Sickle cell disease (SCD) is a genetic disorder of the blood that leads to severe morbidity and early mortality. Between 80,000 and 100,000 individuals in the U.S. are affected by some form of SCD.1 Most hospital utilization for SCD pain begins in the emergency department (ED). Nationally, forty percent of ED visits for SCD pain end with the patient being admitted to the hospital.2 The most well-known burden of SCD is the vaso-occlusive crisis (VOC). These acute, excruciatingly painful events are the leading cause of hospital utilization among patients with SCD.3 Numerous studies show that patients and healthcare providers are dissatisfied with the quality of SCD pain management.4–6 SCD patients tend to report not having enough involvement in decisions about their own care, and that providers do not demonstrate respect, trust, and compassion.4 There is clearly basis for this belief, as studies have demonstrated that providers hold highly negative attitudes toward SCD patients and are strongly predisposed to suspect addiction in patients presenting for VOC care.4
A major system-level barrier to the provision of high quality SCD care is the lack of available centers that can provide expert care to the SCD population. While SCD is more prevalent than hemophilia and cystic fibrosis combined, there are only a handful (approximately 10) of comprehensive adult SCD centers in the U.S. compared to 100 each for hemophilia and cystic fibrosis.7 Partly through lack of education, provider attitudes toward patients with SCD tend to be negative, and poor provider knowledge about SCD worsens pain management.4 In an effort to improve acute care outcomes for SCD patients at our own institution, we developed a systems-level intervention, which we call the Sickle Cell Infusion Clinic (SCIC), to provide an alternative model for the delivery of acute care to our SCD patient population. The purpose of this paper is to describe the impact of the opening of the SCIC on patient outcomes and on hospital discharges for sickle cell disease in the city of Baltimore.
Methods
Infusion Center Model
In an attempt to improve pain management in the acute setting, in 2008 the Johns Hopkins Hospital (JHH) opened a dedicated acute care facility for adults presenting with vaso-occlusive crisis. The SCIC has 5 treatment slots for acute care visits, and is staffed by a clinic coordinator, nurse, clinical nurse associate, social worker and physician extender. Supervision is provided by a medical director. Part-time psychiatry services are available. Initially the SCIC was opened from 9 AM to 5 PM on weekdays. Starting in May of 2011, the SCIC opened from 10 AM to 8 PM on weekend days. The SCIC serves the needs of adult patients only. This is typically patients 21 and over but individuals as young as 18 are eligible for care if they are not patients of the Hopkins pediatric group. Visits fall into two categories; acute follow-ups and infusion visits. Infusion visits are used to treat patients in acute vaso-occlusive crisis and an acute follow-up visit is for patients that need to be seen the same day but do not require extended analgesic treatment or hydration. Patients have to present prior to 2:30 in the afternoon on weekdays and 5:30 PM on weekends, to initiate care in the SCIC. Patients are asked to call prior to presenting in the SCIC and the goal is to accept all patients for which there is space. These calls are triaged by a nurse. Patients who complain of severe chest pain, shortness of breath, or who are too sick for care in the SCIC (as determined by the judgment of the triage nurse) are directed to call 911. Patients do not need to be established patients of the clinic. All patients that are part of the JHH adult sickle cell clinic are informed of the SCIC and are encouraged to present to the SCIC during business hours and not go to the emergency department (ED). If a patient does present to the ED, they are triaged there and then referred to the SCIC during regular business hours. Patients who have presented to the ED overnight are transferred to the SCIC in the morning. Patients are assessed by a nurse and physician extender and analgesic therapy is initiated with a goal of having patients receive their first dose of opioid within 30 minutes of arrival. Laboratory tests are ordered based on the provider’s assessment of the patient; typically a complete blood count and reticulocyte count are drawn. Patients that present to the SCIC and are unstable (i.e. pulse ox <90% on >40% FiO2 by facemask, symptomatically hypotensive without response to fluid bolus) are transferred immediately to the ED. Patients that do not have adequate pain control by the time the clinic closes are assessed either for inpatient admission or for continued care in the ED. Pain management protocols are individualized based on prior patient history. A specific SCIC note template is used that makes it easy to identify patients’ prior treatment protocols. Tolerant patients are identified and dosed appropriately. Adjuvant medications and treatments including non-steroidal anti-inflammatory medications and heat packs are used as appropriate. Patients are typically treated by bolus (IM, IV or subcutaneous) opioid injection, with conversion to patient-controlled analgesia if admission is necessary. There are no specific discharge home criteria. If the patient feels that they can manage their pain at home with oral pain medications and the provider concurs then the patient is discharged. Staff ensure that all patients have access to pain medications at home prior to discharge. Nevertheless, patients who are discharged home from the SCIC are actively encouraged to come back to the SCIC on the following day if they still feel that they need help to control their pain.
Impact Evaluation: Study Design
Overview
To conduct this evaluation of the SCIC, we retrospectively collected outcomes and administrative data available to us from multiple sources. Our aims were to examine and describe SCIC outcomes in three different areas. Specifically, we sought to describe: 1) the General Characteristics of SCIC Care, 2) the Impact of the SCIC on JHH ED Care, and 3) the Impact of the SCIC on Community SCD utilization.
Data Sources
To fulfill aim #1, descriptive data including demographics, length of stay, time to first dose of opioid and pain scores (on the numerical rating scale), were collected prospectively on every patient presenting to the SCIC for care from 2008–2011. For aim #2, data for the JHH ED on number of visits and admission rates was examined from 2008–2011 but data on acuity, triage time, time to first pain medication and disposition was only available from the JHH emergency department from 4/2010–7/2012. For aim #3, data on Baltimore City hospital discharges for adults with sickle cell disease were obtained from the Maryland Health Services Cost Review Commission (MHSCRC). Data for the year prior to the opening of the SCIC (2007) to 2011 was examined to identify any correlation between the opening of the clinic and SCD admissions and readmissions in the State. The MHSCRC database collects annual statistics on the number of hospital discharges by hospital. Data collected include patient demographic characteristics, primary payer, secondary payer, principal diagnosis and other diagnoses, length of stay, complexity, condition code, and charges. The database includes all hospitals in the State, except for Veterans Affairs facilities. We used the following International Classification of Disease-9-Clinical Modification (ICD-9-CM) codes as recorded in the dataset to identify all adults (age 21+) with SCD admitted in the region: 282.41, 282.42 and 282.60–282.69. To select for hospitalizations for vaso-occlusive crisis, only non-elective hospital discharges from a Medicine service were examined for this analysis.
Analytic Methods
The following specific measures are used to describe care and assess outcomes in the SCIC (aim #1) or ED (aim #2): The number of SCIC/ED visits over time and by visit-type, the demographic makeup of patients receiving care in the SCIC, total charges of care, SCIC/ED discharge disposition, length of SCIC/ED treatment, time to receipt of first opioid dose, arrival and discharge pain scores, and the likelihood that a visit is categorized as a readmission.
In order to assess community-level outcomes (aim #3), we operationalized community-level impact of the SCIC in two ways: 1) by examination of community-level trends in SCD-related hospital utilization over time, and 2) by examination of community-level trends in the proportion of SCD-related hospital utilization that was characterized as a 30-day readmission. We categorized individual SCD-related hospital discharges as belonging to one of three broad geographic regions within the state based on distance from the City of Baltimore.
Statistical Analyses
Bivariate analyses were conducted using T-tests, Chi square tests, and simple generalized estimating equation (GEE) regression models accounting for the clustered nature of observations, as appropriate. Multivariable GEE linear and logistic regression models were used to identify any changes in the length of time spent in the SCIC over time, as well as to examine patient and visit-level predictors of being discharged home, all while accounting for the clustered nature of repeated visits by the same individual. Logistic regression models within a GEE framework were used to examine whether the odds of being a patient living in Baltimore changed over time. Because hospital admission rates from the ED are generally high (on the order of 40% or more), we used a modified poisson regression model within a GEE framework to examine factors affecting the risk of hospital admission from the JHH ED setting8. For the hospital discharge trend analysis, we calculated the total number of SCD-related hospital discharges occurring in each geographic region for each year under study. Negative binomial regression models were used to estimate linear trends in the number of SCD-related hospital discharges occurring in each year under study. We conducted the readmission trend analysis using the individual discharge-level data. We constructed logistic regression models within a GEE framework to examine the odds that any single discharge was categorized as a 30-day readmission. The GEE framework was used here to account for the potential non-independence of discharges from the same hospital. The Huber-White sandwich estimator was used to provide robust standard errors.
Results
SCIC
From the period February 2008 through December 2011 there were 3874 visits to the SCIC by 361 unique patients. Of those visits, 653 were categorized as acute follow-up visits while 3221 were infusion visits. Table 1 describes the characteristics of patients seen in the SCIC.
Table 1.
Characteristics of patients seen in the SCIC and ED from 2/2008–12/2011
| Characteristic | SCIC patients (361) | ED patients (558) | Total (655) |
|---|---|---|---|
| Number of visits | 3874 | 3408 | 7282 |
| Mean Age (SD)* | 31.9 (8.8) | 33.(9.5) | 32.4 (9.2) |
| Female, % | 58.1 | 58.4 | 58.9 |
| Number of visits per patient mean (SD, range) | 10 (15.7, 1–84) | 6 (12.3, 1–114) | 11.1 (23.2, 0–202)** |
| Number of visits per patient over 35 months, median (IQR) | 3 (10) | 2 (5) | 3(8) |
| Payor, % * | |||
| Medicaid | 46.3 | 54 | 49.8 |
| Medicare | 28.6 | 25.3 | 27 |
| Private | 22.1 | 14.3 | 18.4 |
| Self-pay | 3.0 | 6.4 | 4.7 |
| Admit (%)* | 15.2 # | 35.9 | 25.8 |
| Charge per visit, mean (95% CI) * | $739 ($718, 760) | $1975 ($1923, $2027)^ | $1185 ($1157.5, $1212.4) |
p<0.001
98 patients had no ED visits
admit from the SCIC means either directly admitted or sent to the ED for further care
charges only from those not admitted from the ED.
Characteristics of SCIC visits
On average there were 3.8 visits to the infusion clinic daily, 3.3 (range 0–10) of those were for infusion visits with the remaining being follow-up visits. One hundred six patients (33% of all patients with an infusion visit) had only a single visit to the SCIC over the time period. There was an annual increase in the number of infusion visits over time with an increase of 0.29 visits/yr (p<0.001). The average time to receipt of first dose of opioid from arrival to the clinic was 57.7 minutes (95% CI 56.5–58.8, median 51 minutes). The average time that patients spent in the SCIC was 4 hours and 55 minutes. The average pain level on the numerical rating scale (NRS) on arrival was 8.4 (95% CI 8.3–8.4). Arrival pain was significantly lower on average for those who were sent home versus those that required ongoing hospital care (8.3 v. 8.7, p<0.001). The average decrease in pain score from arrival to discharge was 2.62 points on the NRS (95% CI 2.55–2.69) with those who went home having a significantly greater decrease in pain score than those that remained for further hospital care (2.9 v. 1.2, p<0.001). There was no statistically significant difference in time to first dose of opioid for patients that were discharged home compared to those that required additional hospital care. (57.2 min v 60.3 min, p=0.06). In examining the association of pain scores and changes in pain scores during an SCIC visit with discharge disposition, we found that after adjustment for patient sex, patients were 2 times (OR 2.01, 95% CI 1.85, 2.19) more likely to be discharged home for every 1 point decrease in their change in pain. We also found that patients were less likely (OR 0.52, 95% CI 0.47, 0.58) to go home for every 1 point increase in pain score reported on arrival to the SCIC.
Emergency Department Visits
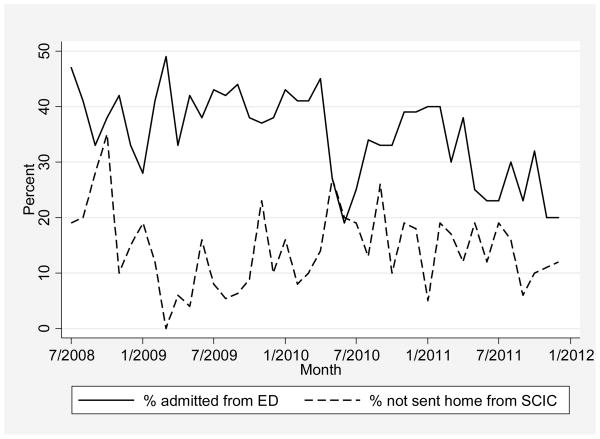
There were 3408 ED visits from 2008–2011for individuals with SCD. There were on average 63.3 emergency department visits for adults with sickle cell disease each month after the opening of the SCIC, which was slightly more than the number of monthly visits the year prior to the opening of the SCIC (53.8 before v 63.3 after, p=0.046). There was a statistically significant decrease in the rate of hospital admission from patients presenting to the ED each month (Figure 1) with the admission rate being reduced to 20% in December of 2011. The average total charge for a patient seen in the JHH ED who was not admitted was significantly higher than a patient seen in the SCIC $1975 (95% CI 1923–2027) vs. ($739 ($718–760).
Figure 1. Change in Admission rate for ED with Comparison SCIC data.
Solid line reflects the percent of patients that were admitted to the hospital from the ED over the study time period. The dotted line represents the percent of patients that were either directly admitted or transferred to the ED from the SCIC for ongoing treatment of VOC.
Characteristics of ED Visits
Due to implementation of an electronic medical record, additional data was available on time to first dose of opioid, acuity and disposition for patients seen in the ED between 4/2010–7/2012. During this time period there were 1554 ED visits made by 254 unique patients. The average time to first dose of pain medication during this time period was 190 minutes (SD 129.8). Eight percent (n =123) of patients were given an acuity level of 2, as measured by the Emergency Severity Index, and 91.8% (n = 1426) were designated as level 3 (the remaining were designated level 1 or 4). Those that were an acuity level 2 were placed in an ED bed more quickly than those at level 3 (42.9 minutes v. 82.3 min, p <0.001). They were also provided with their first dose of pain medication more quickly (134.7 min v 195.2 min, p<0.001) and stayed in the ED a shorter period of time (838.8 min v 1018 min, p<0.001). Patients designated as a level 2 were more likely to be admitted (59% v. 29%, p<0.001). In a model controlling for acuity, for every 10 minute increase in time to first dose of pain medication, the relative risk of admission increased by 0.7% (95% CI 1.001, 1.01, p=0.024).
Community-Level Impact
Trends in Hospital Discharges Over Time
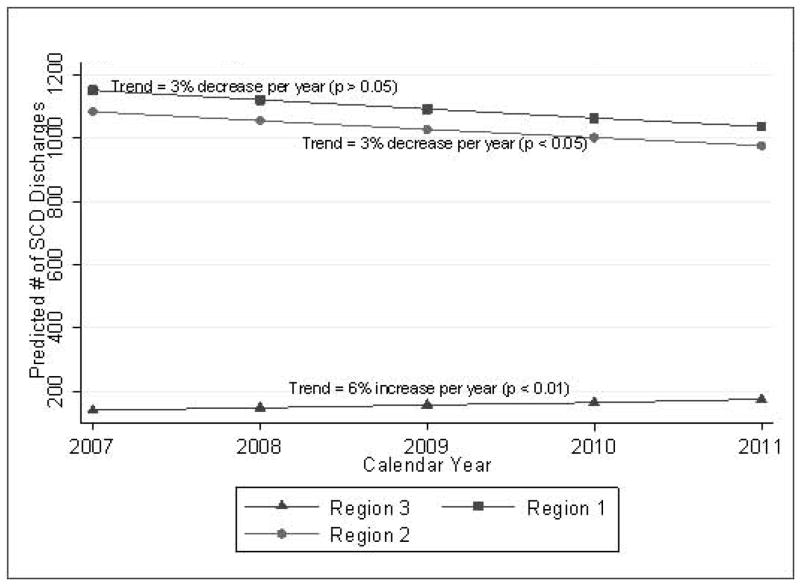
There are 13 community hospitals and 2 academic medical centers in the Metropolitan Baltimore area (within Hopkins market zone). Among the 15 hospitals, comparing 2008 to 2011, 9 had a reduction in hospital discharges for SCD. JHH saw an increase of 140 SCD discharges with a greater percentage of all Baltimore City SCD hospital discharges occurring at JHH (23% to 33%) over that time period. The odds that a patient admitted to Hopkins Hospital did not live in Baltimore increased by 15% each year, suggesting that a substantial number of hospital discharges for patients at JHH and therefore in Baltimore City was due to an influx over time of patients seeking care at JHH from outside of Baltimore City. Figure 2 demonstrates the trends in hospital discharges over the time period for 3 different regions in Maryland. Region 1 includes all discharges from hospitals in the city of Baltimore, Region 2 are all hospital discharges from hospitals within a 90 minute car ride of Baltimore and Region 3 are all discharges from hospitals that were greater than 90 minutes outside of Baltimore. We found that the number of SCD-related hospital discharges occurring in Maryland over time decreased by 2% each year, though this result was not statistically significant (IRROverall = 0.98, p = 0.881). When stratified by region a significant increase in SCD-related hospital discharges was seen each year in region 3 (IRR= 1.06, p = 0.036). Region 1 saw a trend towards a decrease in SCD-related hospital discharges over time (IRR= 0.97, p = 0.114) and Region 2 saw a significant decrease (IRR= 0.97, p = 0.008).
Figure 2. Regional Trends in MD SCD Hospital Discharges.
Trends in hospital admissions from 2007–2011 by region. Region 1: Baltimore City, Region 2: Within 90 miles of Baltimore Region 3: More than 90 miles from Baltimore
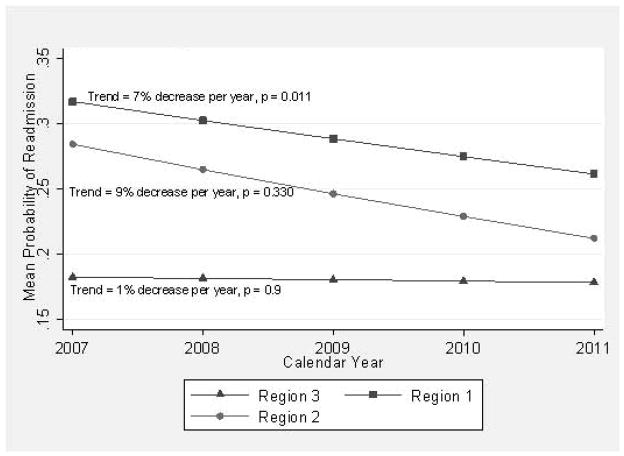
Trends in Hospital Readmissions Over Time
Figure 3 shows the trends in readmission over time. The likelihood that a SCD-related discharge was categorized as a 30-day readmission decreased by 8% annually, though this was not statistically significant (OR = 0.92, p = 0.093). At the regional level, readmissions in Region 3 were stable (unchanging) over time (OR = 0.99, p = 0.90). There was a significant decrease in readmissions over time for the Baltimore Metro area, Region 1, with the likelihood of readmission decreasing by 7% annually (OR = 0.93, p = 0.011). Region 2 showed a trend towards an annual decrease in readmissions, though this was not statistically significant (OR = 0.91, p = 0.33). For JHH the readmission rate dropped from 42% prior to the opening of the SCIC to 31% in 2011.
Figure 3. Regional Trends in MD SCD Readmission Rates.
Trends in hospital 30 day readmissions from 2007–2011 by region. Region 1: Baltimore City, Region 2: Within 90 miles of Baltimore Region 3: More than 90 miles from Baltimore
Discussion
The paucity of high quality sickle cell disease care for adults leads to many potentially avoidable hospital admissions. Our results suggest that our highly trained and dedicated sickle cell work force working within an infusion center has decreased hospital admissions for sickle cell disease across a community. The effect of the infusion center in decreasing the risk that a patient presenting to Johns Hopkins Hospital with sickle crisis gets admitted is similar to the findings of Benjamin and colleagues. They reported that the establishment of a dedicated SCD day hospital led to a 40% reduction in inpatient admissions relative to ED management.9 Since this seminal finding, supporting evidence confirms that rapid assessment of VOC, close monitoring, social service support, and individualized care improves outcomes.10–13 We have shown that 85% of the patients presenting to the SCIC are discharged home.
A novel finding of our study, though, is the finding that working in coordination with our emergency department, transporting patients who presented with crisis to the ED in the evenings to the infusion clinic in the mornings has resulted in a significant decrease in the SCD admission rate from the ED as well. While a full analysis of the cost effectiveness of an infusion clinic is beyond the scope of this report, the average charge associated with a visit to the SCIC was significantly lower than the average charge from the JHH ED. This, along with a decrease in hospital admissions suggests that this model of care not only significantly improves the quality of care but could also result in significant cost savings.
Another novel finding of this study is the potential community-level impact the opening of the infusion clinic appears to have had on hospital discharges for the Baltimore region. The total number of hospital discharges for medicine admissions and readmissions for sickle cell disease decreased over the time period for Baltimore and the local region. It is not possible to prove that the decrease in admissions and readmissions were due solely to the opening of the infusion clinic at JHH. Nevertheless, supporting evidence for this conclusion may be found in the fact that the region farthest from Baltimore saw none of the positive trends in SCD utilization over time that we found in the other regions.
There are several possible explanations for the improved outcomes seen when patients are treated in an infusion clinic setting as opposed to the emergency department. One main difference between the two settings is that a patient presenting to the infusion clinic is seen with less delay whereas in the emergency department delays in care due to overcrowding continue to occur14. We and others15;16 have shown that delays in treatment in the emergency department occur more often in African Americans and our prior research has demonstrated that compared to individuals of the same race, wait times for people with sickle cell disease are longer on average than wait times for people with long bone fractures in the ED setting.17 This delay in treatment may lead to worsening of pain prior to treatment as patients may delay coming to the ED due to concerns over long wait times. Importantly, we have shown that delays in the administration of pain medication in the ED are associated with an increased risk of admission. We likely did not see these differences in the SCIC because the admission rate is so low and the time to first dose of pain medications is less variable than in the ED setting. Another possible reason for improved outcomes in the infusion clinic is the continuity of care. Patients are seen by a team of professionals that know them well and have an in-depth knowledge of their disease. In addition patients have the option of returning the following day for treatment if needed, knowing that there will be no delay in access to care. This provides reassurance to both the patient and the provider that care is available on a daily basis without delay. Finally, some may argue that patients that present to the ED are sicker than those that present to the infusion clinic and therefore the ED will have higher admission rates. While this is likely to be true for a small percentage of patients seen in the ED, the overall decrease of the admission rate from a high of 47% down to 20% for all SCD patients presenting to the JHH ED suggests that many of the people who presented to the ED prior to the opening of the infusion clinic could have been successfully managed as outpatients in an infusion clinic setting.
One of the limitations of this study was the use of administrative data for collection of both the ED data and data from the MHSCRC. These data depend on proper ICD9 coding which may have had an effect on our ability to accurately identify those with a sickle cell diagnosis. As this was a problem for each year of the study it was unlikely that it had any significant impact on our results. In addition, re-evaluation frequency or illness severity may have varied between the ED and the SCIC, which might influence the risk of hospital admission. Data from the ED on time to first dose was collected over a slightly different time period than that presented for the SCIC, which potentially may reduce the extent to which the outcomes in the two settings can be compared. However, while the time periods were not exactly the same, there was significant overlap between to the two, so it is likely that the data presented was a valid representation of ED practices. Future studies are needed in order to more directly compare these measures between an infusion center and an ED setting and see how they may predict hospital admission. This information might allow investigators to determine the specific aspects of infusion center care that leads to improved outcomes. An additional limitation is that we have assumed that the changes in hospital utilization that occurred across Baltimore City after the opening of the infusion clinic were due to the opening of this clinic. This assumption is based on there being no other sickle specialty clinics in the Baltimore area during the time period under study. We know of no other changes in health care delivery that might have had an effect on hospital admission for adults with SCD across the geographic regions we studied. This, coupled with the increased volumes of patients seen at JHH, suggests that the decrease in hospital admissions in all of Baltimore was likely due to the opening of the SCIC and the subsequent increase in the number of individuals seeking care through this particular infusion clinic.
In summary, the infusion clinic model provides adults with sickle cell disease access to high quality care that decreases the need for hospital admission. The impact of such a clinic goes beyond the institution where it is based and can affect an entire community. Further research needs to be done to evaluate the cost effectiveness of infusion clinics and to confirm high levels of patient satisfaction with this form of care.
Acknowledgments
The authors acknowledge the staff of the Sickle Cell Infusion Center, Johns Hopkins Hospital, Baltimore, MD, for assistance in implementation
Sophie Lanzkron’s work was supported by grant #K23HL083089 from the National Heart, Lung, and Blood Institute (NHLBI). Carlton Haywood’s work was supported by grant #K01HL108832-01 from the NHLBI.
Contributor Information
Sophie Lanzkron, Email: slanzkr@jhmi.edu, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, 1830 E. Monument St. Suite 7300, Baltimore, MD 21205, phone 410-502-7770, fax 410-614-8601.
Patrick C. Carroll, Department of Psychiatry and Behavioral Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Peter Hill, Department of Emergency Medicine, Johns Hopkins University School of Medicine, Baltimore, MD.
Mandy David, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD.
Nicklaine Paul, Department of Nursing, Johns Hopkins Hospital, Baltimore, MD.
Carlton Haywood, Jr., Department of Medicine, Johns Hopkins School of Medicine, Core Faculty, The Johns Hopkins Berman, Institute of Bioethics, Baltimore, Maryland.
Reference List
- 1.Hassell KL. Population estimates of sickle cell disease in the U.S. Am J Prev Med. 2010;38:S512–S521. doi: 10.1016/j.amepre.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 2.Lanzkron S, Carroll CP, Haywood C., Jr The burden of emergency department use for sickle-cell disease: an analysis of the national emergency department sample database. Am J Hematol. 2010;85:797–799. doi: 10.1002/ajh.21807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Platt OS, Brambilla DJ, Rosse WF, et al. Mortality In Sickle Cell Disease -- Life Expectancy and Risk Factors for Early Death. N Engl J Med. 1994;330:1639–1644. doi: 10.1056/NEJM199406093302303. [DOI] [PubMed] [Google Scholar]
- 4.Haywood C, Jr, Beach MC, Lanzkron S, et al. A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. J Natl Med Assoc. 2009;101:1022–1033. doi: 10.1016/s0027-9684(15)31069-5. [DOI] [PubMed] [Google Scholar]
- 5.Murray N, May A. Painful crises in sickle cell disease--patients’ perspectives. BMJ. 1988;297:452–454. doi: 10.1136/bmj.297.6646.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alleyne J, Thomas VJ. The management of sickle cell crisis pain as experienced by patients and their carers. J Adv Nurs. 1994;19:725–732. doi: 10.1111/j.1365-2648.1994.tb01144.x. [DOI] [PubMed] [Google Scholar]
- 7.Grosse SD, Schechter MS, Kulkarni R, et al. Models of comprehensive multidisciplinary care for individuals in the United States with genetic disorders. Pediatrics. 2009;123:407–412. doi: 10.1542/peds.2007-2875. [DOI] [PubMed] [Google Scholar]
- 8.Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol. 2011;174:984–992. doi: 10.1093/aje/kwr183. [DOI] [PubMed] [Google Scholar]
- 9.Benjamin LJ, Swinson GI, Nagel RL. Sickle cell anemia day hospital: an approach for the management of uncomplicated painful crises. Blood. 2000;95:1130–1136. [PubMed] [Google Scholar]
- 10.Raphael JL, Kamdar A, Beavers MB, Mahoney DH, Mueller BU. Treatment of uncomplicated vaso-occlusive crises in children with sickle cell disease in a day hospital. Pediatr Blood Cancer. 2008;51:82–85. doi: 10.1002/pbc.21483. [DOI] [PubMed] [Google Scholar]
- 11.Wright J, Bareford D, Wright C, et al. Day case management of sickle pain: 3 years experience in a UK sickle cell unit. Br J Haematol. 2004;126:878–880. doi: 10.1111/j.1365-2141.2004.05123.x. [DOI] [PubMed] [Google Scholar]
- 12.Adewoye AH, Nolan V, Mcmahon L, Ma Q, Steinberg MH. Effectiveness of a dedicated day hospital for management of acute sickle cell pain. Haematologica. 2007;92:854–855. doi: 10.3324/haematol.10757. [DOI] [PubMed] [Google Scholar]
- 13.Raphael JL, Kamdar A, Wang T, et al. Day hospital versus inpatient management of uncomplicated vaso-occlusive crises in children with sickle cell disease. Pediatr Blood Cancer. 2008;51:398–401. doi: 10.1002/pbc.21537. [DOI] [PubMed] [Google Scholar]
- 14.U.S.Government Accountability Office and Report to the Chairman. Crowding Continues to Occur and Some Patients Wait Longer than Recommended Time Frames. GAO; 2009. Committee on Finance U. S. Senate. report online Washington DC. Hospital Emergency Departments. GAO-09-347. 2009. 6-26-2012. Ref Type: Report. [Google Scholar]
- 15.Johnston V, Bao Y. Race/ethnicity-related and payer-related disparities in the timeliness of emergency care in U.S. emergency departments. JHealth Care Poor Underserved. 2011;22:606–620. doi: 10.1353/hpu.2011.0050. [DOI] [PubMed] [Google Scholar]
- 16.Mills AM, Shofer FS, Boulis AK, Holena DN, Abbuhl SB. Racial disparity in analgesic treatment for ED patients with abdominal or back pain. Am J Emerg Med. 2011;29:752–756. doi: 10.1016/j.ajem.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 17.Haywood C, Jr, Tanabe P, Naik R, Beach MC, Lanzkron S. The impact of race and disease on sickle cell patient wait times in the emergency department. Am J Emerg Med. 2013;31:651–656. doi: 10.1016/j.ajem.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]