Abstract
The purpose of this research was to develop and pilot test an intervention to optimize functional recovery for breast cancer survivors. Over two studies, 31 women enrolled in a goal-setting program via telephone. All eligible women enrolled (37% of those screened) and 66% completed all study activities. Completers were highly satisfied with the intervention, using it to address, on average, four different challenging activities. The longitudinal analysis showed a main effect of time for overall quality of life (F(5, 43.1) = 5.1, p = 0.001) and improvements in active coping (F (3, 31.7) = 4.9, p = 0.007), planning (F (3, 36.0) = 4.1, p = 0.01), reframing (F (3, 29.3) = 8.5, p < 0.001), and decreases in self-blame (F (3,31.6) = 4.3, p = 0.01). The intervention is feasible and warrants further study to determine its efficacy in fostering recovery and maximizing activity engagement after cancer treatment.
At the start of 2012, there were 2.9 million women with a history of breast cancer living in the United States (American Cancer Society, 2013). While quality of life generally improves after completion of breast cancer treatment (Deshields et al., 2005), 10% to 23% of women experience reduced quality of life over the year after breast cancer treatment (Penttinen et al., 2011). That reduced quality of life is often associated with a reduction in activity level. Most breast cancer survivors experience a reduction in physical activity levels by as much as 50% from pre-diagnosis to one year post-diagnosis, particularly for moderate- and vigorous-intensity activities (Irwin et al., 2003; Littman, Tang, & Rossing, 2010; Ness, Wall, Oakes, Robison, & Gurney, 2006). Breast cancer survivors are also 1.5 times more likely to take extended sick leave from work (>16 days) than non-cancer controls for up to five years following diagnosis (Torp, Nielsen, Gudbergsson, Fossa, & Dahl, 2012) and are two to three times more likely to go on permanent disability (Hauglann, Benth, Fossa, & Dahl, 2012). Challenges in performing activities related to roles in work, home or self-care are most apparent in women under the age of 60 (Ness et al., 2006). For young to middle-aged women, cancer diagnosis and treatment can occur during a period of their lives when there are high demands for peak performance in work and family management and less flexibility in scheduling one’s daily activities.
Although breast cancer survivorship rates have increased over the past two decades (American Cancer Society, 2013), cancer rehabilitation research has struggled to keep pace. Egan and McEwen (2013) noted good evidence supporting the use of exercise and other physical rehabilitation techniques to improve physical function, but an absence of research on interventions that encourage satisfying role resumption and full participation in valued daily activities. To address this gap, we developed a brief, telephone-based intervention and pilot tested it with breast cancer survivors across two studies. The intervention was based on principles of two cognitive-behavioral therapies: Behavioral Activation (BA) (Cuijpers, van Straten, & Warmerdam, 2007a; Lejuez, Hopko, LePage, Hopko, & McNeil, 2001) and Problem Solving Treatment (PST) (Cuijpers, van Straten, & Warmerdam, 2007b; Hegel & Arean, 2003). Participants used the goal setting and problem-solving structure of the Behavioral Activation/Problem Solving (BA/PS) intervention to address challenges in many areas of life, including getting exercise, managing stress, and functioning better at work and home. The present study examines the intervention development process and reports initial data regarding the feasibility and potential efficacy of this manualized intervention.
Method
Overview of the Intervention Development Process
Study 1
The aims of the first study were to develop the treatment manual and collect data on the acceptability of the intervention and possible treatment outcomes. The study used a pre-post design with three assessment points. Women were eligible for the study if they had received chemotherapy for Stage I - III breast cancer, were between the ages of 18 and 60, were English-speaking with access to a reliable telephone service, and were experiencing impaired functioning upon completion of or up to six months after chemotherapy. We screened for functional impairment using the Valued Activities Inventory (Lyons et al., 2012). To be eligible women had to report moderate difficulty performing at least one activity that was of moderate importance to them.
The intervention consisted of nine telephone-delivered sessions that occurred once a week for six weeks, with three monthly follow-up sessions. We delivered the intervention via telephone because our patient population has wide geographic dispersion and previous research participants have appreciated the convenience of being able to enroll in research without increasing the time spent at our cancer center (Bakitas et al., 2009; Bakitas et al., 2004; Hegel et al., 2011; Maloney et al., 2013).
We encountered two central challenges in Study 1. First, it was difficult for the participants to complete the weekly sessions in a timely manner. This was partly because the interventionist had limited availability during working hours. The second challenge was that the problem-solving portion of the intervention (i.e., brainstorming and weighing options) was not well-integrated and the interventionist relied exclusively on the Behavioral Activation process (i.e., problem identification, goal setting, and action planning).
Study 2
Using what we learned in Study 1, we made changes to the intervention and design of Study 2. The aims of Study 2 were to revise the treatment manual, develop a fidelity measure, and assess the feasibility and potential efficacy of the revised BA/PS intervention. Study 2 employed a pre-post design, but used four assessment points that included a no-treatment run-in phase to allow us to estimate the amount of spontaneous functional recovery in this sample. The eligibility criteria were modified to exclude women if they had non-correctable hearing loss, a diagnosis of schizophrenia or bipolar disorder, or gross cognitive impairment i.e., a score of less than three on the Callahan Cognitive Screener (Callahan, Unverzagt, Hui, Perkins, & Hendrie, 2002). We also adopted a shorter functional screening instrument (i.e., women were eligible if they scored 11 or higher on the Work and Social Adjustment Scale (Mundt, Marks, Shear, & Greist, 2002)) and excluded women who reported functional limitations from a non-cancer related physical disorder. We adopted these changes to reduce the influence of confounding or extraneous variables when exploring potential treatment efficacy.
To improve the intervention, we created an explicit decision rule regarding when to utilize the problem-solving process (described in the next section). We hired an interventionist who was available to deliver the intervention by telephone at participant’s convenience (day or night of all weekdays) and reduced the intervention to six weekly sessions. We used the same feasibility and acceptability metrics as Study 1, but incorporated some new outcome measures.
The Behavioral Activation/Problem Solving (BA/PS) Intervention
Behavioral Activation (BA) (Cuijpers et al., 2007a; Lejuez et al., 2001) and Problem-solving Treatment (PST) (Cuijpers et al., 2007b; Hegel & Arean, 2003) are two manualized, evidence-based interventions originally designed to treat depression. BA seeks to increase the frequency with which people engage in rewarding, pleasurable, or valued daily activities. PST supposes that people with weak problem-solving skills are vulnerable to depression because of the stress that results from ineffective coping attempts. Both interventions use structured formats to teach people ways to adapt to and cope with stress in various life domains such as work, interpersonal relationships, and leisure. Both interventions focus on finding practical solutions to daily challenges in life. Although they were initially designed to treat depression, we believe the pragmatic and activity-focused nature of both BA and PST offer accessible, structured frameworks with which to address a variety of functional challenges faced by cancer survivors.
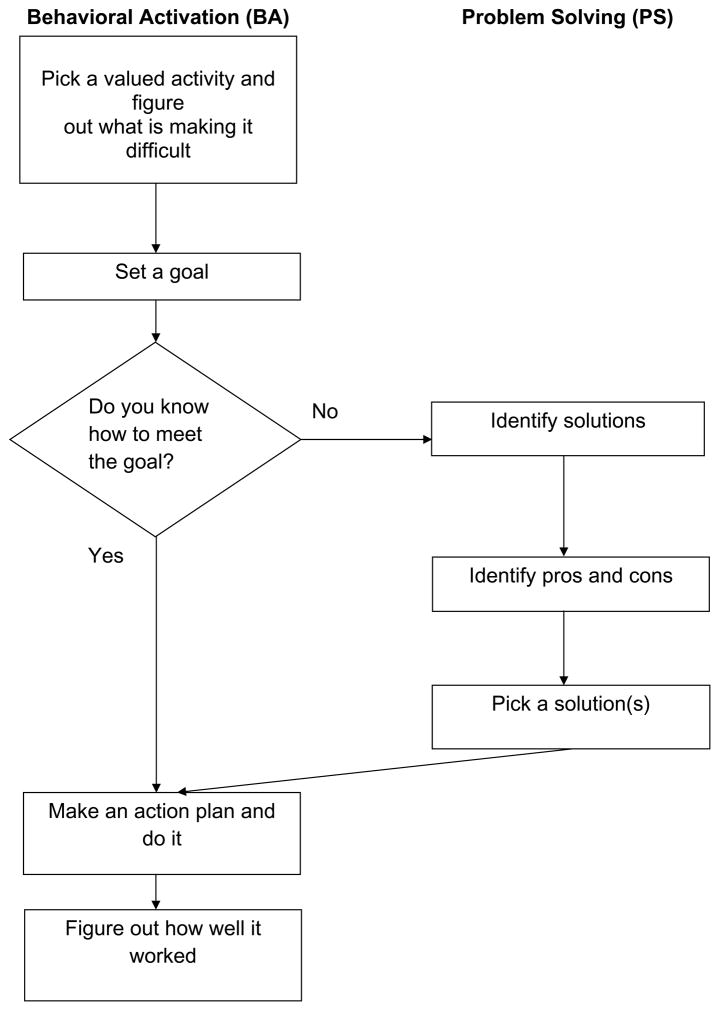
We blended BA and PST into our BA/PS intervention as depicted in Figure 1. The BA process involved four steps: (1) identifying why an activity was challenging, (2) setting a goal that was behavioral, measurable and achievable within the next seven days, (3) constructing a detailed action plan that delineates when, where, and how the activity will be conducted, and (4) assessing how well the goal was met and the activity was performed. Problem-solving adds two additional steps to this process. If a goal is very general and a woman is unsure of how to meet her goal, she is prompted to (1) brainstorm various solutions and (2) weigh their advantages and disadvantages before selecting one and proceeding to develop an action plan. BA is a parsimonious and efficient method of setting goals when the woman knows exactly what she wants to accomplish and primarily needs to create an adaptable action plan. Alternatively, problem-solving is useful in situations when the woman knows the goal she wants to set regarding the challenge but does not know exactly how to best meet the goal. For example, one woman’s goal was to engage in a replacement activity when experiencing the urge to smoke, but she did not immediately know what activities might be effective options. With problem-solving, she brainstormed possible solutions of going for a walk, knitting, reading a book, and calling a friend. After listing the advantages and disadvantages of each, she tailored her action plan to what she perceived as the best solution.
Figure 1.
The integrated structure of the BA/PS intervention
The women received a workbook that contained background information and worksheets that they used to set and monitor weekly goals. During the first session the interventionist explained the rationale for the study, discussed the relationship between activity engagement and health, reviewed the benefits of regular exercise and effective stress management techniques, and explained the structure of BA/PS. Women were told that each week we would ask them to set at least one, but ideally two goals related to activities that they wanted to do but found challenging. We encouraged them to think about setting goals for activities that supported their health (exercise, nutrition, stress management, smoking cessation, sleep, or upper extremity exercise or lymphedema management) and other aspects of functioning (work, childcare, leisure, activities of daily living, home management, sexual functioning, and spirituality). During the first session we asked women to tell us about their cancer treatment and how satisfied they felt with their engagement in the above-listed activity domains. Each subsequent session involved using the BA/PS structured worksheets to address one or two challenging activities. The first step of each subsequent session was to review how well the previous action plan worked, how satisfied the woman was with the effort she put into executing her action plan, and whether the goal was met. The woman could then choose to address the same goal(s) for the coming week or could identify new activities to address with BA/PS. Women used the sessions to address activities they found challenging including exercise, stress management activities, work, instrumental activities of daily living, nutrition, smoking cessation, leisure and social activities, sleep, child care, and other miscellaneous activities. Details regarding session content are available from the first author and described in another manuscript (Lyons, Svensborn, Kornblith, & Hegel, in press).
Sessions were audiorecorded for the purposes of fidelity monitoring and intervention development. We monitored the fidelity of the interventionists to the developing treatment manuals in two ways. In Study 1, the principal investigator (last author) met at least monthly with the interventionist to discuss the challenges and pragmatics of delivering the intervention. He also formally rated interventionist fidelity on seven randomly chosen sessions from four participants using a 10-item scale developed for other studies of Behavioral Activation. In Study 2, the principal investigator and interventionist (first author) met weekly to discuss the study and the intervention development process. They developed a 17-item scale that reflected the BA/PS intervention tasks and a psychologist (fifth author) trained in both Behavioral Activation and Problem-Solving Treatment used the scale to rate 20 sessions (a first session and a randomly chosen subsequent session from 10 participants). In both studies, all rated sessions met the performance standards set by the fidelity rating systems.
Data Collection
This paper reports the quantitative data reflecting feasibility and the four outcome measures (i.e., quality of life, depression, anxiety, and coping style) that were used in both Studies 1 and 2. Both studies administered satisfaction and outcome assessments by telephone. In Study 1, women were assessed at three time points: at enrollment, 8 weeks after enrollment (after completing the six weekly sessions), and 26 weeks after enrollment (after completing the three monthly follow up sessions). In Study 2, women were assessed at enrollment and six weeks later. These six weeks represented a no- treatment run-in phase, included to estimate the amount of change or spontaneous recovery women experienced in the absence of treatment. After the six week assessment, women began the intervention and were assessed again at 12 weeks (immediately after the six weekly sessions) and at 18 weeks after enrollment.
Measures of Feasibility
We recorded the number of women who a) were informed of the study in the clinic b) agreed to complete the screening process, c) completed each assessment, and d) completed each treatment session. For each session, the interventionist recorded whether behavioral activation or problem-solving was used. For Study 2 we also recorded the time and length of each session. A research assistant assessed satisfaction with the intervention using investigator-developed Likert scales of a) satisfaction with the study, b) helpfulness of the intervention, c) satisfaction with the intervention, d) relevance of topics addressed in the sessions, e) satisfaction with therapist, and f) satisfaction with the length and timing of sessions.
Measures of Potential Efficacy
Goal attainment
Interventionists recorded whether the participant reported meeting her weekly goal. For Study 2, we also recorded the level of satisfaction each woman reported regarding the effort she put into executing her action plan on a 0–10 scale and degree of goal attainment (e.g., number of days that progress towards a goal was reported or proportion of tasks that were accomplished).
Quality of Life
The Functional Assessment of Cancer Therapy-Breast Cancer + Arm Morbidity (FACT-B+4) is a 41-item self-report measure of health-related quality of life specifically designed for breast cancer patients (Brady et al., 1997; Coster, Poole, & Fallowfield, 2001). The first 27 items of the tool represent the FACT-G and assess perceived well-being in physical, social, emotional, and functional domains. The remainder of the tool addresses 10 concerns directly relevant to breast cancer (e.g., concerns about weight change, familial patterns of cancer, appearance) and four questions about upper extremity symptoms (e.g., range of motion, lymphedema). The FACT-B+4 has an internal consistency of α=.88 and high (r = .97) five-day test-retest reliability (Coster et al., 2001). Scores range from 0 to 164 (higher scores indicate better quality of life).
Depression and Anxiety
The Hospital Anxiety and Depression Scale (HADS) is a 14-item self-report measure of depressive and anxiety symptoms specifically designed for medical patients (Zigmond & Snaith, 1983). The HADS contains only the cognitive symptoms of depression and anxiety, thus eliminating the somatic symptoms that are poor indicators of psychiatric distress in the medically ill. A recent meta-analysis suggests that the HADS is an adequate screening tool for depression and anxiety in a cancer population (Vodermaier & Millman, 2011). Scores range from 0 to 21 on each of the subscales of depression and anxiety (higher scores indicate more severe symptoms).
Coping style
The Brief Cope has 28 items that combine to form 14 subscales of coping reactions (Carver, 1997). The Brief COPE (Carver, 1997) is a shortened version of the original COPE (Carver, Scheier, & Weintraub, 1989). The internal consistency for each subscale is at or above minimally acceptable levels (α ranging from .50-.90). The Brief COPE has been shown to have excellent psychometric properties among breast cancer patients (Fillion, Kovacs, Gagnon, & Endler, 2002). The fourteen coping reactions include: active coping, planning, seeking emotional support, seeking instrumental support, behavioral disengagement, denial, reframing, venting, distraction, self-blame, humor, substance use, acceptance, and religion. Scores range from 0 to 6 for each subscale (higher scores indicate greater use of the coping style).
Analysis
To explore feasibility, we analyzed data regarding recruitment and retention, satisfaction with the intervention, and session content. To do so, we a) compiled the number of patients identified, screened, eligible, enrolled, and retained in the intervention and assessments, b) summarized the numbers and reasons for withdrawals for each study, c) compiled descriptive statistics on the participant satisfaction ratings, and d) summarized details regarding the length of sessions and number of goals set.
To explore potential efficacy, we analyzed data regarding goal attainment, the outcomes of quality of life, depression, and anxiety, and we looked at coping style as a potential mechanism of change. First we summarized the rates of goal attainment in the sessions. We combined the outcome data from both studies and created one dataset that had five assessment points. As can be seen in Table 1, time was conceived as a 27–week continuum. Weeks −6 to 0 reflected the no-treatment, run-in phase employed in Study 2. The acute intervention for both studies occurred during weeks 0 to 6. The follow-up intervention of Study 1 occurred during weeks 6 through 18. Assessments occurred at Week −6 (before the start of the no-treatment run-in phase of Study 2, labeled Assessment 0), Week 0 (immediately pre-treatment in both studies, labeled Assessment 1), Weeks 6 and 8 (after acute treatment in both studies, labeled Assessment 2 and 3, respectively) and Weeks 12 and 20 (after no treatment in Study 2 and maintenance treatment in Study 1, labeled Assessment 4 and 5, respectively). We used a repeated measures approach to linear mixed modeling to explore main effects of time for quality of life, depression, and anxiety. We tested the difference between estimated marginal means using least significant difference (LSD) tests. When we noticed that the women who withdrew had high rates of anxiety and depression, we repeated the analyses on anxiety and depression using only data from the women who did not withdraw from the study.
Table 1.
Overview of How Study Assessments and Intervention Activities Overlapped and were Merged
| Week | −6 | −5 | −4 | −3 | −2 | −1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study 1 | E | I | I | I | I | I | I | I | I | I | |||||||||||||||||
|
| |||||||||||||||||||||||||||
| A1 | A3 | A5 | |||||||||||||||||||||||||
|
| |||||||||||||||||||||||||||
| Study 2 | E | I | I | I | I | I | I | ||||||||||||||||||||
| A0 | A1 | A2 | A4 | ||||||||||||||||||||||||
E = Enrollment
A = Study Assessment
I = Intervention Telephone Call
We also used a repeated measures approach to linear mixed modeling to examine changes in coping style before and after the acute intervention as a potential mechanism for change in well-being. Finally, we examined the plausibility of this mechanism by testing correlations of change in coping style with change in quality of life, depression, and anxiety.
Results
Participants
Participant characteristics were similar across the studies and are presented in Table 2.
Table 2.
Participant Characteristics
| Characteristic | Study 1 (N = 15) Mean (sd) |
Study 2 (N = 16)1 Mean (sd) |
|---|---|---|
| Age in years | 52 (6) | 46 (7) |
| Number lymph nodes dissected | 8 (7) | 9 (9) |
|
| ||
| n (%) | n (%) | |
|
| ||
| Stage | ||
| 1 | 6 (40) | 3 (19) |
| 2 | 7 (47) | 8 (50) |
| 3 | 2 (13) | 5 (31) |
| Surgery | ||
| Mastectomy | 13 (87) | 13 (81) |
| Lumpectomy | 2 (13) | 3 (19) |
| Axillary node dissection | 15 (100) | 13 (81) |
| Received radiation | 8 (53) | 10 (63) |
| Receiving herceptin | 4 (27) | 9 (56) |
| Receiving aromatase inhibitor | 7 (47) | 7 (44) |
| Race and Ethnicity | ||
| White and Non-Hispanic | 15 (100) | 15 (94) |
| Asian and Non-Hispanic | 0 | 1 (6) |
| Marital status | ||
| Never married | 0 | 1 (6) |
| Married | 13 (87) | 12 (75) |
| Living with a partner | 0 | 2 (13) |
| Divorced | 2 (13) | 1 (6) |
| Living with children < 16 yrs old | 4 (27)2 | 9 (56) |
| Employment | ||
| Full time | 4 (27) | 8 (50) |
| Part time | 5 (33) | 4 (25) |
| Not working | 6 (40) | 4 (25) |
| Income | ||
| Less than $40,00 per year | 5 (33) | 7 (44) |
| $40,000 or more per year | 8 (53) | 5 (56) |
| Declined to answer | 2 (13) | 0 |
| Education | ||
| High school graduate/GED | 2 (13) | 5 (31) |
| Some college/technical school | 4 (27) | 3 (19) |
| College graduate | 1 (7) | 5 (31) |
| Graduate degree | 6 (40) | 3 (19) |
| Declined to answer | 2 (13) | 0 |
Seventeen women enrolled, but one woman withdrew before completing the baseline assessment.
In Study 1, we did not ask the age of children, only whether children were members of the household.
Feasibility
Recruitment and Retention
Recruitment and retention statistics were similar across the two studies and are summarized in Table 3. Approximately one-third of the women who agreed to be screened were experiencing participation restrictions. Although every eligible woman agreed to enroll (N = 15 in Study 1 and N = 17 in Study 2), both studies experienced attrition. In Study 1, one woman withdrew after completing the baseline assessment, one after session 1, one after three sessions, and two after four sessions. All women except one reported withdrawing because of time constraints and inability to fit the program into their schedule. The remaining woman reported feeling overwhelmed by the paperwork involved in the intervention. All of the women who withdrew from Study 1 were experiencing high levels of depressive symptoms (≥ 5 on baseline HADS) and four of the five women who withdrew were experiencing high levels of anxiety symptoms (≥7 on baseline HADS) according to recent cut off scores identified for cancer patients (Vodermaier & Millman, 2011).
Table 3.
Identification, Enrollment, and Retention of Participants
| Construct | Operational definition | Study 1 | Study 2 |
|---|---|---|---|
| Identification | # screened/ # approached | Not collected | 45/78 (58%) |
| Eligibility | # eligible/ # screened | 15/42 (36%) | 17/45 (38%) |
| Enrollment | # enrolled / # eligible | 15/15 (100%) | 17/17 (100%) |
| Baseline assessment completion | # completing baseline assessment/ # enrolled | 15/15 (100%) | 15/17 (88%) |
| Acute intervention retention | # completing acute (6 sessions) treatment / # enrolled | 10/15 (67%) | 11/17 (65%) |
| Maintenance intervention retention | # completing maintenance (sessions 7,8,9) treatment / # enrolled | 10/15 = (67%) | N/A |
| First follow-up assessment retention | # completing second assessment / # enrolled | 9/15 = (60%) | 12/17 (71%) |
| Second follow-up assessment retention | # completing third assessment / # enrolled | 9/15 = (60%) | 11/17 (65%) |
| Third follow-up assessment retention | # completing fourth assessment / # enrolled | N/A | 10/17 (59%) |
In Study 2, most of the attrition occurred before the start of the intervention. Two women withdrew after enrolling but before completing the baseline (one provided demographic information upon enrollment but the other one did not). Another three women withdrew after completing the baseline, but before beginning the intervention (during the six week no-treatment phase). All three of those women were experiencing high levels of depressive and anxiety symptoms at baseline (≥ 5 on baseline HADS and ≥ 7 on baseline HADS). Eleven of the 12 women who began the intervention completed all six sessions; the remaining woman withdrew after one session (saying that she appreciated what the program was trying to accomplish but she felt she had too many medical appointments and work activities to continue participation).
Satisfaction with the Intervention
Table 4 contains the satisfaction data for both studies. The results indicate that the women who completed the program were highly satisfied. When asked to provide details participants’ comments reflected four themes: (1) It helped me to focus on healthy behaviors; (2) It helped me to realize that my abilities are still there and my limitations are acceptable; (3) It gave me inspiration to plan and meet a goal; and (4) It helped to look at things differently and set personal goals.
Table 4.
Participant Satisfaction
| Study 1 n (%)(N = 9) |
Study 2 n (%)(N = 10) |
|
|---|---|---|
| Satisfaction with Study | ||
| Mostly satisfied | 4 (44) | 1 (10) |
| Very satisfied | 5 (56) | 9 (90) |
| Helpfulness of intervention | ||
| Mostly helpful | 2 (22) | 0 |
| Very helpful | 7 (78) | 10 (100) |
| Satisfaction with the intervention | ||
| Neither satisfied nor dissatisfied | 1 (12) | 0 |
| Mostly satisfied | 4 (44) | 3 (30) |
| Very satisfied | 4 (44) | 7 (70) |
| Relevance of topics | ||
| Somewhat irrelevant | 1 (12) | 0 |
| Mostly relevant | 3 (32) | 3 (30) |
| Very relevant | 5 (56) | 7 (70) |
| Satisfaction with therapist | ||
| Mostly satisfied | 2 (22) | 2 (20) |
| Very satisfied | 7 (78) | 8 (80) |
| Satisfaction with length and schedule of sessions | ||
| Mostly satisfied | 4 (44) | 4 (40) |
| Very satisfied | 5 (56) | 6 (60) |
Session Content
Of the 67 completed sessions for Study 2, 19 occurred in the morning (28%), 37 in the afternoon (55%), and 11 in the evening (17%). The first sessions averaged 76 minutes in length (sd = 15) and the subsequent sessions averaged 36 minutes in length (sd = 18). The first session was the longest because the therapist reviewed the rationale for the intervention and asked about the woman’s participation restrictions and long-term goals.
In Study 1, all sessions used Behavioral Activation alone. In Study 2, 85% of the goals were set using Behavioral Activation alone, while Problem-Solving was added to Behavioral Activation to set 15% of the goals. The goals addresseded getting more exercise (28%), managing stress (15%), following physical therapy regimens for upper extremity stretching or lymphedema management (14%), work (10%), instrumental activities of daily living (8%) and other miscellaneous activities. Women addressed an average of 4 different types of activities over the six sessions (range: 2 – 6, mean = 3.8, sd = 1.1).
Potential Efficacy
Goal Attainment
Over both studies, participants were able to meet 64% of the goals they set. We further looked at the unmet goals of Study 2 and calculated a percentage to reflect the amount of success or how close the women came to meeting each goal. For example, if the woman’s goal was to exercise 5 out of 7 days in a week and she exercised 4 days then she did not meet the goal, but came close (4/5 = 80%). Or if a woman set a goal to accomplish 4 tasks and only accomplished two, then we assigned her 50% (2/4). For the unmet goals, the average percentage accomplished was 40% (range 0–83, sd = 31). The women in Study 2 reported on their level of satisfaction with the effort they put in on achieving their goals. They reported an average satisfaction of 7.4 per goal (sd = 1.7) on a scale of 0 to 10 (0 = “not at all satisfied with the effort I put into solving the problem” and 10 = “completely satisfied with the effort I put into solving the problem”; data not collected in Study 1).
Quality of Life
A main effect of time was seen for overall quality of life (F(5, 43.1) = 5.1, p = 0.001). Estimated marginal means indicate that there was no change in quality of life during the no-treatment run in phase of Study 2 (97.0 at Week −6 and 97.7 at Week 0, LSD p = 0.83) and an improvement in quality of life immediately after the acute intervention (scores increased from 97.7 at Week 0 to 107.8 at Week 6 and 107.6 at Week 8, LSD p = 0.009 and 0.007, respectively). There was no significant reduction in quality of life in the follow-up phase of the studies (mean scores at Week 12 = 105.0 and Week 20 = 108.8, LSD ns). All of the subscales of the FACT-B+4 showed a similar main effect of time with the exception of social well-being. The improvement on the total score exceeded five points, which has been found to represent clinically meaningful improvement on the FACT tools (Cella, Hahn, & Dineen, 2002).
Depression
A main effect of time was seen for depression (F(5, 51.2) = 6.0, p < 0.001). Scores generally decreased over time with improvement beginning during the no-treatment run in phase of Study 2 (12.3 at Week −6 and 9.5 at Week 0, LSD p = 0.002). Further improvement was seen after the acute intervention when scores dropped to 7.4 at Week 8 (LSD p = 0.046), but other changes in depressive symptoms were not significantly different when compared to the immediately preceding time point (9.2 at Week 6, LSD p = 0.77; 10.5 at Week 12, LSD p = 0.20; and 5.9 at Week 20, LSD p = 0.18). The same pattern of effects was seen when the analyses were repeated using only data from women who did not withdraw from the study, thus suggesting that it was not a consequence of differential attrition.
Anxiety
A main effect of time was also seen for anxiety (F(5, 47.6) = 4.4, p = 0.002). Similar to depression, improvement began during the no-treatment run-in phase of Study 2 (14.3 at Week −6 and 11.7 at Week 0, LSD p = 0.01). Further significant improvements were seen after the acute intervention when scores dropped to 8.5 at Week 8 (LSD p = 0.01), but other changes in anxiety symptoms were not significantly different when compared to the immediately preceding time point (11.3 at Week 6; 10.9 at Week 12; and 8.9 at Week 20, all LSD ns). The same pattern of effects was seen when the analyses were repeated using only data from women who did not withdraw from the study.
Coping as a Possible Mechanism of Action
A main effect of time was seen for active coping (F (3, 31.7) = 4.9, p = 0.007), planning (F (3, 36.0) = 4.1, p = 0.01), reframing (F (3, 29.3) = 8.5, p < 0.001), and self-blame (F (3,31.6) = 4.3, p = 0.01). The improvements all appeared during acute treatment. Reductions in self-blame were associated with reductions in depression (r(18) = 0.57, p = 0.009) and anxiety (r(17) = 0.44, p = 0.06). The change scores for the other three coping styles were not correlated with changes in quality of life, depression, or anxiety (all r < 0.34, ns).
Discussion
These studies explored the acceptability and potential efficacy of the BA/PS intervention and the feasibility of conducting research on this intervention for the population of breast cancer survivors. Regarding feasibility, our enrollment statistics mirror the research literature: although most women experience satisfactory recovery after treatment, a little more than a third of women report difficulty doing valued activities. The data regarding acceptability and potential efficacy of the BA/PS intervention are encouraging. The participants who completed the intervention reported high satisfaction and found the intervention useful. The relatively high rate of goal attainment and effort satisfaction also supports the usefulness of the intervention. While problem-solving was used only 15% of the time, we feel it is an important component of the intervention that is crucial in the rare circumstances when women do not know exactly how to best meet their goals. To possibly enhance the goal attainment further, we have revised the manual to encourage greater use of the problem-solving steps in situations where the initial goal was not able to be met with participant satisfaction.
Qualitative comments from participants mirror the results regarding quality of life. Quality of life did not change during the no treatment run-in phase, but increased immediately after the intervention and did not decrease over time. These improvements reached thresholds for both statistical and clinical significance. Women also experienced increases in active coping, planning, reframing, and decreases in self-blame during the treatment period. These findings are encouraging as the BA/PS program was specifically designed to help women actively strive to improve their functioning as opposed to waiting for things to improve on their own.
The results for depression and anxiety were less clear. Although we were not specifically targeting depression or anxiety, a) these are problems faced by many survivors and b) Behavioral Activation and Problem-Solving Treatment were originally developed to manage these disorders. The participants demonstrated reductions in both depressive and anxiety symptoms, but those changes began before treatment was initiated. We, therefore, cannot conclude that the intervention itself affects depression and anxiety, although the women showed continued declines over time. The longitudinal analyses of the anxiety and depression scores were robust in that depression and anxiety did tend to resolve over time for both the full sample and for the subsample of people who did not withdraw from the study. This suggests that the main effect of time on depression and anxiety is not an artifact seen simply because the women high on depression and anxiety withdrew early on in the study. However, depressive or anxiety symptoms may preclude sustained participation in rehabilitation interventions and warrant immediate attention in both clinical and research endeavors.
All of the women in the study were uniformly interested in the program, but only two-thirds were able to complete the intervention and study activities. It is possible that study features could have affected the attrition rate. In Study 1, most of the women (13/15) were treated by one nurse practitioner who had limited availability. This may have made it too difficult for some women to participate and it is possible that some of the attrition was due to this reduced amount of flexibility in scheduling. In Study 2, the interventionist had more flexibility and scheduled calls at the participants’ convenience. All but one woman who started the intervention completed it in Study 2, with all others withdrawing during the no treatment run-in phase. It is possible that women who enrolled hoping to receive a benefit from the intervention may have been discouraged by the no treatment phase and the need to do a second survey before beginning the intervention. The project coordinator conducting the surveys was also only available during daytime hours. It is notable that when asked about their reasons for withdrawal women reported being too busy to continue with the study as opposed to no longer needing the intervention. It is also notable that most of the women who withdrew were experiencing clinically significant depressive and anxiety symptoms, as detected by the HADS at baseline. To improve the feasibility of conducting future research on this intervention with this population we recommend the following strategies. First, all study personnel need to be available during evening hours of weekdays to accommodate busy and working participants. Second, it may be wise to explicitly screen for depression and anxiety upon enrollment so that women with depressive or anxious symptoms have immediate access to mental health treatment as these symptoms may preclude effective participation in rehabilitation. Finally, a randomized design that eliminates the no-treatment phase and offers an attention control group may maximize study retention.
Limitations and Future Research
The findings need to be considered in light of several limitations. In order to gain more experience delivering the intervention, we did not use a control group to identify what changes may naturally occur over time. This limits our ability to infer that any changes were due to our intervention, although the fact that many of the changes did not occur until after the run in phase and concurrently with treatment are suggestive of a specific intervention effect. Also, there was only one interventionist in each of the studies. While we were able to train two different people to do the intervention, the findings of each study may not reflect what would occur in the hands of other interventionists. As we train more interventionists to conduct the intervention, we are also exploring how to standardize the process of how the interventionist decides whether to encourage the use of PST over BA, possibly by incorporating instruments that assess problem-solving efficacy. Finally, although the sample reflected the demographics of Northern New England (primarily Caucasian), we do not know how women of other ethnic/racial groups would experience the intervention. Further, the women who withdrew did not complete the remaining assessments (with one exception), thus limiting our ability to describe the overall effectiveness of the program.
Future research is needed to explore both the efficacy and sustainability of the intervention. In subsequent studies we plan to utilize an attention control condition (e.g., supportive therapy) and assess the psychometrics of the fidelity monitoring worksheet we developed, comparing the scores of two blinded raters. We also plan to explore models of delivery, comparing ways the intervention could be reimbursed as a stand-alone telerehabilitation method or used to complement and augment another rehabilitative technique.
Conclusion
These two pilot studies indicate that a telephone-delivered BA/PS intervention may help breast cancer survivors to meet their personal recovery goals and catalyze their functional recovery. Further work is warranted with larger, diverse samples that include control conditions to determine the efficacy of intervention. The attrition rate indicates the need for brief, timely and accessible interventions for this busy, stressed, and hard-to-reach subgroup of women. More work is needed to determine models of care that could best meet the needs of women who report reduced functional recovery but feel too busy or overwhelmed to engage in a clinical trial.
Acknowledgments
These studies were funded by grants to Dr. Hegel from the Cancer and Leukemia Group B Foundation (now the Alliance for Clinical Trials in Oncology Foundation; #70804; Study 1) and the National Cancer Institute (1 R21 CA140849-01; Study 2). The first author was supported by a Mentored Research Scholar Grant in Applied and Clinical Research, MRSG-12-113-01 –CPPB from the American Cancer Society.
The authors appreciate the contributions of Elaine Owen, APRN of Central Vermont Medical Center in Vermont, and Wendy Bayles-Dazet, APRN and Daphne Ellis, both of Dartmouth College.
References
- American Cancer Society; AC Society, editor. Breast Cancer facts and Figures 2013–2014. Atlanta: 2013. [Google Scholar]
- Bakitas M, Lyons KD, Hegel MT, Balan S, Barnett KN, Brokaw FC, Ahles TA. The Project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: Baseline findings, methodological challenges, and solutions. Palliative and Supportive Care. 2009;7:75–86. doi: 10.1017/S1478951509000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakitas M, Stevens M, Ahles T, Kirn M, Skalla K, Kane N, Greenberg R. Project ENABLE: A palliative care demonstration project for advanced cancer patients in three settings. Journal of Palliative Medicine. 2004;7(2):363–372. doi: 10.1089/109662104773709530. [DOI] [PubMed] [Google Scholar]
- Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, Shiomoto G. Reliability and validity of the functional assessment of cancer therapy - Breast Quality-of-Life instrument. Journal of Clinical Oncology. 1997;15(3):974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. doi: 10.1097/01.MLR.0000024610.33213.C8. [DOI] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychologyl. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Cella D, Hahn EA, Dineen K. Meaningful change in cancer-specific quality of life scores: Differences between improvement and worsening. Quality of Life Research. 2002;11:207–221. doi: 10.1023/a:1015276414526. [DOI] [PubMed] [Google Scholar]
- Coster S, Poole K, Fallowfield LJ. The validation of a quality of life scale to assess the impact of arm morbidity in breast cancer patients post-operatively. Breast Cancer Research and Treatment. 2001;68(3):273–282. doi: 10.1023/a:1012278023233. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007a;27(3):318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Warmerdam L. Problem solving therapies for depression: A meta-analysis. European Psychiatry. 2007b;22(1):9–15. doi: 10.1016/j.eurpsy.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Deshields T, Tibbs T, Fan MY, Bayer L, Taylor M, Fisher E. Ending treatment: the course of emotional adjustment and quality of life among breast cancer survivors immediately following radiation therapy. Supportive Cancer Care. 2005;13:1018–1026. doi: 10.1007/s00520-005-0801-z. [DOI] [PubMed] [Google Scholar]
- Egan MY, McEwen S, Sikora L, Chasen M, Fitch M, Eldred S. Rehabilitation following cancer treatment. Disability and Rehabilitation. 2013;35(26):2245–2258. doi: 10.3109/09638288.2013.774441. [DOI] [PubMed] [Google Scholar]
- Fillion L, Kovacs A, Gagnon P, Endler N. Validation of the Shortened COPE for use with Breast Cancer Patients Undergoing Radiation Therapy. Current Psychology. 2002;21(1):17–34. [Google Scholar]
- Hauglann B, Benth JS, Fossa SD, Dahl AA. A cohort study of permanently reduced work ability in breast cancer patients. Journal of Cancer Survivorship. 2012;6(3):345–356. doi: 10.1007/s11764-012-0215-0. [DOI] [PubMed] [Google Scholar]
- Hegel MT, Arean PA. Problem-solving treatment for primary care:A treatment manual for depression, Project IMPACT. Hanover, NH: Dartmouth College; 2003. [Google Scholar]
- Hegel MT, Lyons KD, Hull JG, Kaufman P, Urquhart L, Li Z, Ahles TA. Feasibility study of a randomized controlled trial of a telephone-delivered problem-solving-occupational therapy intervention to reduce participation restrictions in rural breast cancer survivors undergoing chemotherapy. Psychooncology. 2011;20(10):1092–1101. doi: 10.1002/pon.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin ML, Crumley D, McTiernan A, Bernstein L, Baumgartner R, Gilliland FD, Ballard-Barbash R. Physical activity levels before and after a diagnosis of breast carcinoma: the Health, Eating, Activity, and Lifestyle (HEAL) study. Cancer. 2003;97(7):1746–1757. doi: 10.1002/cncr.11227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, LePage JP, Hopko SD, McNeil DW. A brief behavioral activation treatment for depression. Cognitive and Behavioral Practice. 2001;8(2):164–175. http://dx.doi.org/10.1016/S1077-7229(01)80022-5. [Google Scholar]
- Littman AJ, Tang MT, Rossing MA. Longitudinal study of recreational physical activity in breast cancer survivors. Journal of Cancer Survivorship. 2010;4(2):119–127. doi: 10.1007/s11764-009-0113-2. [DOI] [PubMed] [Google Scholar]
- Lyons KD, Hegel MT, Hull JG, Li Z, Balan S, Bartels S. Reliability and validity of the Valued Activity Inventory for Adults with Cancer. OTJR: Occupation, Participation and Health. 2012;32(1):238–245. doi: 10.3928/15394492-20110623-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons KD, Svensborn IA, Kornblith AB, Hegel MT. A content analysis of recovery strategies of breast cancer survivors enrolled in a goal-setting intervention. OTJR: Occupation, Participation and Health. doi: 10.1177/1539449214567306. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney C, Lyons KD, Li Z, Hegel M, Ahles TA, Bakitas M. Patient perspectives on participation in the ENABLE II randomized controlled trial of a concurrent oncology palliative care intervention: Benefits and burdens. Palliative Medicine. 2013;27(4):375–383. doi: 10.1177/0269216312445188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. British Journal of Psychiatry. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Ness KK, Wall MM, Oakes JM, Robison LL, Gurney JG. Physical performance limitations and participation restrictions among cancer survivors: a population-based study. Annals of Epidemiology. 2006;16(3):197–205. doi: 10.1016/j.annepidem.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Penttinen HM, Saarto T, Kellokumpu-Lehtinen P, Blomqvist C, Huovinen R, Kautiainen H, Hakamies-Blomqvist L. Quality of life and physical performance and activity of breast cancer patients after adjuvant treatments. Psychooncology. 2011;20(11):1211–1220. doi: 10.1002/pon.1837. [DOI] [PubMed] [Google Scholar]
- Torp S, Nielsen RA, Gudbergsson SB, Fossa SD, Dahl AA. Sick leave patterns among 5-year cancer survivors: a registry-based retrospective cohort study. Journal of Cancer Survivorship. 2012;6(3):315–323. doi: 10.1007/s11764-012-0228-8. [DOI] [PubMed] [Google Scholar]
- Vodermaier A, Millman R. Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: a systematic review and meta-analysis. Supportive Care in Cancer. 2011;19(12):1899–1908. doi: 10.1007/s00520-011-1251-4. [DOI] [PubMed] [Google Scholar]
- Zigmond A, Snaith R. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]