Abstract
Objectives:
Diagnosis of hearing loss and prescription of amplification for infants and young children require accurate estimates of ear- and frequency-specific behavioral thresholds based on auditory brainstem response measurements. Although the overall relationship between ABR and behavioral thresholds has been demonstrated, the agreement is imperfect, and the accuracy of predictions of behavioral threshold based on ABR may depend on degree of hearing loss. Behavioral thresholds are lower than ABR thresholds, at least in part due to differences in calibration interacting with the effects of temporal integration, which are manifest in behavioral measurements but not ABR measurements and depend on behavioral threshold. Listeners with sensory hearing loss exhibit reduced or absent temporal integration, which could impact the relationship between ABR and behavioral thresholds as degree of hearing loss increases. The current study evaluated the relationship between ABR and behavioral thresholds in infants and children over a range of hearing thresholds, and tested an approach for adjusting the correction factor based on degree of hearing loss as estimated by ABR measurements.
Design:
A retrospective review of clinical records was completed for 309 ears of 177 children with hearing thresholds ranging from normal to profound hearing loss and for whom both ABR and behavioral thresholds were available. Children were required to have the same middle-ear status at both evaluations. The relationship between ABR and behavioral thresholds was examined. Factors that potentially could affect the relationship between ABR and behavioral thresholds were analyzed, including degree of hearing loss observed on the ABR, behavioral test method (visual reinforcement, conditioned play or conventional audiometry), the length of time between ABR and behavioral assessments, and clinician-reported reliability of the behavioral assessment. Predictive accuracy of a correction factor based on the difference between ABR and behavioral thresholds as a function of ABR threshold was compared to the predictive accuracy achieved by two other correction approaches in current clinical use.
Results:
As expected, ABR threshold was a significant predictor of behavioral threshold. The relationship between ABR and behavioral thresholds varied as a function of degree of hearing loss. The test method, length of time between assessments and reported reliability of the behavioral test results were not related to the difference between ABR and behavioral thresholds. A correction factor based on the linear relationship between the differences in ABR and behavioral thresholds as a function of ABR threshold resulted in more accurately predicted behavioral thresholds than other correction factors in clinical use.
Conclusions:
ABR is a valid predictor of behavioral threshold in infants and children. A correction factor that accounts for the effect of degree of hearing loss on the difference between ABR and behavioral thresholds resulted in more accurate predictions of behavioral thresholds than methods that used a constant correction factor regardless of degree of hearing loss. These results are consistent with predictions based on previous research on temporal integration for listeners with hearing loss.
INTRODUCTION
Identification of hearing loss and provision of amplification within the timeframe recommended by the Joint Committee on Infant Hearing (American Academy of Pediatrics, 2007) requires estimates of infants’ hearing thresholds using electrophysiological tests. The auditory brainstem response (ABR) is the most widely studied method of hearing-threshold estimation in infants and young children for whom behavioral assessment of hearing is not feasible. ABR thresholds are the basis for diagnostic assessment performed after newborn hearing screening that either indicates that a child has normal peripheral hearing sensitivity or quantifies the degree and configuration of hearing loss. If hearing loss is confirmed, ear-specific estimates of behavioral threshold based on the ABR are used to prescribe amplification (Bagatto et al. 2010). Inaccurate estimates of behavioral threshold from ABR could lead to inappropriate diagnoses of hearing loss in children with normal hearing. It is also possible to obtain incorrect estimates of behavioral thresholds based on ABR measurements for children with hearing loss. For example, underestimation of thresholds could limit speech audibility with amplification, and, in turn, negatively impact speech and language development (e.g., Tomblin et al. 2013; Koehlinger et al. 2013). In contrast, overestimation of thresholds could lead to over-amplification, leading to hearing damage from exposure to unnecessarily high sound levels (Ching et al. 2013; Macrae 1994; 1995). Thus, there is value in continued efforts to improve the accuracy with which behavioral thresholds are predicted from ABR measurements.
The relationship between ABR and behavioral threshold has been described previously for infants, children, and adults with normal hearing and with hearing loss. Stapells (2000) provided a meta-analysis that included tone-burst ABR results from over 1200 adults and children taken from 32 studies, including approximately 125 infants and children with sensorineural hearing loss. For tone-burst stimuli at octave frequencies from 500 Hz to 4000 Hz, ABR thresholds predicted behavioral thresholds to within 5-10 dB in approximately 95% of cases. Subsequent studies have supported the conclusion that ABR thresholds accurately predict behavioral thresholds in children with normal hearing (Rance et al. 2006; Gorga et al. 2006; Lee et al. 2008; Vander Werff et al. 2009) and children with hearing loss (Gorga et al. 2006; Lee et al. 2008; Vander Werff et al. 2009). The accuracy of predictions, however, are frequency dependent; predictions of behavioral threshold based on ABR tend to be more accurate and less variable for 2000 Hz and 4000 Hz than for 500 Hz and 1000 Hz (Lee et al. 2008; Vander Werff et al. 2009). Overall, these results support the clinical utility of ABR as a useful predictor of hearing sensitivity in infants and young children. In the absence of progressive or fluctuating hearing loss, the relationship between ABR and behavioral thresholds exists regardless of whether the measures are obtained in close temporal proximity (e.g. Lee et al. 2008) or when the time period between assessments is similar to the extended timeframe that often occurs clinically (e.g. Gorga et al. 2006).
Two approaches have been followed in efforts to estimate audiometric thresholds from ABR thresholds: behavioral correction alone (BEH; Gorga et al. 2006) and behavioral correction followed by corrections based on ABR thresholds (BEH/ABR; Vander Werff et al. 2009; Bagatto et al. 2010). In both approaches, the normal level (0 dB nHL) for ABR stimuli are calibrated by measuring the behavioral thresholds for the stimuli that will be used during ABR measurements in a group of adults with normal hearing. The peak or peak-equivalent SPL levels of the average behavioral thresholds for the ABR stimuli at each test frequency are defined as 0 dB nHL. In addition to determining the 0 dB nHL level for each ABR stimulus frequency, the BEH/ABR correction approach also subtracts a correction from the clinically observed ABR threshold to estimate audiometric threshold at each test frequency. The correction factor at each frequency is determined by the difference between the average ABR threshold for adults with normal hearing in dB nHL and the behavioral threshold at that frequency in dB HL. Frequency-specific BEH/ABR correction factors have been described by Vander Werff (2009), Bagatto et al. (2010) and Stapells (2011). An example of correction factors derived from this approach are 15 dB, 10 dB, 5 dB and 0 dB for 500, 1000, 2000, and 4000 Hz, respectively (Bagatto et al. 2010). The BEH correction approach does not apply an additional correction to the ABR threshold. Rather, ABR thresholds are used to directly predict audiometric thresholds without additional corrections beyond those that occur as part of the calibration procedure. Whether BEH or BEH/ABR corrections are used, neither approach takes the listener’s degree of hearing loss into account when predicting behavioral thresholds.
Despite the consistent relationship between ABR and behavioral thresholds across multiple studies, predictions of behavioral thresholds from ABR thresholds may vary as a function of degree of hearing loss. For example, Gorga and colleagues (2006) found that the difference between ABR and behavioral thresholds depended on the degree of hearing loss. ABR overestimated behavioral thresholds in children with normal hearing due, in part, to the fact that ABR measurements were terminated when an ABR was observed at 20 dB nHL, which was considered to be normal. However, lower intensity levels were evaluated during behavioral assessment. In contrast, for children with moderate or greater degrees of hearing loss, the ABR underestimated behavioral threshold by as much as 20 dB, depending on stimulus frequency. These differences were evident despite the fact that the overall correlations between ABR and behavioral thresholds ranged from 0.92 to 0.95 for tonal stimuli for frequencies from 250 Hz through 4000 Hz, and for click stimuli, when clicks were used to predict behavioral thresholds at 2000 Hz and 4000 Hz. Lee et al. (2008) also reported results to suggest that the difference between ABR and behavioral threshold varied across degree of hearing loss.
However, a comparison of different correction factors by Vander Werff and colleagues (2009) observed that applying different frequency-specific correction factors did not affect the correlation between ABR and behavioral measures. These observations may not be surprising because the correlation between the two threshold measures represents the slope of the linear relationship, which is not altered by the subtraction of a constant value. This suggests that correlations between ABR and behavioral thresholds may not completely describe changes in threshold-prediction accuracy following the application of correction factors whose values are constant. There may be value in taking this threshold-dependent relationship into account when developing correction factors in order to bring the two measurements into closer agreement. This approach differs from previous efforts in that the correction factor is not constant, but varies with ABR threshold.
An explanation for the tendency of ABR to overestimate behavioral thresholds in individuals with normal hearing and underestimate behavioral threshold in patients with greater than mild degrees of hearing loss was proposed by Gorga et al. (2006). They suggest that this effect is related to an interaction between differences in temporal integration between listeners with normal hearing and those with hearing loss and the typical way in which stimulus level is calibrated for ABR measurements. Temporal integration refers to the dependence of behavioral threshold on stimulus duration, with short-duration sounds requiring higher levels for detection, compared to sounds of longer duration. Generally, behavioral thresholds are constant for durations greater than or equal to 300-500 ms, but increase by 10 dB for every 10-fold decrease in stimulus duration (Watson & Gengel, 1969). Thus, the threshold for a 30-ms tone burst is expected to be about 10 dB higher than it is for a 300-ms tone, and the threshold for 3-ms tone burst would be expected to be about 20 dB higher than it is for the long-duration tone. In contrast, listeners with cochlear hearing loss show reduced or absent temporal integration (Wright, 1968; Gengel & Watson, 1971; Reed, Braida & Zurek, 2009). That is, the difference in behavioral thresholds for short- and long-duration stimuli are less when hearing loss exists. The amount of temporal integration in listeners with normal hearing also depends on stimulus frequency with the larger durational effects on threshold at low frequencies (250 Hz) and smaller effects as frequency increases up to 4000 Hz (Watson & Gengel, 1969). The ABR is typically elicited using short-duration stimuli that differ in duration from the pure tones used in behavioral audiometry. Given the shorter stimulus duration for ABR measurements compared to the stimuli used for behavioral assessment, ABR thresholds tend to be approximately 10-20 dB higher than behavioral thresholds at the same frequency for listeners with normal hearing. The difference between ABR thresholds and behavioral thresholds would be predicted to be less in listeners with hearing loss.
Current clinical practices for predicting behavioral thresholds from ABR thresholds implicitly assume that differences in threshold between the stimuli used for ABR and behavioral assessments are constant for listeners with normal hearing and all degrees of sensorineural hearing loss. Thus, correction factors, whether applied to the calibration or to ABR thresholds, are constant regardless of the ABR threshold. However, as noted above, listeners with sensorineural hearing loss exhibit less temporal integration than listeners with normal hearing (Wright, 1968; see also Reed, Braida & Zurek, 2009 for review). Subtracting a constant correction factor from the ABR threshold for a listener with sensorineural hearing loss who exhibits less temporal integration than a person with normal hearing could result in an underestimation of behavioral threshold. If temporal integration decreases as the degree of hearing loss increases, the underestimation created by a constant correction factor also would be expected to increase as hearing loss increases.
Results reported by Gorga et al. (2006) are consistent with the above hypothesis. They observed that ABR thresholds underestimated behavioral thresholds for listeners with moderate or greater degrees of hearing loss and that the difference increased systematically as thresholds increased. However, data from Gorga et al. (2006) at 2000 and 4000 Hz were limited by the clinical practice at that time of using click-evoked ABRs to estimate hearing at high frequencies. Despite the strong relationship between clicks and high-frequency behavioral thresholds in that study and others (Baldwin & Watkin, 2013), tone-burst data at 2000 Hz and 4000 Hz would allow for a more direct comparison of the relationship between ABR threshold and behavioral threshold across a range of frequencies that are important for the diagnosis of hearing loss and for the prescription of amplification for infants. Additionally, the data from Gorga et al. were reported as a function of degree of behavioral threshold, which typically is not available at the time that the ABR is conducted; thus, the data could not be used to generate a correction that could be applied directly to ABR thresholds.
The purpose of the current study was to further analyze the relationship between ABR thresholds and behavioral thresholds in children with behavioral thresholds ranging from normal to profound hearing loss using a retrospective analysis of a large clinical sample of ABR and behavioral audiometric data. These data were used to develop an approach to analyses that reduced the variance of the differences between threshold estimations. We predicted that a relationship between ABR and behavioral threshold will be observed, as in previous studies, but can be improved by applying threshold-dependent corrections. An objective of this study was to develop and assess the validity of an approach such that the magnitude of the correction depends on the degree of hearing loss estimated by the ABR. The differences between ABR and behavioral thresholds observed using this approach were compared to those observed when using conventional approaches that use correction factors that do not vary as a function of degree of hearing loss. Reducing the correction factor as hearing loss increases is in accordance with predictions of reduced temporal integration for listeners with hearing loss. Age, the amount of time between ABR and behavioral assessment, and audiological variables such as reliability and assessment method from the behavioral assessment, were also analyzed as potential contributing factors.
METHOD
Participants
Retrospective data were analyzed for 309 ears (161 right ears and 148 left ears) from 177 children who received clinical ABR evaluation and behavioral audiological assessment at Boys Town National Research Hospital. In order to be included in the sample, the children had to have the same middle-ear status (i.e., either normal middle-ear status or patent tympanostomy tubes based on tympanometry) for both behavioral and ABR evaluations and have behavioral results, the reliability of which had to be judged as fair or good by the pediatric audiologists who performed the assessment. When ABR or behavioral thresholds exceeded the maximum stimulus levels produced by the hardware for either assessment, those data were not included in the analysis. Ears with evidence of auditory neuropathy spectrum disorder (based on the presence of cochlear microphonic or distortion-product otoacoustic emissions and absent or grossly abnormal ABRs) were not included in the sample due to known discrepancies between ABR and behavioral thresholds in children with this disorder (e.g., Rance, 2005). For the purposes of simplicity, ears with conductive hearing loss were not included in the analyses as well. The average age at the time of the ABR was 24.4 months (Median = 18 months; Range = 0 – 210 months; SD = 32.3) and the average age at the time of behavioral assessment was 38.2 months (Median = 33 months; Range = 6 – 210 months; SD = 30.03). Nine children received behavioral testing prior to ABR evaluation, 42 children received ABR and behavioral evaluations on the same day, and 126 children received the ABR evaluation prior to the behavioral assessment. The average time between ABR and behavioral assessments was 13.8 months (Median = 9 months; Range = −55 – 77 months; SD= 17.7).
ABR assessment
Stimuli
The primary stimuli used to estimate frequency-specific thresholds were Blackman-windowed tone bursts with nominal frequencies of 250, 1000, 2000 and 4000 Hz. The 250-Hz and 1000-Hz tone bursts had a 2-ms rise and fall times with no plateau. The windowing durations at 1000, 2000, and 4000 Hz represent a compromise between uniform duration in milliseconds and uniform duration in sinewave cycles. The 2000 and 4000 Hz tone bursts had 1.5 ms and 1 ms rise/fall times, respectively, with no plateau. The 250-Hz, single-cycle tone burst has a broad low-frequency bandwidth with energy up to 600 Hz and little energy above this frequency as a result of the Blackman window. Previous data have shown that the ABR thresholds to this stimulus correlate with behavioral thresholds at both 250 and 500 Hz (Gorga et al. 1991; Gorga et al. 2006). For this reason, a 500-Hz toneburst was not included in the stimulus set. Rarefaction clicks (100 μs) were also used to provide an efficient test for auditory neuropathy, to provide guidance for ABR responses elicited with tone bursts, and to provide information about high-frequency hearing sensitivity in addition to the data obtained with high-frequency tone bursts. Stimuli were presented at a rate of either 27 or 37/second. For all stimuli (clicks and tone bursts), stimuli were presented at a fixed phase/polarity characterized by a negative-going pressure at their onset.
Calibration
The peak SPL (pSPL) values for 0 dB nHL for 250, 1000, 2000, and 4000 Hz tone burst and the click were 43, 24, 28, 32, and 35 dB pSPL, respectively (Gorga et al., 2006). The maximum stimulus levels were 90 dB nHL at 250 Hz and 105 dB nHL for all other stimuli.
EEG recording parameters
Brain activity was amplified with gain set at 100,000 and a band pass filter of 30 to 3000 for 250 Hz tone burst and 100 to 3000 Hz for all other ABR stimuli. The high-pass filter setting for 250 Hz was selected because evidence suggests that the ABR response for stimulus frequencies less than 1000 Hz may contain more low frequency energy than the responses to stimuli with higher nominal frequencies (e.g. Takagi, Suzuki & Kobayashi, 1985). A single-channel electrode montage was used with one electrode placed on the high forehead (Fz) and one electrode behind each ear on the mastoid process. The ground electrode was the mastoid electrode contralateral to the test ear. Electrode impedances were less than 5 kΩ prior to testing.
Procedure
ABR evaluations were completed in a sound-treated audiometric test booth or surgical operating room using a Biologic Navigator Pro system (Natus Medical Inc.), and stimuli were delivered with insert earphones. For infants less than 3 months-old, ABR testing was completed during natural sleep. Infants between 3 and 6 months-old were tested during natural sleep whenever possible. Infants 3-6 months-old who could not be tested in natural sleep and children over 6 months-old were tested under sedation administered by a physician and following appropriate monitoring protocols, either with oral chloral hydrate (now discontinued) or under general anesthesia (current protocol).
A minimum of 1000 stimuli were averaged for each response, which was increased to 2000 stimuli for tone bursts and for levels near threshold. Each response was usually replicated unless a clear response was evident after one average; measurements near ABR threshold always included a minimum of two tracings. Initial changes in the stimulus level were in 20-dB steps if a response was observed. Near threshold, stimulus-level step size was reduced to 10 dB. The order of the test stimuli and the number of frequencies tested were dependent on the level of arousal of the child. Generally, the test began with a 4000-Hz tone burst or click in each ear, followed by 250-Hz tone bursts. Based on the results obtained up to that point and the state of arousal of the child, either 1000-Hz tone bursts or 2000-Hz tone bursts were tested next. ABR responses obtained at 20 dB nHL were considered to be within the normal range; thus, levels less than 20 dB nHL were not usually tested in the interest of time. The average number of ABR thresholds obtained for each ear was 3.2 (range = 1-5).
Behavioral assessment
Behavioral assessments were completed in a sound-treated audiometric test booth using insert earphones (n = 136) or TDH-49 circumaural headphones (n = 41). Age-appropriate assessment techniques were used, including visual reinforcement audiometry (VRA; n=84), conditioned play audiometry (CPA; n =75) or conventional audiometry (n = 18). For all behavioral assessments, the stimuli were pure tones at octave test frequencies. Similar to the order of test frequencies for ABR assessment, the order that frequencies were tested was intended to yield a range of frequency-specific values in the event that the child stopped participating in the assessment. Testing generally began with 2000 Hz in each ear, followed by 500, 4000 and 1000 Hz. A test assistant or a second pediatric audiologist participated during behavioral assessments in which VRA and CPA were used.
For VRA, the child was seated on the lap of a parent or caregiver with an audiologist or test assistant in front of the child to direct the child’s attention forward. Visual reinforcement occurred with either lighted mechanical toys within tinted plastic boxes or animated pictures or videos presented via personal computer through LCD monitors. To link the visual reinforcement with the stimulus, pure tones were presented at approximately 60 dB HL, which was assumed to be a suprathreshold level for most children. The pure tone was paired with the visual reinforcement until a reliable response to the stimulus was observed. If a response was not observed at 60 dB HL, the level of the pure tone was increased until a response was observed. Once reliable responses were observed at a suprathreshold level, the level of the stimulus was decreased in 10-dB steps until the child did not respond. After a no response, the level of the stimulus was increased by 5 dB. This bracketing process was repeated until a response was observed at a minimum of two out of three trials at a specific intensity level, but not at the intensity level that was 5 dB lower.
For CPA, the child was seated either on the parent’s or caregiver’s lap or on a small chair at a table in an audiometric test booth. The test assistant or second audiologist presented the child with a play task using toys or a response button. The response button was not linked to a computer, but the audiologist completing the test could activate animation or computer games on an LCD monitor when the child appropriately pushed the button in response to a stimulus. Similar to VRA, pure-tone stimuli were presented at what were presumed to be suprathreshold levels to link the stimulus and the play response. Once conditioning was established, the same approach that was described for VRA was used to establish thresholds. The reliability of the behavioral audiometric test as reported by the pediatric audiologist performing the test was good (n = 89), good-fair (n=68) or fair (n = 20).
Statistical analyses
All statistical analyses were completed in the R software interface (Version 3.0.2; R Core Team, 2014). Bivariate correlations were used to analyze the relationship between ABR and behavioral thresholds at each test frequency. Linear regressions were used to analyze the influence of continuous factors (degree of hearing loss, age at the time of the behavioral assessment, and length of time between the ABR and behavioral evaluation) on the difference between ABR and behavioral thresholds. Mean differences for categorical variables, including the behavioral test method and behavioral test reliability, were evaluated using analyses of variance (ANOVA). Two-fold cross-validation was applied to the data set to determine if two random sub-samples of the data yielded similar estimates of a linear regression correction factor. The estimation errors for the three different correction-factor approaches (BEH correction, BEH/ABR correction and linear regression) were compared using multivariate analysis of variance (MANOVA) at each test frequency. Note that, unlike Gorga et al. (2006; see Figure 6), where the independent variable was behavioral audiometric threshold, ABR threshold was used as the independent variable in the present analyses. This approach is more appropriate clinically, compared to the previous analysis, as the goal is to predict audiometric threshold from ABR threshold. The time between ABR and behavioral threshold in months was included in regression analyses because the time separation between these two measurements varied widely for the study sample. The age in months at behavioral evaluation was also included in the model, as previous studies have suggested that behavioral thresholds improve with age (e.g. Parry et al. 2003).
RESULTS
ABR threshold as a predictor of behavioral threshold
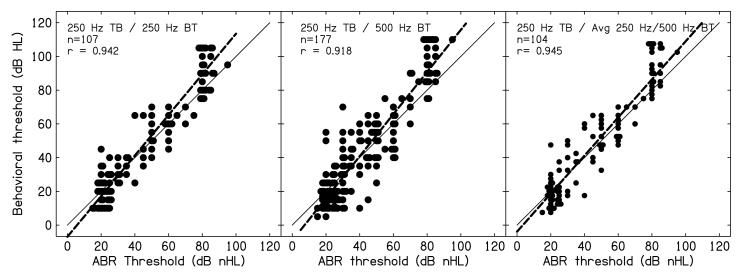
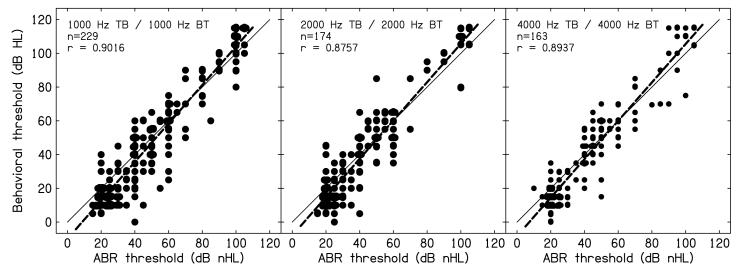
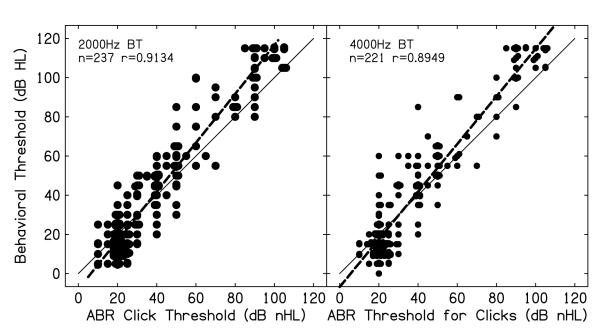
Figure 1 displays the relationship between ABR threshold for a 250-Hz tone burst and behavioral thresholds at 250 Hz, 500 Hz and the average of 250 Hz and 500 Hz. Figure 2 displays the relationship between ABR threshold for 1000, 2000, and 4000 Hz tone bursts and the behavioral thresholds at those frequencies. Figure 3 displays the relationship between ABR threshold for clicks and 2000 Hz and 4000 Hz behavioral thresholds. The slopes of best-fit lines to the data in each panel suggest that behavioral thresholds maybe overestimated when hearing is normal and underestimated when significant hearing loss exists. This pattern was observed in every panel of Figs. 1-3. Nonetheless, the correlations between ABR threshold and behavioral threshold are greater than r = 0.87 for all stimulus conditions, suggesting correspondence between these measures at each test frequency. The average differences between ABR and behavioral threshold for each condition are reported in Table 1. On average, the differences were close to zero, with standard deviations of about 10-12 dB. However, the range of these differences was large. These results indicate that the ABR predicts behavioral threshold across different stimulus frequencies, but not without errors.
Figure 1.
Behavioral thresholds (BT) as a function of ABR thresholds for a 250-Hz tone burst. Left panel: 250-Hz behavioral threshold; middle panel: 500-Hz behavioral threshold; right panel: Average behavioral threshold at 250 and 500 Hz. The number of observations (n) and the correlations are provided within each panel. The solid thin line is provided as a reference and has a slope of one. The dashed line represents a best-fit line to the data in each panel, and has a slope greater than one.
Figure 2.
Behavioral thresholds (BT) as a function of auditory brainstem response (ABR) thresholds for 1000 Hz (left panel), 2000 Hz (middle panel), and 4000 Hz (right panel). The number of observations (n) and the correlations are provided within each panel. The solid thin line is provided as a reference and has a slope of one. The dashed line represents a best-fit line to the data in each panel, and has a slope greater than one.
Figure 3.
Behavioral thresholds (BT) as a function of auditory brainstem response (ABR) thresholds at 2000 Hz (Left panel) and 4000 Hz (Right panel) as a function of click-evoked auditory brainstem response (ABR) thresholds. The solid thin line is provided as a reference and has a slope of one. The dashed line represents a best-fit line to the data in each panel, and has a slope greater than one.
Table 1.
Mean difference between ABR threshold and behavioral threshold
| Mean (dB) | Standard Deviation | Range (ABR – Behavioral) | |
|---|---|---|---|
| 250 Hz | −0.71 | 10.4 | −25 – 25 |
| 500 Hz* | −0.03 | 12.1 | −20 – 40 |
| 1000 Hz | 3.1 | 11.1 | −20 – 40 |
| 2000 Hz | 2.3 | 11.0 | −35 – 35 |
| Click – 2000 Hz BT | −1.2 | 11.6 | −40 – 20 |
| 4000 Hz | 2.2 | 10.3 | −25 – 35 |
| Click – 4000 Hz BT | −1.5 | 12.3 | −45 – 20 |
500 Hz behavioral threshold predicted by 250 Hz tone burst. BT= behavioral threshold
Factors influencing differences between ABR threshold and behavioral threshold
To test the hypothesis that the difference between ABR and behavioral thresholds varied as a function of degree of hearing loss, the relationship between the ABR/behavioral threshold difference and the ABR threshold was examined using linear regression. Table 2 summarizes the results of linear regression for each frequency. Results suggested that the relationship between ABR and behavioral threshold varied significantly as a function of degree of hearing loss on the ABR, controlling for the time between ABR and behavioral assessment and the child’s age when behavioral thresholds were measured. Based on the standardized regression coefficients at each frequency, the correspondence between ABR threshold and behavioral threshold decreased approximately 1 dB for every 3 dB increase in ABR threshold, controlling for the length of time between assessments and the child’s age at the behavioral hearing evaluation (Range of β across stimulus frequency −0.306 to −0.348). ABR threshold accounted for 12-18% of the variance (see Model R2 in Table 2) of the difference between ABR and behavioral thresholds depending on the test frequency. Thus, these statistical results support the hypothesis that difference between ABR and behavioral threshold depended on the degree of hearing loss. Length of time between ABR and behavioral assessments was not a significant predictor of the difference between the two measures at any test frequency (range of β = 0.04 – 0.07, range of p = 0.10 - 0.55).
Table 2.
Linear regression analyses between ABR-BT difference as a function of ABR threshold
| Model R2 | β for ABR threshold | p value | |
|---|---|---|---|
| 250 Hz | 0.18 | −.313 | <0.001 |
| 1000 Hz | 0.12 | −.333 | <0.001 |
| 2000 Hz | 0.16 | −.306 | <0.001 |
| 4000 Hz | 0.13 | −.348 | <0.001 |
Controlling for length of time (months) between ABR and behavioral assessment and age at behavioral
The influence of behavioral-assessment method and reliability on the accuracy of ABR predictions of behavioral threshold were analyzed using a repeated-measures MANOVA with the assessment method (VRA, CPA and Conventional) and reliability (Good, Good-Fair, and Fair) as between-subjects factors. The multivariate effect of frequency was significant [F(3,108) = 5.985, Wilks λ = 0.857, p= 0.001], indicating that the difference between ABR threshold and behavioral threshold varied significantly across frequencies. Post-hoc testing (Tukey’s Honestly Significant Difference; HSD) with a minimum mean significant difference of 3.5 dB indicated that the ABR-behavioral threshold difference was significantly lower at 500 Hz (−2.1 dB) than at 1000 Hz (4.9 dB) and 2000 Hz (3.6 dB), but not significantly different at 4000 Hz (0.7 dB). The difference between 1000 Hz and 4000 Hz (4.2 dB) was also significant. The main effect of frequency in this analysis represents the average difference at each frequency, but does not reflect the significant effect of degree of hearing loss on the difference between ABR and behavioral thresholds that was examined in the linear regression analysis. The multivariate effects of assessment method [F(6,216) = 1.727, Wilks λ = .911, p= 0.116] and reliability [F(6,216) = 1.493, Wilks λ = 0.922, p= 0.186] were not significant.
Correction factor
Because the difference between ABR and behavioral thresholds varied as a function of degree of hearing loss and stimulus frequency, the results of the linear regression were used to develop ABR correction factors that took these variables into account. First, two-fold cross validation was completed by randomly splitting the entire sample into two groups. The relationship between ABR and behavioral threshold was tested for each group as a function of hearing loss at 500, 1000, 2000, and 4000 Hz. Fisher’s Z-test was used to compare the strength of association between groups at each frequency. Significant differences between groups would suggest that the resulting correction factors would be different for each group. The number of subjects represented at each frequency differed in this analysis because subjects were randomly assigned to group A or B overall, but not on a frequency-by–frequency basis. Results are presented in Table 3. The relationship between ABR and behavioral thresholds as a function of degree of hearing loss did not differ significantly between Groups A and B at any frequency. Therefore, the data from the two groups were combined for the development of ABR threshold-dependent correction factors at each frequency.
Table 3.
Comparison of linear regression between groups for each test frequency
| Group A (n) | Group B (n) | Fisher’s Z (p value) | |
|---|---|---|---|
| 500 Hz* | 141 | 136 | 1.032 (.3063) |
| 1000 Hz | 110 | 119 | 1.440 (.1499) |
| 2000 Hz | 76 | 98 | 0.354 (.7233) |
| 4000 Hz | 82 | 82 | 0.656 (.5183) |
500 Hz based on 250 Hz tone burst predicting 500 Hz behavioral threshold
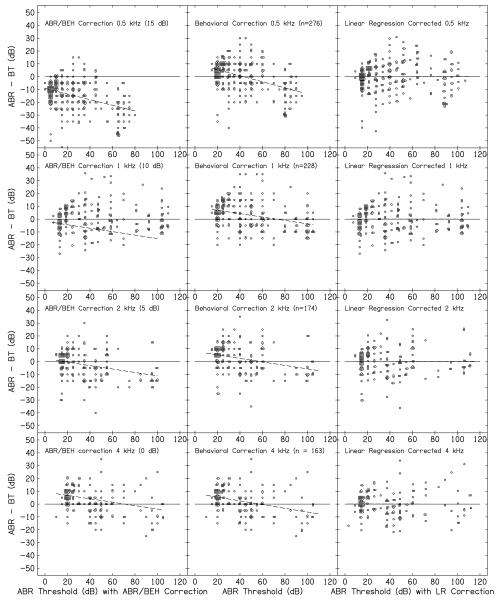
The derived frequency-specific linear regression (LR) correction factors were compared with two existing approaches to ABR correction factors: BEH/ABR correction factors reported by Bagatto et al. (2010) and the BEH correction method reported by Gorga et al. (2006). The LR factors were developed for each frequency by performing linear regressions on the relationship between the ABR-behavioral threshold difference as a function of ABR threshold. The resulting equation describing the regression line was applied to the measured ABR threshold to generate a correction factor specific to that ABR threshold. The linear regression equations for each frequency are reported in Table 4. The resulting LR correction factors (which depended on ABR threshold) were subtracted from measured ABR thresholds to provide of the predicted behavioral thresholds. Figure 4 plots a comparison of the three methods as a function of ABR threshold with each column representing results for a different correction method (constant correction factor from Bagatto et al. 2010, calibration correction from Gorga et al. 2006, and LR correction approaches in left, middle and right columns, respectively) and each row representing results for a different frequency (500, 1000, 2000, and 4000 Hz). The slope of the lines for each frequency in the constant correction factor and calibration correction factor approaches are negative, consistent with the prediction that methods that use a constant correction regardless of degree of hearing loss would lead to an underestimation of behavioral threshold that increases as the degree of hearing loss increases. As expected, the slope of the best fit lines is zero in the third column with the LR correction factor, reflecting the fact that when the correction factor is varied as degree of hearing loss increases, the agreement between ABR and behavioral thresholds is constant. The variance around any ABR threshold is similar for all three approaches; however, in the case of the LR correction, the variance is centered around zero, which was not the case for the other two approaches.
Table 4.
Linear regression equations and correction factors for each test frequency
| Equation | Correction | ||||
|---|---|---|---|---|---|
| 20 | 40 | 60 | 80 | ||
| 500 Hz | y=−0.22x+5.90 | 5 | −3 | −7 | −12 |
| 1000 Hz | y=−0.13x+8.32 | 5 | 3 | 0 | −2 |
| 2000 Hz | y=−0.14x+7.31 | 5 | 2 | −1 | −4 |
| 4000 Hz | y=−0.16x+9.32 | 6 | 3 | 0 | −3 |
Correction factors to be subtracted from ABR threshold to predict behavioral threshold
Figure 4.
The difference between auditory brainstem response (ABR) threshold and behavioral threshold (BT) as a function of the ABR threshold. Data for different frequencies (500, 1000, 2000, and 4000 Hz) are shown in each row and the results when different correction factors (BEH/ABR correction from Bagatto et al. 2010, BEH correction from Gorga et al. 2006, LR correction) were applied to the data are shown in each column. The correction factors used by Bagatto et al. are provided in parentheses in each panel in the left column. The solid line at 0 dB is provided as a reference. Points above this line represent cases in which the ABR overestimated behavioral threshold while points below this line represent cases in which ABR thresholds underestimated behavioral thresholds. Dashed lines within the panels in the left and middle columns are best-fit lines to the data. No dashed line is shown in the right column the application of the LR correction results in a line at 0 dB with a slope of zero.
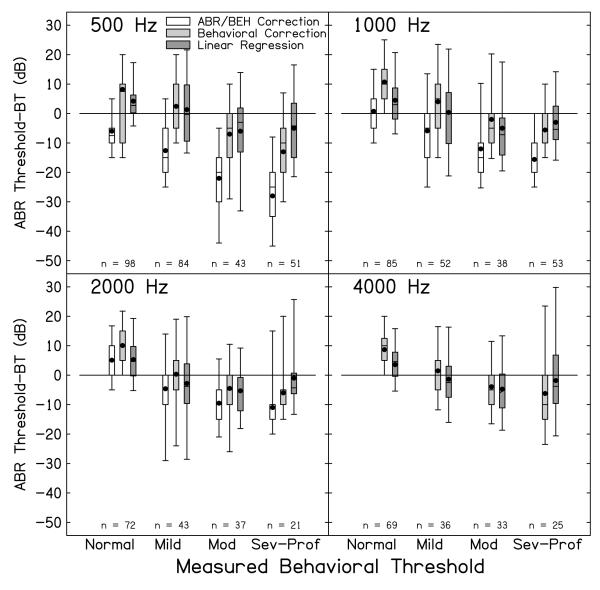
To estimate the size of the estimation error with each correction factor, Fig. 5 displays the mean difference between ABR and behavioral thresholds when degree of behavioral hearing loss is represented as a categorical variable (normal = ≤20 dBHL; mild = 21-49 dBHL; moderate = 50-70 dB HL; severe-profound = >70 dB HL). To analyze the differences shown in this figure, a repeated-measures ANOVA was completed at each stimulus frequency with correction-factor method (BEH/ABR, BEH and LR corrections) as a within-subjects factor and degree of hearing loss (normal, mild, moderate, and severe-to-profound) as a between-subjects factor. For 4000 Hz, where the constant correction factor was 0 dB (see bottom right panel, Fig. 4), only the behavioral and LR correction factors were contrasted. The ANOVA statistics and post hoc comparisons for each frequency are included in Table 4. The main effects of degree of hearing loss and correction method were significant for all test frequencies. For all four frequencies, the interaction between correction factor and degree of hearing loss was significant indicating that there were significant differences among correction factors across hearing-loss groups for each frequency. Post-hoc testing (Tukey’s HSD) was used to evaluate the patterns of significant differences between ABR/BEH correction, BEH correction and LR correction approaches. The minimum mean significant differences for each frequency was 0.5 dB at 500 Hz, 0.4 dB at 1000 Hz, 0.4 dB at 2000 Hz and 0.3 dB at 4000 Hz.. The average differences within each category of hearing loss for each method are reported in Table 5. Due to the small minimum mean significant differences, all correction-factor differences were significantly different across categories of hearing loss. Importantly, frequency-specific LR correction factors resulted in average predictions that were closer to behavioral threshold than either BEH/ABR or BEH correction approaches.
Figure 5.
Box-and-whisker plots of the differences between ABR threshold and behavioral threshold as a function of degree of hearing loss as defined by the behavioral audiogram [Normal hearing ( < 20 dB HL), mild hearing loss (21-49 dB), moderate hearing loss (50-70 dB), severe-profound (> 70)]. Each panel represents data for a different test frequency as indicated. The number of observations in each category of hearing loss and at each frequency is shown as insets in each panel. Boxes for each condition represent the interquartile range (25th to 75th percentile) and whiskers represent the range from the 5th to the 95th percentiles. Lines within each box represent the median and filled circles represent the mean. Shading represents correction factor method (No shading – ABR/BEH; light gray – BEH; dark gray – linear regression). Note that for 4000 Hz, the ABR/BEH correction factor is 0 dB, so only the data for the BEH correction factors are plotted to represent both approaches.
Table 5.
ABR-behavioral differences (dB) for each correction factor by frequency and degree of hearing loss
| Correction approach | 500 Hz = F (6,554) = 437.103, p < 0.001, η2p= 0.828 | |||
| Normal | Mild | Moderate | Severe-Profound | |
| ABR/BEH | −6.8 | −12.6 | −22.6 | −28.6 |
| Behavioral | 8.2 | 2.4 | −7.6 | −13.6 |
| Linear regression | 4.2 | 1.3 | −6 | −5 |
| Correction approach | 1000 Hz = F (6,448) = 417.35, p < 0.001, η2p= 0.848 | |||
| Normal | Mild | Moderate | Severe-Profound | |
| ABR/BEH | 0.8 | −5.9 | −12.9 | −15.6 |
| Behavioral | 10.7 | 4.1 | −2.9 | −5.6 |
| Linear regression | 4.5 | −.4 | −5.2 | −3.1 |
| Correction approach | 2000 Hz = F (6,338) = 427.13, p < 0.001, η2p= 0.883 | |||
| Normal | Mild | Moderate | Severe-Profound | |
| ABR/BEH | 5.1 | −4.7 | −9.5 | −11.4 |
| Behavioral | 10.1 | 0.4 | −4.5 | −6.4 |
| Linear regression | 5.3 | −2.8 | −5.3 | −1.2 |
| Correction approach | 4000 Hz = F (3,159) = 323.43, p < 0.001, η2p= 0.859 | |||
| Normal | Mild | Moderate | Severe-Profound | |
| Behavioral | 8.7 | 1.5 | −3.9 | −6.2 |
| Linear regression | 3.6 | −1.3 | −4.7 | −1.8 |
Model statistics represent the interaction between correction approach and degree of hearing loss at each frequency
Minimum mean significant differences based on Tukey’s HSD, 0.5 dB at 500 Hz, 0.4 dB at 1000 Hz, 0.4 dB at 2000 Hz and 0.3 at 4000 Hz
Negative numbers indicate lower ABR threshold than behavioral threshold.
DISCUSSION
The purpose of the current study was to evaluate the relationship between ABR and behavioral thresholds as a function of degree of hearing loss in a large sample of infants and young children. The data support three primary conclusions. First, there is a relationship between ABR and behavioral threshold that allows for the estimation of behavioral threshold from ABR thresholds. Second, the difference between ABR and behavioral thresholds varied as a function of degree of hearing loss; specifically, the ABR underestimated hearing loss for listeners with moderate or greater hearing loss. Third, frequency-specific correction factors based on the linear relationship between the ABR-behavioral threshold differences resulted in more accurate predictions of behavioral threshold for all test frequencies across the range of degrees of hearing loss included in the present study. Although the linear correction factor did not reduce the variance of these predictions, it resulted in differences between ABR and behavioral thresholds that were closer to zero, compared to the two other approaches.
The correspondence between ABR and behavioral threshold is not a novel finding, as it has been observed in previous studies with infants and children (e.g., Stapells, 2000; Rance et al. 2006; Gorga et al. 2006; Lee et al. 2008; Vander Werff et al. 2009). ABR predictions of behavioral threshold were accurate on average, with mean differences less than 3 dB for all comparisons and correlations between the two measures were consistently high. The correlations between ABR thresholds for a 250-Hz tone burst and the behavioral thresholds at both 250 and 500 Hz are not surprising, given the spectral content of the single-cycle tone burst at 250 Hz. More importantly, these correlations suggest that the single-cycle 250-Hz tone burst can be used to estimate thresholds at the lower frequencies that may be problematical during ABR assessments using 500-Hz tone bursts with longer durations. The average differences between ABR and behavioral thresholds were small, despite the fact that the ABR and behavioral thresholds were often measured months apart. Although measuring the ABR and behavioral threshold in closer temporal proximity would more directly assess the relationship between these two measures and thus reduce the influence of confounding factors, such as progression of hearing loss or increases in ear-canal size that might influence stimulus level, the present data were collected using a method consistent with clinical practices. That is, ABR and behavioral assessments are rarely completed in close temporal proximity. The average length between ABR and behavioral in this study was 13 months, but a wide range of test intervals existed in the present data set. By the time children reach the age where they can participate in a behavioral audiological assessment and provide reliable data, the acquisition of reliable ABR data typically requires sedation. Thus, ABR is usually only recommended in cases in which the child is not developmentally able to participate in behavioral hearing assessment or when behavioral assessments have been repeatedly unsuccessful or inconclusive. The length of time between ABR and behavioral assessment did not affect the differences between measures in the current study. This observation is clinically important and suggests that the agreement between the two threshold estimates and, therefore, the predictive value of the ABR estimate is robust.
The two current clinical methods for predicting behavioral thresholds from ABR thresholds, using either ABR/BEH or BEH correction, are similar in that they determine 0 dB nHL based on the behavioral thresholds to ABR stimuli for a group of adults with normal hearing. The two approaches differ in the sense that the ABR/BEH subtracts a frequency-specific correction factor from the obtained ABR threshold. If these two approaches were otherwise equivalent, subtracting the published correction factor from the calibration values reported by Gorga et al. (2006) should yield results similar to other studies using similar stimulus parameters. However, comparison of the correction factors reported across studies suggests that differences between these approaches cannot entirely be accounted for by applying the correction factor to the dB nHL at each test frequency. For example, 0 dB nHL for 4000 Hz tone bursts from Gorga et al. is 32 dB pSPL, whereas the value from Stapells (2000) is 15 dB pSPL. The recommended correction factors for this frequency are either 5 dB (Bagatto et al. 2008) or −10 dB (Stapells, 2000), neither of which would completely account for the difference from the dB nHL value used by Gorga et al. and in the present study. Furthermore, recommended correction factors often differ for studies that report similar pSPL for 0 dB nHL. For example, the correction factors reported from Bagatto et al. (2008) and Stapells (2000) (as described by Vander Werff and colleagues, 2009) differed by as much as 15 dB at 500 Hz. Additionally, the current data suggest that a constant correction factor, whether derived from ABR thresholds or behavioral thresholds for ABR stimuli, cannot account for changes in the relationship between these two measures that is related to the degree of hearing loss.
Degree of hearing loss influenced the ABR-behavioral threshold differences for all frequencies. Of particular importance is the observation that ABR thresholds underestimated behavioral thresholds in cases of greater than moderate hearing loss. This underestimation has the potential to result in under-amplification when ABR is used as the basis for hearing-aid gain prescriptions. The underestimation of behavioral thresholds for listeners with hearing loss is likely related to the development of ABR stimulus reference levels based on behavioral thresholds for short-duration stimuli in listeners with normal hearing. These reference levels are then used to set 0 dB nHL for ABR measurements. As a consequence of temporal integration, there are differences of as much as 20-25 dB between normal behavioral thresholds for brief tones, compared to normal behavioral thresholds for the long-duration pure tones used in audiometry. These differences, however, are reduced or absent in ears with cochlear hearing loss (Wright, 1968; Reed, Braida & Zurek, 2009). Indeed, reduced temporal integration in ears with sensorineural hearing loss was proposed as a diagnostic tool, known as brief-tone audiometry (Sanders & Honig 1967). That is, the observation of a reduced difference between brief-tone and long-tone behavioral thresholds, compared to what is observed in normal ears, would be consistent with cochlear hearing loss. ABRs are onset responses, occurring as a result of the large initial increase in discharge rate at stimulus onset for auditory neurons. In contrast, ABRs do not reflect the steady-state responses of these neurons that occur throughout the length of long-duration stimuli. As a consequence, increases in stimulus duration have little or no effect on ABR thresholds (e.g., Gorga et al., 1984). Combining the difference in temporal integration between normal-hearing and hearing-impaired subjects with the fact that ABRs are onset responses, results in threshold-dependent differences between ABR and behavioral thresholds. Interestingly, estimates of behavioral threshold based on auditory steady-state responses (ASSR), which are measured using longer-duration stimuli, show the same overestimation when hearing is normal, but show a different pattern as hearing loss increases. Whereas, ABR thresholds tend to underestimate behavioral thresholds for moderate or greater hearing losses, ASSR thresholds tend to agree more closely with behavioral thresholds when severe hearing loss exists (see Rance et al. 2005, Figure 1, for example).
The pattern of ABR-behavioral threshold differences across frequency is similar to what has been observed in previous behavioral studies of temporal integration (Gengel & Watson, 1971) with larger differences at lower frequencies (250 Hz) than at higher frequencies (4000 Hz). Using a constant correction factor (independent of ABR threshold and frequency) will result in accurate ABR predictions of behavioral threshold for listeners with normal hearing or perhaps even ears with mild hearing loss. However, for listeners with moderate or greater hearing loss with reduced or absent temporal-integration effects, subtracting a correction factor from the ABR threshold or basing the calibration reference on a group of listeners with normal hearing leads to an underestimation of behavioral thresholds. The average magnitude of underestimation was approximately 10 dB, with errors greater than 20 dB at 500 Hz. The same pattern was observed in the ABR data reported by Gorga et al. (2006).
Clinical implications
The approach proposed herein was to generate corrections for each frequency that vary as a function of the degree of hearing loss as an alternative to constant corrections based on data from listeners with normal hearing. These new corrections resulted in more accurate ABR predictions of behavioral threshold across a wide range of hearing losses, compared to the results that were obtained when constant corrections were used. The largest improvement observed for the LR corrections occurred at 500 Hz for individuals with greater than moderate degrees of hearing loss, where the constant correction resulted in an approximately 28 dB underestimation of behavioral threshold. Some of the differences between methods were less than the step size (10 dB) used for ABR assessment in this study; however, differences for greater degrees of hearing loss and lower frequencies often exceeded 10 dB when constant corrections were applied. Importantly, the LR corrections never resulted in larger mean estimation errors for behavioral threshold than those observed for constant or calibration correction approaches, and, in most cases, reduced the size of the error.
The clinical application of LR corrections to infant assessment should improve the accuracy of ABR predictions of behavioral threshold. Improvements in prediction will be most pronounced for low frequencies and greater degrees of hearing loss. More accurate estimates of behavioral thresholds would be expected to lead to better prescriptive outcomes for hearing aids, especially for children with moderate-to-profound hearing loss. Given the relations between ABR-behavioral threshold differences and degree of hearing loss, hearing-aid fittings based on the use of constant corrections (regardless of threshold) may underestimate behavioral thresholds by as much as 25 dB, and thus result in less gain than is needed. While many of these children will eventually be candidates for cochlear implantation, the importance of hearing-aid use for providing auditory stimulation prior to cochlear implantation has been a predictor of improved auditory outcomes after implantation (e.g. Lazard et al. 2012).
Limitations
Although the present results were derived from a large sample of children and have the potential to improve the diagnostic accuracy and subsequent treatment outcomes related to ABR assessment of infants, several limitations should be noted. Because both ABR and behavioral data were collected as part of clinical evaluations, audiologists were not blinded to the results of previous assessments, which may have introduced bias. However, any resulting bias would not be expected to follow a systematic pattern of decreasing accuracy as degree of hearing loss increases, as observed in this and other studies. In addition, any bias would be expected to equally affect clinical results for both constant corrections and those based on LRs. Furthermore, knowledge of previous test results would be expected to occur in clinical settings in which clinicians are aware of previous audiological findings. Thus, the improvements in predictions of behavioral thresholds following the application of LR models to ABR thresholds should apply under the conditions in which these measurements are made in the clinic.
Because the data in this study are from a retrospective analysis of clinical records, the etiology of hearing loss was not available for analysis. Limited information about the etiology of hearing loss prevented exclusion of conditions which are associated with fluctuating or progressive hearing loss. Despite this limitation, predictions of behavioral thresholds from ABR thresholds were sufficiently accurate to guide initial interventions, including the selection of amplification characteristics Additionally, restricting the sample to children with sensorineural hearing loss limits the application of these data to children with conductive or mixed hearing losses. Because the mechanism proposed for the variance in the relationship between ABR thresholds and behavioral thresholds is specifically related to loss of temporal integration with sensorineural hearing loss, the present results may not be applicable in cases in which conductive or mixed hearing loss exists.
The results reported may be limited to situations where similar stimulus and data collection parameters are used for ABR assessment. Although the effect of degree of hearing loss is anticipated to occur independently of the stimulus and collection parameters used to measure the ABR, the magnitude of the effect may vary across alternative protocols. However, the data reported here suggest that the paradigm used to measure ABR thresholds is reliable and accurate. The data-collection parameters reported here, in many ways, are similar to those used in other centers and could be implemented in most clinical evoked potentials systems.
Conclusions
The present study sought to estimate the extent to which degree of hearing loss influenced the relationship between ABR and behavioral thresholds in an effort to improve the accuracy of behavioral-threhsold predictions for fitting amplification in children. Thresholds for ABR and behavioral assessments were compared using retrospective analyses of clinical data. The key findings were:
-The relationship between ABR and behavioral thresholds was reliable, as has been documented in previous studies.
-A frequency-specific correction factor that takes into account degree of hearing loss resulted in more accurate predictions of behavioral threshold than approaches that used behavioral correction or used behavioral correction and then applied a constant correction factor regardless of degree of hearing loss.
-The approach used here can be applied to other clinics where similar stimulus and data-collection parameters are applied.
ACKNOWLEDGMENTS
The authors declare no conflicts of interest. This work was supported by NIH-NIDCD grants to Ryan McCreery (R03 DC012635; R01 DC013591) and Michael Gorga (R01 DC002251). The authors wish to thank the audiologists and staff at Boys Town National Research Hospital who collected the ABR and behavioral data used in the current study and Kris Fernau for her assistance.
This work was supported by the following grants from NIH/NIDCD: R01 DC002251, R03 DC012635.
Footnotes
The authors do not declare any other conflict of interest.
References
- American Academy of Pediatrics Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898–921. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- Bagatto M, Scollie SD, Hyde M, Seewald R. Protocol for the provision of amplification within the Ontario infant hearing program. Int J Audiol. 2010;49(Suppl 1):S70–9. doi: 10.3109/14992020903080751. [DOI] [PubMed] [Google Scholar]
- Baldwin M, Watkin P. Predicting the degree of hearing loss using click auditory brainstem response in babies referred from newborn hearing screening. Ear Hear. 2013;34:361–369. doi: 10.1097/AUD.0b013e3182728b88. [DOI] [PubMed] [Google Scholar]
- Ching TYC, Johnson EE, Seeto M, Macrae JH. Hearing-aid safety : A comparison of estimated threshold shifts for gains recommended by NAL-NL2 and DSL m [ i / o ] prescriptions for children. Int J Audiol. 2013;52:S39–S45. doi: 10.3109/14992027.2013.847976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gengel R, Watson C. Temporal integration: I. Clinical implications of a laboratory study. II. Additional data from hearing-impaired subjects. J Speech Hear Disord. 1971;36(2):213–225. doi: 10.1044/jshd.3602.213. [DOI] [PubMed] [Google Scholar]
- Gorga M, Beauchain K, Reiland J, Worthington D, Javel E. The effects of stimulus duration on ABR and behavioral thresholds. J Acoust Soc Am. 1984;76(2):616–619. doi: 10.1121/1.391158. [DOI] [PubMed] [Google Scholar]
- Gorga M, Kaminski J, Beauchaine K. Effects of Stimulus Phase on the Latency of the Auditory Brainstem Response. J Am Acad Audiol. 1991;2:1–6. [PubMed] [Google Scholar]
- Gorga MP, Johnson T. a, Kaminski JR, Beauchaine KL, Garner C. a, Neely ST. Using a combination of click- and tone burst-evoked auditory brain stem response measurements to estimate pure-tone thresholds. Ear Hear. 2006;27(1):60–74. doi: 10.1097/01.aud.0000194511.14740.9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehlinger KM, Van Horne AJO, Moeller MP. Grammatical Outcomes of 3-and 6-Year-Old Children Who Are Hard of Hearing. J Speech Hear Res. 2013;56(5):1701. doi: 10.1044/1092-4388(2013/12-0188). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazard DS, Vincent C, Venail F, Van de Heyning P, Truy E, Sterkers O, Blamey PJ. Pre-, per-and postoperative factors affecting performance of postlinguistically deaf adults using cochlear implants: a new conceptual model over time. PloS one. 2012;7(11):e48739. doi: 10.1371/journal.pone.0048739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C-Y, Jaw F-S, Pan S-L, Hsieh T-H, Hsu C-J. Effects of age and degree of hearing loss on the agreement and correlation between sound field audiometric thresholds and tone burst auditory brainstem response thresholds in infants and young children. J Formos Med Assoc. 2008;107(11):869–75. doi: 10.1016/S0929-6646(08)60203-X. [DOI] [PubMed] [Google Scholar]
- Macrae JH. An investigation of temporary threshold shift caused by hearing aid use. J Speech Hear Res. 1994;37:227–37. doi: 10.1044/jshr.3701.227. [DOI] [PubMed] [Google Scholar]
- Parry G, Hacking C, Bamford J, Day J. Minimal response levels for visual reinforcement audiometry in infants. Int J Audiol. 2003;42(7):413–417. doi: 10.3109/14992020309080050. [DOI] [PubMed] [Google Scholar]
- R Core Development Team R: A language and environment for statistical computing [Computer software] 2014 Available from www.R-project.org. [Google Scholar]
- Rance G. Auditory neuropathy/dys-synchrony and its perceptual consequences. Trends Amplif. 2005;9(1):1–43. doi: 10.1177/108471380500900102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rance G, Roper R, Symons L, Moody LJ, Poulis C, Dourlay M, Kelly T. Hearing threshold estimation in infants using auditory steady-state responses. Journal of the American Academy of Audiology. 2005;16(5):291–300. doi: 10.3766/jaaa.16.5.4. [DOI] [PubMed] [Google Scholar]
- Reed C, Braida L, Zurek P. Review article: Review of the literature on temporal resolution in listeners with cochlear hearing impairment: A critical assessment of the role of suprathreshold deficits. Trends Amplif. 2009;13:4–43. doi: 10.1177/1084713808325412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapells D. Threshold estimation by the tone-evoked auditory brainstem response: a literature meta-analysis. J Speech Hear Res. 2000;24(2):74–83. [Google Scholar]
- Stapells D. Frequency-Specific ABR and ASSR Threshold Assessment in Young Infants. Proceedings from A Sound Foundation Through Early Amplification phonak.com. 2011:409–448. [Google Scholar]
- Takagi N, Suzuki T, Kobayashi K. Effect of tone-burst frequency on fast and slow components of auditory brain-stem response. Scand Audiol. 1985;14(2):75–79. doi: 10.3109/01050398509045926. [DOI] [PubMed] [Google Scholar]
- Tomblin JB, Oleson J, Ambrose SE, Walker EA, Moeller MP. The Influence of Hearing Aids on the Speech and Language Development of Children with Hearing Loss. JAMA Otolaryngol Head Neck Surg. 20142014 doi: 10.1001/jamaoto.2014.267. Online First Published online April 03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Werff KR, Prieve B. a, Georgantas LM. Infant air and bone conduction tone burst auditory brain stem responses for classification of hearing loss and the relationship to behavioral thresholds. Ear Hear. 2009;30(3):350–68. doi: 10.1097/AUD.0b013e31819f3145. [DOI] [PubMed] [Google Scholar]
- Watson CS, Gengel EL. Signal duration and signal frequency in relation to auditory sensitivity. J Acoust Soc Am. 1969;46:989–997. doi: 10.1121/1.1911819. R. W. [DOI] [PubMed] [Google Scholar]
- Wright HN. The effect of sensori-neural hearing loss on threshold-duration functions. J Speech Hear Res. 1968;11(4):842–52. doi: 10.1044/jshr.1104.842. [DOI] [PubMed] [Google Scholar]