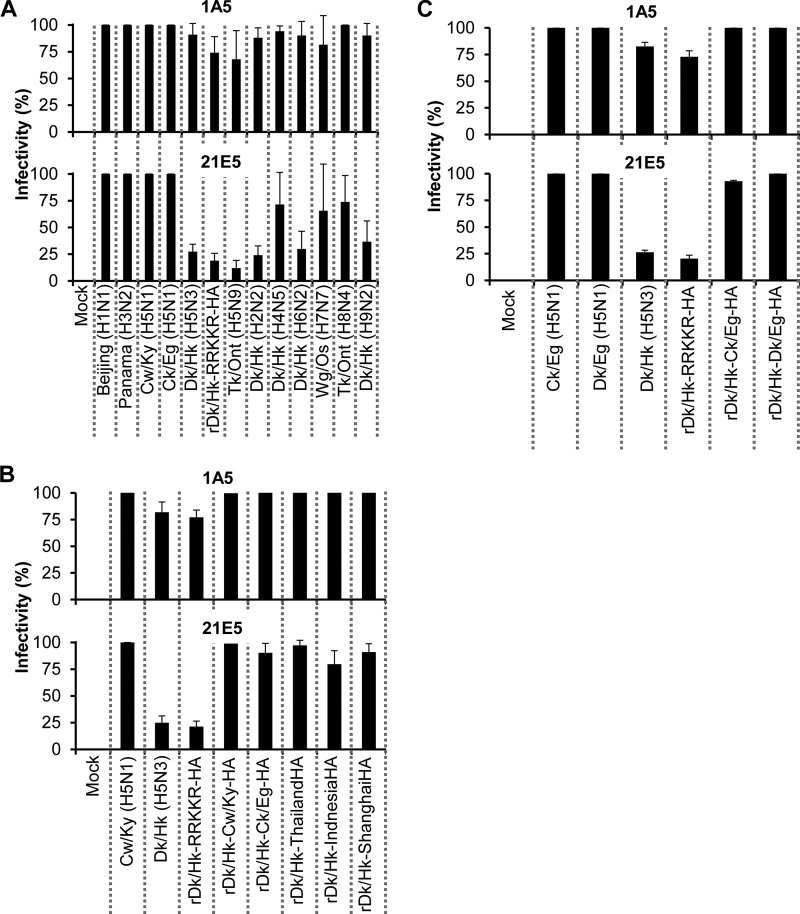
Next, we examined whether clones 1A5 and 21E5 were susceptible to infection by other classical AI viruses. 1A5 and 21E5 were infected with Dk/Hk (H2N2), Dk/Hk (H4N5), Tk/Ont (H5N9), Dk/Hk (H6N2), Wg/Os (H7N7), Tk/Ont (H8N4), and Dk/Hk (H9N2). Clones 1A5 and 21E5 showed moderate and low susceptibility to infection by AI viruses, respectively (Fig. 2A). By contrast, the clones showed high susceptibility to another H5N1 strain, Ck/Eg (H5N1), and to human influenza virus Panama (H3N2) (Fig. 2A). These results suggested that human influenza viruses broadly infect human airway epithelial cells; however, AI viruses could only infect specific cell clones, whereas H5N1 infected all SAEC-T clones.
FIGURE 2.
Susceptibility of human SAEC-T clones to infection by different influenza virus strains. A, high (1A5) and low (21E5) susceptibility clones were infected with human influenza (Beijing (H1N1), Panama (H3N2)), H5N1 (Cw/Ky (H5N1), and Ck/Eg (H5N1)) and previously circulating AI viruses (Dk/Hk (H5N3), rDk/Hk-RRKKR-HA, Tk/Ont (H5N9), Dk/Hk (H2N2), Dk/Hk (H4N5), Dk/Hk (H6N2), Wg/Os (H7N7), Tk/Ont (H8N4), and Dk/Hk (H9N2)) at an m.o.i. of 10. Viral infectivity was determined by calculating the percentage of antigen-positive SAEC-T clones after immunostaining at 16 h post-infection. Data are expressed as the mean ± S.D. of more than three independent experiments. B, high susceptibility clone (1A5) and low susceptibility clone (21E5) were infected with recombinant H5N3 (rDk/Hk-Cw/Ky-HA, rDk/Hk-Ck/Eg-HA, rDk/Hk-ThailandHA, rDk/Hk-IndonesiaHA, or rDk/Hk-ShanghaiHA) viruses containing the HA gene from H5N1 (A/crow/Kyoto/53/04 (clade 2.5), A/chicken/Egypt/CL6/07 (clade 2.2.1), A/Thailand/Kan353/04 (clade 1), A/Indonesia/5/05 (clade 2.1.3), or A/Shanghai/1/06 (clade 2.3.4)) at an m.o.i. of 10. Viral infectivity was determined as described in A. Data are expressed as the mean ± S.D. of three independent experiments. C, high susceptibility clone (1A5) and the low susceptibility clone (21E5) were infected with recombinant Dk/Eg (H5N1) (clade 2.2.1), which shows very high amino acid homology (HA, NP, M1, M2, NS2: 100%; another gene: >99.46%) to the H5N1 human isolate A/Egypt/902786/2006 (H5N1) (clade 2.2.1) and with recombinant H5N3 (rDk/Hk-Dk/Eg-HA) viruses containing the HA gene from A/Egypt/902786/2006 (H5N1) at an m.o.i. of 10. Viral infectivity was determined as described in A. Data are expressed as the mean ± S.D. of three independent experiments. The amino acid homology of Ck/Eg (H5N1) (clade 2.2.1) to the human influenza virus A/Egypt/902786/2006 (H5N1) is as follows: M1, M2, and NS1, 100%; another gene, >99.46%.
A multibasic amino acid motif within the HA cleavage site is associated with the high virulence of HPAI viruses in both birds and mammals (23, 24). To examine whether differences in the sequences at the HA cleavage sites in Cw/Ky (H5N1) and Dk/Hk (H5N3) contribute to their differing ability to infect 1A5 and 21E5 cells, we examined the susceptibility of the two clones to a recombinant H5N3 virus harboring multiple basic sequences derived from Cw/Ky (H5N1) (N′-RRKKR-C') within the HA cleavage site (rDk/Hk-RRKKR-HA). As shown in Figs. 1B and 2A, both rDk/Hk-RRKKR-HA and wild-type Dk/Hk (H5N3) infected 21E5 and 1A5 cells to a similar extent, suggesting that the multiple basic amino acid sequences within H5N1 HA are not responsible for its ability to infect SAEC-T.
By contrast, a recombinant Dk/Hk virus harboring H5N1 HA genes from avian Cw/Ky (clade 2.5) and Ck/Eg (clade 2.2.1) (denoted here as rDk/Hk-Cw/Ky-HA and rDk/Hk-Ck/Eg-HA, respectively) or H5N1 HA genes from human A/Thailand/Kan353/04 (clade 1), A/Indonesia/5/05 (clade 2.1.3), or A/Shanghai/1/06 (clade 2.3.4) (denoted here as rDk/Hk-ThailandHA, rDk/Hk-Indonesia, and rDk/Hk-ShanghaiHA, respectively) showed broad infectivity (similar to Cw/Ky (H5N1)) (Fig. 2B). Furthermore, a recombinant Dk/Hk virus carrying H5N1 HA genes from Dk/Eg (H5N1) (clade 2.2.1) (denoted here as rDk/Hk-Dk/Eg-HA) also showed broad infectivity (similar to a recombinant Dk/Eg (H5N1), which shows very high amino acid homology (HA, NP, M1, M2, NS2: 100%; another gene >99.46%) to the H5N1 human isolate A/Egypt/902786/2006 (H5N1) (clade 2.2.1)) (Fig. 2C). These results suggest that the H5N1 HA protein confers the ability to broadly infect SAECs.
We also examined the expression of α2,3SA and α2,6SA residues on SAEC-Ts by flow cytometry. The results showed that α2,6SA and α2,3SA were expressed on all SAEC-T examined and that the levels were comparable with those on the surface of MDCK cells (Fig. 3).
FIGURE 3.
Receptor expression by human SAEC-T clones. Expression of SA receptors on high (1A5) and low (21E5) susceptibility human SAEC-T clones was analyzed by flow cytometry. α2,3SA (solid line) and α2,6SA (dotted line) receptors were detected using FITC-conjugated Maackia amurensis (MAA)-FITC and Sambucus nigra (SNA)-FITC lectins, respectively. Control cells (without lectin) are shown as a bold line. MDCK cells (viral susceptible controls) express both α2,3SA and α2,6SA receptors. MDCK, 1A5, and 21E5 cells were treated with neuraminidase to confirm the reliability of lectin staining.
Binding and Internalization of Viruses by Human SAEC-T Clones
We next examined the mechanism underlying the ability of H5N1 to broadly infect SAEC-Ts. First, we examined the cell binding ability of two H5N1 strains, Cw/Ky (H5N1) and Ck/Eg (H5N1), and two AI viruses, rDk/Hk-RRKKR-HA and Tk/Ont (H5N9). SAEC-Ts (clones 1A5 and 21E5 (1.0 × 105 cells)) were infected at an m.o.i. of 10 (see “Experimental Procedures”), lysed, and then immunoblotted with an anti-influenza polyclonal antibody (which recognizes the M1 conserved region) (Fig. 4). There was no significant difference in the number of H5N1 or other virions bound to the surface of 1A5 or 21E5 cells (Fig. 4, A, right panel, and B, right panel). Even H5 viruses (rDk/Hk-RRKKR-HA and Tk/Ont (H5N9)), which showed low infectivity, bound to 1A5 and 21E5 cells. The amount of rDk/Hk-RRKKR-HA and Tk/Ont (H5N9) bound to 21E5 cells (which showed low susceptibility to previously circulating H5 viruses) was similar to that of the currently circulating H5N1 virus (Cw/Ky (H5N1)). The amount of bound Beijing (H1N1) particles was comparable with that of previously circulating AI viruses (Fig. 4, A, right panel, and B, right panel).
FIGURE 4.
Analysis of viral binding and internalization by human SAEC-T clones. A, virus binding to human SAEC-T clones was analyzed by Western blotting. 1A5 and 21E5 cells (1.0 × 105) were infected with human influenza (Beijing (H1N1)), H5N1 (Cw/Ky (H5N1), or Ck/Eg (H5N1)) and previously circulating AI viruses (rDk/Hk-RRKKR-HA or Tk/Ont (H5N9)) at an m.o.i. of 10. Purified virions were used as a detection limit control (left panel). Cells were infected with viruses for 1 h at 4 °C and harvested immediately. The viral M1 protein was detected with an anti-H5N2 polyclonal antibody. The relative intensity of the bands representing each viral protein was measured using ImageJ. The intensities of Cw/Ky (H5N1) viral proteins in individual membranes were set to 1 (see also B). B, summary of the relative intensities of the viral protein (M1) bands shown in A. C and D, viral internalization was analyzed by confocal imaging of live virus-infected human SAEC-T cells. High (1A5) (C) and low (21E5) (D) susceptibility clones were infected with R18-labeled Cw/Ky (H5N1) or rDk/Hk-RRKKR-HA viruses at an m.o.i. of 3 and virus internalization monitored using time-lapse confocal imaging. The arrow indicates R18-labeled virus (red). The cytoplasm was stained simultaneously with CellTracker Green 5-chloromethylfluorescein diacetate. Nuclei were counterstained with Hoechst 33342 (blue). Left panels, z stack projection of confocal images. Right panels, side-on view of z stacks. Scale bars, 10 μm.
We next focused on viral internalization, which was visualized by labeling viral particles with a fluorescent dye. The labeled Cw/Ky (H5N1) and rDk/Hk-RRKKR-HA virions entered 1A5 cells within 1 h (Fig. 4C). In addition, both virions entered 21E5 cells with similar kinetics (Fig. 4D). These results suggest that both currently circulating H5N1 and previously circulating AI viruses use the same internalization pathway.
Effect of pH on H5N1-Membrane Fusion
We next examined the virus-membrane fusion step, which is triggered by the mildly acidic pH within the endosomal lumen after internalization. MDCK cells were transfected with HA expression plasmids and were used in a cell-to-cell fusion assay (25). The highest pH at which viruses showed fusogenic activity was measured, and the pH threshold was determined. The results showed that the pH threshold for H5N1 viruses (Cw/Ky (H5N1), Ck/Eg (H5N1), Indonesia (H5N1), and Shanghai (H5N1)) was 5.625 (the exception was Thailand (H5N1) (pH 5.75)), whereas that of the AI viruses (Dk/Hk (H2N2), Dk/Hk (H4N5), Dk/Hk (H5N3), rDk/Hk-RRKKR-HA, Tk/Ont (H5N9), and Dk/Hk (H6N2)) was pH 5.125–5.375 (the exceptions were Tk/Ont (H8N4) and Wg/Os (H7N7) (pH 5.5)) (Fig. 5, A, B and E). These results suggest that H5N1-HA genes have a high pH threshold for HA-mediated membrane fusion compared with that of other AI viruses. The pH threshold for each virus corresponded well to that in MDCK cells infected with each virus (Fig. 5, C–E).
FIGURE 5.
Virus-membrane fusion at low pH in MDCK cells. A, MDCK cells were transfected with the influenza virus HA gene from different H5N1 viruses (Cw/Ky (H5N1), Ck/Eg (H5N1), A/Thailand (H5N1), Indonesia (H5N1), and Shanghai (H5N1)) or with the HA gene from previously circulating AI viruses (Dk/Hk (H2N2), Dk/Hk (H4N5), Dk/Hk (H5N3), rDk/Hk-RRKKR-HA, Tk/Ont (H5N9), Dk/Hk (H6N2), Wg/Os (H7N7), or Tk/Ont (H8N4)). Fusion induction at pH 5.0–5.875 was measured at 24 h post-transfection. Representative fields of cells transfected with each of the indicated viruses and exposed to pH 5.125–5.875 are shown. Red squares show polykaryon formation. Micrographs lacking a red square represent a pH above the fusion threshold. Values in red indicate the pH threshold of HA membrane fusion. The pH threshold was determined as described under “Experimental Procedures.” Scale bars, 200 μm. B, efficiency of polykaryon formation over a pH range of 5.0–5.875 was estimated by dividing the number of nuclei in polykaryons by the total number of nuclei in the same field. Data represent the mean ± S.D. from more than three independent cell culture experiments. C, MDCK cells were infected with H5N1 viruses (Cw/Ky (H5N1) and Ck/Eg (H5N1)), or previously circulating AI viruses (Dk/Hk (H5N3), rDk/Hk-RRKKR-HA, Tk/Ont (H5N9), Dk/Hk (H2N2), Dk/Hk (H4N5), Dk/Hk (H6N2), Wg/Os (H7N7), Tk/Ont (H8N4), or Dk/Hk (H9N2)) at an m.o.i. of 1. At 8 h post-infection, fusion formation over a pH range of 5.0–5.875 was estimated. Representative fields showing cells infected with each of the indicated viruses and exposed to pH 5.0–5.75. Red squares show polykaryon formation. Micrographs lacking a red square represent a pH above the fusion threshold. pH values in red indicate the pH threshold for HA membrane fusion. pH thresholds were determined as described under “Experimental Procedures.” Scale bars, 200 μm. D, efficiency of polykaryon formation over a pH range of 5.0–5.875 was estimated by dividing the number of nuclei in the polykaryons by the total number of nuclei in the same field. Data are expressed as the mean ± S.D. from more than three independent experiments. E, summary of the pH thresholds for membrane fusion for all viral subtypes in transfected cells and infected cells.
No cell-to-cell fusion was observed in cells infected with Dk/Hk (H9N2) (Fig. 5C) over the pH range tested (5.0–5.875). In this study, the culture medium used for the fusion assays included trypsin as the only protease to mediate HA protein cleavage, suggesting that HA cleavage in Dk/Hk (H9N2) requires another protease (e.g. human airway trypsin-like protease or TMPRSS2) (26).
Endosomal pH in High and Low Susceptibility SAEC-T Clones
After internalization, influenza viruses are trafficked to late endosomes, where the acidic environment triggers HA-mediated membrane fusion and delivery of the viral genome to the cytoplasm (27–29). Thus, we hypothesized that differences in late endosomal pH values may define susceptibility to viral infection. We measured the actual late endosomal pH values in representative high (1A5) and low (21E5) susceptibility clones using LysoSensor Green DND-189, which accumulates in acidic organelles (e.g. late endosomes and lysosomes) and emits green fluorescence at low pH (19, 30, 31). Confocal microscopy (Fig. 6A, upper panels) and flow cytometry (Fig. 6B) showed that the fluorescence intensity in many vesicles within 1A5 cells was higher than that within 21E5 cells. Other high and low susceptibility cell clones showed similar results (data not shown). High levels of fluorescence were also seen in control CEFs (Fig. 6B), which are also susceptible to virus infection.
FIGURE 6.
pH levels in the vesicles within high and low susceptibility SAEC-T clones. A, high (1A5) and low (21E5) susceptibility cell clones were treated with PBS (upper micrographs, n = 6 micrographs) or calibration buffer (pH 4.5–6.5) (lower micrographs, representative fluorescence images (each micrograph is representative of six individual micrographs per pH value)) and then stained with LysoSensor Green DND-189. Cells were then examined under a confocal microscope. Scale bars, 20 μm. B, stained 1A5 and 21E5 cells were also analyzed by flow cytometry. The profiles of the stained cells are shown as black (1A5) and gray (21E5) lines. Stained CEFs, which are susceptible to AI viruses, are represented by a black line. Control cells (no staining) are represented by bold lines. C, high (1A5) and low (21E5) susceptibility clones were infected with R18-labeled rDk/Hk-RRKKR-HA at an m.o.i. of 10. Immediately after infection, cells were stained with LysoSensor Green DND-189 or LysoTracker Green DND-26 and examined under a confocal microscope. Representative images are shown. Confocal microscopy was used to observe virus localization in infected 1A5 and 21E5 clones (white arrows). Virus particles within vesicles are yellow (merged particles). Upper panels, Z stack projection of confocal images. Lower panels, Z stacks viewed side-on from the dashed line. Scale bars, 10 μm. D, number of virus particles (red and yellow) and merged particles (yellow) is shown. Data are expressed as the mean ± S.D. (n = 10 cells). **, p < 0.01, significantly different from the number of virus particles in the 21E5 clone. E, standard curve constructed using 1A5 and 21E5 clones treated with calibration buffer (pH 4.5–6.5) and stained with LysoSensor Green DND-189 (based on the staining intensity of the calibration buffer-treated cells shown in A). Six micrographs per individual pH value were used to construct the standard curve. F, constitutive vesicular pH value in 1A5 and 21E5 clones calculated from the standard curve. The data are expressed as the mean ± S.D. (based on six individual micrographs for each pH measurement). **, p < 0.01, significantly different from the vesicular pH value in the 21E5 clone.
We then examined the co-localization of internalized virions with late endosomes in 1A5 or 21E5 cells. Cells were infected with rDk/Hk-RRKKR-HA particles labeled with octadecyl rhodamine B (R18) and then treated with LysoSensor Green DND-189 or LysoTracker Green DND-26, which accumulates in acidic organelles and emits green fluorescence regardless of pH (32). Micrographs of DND-189- or DND-26-treated 1A5 and 21E5 cells (10 cells per group) infected with labeled viruses were obtained, and the number of particles was counted. The number of intracellular particles in DND-189-treated 1A5 cells was comparable with that in 21E5 cells; however, the number of merged particles (yellow) was significantly higher in 1A5 cells than in 21E5 cells (Fig. 6, C, left panel, and D, upper panel). By contrast, there was no significant difference in the number of merged particles in stained vesicles within 1A5 and 21E5 cells treated with DND-26 (Fig. 6, C, right panel, and D, lower panel). Taken together, these results suggest that late endosomes (containing virus particles) in 1A5 cells were more acidic than those in 21E5 cells.
The endosomal pH difference between the two clones was also confirmed by measuring endosomal pH after internalization of influenza viral particles (21, 22) fluorescently labeled with fluorescein octadecyl ester. The fluorescence (green) intensity of F-virions within the endosome becomes weaker as the pH falls. Confocal imaging revealed that F-virions in 1A5 cells showed weaker fluorescence intensity than those in 21E5 cells (Fig. 7A), indicating that the endosomal pH was lower in 1A5 cells than in 21E5 cells. To determine the pH of endosomes containing virions, we measured the fluorescence intensity of the F-virions. The endosomal pH of cells inoculated with rDk/Hk-RRKKR-HA was read off a standard curve (Fig. 7, B–D) (for details, see “Experimental Procedures”). The average deduced endosomal pH values in 1A5 and 21E5 cells was 5.01 and 5.66 (Fig. 7), respectively, which are almost identical to the values estimated in the DND-189 assay (pH 5.13 and 5.62, respectively) (Fig. 6, A, E and F; see “Experimental Procedures” for details). This pH range (pH 5.01–5.66) corresponded with that required for H5N1HA membrane fusion (Fig. 5).
FIGURE 7.
Endosomal pH levels in high and low susceptibility SAEC-T clones. A, high (1A5) and low (21E5) susceptibility clones were infected with fluorescein-labeled rDk/Hk-RRKKR-HA (white arrows) at an m.o.i. of 3, followed by analysis under a confocal microscope 45 min later. Six representative fluorescence images are shown (from a total of n = 25 micrographs). The cytoplasm was stained simultaneously with CellTrace Far Red (dark blue). Insets show images at higher magnification. Scale bars, 10 μm. B, 1A5 and 21E5 cells were infected with fluorescein-labeled rDk/Hk-RRKKR-HA (white arrows) at an m.o.i. of 3. Immediately after infection, the cells were treated with different calibration buffers (pH 5.0–7.0) and analyzed under a confocal microscope. Five representative fluorescence images are shown (from a total of n = 8 or 9 micrographs showing cells in different pH calibration buffers). The cytoplasm was stained simultaneously with CellTrace Far Red (dark blue). Insets show images at higher magnification. Scale bars, 10 μm. C, standard curve for the fluorescence intensity of fluorescein-labeled rDk/Hk-RRKKR-HA in 1A5 and 21E5 clones was constructed by treating the cells with different calibration buffers (pH 5.0–7.0). At least eight different cells from each micrograph at each individual pH were used to construct the standard curve. D, pH values in the vesicles within 1A5 and 21E5 cells were read off the standard curve. Data are expressed as the mean ± S.D. Each pH measurement in 1A5 and 21E5 cells was based on n = 25 micrographs. **, p < 0.01, significantly different from the vesicular pH value in the 21E5 clone.
Viral Infectivity Is Regulated by Changes in Endosomal pH
The different endosomal pH values observed in high (1A5) and low (21E5) susceptibility clones prompted us to examine the relationship between viral infection and host endosomal pH levels. To this end, we effected changes in endosomal pH using the specific reagent BafA1, which increases endosomal pH via its vacuolar-type H+-ATPase activity. Thus, the reagent prevents endosomal acidification and traps influenza viruses within immature endosomes (33).
BafA1 reduced the acidity in 1A5 and 21E5 endosomes in a dose-dependent manner (Fig. 8A). We calculated the pH of the endosomes in BafA1-treated cells (1A5 and 21E5) using the standard curve for fluorescence intensity generated using LysoSensor Green DND-189-stained cells (Fig. 6E). BafA1 increased the endosomal pH from 5.13 (0 nm) to 6.37 (25 nm) in 1A5 cells and from 5.62 (0 nm) to 6.35 (25 nm) in 21E5 cells (Fig. 8B). Furthermore, BafA1 treatment (minimum 1.56 nm) of 1A5 cells markedly inhibited Dk/Hk (H5N3) replication. However, BafA1 treatment did not inhibit the growth of Cw/Ky (H5N1) in 1A5 cells, even at 3.125 nm. Higher doses of BafA1 (≥6.25 nm) increased the endosomal pH in 1A5 cells to more than 5.95 and inhibited the growth of Cw/Ky (H5N1) (Fig. 8C). By contrast, lower doses of BafA1 (1.56 nm) increased the endosomal pH in 21E5 cells to 5.83 and inhibited the growth of Cw/Ky (H5N1) (Fig. 8C). Dk/Hk (H5N3) did not replicate well in 21E5 cells in the presence or absence of BafA1 (see Figs. 2 and 8C). These results suggest that the pH within the endosomes in SAEC-Ts plays a role in their differing susceptibility to infection by H5N1 and other AI viruses.
FIGURE 8.
BafA1 inhibits virus infectivity. A, high (1A5) and low (21E5) susceptibility clones were treated with BafA1 (1.56–25 nm) and then stained with LysoSensor Green DND-189. Clones were then analyzed under a confocal microscope. Representative fluorescence images are shown (n = 6 micrographs per individual reagent concentration (except for the group treated with 3.125 nm BafA1 (n = 5 micrographs)). Scale bars, 20 μm. B, vesicular pH values in 1A5 and 21E5 clones treated with BafA1 (1.56–25 nm) were calculated from standard curves as described in Fig. 6E. Vesicular pH values in 1A5 and 21E5 clones not treated with BafA1 are shown for comparison (taken from Fig. 6F). Data are expressed as the mean ± S.D. (based on six individual micrographs). C, high (1A5) and low (21E5) susceptibility clones were treated with BafA1 (0–25 nm) for 2 h and then simultaneously infected with Cw/Ky (H5N1) or Dk/Hk (H5N3) at an m.o.i. of 10. Twelve hours later, infectivity was determined by calculating the percentage of antigen-positive SAEC-T cells as described in Fig. 2. Representative micrographs of antigen-positive cells treated with BafA1 are shown. Cell nuclei were also counted. Data are expressed as the mean ± S.D. of three independent experiments. The deduced endosomal pH for each cell clone (1A5 and 21E5) was taken from B. Scale bars, 200 μm.
DISCUSSION
Here, we show the following: (i) SAEC-T clones derived from human bronchiolar epithelia could be broadly classified into two groups (high and low) based on their susceptibility to H5N1 and other AI viruses; (ii) the H5N1 HA protein showed a broader tropism for SAEC-Ts and showed membrane fusion activity at higher pH values than previously circulating AI viruses; and (iii) the pH value within the endosomes of high susceptibility SAEC-T clones was low, but in low susceptibility clones it was high. The pH in endosomes correlated well with the susceptibility of a cell to AI viruses.
In contrast to other classical AI viruses, H5N1 infected all primary SAECs and low susceptibility SAEC-Ts tested. Also, a recombinant H5N3 virus expressing H5N1-HA showed a tropism similar to that of the parental H5N1 virus; however, a recombinant H5N3 virus expressing the multiple basic amino acid sequence from H5N1 within its HA (rDk/Hk-RRKKR-HA) did not show altered cell tropism. These results suggest that the H5N1-HA protein plays a critical role in the broad tropism for SAECs. The HA protein plays a crucial role in the early replication of influenza viruses (29); therefore, we focused on this phase of the viral replication cycle when examining the molecular mechanism(s) underlying the distinct susceptibilities of SAEC-T clones to AI viruses.
Surface binding analysis showed that H5N1, H5N3, and H5N9 bound comparably to both high susceptibility (1A5) and low susceptibility (21E5) SAEC-Ts. In addition, confocal microscopy revealed that H5N3 showed similar internalization kinetics to H5N1. These results suggest that an event(s) occurring after virus binding and internalization is associated with the differences in infectivity between H5N1 and H5N3 viruses.
After viral internalization via endocytosis, influenza viruses establish infection by fusion between viral and endosomal membranes as a result of a low pH-dependent conformational change in HA (34–39). Some residues must be protonated to activate the HA conformational change in a low endosomal pH because protonated residues can affect salt bridges or hydrogen bonds within each HA domain. Therefore, in many cases, basic residues such as histidine can act as a pH sensor to induce the HA conformational change for virus-cell membrane fusion (40–42). The cell fusion assay revealed that the fusogenic activity of H5N1 viruses occurred at pH 5.625–5.75, which was higher than that for other AI viruses (pH 5.125–5.375); the exceptions were Wg/Os (H7N7) (pH 5.25–5.5) and Tk/Ont (H8N4) (pH 5.5). Galloway et al. (43) reported that the pH threshold for HA membrane fusion in A/Vietnam/1204/2004 (H5N1) was higher (pH 5.6) than that for other AI viruses (pH 5.1–5.5), although some non-H5 AI viruses showed a similar pH threshold to that of the H5N1 viruses (and slightly higher than that of the previously circulating AI strains examined in this study (mostly pH 5.125–5.375)). The results of this study, together with those of Galloway et al. (43), suggest that the ability of classical avian viruses to show fusogenic activity at relatively low pH levels may be advantageous, allowing the virus to survive within the host bird. AI viruses target the intestinal tissues in birds (2, 44); thus, the balance between intestinal pH and viral acid stability is likely to be important for viral persistence. The pH of the contents of the avian intestine is around 5.23–6.73 (45, 46). Based on these values, classical AI viruses showing fusogenic activity at low pH (5.125–5.375) are acid-stable, which allows them to persist in the avian intestine, whereas H5N1 viruses may be attenuated due to their lower acid stability and fusogenic activity at higher pH levels (5.625–5.75). The duck intestine is mildly acidic (45), reflecting the fact that waterfowl act as a reservoir for all AI subtypes (47, 48). Despite the fact that H5N1 HA is vulnerable to acidic conditions, H5N1 viruses continue to cause influenza outbreaks in poultry in central Asia, Europe, the Middle East, and Africa (49). This discrepancy raises questions about H5N1 infection in birds. The gastrointestinal contents (proteins, lipids, or carbohydrates) might protect the viral HA protein, allowing H5N1 to remain infectious. Another possibility is that pH changes in the intestinal lumen of H5N1-infected birds could contribute to viral persistence. If virus-infected cells are efficiently destroyed by H5N1, blood is released into the intestinal lumen, thereby increasing the pH. A similar phenomenon is observed in bovine mastitis, in which bacterial infection damages the blood-milk barrier resulting in increased pH values in milk (50). We previously reported that H5N1 viruses induce apoptosis in duck embryonic fibroblasts and mammalian airway epithelial cells (10, 51), supporting the hypothesis that luminal pH changes occur in the intestine of H5N1-infected birds.
However, although H5N1HA may be vulnerable to low pH, this vulnerability may support efficient viral infection once H5N1 enters the target cell. During viral internalization via endocytosis, virions are exposed to reduced pH within the endosomal compartment. When the pH reaches a threshold value, virus-cell membrane fusion occurs, and the viral genome is liberated into the cytoplasm, resulting in viral infection (22, 27, 29). The present results, together with those of Galloway et al. (43), indicate that the H5N1-HA protein adopts its fusogenic form when the endosomal pH is high, whereas the HA proteins of other AI viruses do so at lower pH levels. Two recent studies show that HA membrane fusion at a higher pH is associated with the virulence of AI viruses. The sensitivity of membrane fusion to different pH values alters the virulence of H5N1 viruses in birds (25, 52). Taken together with the results reported herein, these reports lead us to surmise that early uncoating and liberation of the viral genome at high pH can enable the virus to leave the endosome quickly and escape transportation to the lysosomal compartment. Recently, Imai et al. (53) reported that human-to-human transmission of AI virus requires that the HA protein must show a certain level of acid stability and recognize human receptors; this is because the human nasal mucosa is relatively acidic (approximately pH 5.5–6.9) (54, 55). Taken together with the results of this study, this suggests that viral infectivity and transmissibility are independent of each other. Therefore, in the case of bird-to-human transmission, in which viral particles that bypass the acidic nasal cavity cause infection, a higher pH threshold for membrane fusion seems to allow efficient viral infection of the lower respiratory tract.
Thus, it seems that the pH in the endosomes of the high susceptibility clone, 1A5, is more conducive to influenza fusogenic activity than that in the endosomes of the low susceptibility clone, 21E5. The endosomal pH in 1A5 cells was 5.01 ± 0.94 to 5.13 ± 0.10 (value ± S.D.) and that in 21E5 cells was 5.62 ± 0.10 to 5.66 ± 0.76 (value ± S.D.). The lower endosomal pH in 1A5 cells reaches the pH threshold for fusogenic activity for all influenza viruses tested in this study. In contrast, the endosomal pH in 21E5 cells reaches the pH threshold for H5N1 but not for previously circulating AI viruses. Thus, cell susceptibility to influenza viruses depends on a delicate balance between endosomal pH and the pH threshold for fusogenic activation for each viral strain.
Early and late endosomes within cell lines or primary cells derived from different species and/or tissues have inherently different pH values (5.9–6.5 and 5.0–6.0, respectively) (21, 56, 57). Representative pH values in the early and late endosomes of some cell lines and primary cultured cells are known (21, 22, 56, 58–64). In these reports and this study, MDCK, CEFs, and 1A5 cells, which have lower endosomal pH values, are all susceptible to infection by influenza viruses. Thus, it would be interesting to determine whether cell lines with higher endosomal pH values are more susceptible to influenza viruses after the endosomal pH is reduced by drug treatment. Further studies are needed to determine whether virus-cell membrane interactions in endosomes are important for the infectivity of other enveloped viruses. Robbins et al. (65) reported that CHO mutants were pleiotropically defective in endocytosis, and Yamashiro and Maxfield (56) showed that the endosomal pH in mutant DTF-1-5-1 and wild-type CHO cells (normal endocytosis) is 5.6 and 5.2, respectively. Overly et al. (66) also reported endosomal pH heterogeneity among primary cultured chicken sympathetic neurons. Thus, the endosomal pH in closely related cell clones may vary, supporting our findings that histologically similar epithelial cells (1A5 and 21E5) contain endosomes with different pH levels. This study is the first to show that endosomal pH is heterogeneous among human airway epithelial cells that have different susceptibilities to AI viral infection. The physiological heterogeneity of SAECs may arise because they comprise either cell types of different origin or the same cell type at different stages of differentiation. Along with Clara cells, basal and parabasal cells (stem cells) within the human airway epithelia play important roles in ciliated epithelial cell renewal (67–69). Therefore, these cell types (which are of different origin) may show differing susceptibility to viral infection. Moreover, the differences in endosomal pH among mammalian cells leads us to speculate that endosomal pH levels may vary between the upper and lower respiratory tracts. Further studies should compare endosomal pH levels in epithelial cells that line the lower and upper human airway. From a physiological point of view, different endosomal pH values in different cells may help to defend tissues against some pathogens, including enveloped viruses and toxins that can be activated in a low pH environment. Therefore, it will be interesting to examine the correlation between the cellular endosomal pH values in host animals and the pH sensitivity of pathogens that infect them.
It is still unclear why H5N1 viruses are directly transmitted from birds to humans. Here, we provide evidence that a delicate balance between the pH sensitivity of the viral HA protein and the pH within the endosomal compartment of the target cell regulates infection by AI viruses, including currently circulating H5N1 viruses. In addition, we showed that the pathogenesis of H5N1 in humans results from its broad tropism for human airway epithelial cells, which comprise histologically similar but biologically distinct cells that contain endosomes with different pH levels. Further studies should perform phylogenetic analysis of currently circulating H5N1 viruses to identify the amino acid sequences responsible for virus-cell membrane fusion at higher pH values.
Acknowledgments
We thank Drs. Ritsuko Koketsu, Yukihiro Akeda, and Yusuke Maeda (Research Institute for Microbial Diseases, Osaka University) for helpful advice. We are grateful to Dr. Takeshi Onodera and Dr. Akikazu Sakudo (University of Tokyo, Japan) for supplying recombinant retrovirus encoding the SV40 large T-antigen. We also thank Dr. Yoshinobu Okuno (Kanonji Institute, the Research Foundation for Microbial Diseases of Osaka University, Kagawa, Japan) for providing viruses and for helpful discussion.
This work was supported by Grants-in aid for Scientific Research 22790953, 24591480, 24659482, and 23406033 from the Ministry of Education, Culture, Sports, Science and Technology.
- AI
- avian influenza
- SAEC
- small airway epithelial cell
- SA
- sialic acid
- BafA1
- bafilomycin A1
- MDCK
- Madin-Darby canine kidney cell
- m.o.i.
- multiplicity of infection
- CEF
- chicken embryonic fibroblast.
REFERENCES
- 1. World Health Organization (2013) Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO. www.who.int/influenza/human_animal_interface/EN_GIP_20131210CumulativeNumberH5N1cases.pdf
- 2. Ito T., Couceiro J. N., Kelm S., Baum L. G., Krauss S., Castrucci M. R., Donatelli I., Kida H., Paulson J. C., Webster R. G., Kawaoka Y. (1998) Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J. Virol. 72, 7367–7373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shinya K., Ebina M., Yamada S., Ono M., Kasai N., Kawaoka Y. (2006) Avian flu: influenza virus receptors in the human airway. Nature 440, 435–436 [DOI] [PubMed] [Google Scholar]
- 4. van Riel D., Munster V. J., de Wit E., Rimmelzwaan G. F., Fouchier R. A., Osterhaus A. D., Kuiken T. (2006) H5N1 virus attachment to lower respiratory tract. Science 312, 399. [DOI] [PubMed] [Google Scholar]
- 5. Fouchier R. A., Schneeberger P. M., Rozendaal F. W., Broekman J. M., Kemink S. A., Munster V., Kuiken T., Rimmelzwaan G. F., Schutten M., Van Doornum G. J., Koch G., Bosman A., Koopmans M., Osterhaus A. D. (2004) Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc. Natl. Acad. Sci. U.S.A. 101, 1356–1361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Xu C., Havers F., Wang L., Chen T., Shi J., Wang D., Yang J., Yang L., Widdowson M. A., Shu Y. (2013) Monitoring avian influenza A (H7N9) virus through national influenza-like illness surveillance, China. Emerg. Infect. Dis. 19, 1289–1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ilyushina N. A., Ikizler M. R., Kawaoka Y., Rudenko L. G., Treanor J. J., Subbarao K., Wright P. F. (2012) Comparative study of influenza virus replication in MDCK cells and in primary cells derived from adenoids and airway epithelium. J. Virol. 86, 11725–11734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang X. Y., Guckian M., Nasiri N., Lovell P. A., Dalgleish A. G., Barton D. P. (2002) Normal and SV40 transfected human peritoneal mesothelial cells produce IL-6 and IL-8: implication for gynaecological disease. Clin. Exp. Immunol. 129, 288–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chapdelaine P., Kang J., Boucher-Kovalik S., Caron N., Tremblay J. P., Fortier M. A. (2006) Decidualization and maintenance of a functional prostaglandin system in human endometrial cell lines following transformation with SV40 large T antigen. Mol. Hum. Reprod. 12, 309–319 [DOI] [PubMed] [Google Scholar]
- 10. Daidoji T., Koma T., Du A., Yang C. S., Ueda M., Ikuta K., Nakaya T. (2008) H5N1 avian influenza virus induces apoptotic cell death in mammalian airway epithelial cells. J. Virol. 82, 11294–11307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Watanabe Y., Ibrahim M. S., Ellakany H. F., Kawashita N., Mizuike R., Hiramatsu H., Sriwilaijaroen N., Takagi T., Suzuki Y., Ikuta K. (2011) Acquisition of human-type receptor binding specificity by new H5N1 influenza virus sublineages during their emergence in birds in Egypt. PLoS Pathog. 7, e1002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Di Lonardo A., Buttinelli G., Amato C., Novello F., Ridolfi B., Fiore L. (2002) Rapid methods for identification of poliovirus isolates and determination of polio neutralizing antibody titers in human sera. J. Virol. Methods 101, 189–196 [DOI] [PubMed] [Google Scholar]
- 13. Kuwahara C., Takeuchi A. M., Nishimura T., Haraguchi K., Kubosaki A., Matsumoto Y., Saeki K., Matsumoto Y., Yokoyama T., Itohara S., Onodera T. (1999) Prions prevent neuronal cell-line death. Nature 400, 225–226 [DOI] [PubMed] [Google Scholar]
- 14. Fodor E., Devenish L., Engelhardt O. G., Palese P., Brownlee G. G., García-Sastre A. (1999) Rescue of influenza A virus from recombinant DNA. J. Virol. 73, 9679–9682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Basler C. F., Reid A. H., Dybing J. K., Janczewski T. A., Fanning T. G., Zheng H., Salvatore M., Perdue M. L., Swayne D. E., García-Sastre A., Palese P., Taubenberger J. K. (2001) Sequence of the 1918 pandemic influenza virus nonstructural gene (NS) segment and characterization of recombinant viruses bearing the 1918 NS genes. Proc. Natl. Acad. Sci. U.S.A. 98, 2746–2751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tumpey T. M., García-Sastre A., Mikulasova A., Taubenberger J. K., Swayne D. E., Palese P., Basler C. F. (2002) Existing antivirals are effective against influenza viruses with genes from the 1918 pandemic virus. Proc. Natl. Acad. Sci. U.S.A. 99, 13849–13854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sakai T., Ohuchi M., Imai M., Mizuno T., Kawasaki K., Kuroda K., Yamashina S. (2006) Dual wavelength imaging allows analysis of membrane fusion of influenza virus inside cells. J. Virol. 80, 2013–2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li Y., Drone C., Sat E., Ghosh H. P. (1993) Mutational analysis of the vesicular stomatitis virus glycoprotein G for membrane fusion domains. J. Virol. 67, 4070–4077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Teichgräber V., Ulrich M., Endlich N., Riethmüller J., Wilker B., De Oliveira-Munding C. C., van Heeckeren A. M., Barr M. L., von Kürthy G., Schmid K. W., Weller M., Tümmler B., Lang F., Grassme H., Döring G., Gulbins E. (2008) Ceramide accumulation mediates inflammation, cell death and infection susceptibility in cystic fibrosis. Nat. Med. 14, 382–391 [DOI] [PubMed] [Google Scholar]
- 20. Thomas J. A., Buchsbaum R. N., Zimniak A., Racker E. (1979) Intracellular pH measurements in Ehrlich ascites tumor cells utilizing spectroscopic probes generated in situ. Biochemistry 18, 2210–2218 [DOI] [PubMed] [Google Scholar]
- 21. Tycko B., Maxfield F. R. (1982) Rapid acidification of endocytic vesicles containing α2-macroglobulin. Cell 28, 643–651 [DOI] [PubMed] [Google Scholar]
- 22. Yoshimura A., Ohnishi S. (1984) Uncoating of influenza virus in endosomes. J. Virol. 51, 497–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Garten W., Klenk H. D. (1999) Understanding influenza virus pathogenicity. Trends Microbiol. 7, 99–100 [DOI] [PubMed] [Google Scholar]
- 24. Hatta M., Gao P., Halfmann P., Kawaoka Y. (2001) Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293, 1840–1842 [DOI] [PubMed] [Google Scholar]
- 25. Reed M. L., Bridges O. A., Seiler P., Kim J. K., Yen H. L., Salomon R., Govorkova E. A., Webster R. G., Russell C. J. (2010) The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity and transmissibility in ducks. J. Virol. 84, 1527–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Böttcher E., Matrosovich T., Beyerle M., Klenk H. D., Garten W., Matrosovich M. (2006) Proteolytic activation of influenza viruses by serine proteases TMPRSS2 and HAT from human airway epithelium. J. Virol. 80, 9896–9898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pelkmans L., Helenius A. (2003) Insider information: what viruses tell us about endocytosis. Curr. Opin. Cell Biol. 15, 414–422 [DOI] [PubMed] [Google Scholar]
- 28. Sieczkarski S. B., Whittaker G. R. (2003) Differential requirements of Rab5 and Rab7 for endocytosis of influenza and other enveloped viruses. Traffic 4, 333–343 [DOI] [PubMed] [Google Scholar]
- 29. Lakadamyali M., Rust M. J., Zhuang X. (2004) Endocytosis of influenza viruses. Microbes Infect. 6, 929–936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Akita H., Ito R., Khalil I. A., Futaki S., Harashima H. (2004) Quantitative three-dimensional analysis of the intracellular trafficking of plasmid DNA transfected by a nonviral gene delivery system using confocal laser scanning microscopy. Mol. Ther. 9, 443–451 [DOI] [PubMed] [Google Scholar]
- 31. Zhang Y., Li X., Grassmé H., Döring G., Gulbins E. (2010) Alterations in ceramide concentration and pH determine the release of reactive oxygen species by Cftr-deficient macrophages on infection. J. Immunol. 184, 5104–5111 [DOI] [PubMed] [Google Scholar]
- 32. Nagahama M., Itohayashi Y., Hara H., Higashihara M., Fukatani Y., Takagishi T., Oda M., Kobayashi K., Nakagawa I., Sakurai J. (2011) Cellular vacuolation induced by Clostridium perfringens ϵ-toxin. FEBS J. 278, 3395–3407 [DOI] [PubMed] [Google Scholar]
- 33. Pérez L., Carrasco L. (1994) Involvement of the vacuolar H(+)-ATPase in animal virus entry. J. Gen. Virol. 75, 2595–2606 [DOI] [PubMed] [Google Scholar]
- 34. Daniels R. S., Downie J. C., Hay A. J., Knossow M., Skehel J. J., Wang M. L., Wiley D. C. (1985) Fusion mutants of the influenza virus hemagglutinin glycoprotein. Cell 40, 431–439 [DOI] [PubMed] [Google Scholar]
- 35. Wiley D. C., Skehel J. J. (1987) The structure and function of the hemagglutinin membrane glycoprotein of influenza virus. Annu. Rev. Biochem. 56, 365–394 [DOI] [PubMed] [Google Scholar]
- 36. Bullough P. A., Hughson F. M., Skehel J. J., Wiley D. C. (1994) Structure of influenza haemagglutinin at the pH of membrane fusion. Nature 371, 37–43 [DOI] [PubMed] [Google Scholar]
- 37. Dutch R. E., Jardetzky T. S., Lamb R. A. (2000) Virus membrane fusion proteins: biological machines that undergo a metamorphosis. Biosci. Rep. 20, 597–612 [DOI] [PubMed] [Google Scholar]
- 38. Skehel J. J., Wiley D. C. (2000) Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69, 531–569 [DOI] [PubMed] [Google Scholar]
- 39. Schibli D. J., Weissenhorn W. (2004) Class I and class II viral fusion protein structures reveal similar principles in membrane fusion. Mol. Membr. Biol. 21, 361–371 [DOI] [PubMed] [Google Scholar]
- 40. Chen J., Lee K. H., Steinhauer D. A., Stevens D. J., Skehel J. J., Wiley D. C. (1998) Structure of the hemagglutinin precursor cleavage site, a determinant of influenza pathogenicity and the origin of the labile conformation. Cell 95, 409–417 [DOI] [PubMed] [Google Scholar]
- 41. Stevens J., Corper A. L., Basler C. F., Taubenberger J. K., Palese P., Wilson I. A. (2004) Structure of the uncleaved human H1 hemagglutinin from the extinct 1918 influenza virus. Science 303, 1866–1870 [DOI] [PubMed] [Google Scholar]
- 42. Thoennes S., Li Z. N., Lee B. J., Langley W. A., Skehel J. J., Russell R. J., Steinhauer D. A. (2008) Analysis of residues near the fusion peptide in the influenza hemagglutinin structure for roles in triggering membrane fusion. Virology 370, 403–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Galloway S. E., Reed M. L., Russell C. J., Steinhauer D. A. (2013) Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: implications for host range and adaptation. PLoS Pathog. 9, e1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Slemons R. D., Swayne D. E. (1995) Tissue tropism and replicative properties of waterfowl-origin influenza viruses in chickens. Avian Dis. 39, 521–527 [PubMed] [Google Scholar]
- 45. Farner D. S. (1942) The hydrogen ion concentration in avian digestive tracts. Poult. Sci. 21, 445–450 [Google Scholar]
- 46. Bowen T. E., Waldroup P. W. (1969) The influence of propylene glycol on pH of the gastrointestinal tract and the incidence of leg abnormalities in broiler chicks. Poult. Sci. 48, 608–613 [DOI] [PubMed] [Google Scholar]
- 47. Ito T., Okazaki K., Kawaoka Y., Takada A., Webster R. G., Kida H. (1995) Perpetuation of influenza A viruses in Alaskan waterfowl reservoirs. Arch. Virol. 140, 1163–1172 [DOI] [PubMed] [Google Scholar]
- 48. Spackman E., Stallknecht D. E., Slemons R. D., Winker K., Suarez D. L., Scott M., Swayne D. E. (2005) Phylogenetic analyses of type A influenza genes in natural reservoir species in North America reveals genetic variation. Virus Res. 114, 89–100 [DOI] [PubMed] [Google Scholar]
- 49. Wang G., Zhan D., Li L., Lei F., Liu B., Liu D., Xiao H., Feng Y., Li J., Yang B., Yin Z., Song X., Zhu X., Cong Y., Pu J., et al. (2008) H5N1 avian influenza re-emergence of Lake Qinghai: phylogenetic and antigenic analyses of the newly isolated viruses and roles of migratory birds in virus circulation. J. Gen. Virol. 89, 697–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Viguier C., Arora S., Gilmartin N., Welbeck K., O'Kennedy R. (2009) Mastitis detection: current trends and future perspectives. Trends Biotechnol. 27, 486–493 [DOI] [PubMed] [Google Scholar]
- 51. Ueda M., Daidoji T., Du A., Yang C. S., Ibrahim M. S., Ikuta K., Nakaya T. (2010) Highly pathogenic H5N1 avian influenza virus induces extracellular Ca2+ influx, leading to apoptosis in avian cells. J. Virol. 84, 3068–3078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. DuBois R. M., Zaraket H., Reddivari M., Heath R. J., White S. W., Russell C. J. (2011) Acid stability of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity. PLoS Pathog. 7, e1002398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Imai M., Watanabe T., Hatta M., Das S. C., Ozawa M., Shinya K., Zhong G., Hanson A., Katsura H., Watanabe S., Li C., Kawakami E., Yamada S., Kiso M., Suzuki Y., et al. (2012) Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486, 420–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Washington N., Steele R. J., Jackson S. J., Bush D., Mason J., Gill D. A., Pitt K., Rawlins D. A. (2000) Determination of baseline human nasal pH and the effect of intranasally administered buffers. Int. J. Pharm. 198, 139–146 [DOI] [PubMed] [Google Scholar]
- 55. Fischer H., Widdicombe J. H. (2006) Mechanisms of acid and base secretion by the airway epithelium. J. Membr. Biol. 211, 139–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yamashiro D. J., Maxfield F. R. (1987) Acidification of morphologically distinct endosomes in mutant and wild-type Chinese hamster ovary cells. J. Cell Biol. 105, 2723–2733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Maxfield F. R., McGraw T. E. (2004) Endocytic recycling. Nat. Rev. Mol. Cell Biol. 5, 121–132 [DOI] [PubMed] [Google Scholar]
- 58. van Renswoude J., Bridges K. R., Harford J. B., Klausner R. D. (1982) Receptor-mediated endocytosis of transferrin and the uptake of Fe in K562 cells: identification of a nonlysosomal acidic compartment. Proc. Natl. Acad. Sci. U.S.A. 79, 6186–6190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Yamashiro D. J., Tycko B., Fluss S. R., Maxfield F. R. (1984) Segregation of transferrin to a mildly acidic (pH 6.5) para-Golgi compartment in the recycling pathway. Cell 37, 789–800 [DOI] [PubMed] [Google Scholar]
- 60. Sipe D. M., Murphy R. F. (1987) High resolution kinetics of transferrin acidification in BALB/c 3T3 cells: exposure to pH 6 followed by temperature-sensitive alkalinization during recycling. Proc. Natl. Acad. Sci. U.S.A. 84, 7119–7123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Sipe D. M., Jesurum A., Murphy R. F. (1991) Absence of Na+,K(+)-ATPase regulation of endosomal acidification in K562 erythroleukemia cells. Analysis via inhibition of transferrin recycling by low temperatures. J. Biol. Chem. 266, 3469–3474 [PubMed] [Google Scholar]
- 62. Killisch I., Steinlein P., Römisch K., Hollinshead R., Beug H., Griffiths G. (1992) Characterization of early and late endocytic compartments of the transferrin cycle. Transferrin receptor antibody blocks erythroid differentiation by trapping the receptor in the early endosome. J. Cell Sci. 103, 211–232 [DOI] [PubMed] [Google Scholar]
- 63. Zen K., Biwersi J., Periasamy N., Verkman A. S. (1992) Second messengers regulate endosomal acidification in Swiss 3T3 fibroblasts. J. Cell Biol. 119, 99–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rybak S. L., Murphy R. F. (1998) Primary cell cultures from murine kidney and heart differ in endosomal pH. J. Cell. Physiol. 176, 216–222 [DOI] [PubMed] [Google Scholar]
- 65. Robbins A. R., Peng S. S., Marshall J. L. (1983) Mutant Chinese hamster ovary cells pleiotropically defective in receptor-mediated endocytosis. J. Cell Biol. 96, 1064–1071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Overly C. C., Lee K. D., Berthiaume E., Hollenbeck P. J. (1995) Quantitative measurement of intraorganelle pH in the endosomal-lysosomal pathway in neurons by using ratiometric imaging with pyranine. Proc. Natl. Acad. Sci. U.S.A. 92, 3156–3160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Evans M. J., Cabral-Anderson L. J., Freeman G. (1978) Role of the Clara cell in renewal of the bronchiolar epithelium. Lab. Invest. 38, 648–653 [PubMed] [Google Scholar]
- 68. Boers J. E., Ambergen A. W., Thunnissen F. B. (1998) Number and proliferation of basal and parabasal cells in normal human airway epithelium. Am. J. Respir. Crit. Care Med. 157, 2000–2006 [DOI] [PubMed] [Google Scholar]
- 69. Boers J. E., Ambergen A. W., Thunnissen F. B. (1999) Number and proliferation of Clara cells in normal human airway epithelium. Am. J. Respir. Crit. Care Med. 159, 1585–1591 [DOI] [PubMed] [Google Scholar]