Abstract
Purpose of review
HIV management in PWUD is typically complex and challenging due to the presence of multiple medical and psychiatric comorbidities as well as social, physical, economic and legal factors that often disrupt the HIV continuum of care. In this review we describe the individual, health systems and societal barriers to HIV treatment access and care retention for people who use drugs. Additionally the clinical management of HIV infected PWUD is often complicated by the presence of multiple infectious and non-infectious comorbidities.
Recent findings
Improved ART adherence can be achieved through the provision of opiate substitution therapy (OST), directly administered antiretroviral therapy (DAART) and integration of ART with OST services. Recent advances with direct-acting antivirals (DAA) for HCV have shown superior outcomes compared to interferon based regimes in HIV-HCV co-infected patients. Newer diagnostic technologies for tuberculosis hold promise for earlier diagnosis for PWUD co-infected with TB
Summary
HIV-infected PWUDs are a key population who frequently experience suboptimal outcomes along the HIV continuum of care. A comprehensive strategy that encompasses evidence-based prevention and treatment interventions that target the individual, family, healthcare system, legal and societal structure is required to ensure greater participation and success in HIV treatment and care.
Keywords: HIV, people who use drugs, antiretroviral therapy, opiate substitution treatment, HIV treatment cascade
Introduction
Although globally HIV incidence has decreased, low coverage of harm reduction and treatment services for people who use drugs (PWUD) has resulted in increases up to 30% for new HIV infections reported outside of Sub-Saharan Africa, particularly in Eastern Europe, Central Asia, the Middle East, North Africa and parts of South and East Asia.1–3
Despite the volatile HIV epidemic among PWUD, especially in these low and middle-income countries (LMICs), the benefits from antiretroviral therapy (ART) in reducing HIV-related morbidity and mortality have been less pronounced among HIV-infected PWUD for several reasons.4 Indeed, mortality among PWUDs or alcohol is higher than their counterparts, even after controlling for ART access.5 First and foremost, HIV management in PWUD is typically complex and challenging due to the presence of multiple medical and psychiatric comorbidities6 as well as social, physical, economic and legal factors that often disrupt the HIV continuum of care, including delayed HIV diagnosis and entry into care, decreased ART access and adherence and poor long term retention in care. 7–11 Approximately half of HIV-infected PWUDs have underlying mental illness, and both untreated mental illness or active drug use potentiates the risk of drug overdoses, violence and incarceration.12–15 Shared transmission factors increase likelihood of HIV-infected PWUD becoming co-infected with viral hepatitis (HBV and HCV) and co-infection with tuberculosis facilitates disease progression, overlapping drug toxicities, drug-drug interactions and side-effects.6 Consequence, despite recent ART scale-up that now reaches 13 million people living with HIV (PLH) in LMICs, PWUD (~10% only) are disproportionately less likely than other PLH to receive ART1,16,17 according to a World Bank analysis.18 Viewed across the HIV treatment cascade paradigm, HIV-infected PWUD face significant family and social, health-care system and individual level barriers to each step.7,19,20 Achieving parity in prevention and treatment for PWUDs remains a challenge for individuals, healthcare systems and policy-makers alike. Overcoming obstacles along the entire HIV continuum of care (Figure 1) for PWUDs, from HIV testing through achieving viral suppression, is central to HIV treatment and prevention efforts.
Fig 1.
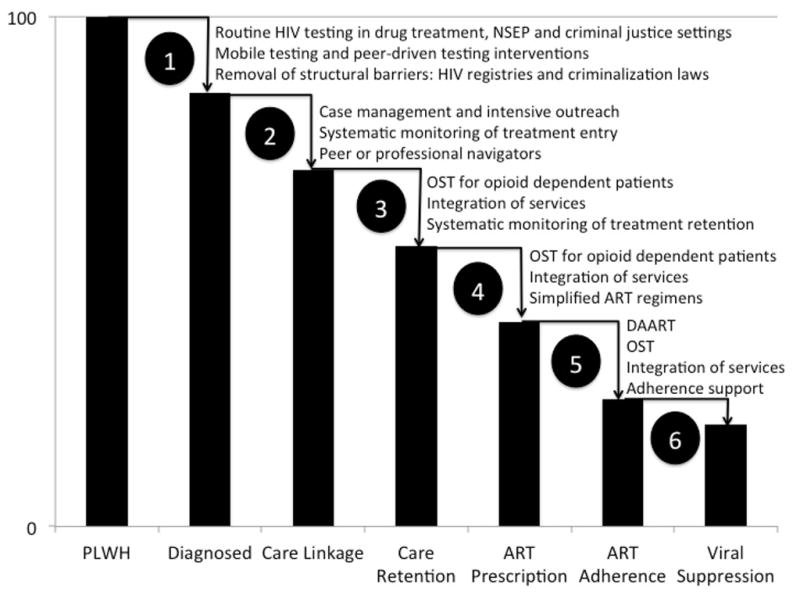
The HIV Continuum of Care for People Who Use Drugs: Strategies to Overcome Obstacles to Effective Treatment as Prevention
PLWH: people living with HIV; ART: antiretroviral therapy; NSEP: needle and syringe exchange programs; OST: opioid substitution therapy; DAART: directly administered antiretroviral therapy.
Challenges with HIV Diagnosis: The First Step Toward Treatment
In a recent review of access to HIV counselling and testing (HTC) in five countries in Central Asia where 60% of HIV infections are attributed to drug injection, the number of PWID who had been tested for HIV in the previous 12 months varied from 29% in Uzbekistan to 65% in Kazakhstan.21 In these countries and elsewhere, stigma, discrimination, human rights violations, and repressive legislation were found to be significant barriers to HTC in the countries examined.22,23 Once diagnosed, PWUDs must be linked to HIV care. Numerous studies in high and LMICs have identified a number of issues related to linking PWUDs’ care. In one U.S. study, PWIDs had delays in linkage to care that exceeded 19 months.24
Strategies to increase HIV testing such as on-site rapid HIV testing in drug treatment programs25,26 and community based point-of-care testing through NSEPs and mobile medical units have been shown to increase the likelihood of HIV testing and successfully reached those who would not otherwise have been tested.27,28 Recent data also support the use of peer-delivered strategies to increase HIV testing, which may further improve HIV testing rates for PWUDs.29
Challenges in Treatment Access and Care Retention
Following HIV diagnosis, linkage and retention in care followed by ART initiation present extraordinary challenges for HIV-infected PWUD. Mutual lack of trust and suspicion between providers and PWUD delays entry into care, the first step of engagement, a scenario that has not improved much despite decades of experience in both high or LMICs.7,20,30,31
A longitudinal assessment of HIV-infected PWIDs showed no substantial improvement in ART initiation over 12 years despite simplified and better-tolerated ART regimens and availability.31 Furthermore, compared to MSM in a Spanish cohort of PLH where over half of the participants were PWUD, PWUD were 33% less likely to initiate low ART; authors cited health professional’s fear of sub-optimal adherence and their inexperience with PWUDs as key contributors to late ART initiation32 despite evidence that PWUDs adhere to ART similarly to other PLH if provided adequate adherence support.33 Both North American34 and Malaysian35 HIV specialists were significantly more likely to withhold ART from HIV-infected PWUDs unless they were abstinent from drugs, further contributing to treatment disparities. Clinicians cite ART non-adherence and development of antiretroviral resistance as major concerns,34,36,37 despite a meta-analysis demonstrating that antiretroviral resistance among PWIDs and non-PWIDs did not differ.38
Physicians often view drug users as manipulative, unmotivated, and undeserving of care while PWUD are often mistrustful of the health care system.39–41 Healthcare avoidance by drug users is further exacerbated in countries where drug use is criminalized or compulsory detention for drug use is used as a means of “drug treatment”.17,42,43, 44,
With improved tolerability and convenience using contemporary ART regimens, evidence from both high45 and LMIC46 confirm improved short-term adherence among PWUD; from 1996 to 2009, >95% adherence increased from 19.3% to 65.9% in Canada.47 Longer studies, however, suggest that a substantial proportion of PWUD either discontinue treatment or have sub-optimal adherence.4,48–53,54 In the ALIVE cohort, for example, two-thirds of PWIDs were not retained in long-term with lack of healthcare insurance and suboptimal provider constancy contributing to reduced care retention, and active drug use further contributed to virological failure.55
Interventions that improve ART adherence and viral suppression have been reviewed extensively.56 Three interventions are recommended to improve viral suppression among HIV-infected PWUDs, including directly administered ART (DAART), providing opioid substitution therapy (OST) like methadone or buprenorphine to opioid dependent patients and integrating HIV and addiction services.57 The best evidence to improve ART adherence is using DAART,58–61 yet one recent study of stably methadone-maintained patients did not confirm this benefit.62 While DAART may involve increased human resources and be logistically challenging, a cost-effectiveness study integrating DAART into MMT support its use, especially in LMIC settings.63 Considerable evidence for OST with buprenorphrine or methadone for opioid dependent patients exists to improve retention in care, ART uptake, ART adherence, and viral suppresion.56,64–68 HIV-infected PWUDs who are in drug treatment adhere to ART similarly to non-PWUDs.69,70 OST, including in LMICs,71,72 improves HIV-related quality-of-life in HIV-infected PWUDs.73 In studies of integrating buprenorphine into HIV care, retention in care74 as well as improved ART initiation and viral suppression have been achieved.64 Contingency management, and multi-component, nurse-delivered interventions have also significantly improved short-term adherence and virologic outcomes, but these effects were not sustained after intervention cessation.56
Challenges in Clinical Management
The frequent co-occurrence of other infectious and non-infectious conditions in HIV-infected PWUD adds to the complexities in their clinical management.6 HIV/HCV co-infected persons have a 6-fold risk of end-stage liver disease and a 2-fold risk of cirrhosis compared with HCV mono-infected patients, leading to a 15%–25% prevalence of cirrhosis within 10–15 years of infection.6,75,76 ART significantly reduces likelihood of hepatic decompensation in HIV/HCV-infected patients by 28%–41%.77 HIV/HCV-infected patients are also at increased risk for cerobrovascular disease78,79 and all-cause mortality80,81 compared to HIV mono-infected patients, thus urging the need for expanded treatment.
HCV treatment in HIV/HCV co-infected patients presents unique challenges, including concerns about adherence, increased adverse side effects, and risk of reinfection from continued injection;82 as a result active drug users are unlikely to be treated82 and are excluded from clinical trials.83 Before direct-acting antivirals (DAA) for HCV, lower sustained virological response (SVR) rates, longer treatment duration and more severe side effects reduced enthusiasm for pegylated interferon-based regimens in HIV/HCV co-infected patients.84 First-generation DAAs like telaprevir and boceprevir, as well as newer DAAs like sofosbuvir and simeprevir markedly improved treatment responses over interferon-based regimens, however, pharmacological drug interactions and overlapping drug toxicities persist.85,86
Interferon-free DAA regimens using sofosbuvir plus ribavirin show greater promise with SVRs in 84%–89% of HIV/HCV coinfected patients with genotypes 1–4,87 while newer interferon-free regimens of ABT-450/ritonavir/ombitasvir/dasabuvir (ABT-333) with ribavirin for 12 weeks show SVRs of 94% in HIV/HCV patients with genotype 1.88 Drug interactions and prohibitive costs of these new breakthroughs treatments, however, will restrict access to treatment for HIV PWUDs, especially in LMICs with limited resources and restricted ART options.89, 90 In the case of HIV/HBV coinfection, the combination of tenofovir with either lamivudine or emtricitabine is now universally recommended as integral to ART regimens to avoid selection and transmission of lamivudine-resistant HBV.91
Drug use, poverty, homelessness, overcrowding and imprisonment independently predispose PWUD to increased TB risk.92–94 HIV-infected PWIDs have a 2–6-fold increased risk of developing TB compared with their non-using counterparts.95,96 Challenges in managing HIV/TB co-infected PWUD are considerable, including delayed diagnosis, medication non-adherence and default from treatment and prophylaxis regimens, drug-drug interactions and increased hepatotoxicity risk.92–94 Recent TB diagnostics developments, including point-of-care testing with Xpert® MTB/RIF and lipopolysaccharide antigen lipoarabinomannan (LAM) antigen urine testing, reduce repeated clinic attendance and accelerate treatment and potentially minimize treatment default among PWUD.97–100 OST improves TB screening rates in HIV-infected PWIDs, receipt of preventive therapy and treatment adherence and persistence.6,72,101–103 TB treatment in HIV-infected PWUD is complicated by complex drug interactions and toxicites between medications to treat TB, HIV, and addiction.6 When OST, HIV and TB treatment are integrated in Ukraine, a recent study documented improved outcomes for each condition72 as well as improved adherence and retention in TB treatment for patients with TB disease.101
Poor hygiene, injection of nonsterile preparations, and poor technique predispose HIV-infected drug users to infections ranging from localised skin and soft-tissue infections to deep-seated infections including pyomyositis, septic arthritis, osteomyelitis, and endocarditis which may account for up to 25% of mortality in HIV-infected PWUD. Additionally, fatal outbreaks of botulism, tetanus, and fungal infections caused by injection of contaminated heroin have also been reported.6
Alcohol-use disorders and smoking are common in HIV infected PWUD. Heavy alcohol use contributes to the decreased retention in care and poor adherence to treatment as well as accelerate hepatic fibrosis in patients co-infected HCV. Similarly, the effects of smoking in HIV-infected drug users are often compounded by the added contribution of HCV, and some classes of ART that lead to accelerated atherosclerosis and increased morbidity and mortality.6
The prevalence of psychiatric disorders is high among HIV-infected PWUDs,6,104 which further complicates management. Psychiatric disorders among HIV-infected PWUDs are associated with increased HIV behaviors, and suboptimal HIV outcomes in all aspects of the treatment cascade.105 Central to improving HIV treatment outcomes is routine screening and pharmacological treatment,57,106 which is fraught with some drug-drug interactions with OST.107
Stigma and Discrimination
HIV-infected PWUDs often operate under the multiple veils of stigma from HIV, addiction, mental illness and criminal justice system involvement,108 which often leads to discrimination. HIV-infected PWUDs and their families are isolated, despised and refused assistance by community members because they assume that those persons are unworthy. Stigma and discrimination often result in negative consequences like imposing shame, lack of trust or disowning them. Neighbors, employers and healthcare workers may similarly shame and discriminate against them, making the individual and family feel like outcasts and avoid treatment engagement.109,110 Intransigent societal level stigma therefore impacts all aspects of the HIV treatment cascade and requires societal level interventions that protect HIV-infected PWUDs from discrimination.111–113
Conclusion
HIV-infected PWUDs are a key population who in the absence of evidence-based prevention and treatment interventions that target the individual, family, healthcare system and societal structure, experience suboptimal outcomes along the HIV continuum of care. Scale-up of interventions and structural changes that improve their health, however, have the greatest benefit to improve society and reduce the scourges of the HIV pandemic.
Key points.
The presence of multiple medical and psychiatric comorbidities as well as social, physical, economic and legal factors present a challenge in the HIV continuum of care for people who use drugs (PWUD)
Long term adherence to ART has been shown to improve through interventions such as DAART, OST and integration of HIV treatment into substance abuse care
Management of the HIV infected PWUD can be complex due to the presence of multiple infectious and noninfectious comorbidities. Earlier diagnosis of HIV and other infectious complications through improved testing technology and service delivery together with integration of service can improve treatment outcomes.
Acknowledgments
This research was funded by the National Institutes on Drug Abuse (R01 DA025943 and K24 DA017072) and the University of Malaya High Impact Research Grant (H-20001-E000001)
Footnotes
Conflict of Interest:
There are no conflicts of interest
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
* of special interest
** of outstanding interest
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) The Gap Report. Geneva, Switzerland: 2014. [Accessed on 24 August 2014]. at: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication//unaids_gap_report_en.pdf. [Google Scholar]
- 2.Vermund SH. Global HIV epidemiology: A guide for strategies in prevention and care. Curr HIV/AIDS Rep. 2014;11:93–8. doi: 10.1007/s11904-014-0208-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global State of Harm Reduction. [Accessed August 17, 2014];2012: Towards and integrated response. 2012 at http://www.ihra.net/files/2012/07/24/GlobalState2012_Web.pdf.
- 4.Weber R, Huber M, Battegay M, et al. Influence of noninjecting and injecting drug use on mortality, retention in the cohort, and antiretroviral therapy, in participants in the Swiss HIV Cohort Study. HIV Med. 2014 doi: 10.1111/hiv.12184. [DOI] [PubMed] [Google Scholar]
- 5.Baum MK, Rafie C, Lai S, Sales S, Page B, Campa A. Crack-cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. J Acquir Immune Defic Syndr. 2009;50:93–9. doi: 10.1097/QAI.0b013e3181900129. [DOI] [PubMed] [Google Scholar]
- 6.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376:59–79. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7*.Meyer JP, Althoff AL, Altice FL. Optimizing Care for HIV-Infected People Who Use Drugs: Evidence-Based Approaches to Overcoming Healthcare Disparities. Clin Infect Dis. 2013;57:1309–17. doi: 10.1093/cid/cit427. This systematic review examines and details the evidence-based strategies for overcoming obstacles to optimizing HIV treatment outcomes among people who use drugs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolfe D. Paradoxes in antiretroviral treatment for injecting drug users: access, adherence and structural barriers in Asia and the former Soviet Union. Int J Drug Policy. 2007;18:246–54. doi: 10.1016/j.drugpo.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Milloy MJ, Kerr T, Buxton J, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis. 2011;203:1215–21. doi: 10.1093/infdis/jir032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Milloy MJ, Marshall BD, Kerr T, et al. Social and structural factors associated with HIV disease progression among illicit drug users: a systematic review. AIDS. 2012;26:1049–63. doi: 10.1097/QAD.0b013e32835221cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donoghoe MC, Bollerup AR, Lazarus JV, Nielsen S, Matic S. Access to highly active antiretroviral therapy (HAART) for injecting drug users in the WHO European Region 2002–2004. Int J Drug Policy. 2007;18:271–80. doi: 10.1016/j.drugpo.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Hakansson A, Berglund M. All-cause mortality in criminal justice clients with substance use problems--a prospective follow-up study. Drug Alcohol Depend. 2013;132:499–504. doi: 10.1016/j.drugalcdep.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Moore E, Winter R, Indig D, Greenberg D, Kinner SA. Non-fatal overdose among adult prisoners with a history of injecting drug use in two Australian states. Drug Alcohol Depend. 2013;133:45–51. doi: 10.1016/j.drugalcdep.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Pabayo R, Alcantara C, Kawachi I, Wood E, Kerr T. The role of depression and social support in non-fatal drug overdose among a cohort of injection drug users in a Canadian setting. Drug Alcohol Depend. 2013;132:603–9. doi: 10.1016/j.drugalcdep.2013.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bartoli F, Carra G, Brambilla G, et al. Association between depression and non-fatal overdoses among drug users: a systematic review and meta-analysis. Drug Alcohol Depend. 2014;134:12–21. doi: 10.1016/j.drugalcdep.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Aceijas C, Oppenheimer E, Stimson GV, Ashcroft RE, Matic S, Hickman M. Antiretroviral treatment for injecting drug users in developing and transitional countries 1 year before the end of the “Treating 3 million by 2005. Making it happen. The WHO strategy” (“3 by 5”) Addiction. 2006;101:1246–53. doi: 10.1111/j.1360-0443.2006.01509.x. [DOI] [PubMed] [Google Scholar]
- 17.Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;376:355–66. doi: 10.1016/S0140-6736(10)60832-X. [DOI] [PubMed] [Google Scholar]
- 18.Dutta A, Wirtz A, Stanciole A, et al. The Global HIV Epidemics among People Who Inject Drugs. Washington, D.C: World Bank; 2013. [DOI] [Google Scholar]
- 19.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52:793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chakrapani V, Velayudham J, Shunmugam M, Newman PA, Dubrow R. Barriers to antiretroviral treatment access for injecting drug users living with HIV in Chennai, South India. AIDS Care. 2014;26:835–41. doi: 10.1080/09540121.2013.861573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Terlikbayeva A, Zhussupov B, Primbetova S, et al. Access to HIV counseling and testing among people who inject drugs in Central Asia: strategies for improving access and linkages to treatment and care. Drug Alcohol Depend. 2013;132(Suppl 1):S61–4. doi: 10.1016/j.drugalcdep.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bojko MJ, Dvoriak S, Altice FL. At the crossroads: HIV prevention and treatment for people who inject drugs in Ukraine. Addiction. 2013;108:1697–9. doi: 10.1111/add.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Izenberg J, Altice FL. Next Steps for Ukraine - Abolition of HIV Registries, Implementation of Routine HIV Testing and Expansion of Services. Addiction. 2010;105:569–70. doi: 10.1111/j.1360-0443.2009.02881.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samet JH, Freedberg KA, Stein MD, et al. Trillion virion delay: time from testing positive for HIV to presentation for primary care. Arch Intern Med. 1998;158:734–40. doi: 10.1001/archinte.158.7.734. [DOI] [PubMed] [Google Scholar]
- 25*.Metsch LR, Feaster DJ, Gooden L, et al. Implementing rapid HIV testing with or without risk-reduction counseling in drug treatment centers: results of a randomized trial. Am J Public Health. 2012;102:1160–7. doi: 10.2105/AJPH.2011.300460. This prospective trial documents the effectiveness of providing onsite HIV counseling and testing within drug treatment settings as a structural intervention. Those with integrated and routine HIV testing were significantly more likely to be HIV tested. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chadwick JJ, Andrade LF, Altice FL, Petry NM. Correlates of Having Never Been HIV Tested among Entrants to Substance Abuse Treatment Clinics: Empiric Findings from Real-World New England Settings. J Psychoactive Drugs. 2014;46:208–14. doi: 10.1080/02791072.2014.915363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liebman J, Pat Lamberti M, Altice FL. Effectiveness of a mobile medical van in providing screening services for STDs and HIV. Public Health Nurs. 2002;19:345–53. doi: 10.1046/j.1525-1446.2002.19504.x. [DOI] [PubMed] [Google Scholar]
- 28.Lipsitz MC, Segura ER, Castro JL, et al. Bringing testing to the people - benefits of mobile unit HIV/syphilis testing in Lima, Peru, 2007–2009. Int J STD AIDS. 2014;25:325–31. doi: 10.1177/0956462413507443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Markwick N, Ti L, Callon C, Feng C, Wood E, Kerr T. Willingness to engage in peer-delivered HIV voluntary counselling and testing among people who inject drugs in a Canadian setting. J Epidemiol Community Health. 2014;68:675–8. doi: 10.1136/jech-2013-203707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruce RD, Altice FL. Clinical care of the HIV-infected drug user. Infect Dis Clin North Am. 2007;21:149–79. doi: 10.1016/j.idc.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehta SH, Kirk GD, Astemborski J, Galai N, Celentano DD. Temporal trends in highly active antiretroviral therapy initiation among injection drug users in Baltimore, Maryland, 1996–2008. Clin Infect Dis. 2010;50:1664–71. doi: 10.1086/652867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodríguez-Arenas MA, Jarrín I, del Amo J, et al. Delay in the initiation of HAART, poorer virological response, and higher mortality among HIV-infected injecting drug users in Spain. AIDS Res Hum Retroviruses. 2006;22:715–23. doi: 10.1089/aid.2006.22.715. [DOI] [PubMed] [Google Scholar]
- 33.Malta M, Magnanini MM, Strathdee SA, Bastos FI. Adherence to antiretroviral therapy among HIV-infected drug users: a meta-analysis. AIDS Behav. 2010;14:731–47. doi: 10.1007/s10461-008-9489-7. [DOI] [PubMed] [Google Scholar]
- 34.Westergaard RP, Ambrose BK, Mehta SH, Kirk GD. Provider and clinic-level correlates of deferring antiretroviral therapy for people who inject drugs: a survey of North American HIV providers. J Int AIDS Soc. 2012;15:10. doi: 10.1186/1758-2652-15-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferro EG, Wickersham JA, Marcus R, et al. Lack of Prescription of Antiretroviral Therapy to Vulnerable Populations by Malaysian Physicians. ID Week. San Francisco, CA: Infectious Diseases Society of America; 2013. Oct 2–6, Abstract WE-1206. [Google Scholar]
- 36.Wood E, Kerr T, Tyndall MW, Montaner JS. A review of barriers and facilitators of HIV treatment among injection drug users. Aids. 2008;22:1247–56. doi: 10.1097/QAD.0b013e3282fbd1ed. [DOI] [PubMed] [Google Scholar]
- 37.Ding L, Landon BE, Wilson IB, Wong MD, Shapiro MF, Cleary PD. Predictors and consequences of negative physician attitudes toward HIV-infected injection drug users. Arch Intern Med. 2005;165:618–23. doi: 10.1001/archinte.165.6.618. [DOI] [PubMed] [Google Scholar]
- 38.Werb D, Mills EJ, Montaner JS, Wood E. Risk of resistance to highly active antiretroviral therapy among HIV-positive injecting drug users: a meta-analysis. Lancet Infect Dis. 2010;10:464–9. doi: 10.1016/S1473-3099(10)70097-9. [DOI] [PubMed] [Google Scholar]
- 39.Ostertag S, Wright BRE, Broadhead RS, Altice FL. Trust and other characteristics associated with health care utilization by injection drug users. Journal of Drug Issues. 2006;36:953–74. [Google Scholar]
- 40.Merrill JO, Rhodes LA, Deyo RA, Marlatt GA, Bradley KA. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17:327–33. doi: 10.1046/j.1525-1497.2002.10625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28:47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- 42.Fu JJ, Bazazi AR, Altice FL, Mohamed MN, Kamarulzaman A. Absence of antiretroviral therapy and other risk factors for morbidity and mortality in Malaysian compulsory drug detention and rehabilitation centers. PLoS One. 2012;7:e44249. doi: 10.1371/journal.pone.0044249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kerr T, Hayashi K, Ti L, Kaplan K, Suwannawong P, Wood E. The impact of compulsory drug detention exposure on the avoidance of healthcare among injection drug users in Thailand. Int J Drug Policy. 2014;25:171–4. doi: 10.1016/j.drugpo.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 44.Beyrer C, Baral S, Kerrigan D, El-Bassel N, Bekker LG, Celentano DD. Expanding the space: inclusion of most-at-risk populations in HIV prevention, treatment, and care services. J Acquir Immune Defic Syndr. 2011 Aug;57(Suppl 2):S96–9. doi: 10.1097/QAI.0b013e31821db944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45**.Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA internal medicine. 2014;174:721–9. doi: 10.1001/jamainternmed.2014.601. This is the largest contemporary cohort of HIV-infected prisoners, nearly all of whom used drugs, documenting that extremely high levels of viral suppression could be achieved during incarceration when drug use, social and structural impediments were removed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jordan M, Obeng-Aduasare Y, Sheehan H, et al. Correlates of non-adherence to antiretroviral therapy in a cohort of HIV-positive drug users receiving antiretroviral therapy in Hanoi, Vietnam. Int J STD AIDS. 2013;25:662–8. doi: 10.1177/0956462413516301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mann B, Milloy MJ, Kerr T, Zhang R, Montaner J, Wood E. Improved adherence to modern antiretroviral therapy among HIV-infected injecting drug users. HIV Med. 2012;13:596–601. doi: 10.1111/j.1468-1293.2012.01021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kerr T, Marshall A, Walsh J, et al. Determinants of HAART discontinuation among injection drug users. AIDS Care. 2005;17:539–49. doi: 10.1080/09540120412331319778. [DOI] [PubMed] [Google Scholar]
- 49.Kim TW, Palepu A, Cheng DM, Libman H, Saitz R, Samet JH. Factors associated with discontinuation of antiretroviral therapy in HIV-infected patients with alcohol problems. AIDS Care. 2007;19:1039–47. doi: 10.1080/09540120701294245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maru DS, Bruce RD, Walton M, et al. Initiation, adherence, and retention in a randomized controlled trial of directly administered antiretroviral therapy. AIDS Behav. 2008;12:284–93. doi: 10.1007/s10461-007-9336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robison LS, Westfall AO, Mugavero MJ, et al. Short-term discontinuation of HAART regimens more common in vulnerable patient populations. AIDS Res Hum Retroviruses. 2008;24:1347–55. doi: 10.1089/aid.2008.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Werb D, Milloy MJ, Kerr T, Zhang R, Montaner J, Wood E. Injection drug use and HIV antiretroviral therapy discontinuation in a Canadian setting. AIDS Behav. 2013;17:68–73. doi: 10.1007/s10461-012-0136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Batista J, de Albuquerque MF, Santos ML, et al. Association between smoking, crack cocaine abuse and the discontinuation of combination antiretroviral therapy in Recife, Pernambuco, Brazil. Revista do Instituto de Medicina Tropical de Sao Paulo. 2014;56:127–32. doi: 10.1590/S0036-46652014000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jiamsakul A, Kumarasamy N, Ditangco R, et al. Factors associated with suboptimal adherence to antiretroviral therapy in Asia. J Int AIDS Soc. 2014;17:18911. doi: 10.7448/IAS.17.1.18911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55*.Westergaard RP, Hess T, Astemborski J, Mehta SH, Kirk GD. Longitudinal changes in engagement in care and viral suppression for HIV-infected injection drug users. AIDS. 2013;27:2559–66. doi: 10.1097/QAD.0b013e328363bff2. This longitudinal study demonstrated the low rates of long term retention in care among PWUD. Factors that were associated with suboptimal engagement in care included poor access to medical care, active drug use, and incarceration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56**.Binford MC, Kahana SY, Altice FL. A systematic review of antiretroviral adherence interventions for HIV-infected people who use drugs. Curr HIV/AIDS Rep. 2012;9:287–312. doi: 10.1007/s11904-012-0134-8. This systematic review provides the data and evidence for improved antiretroviral medication adherence among people who use drugs, including the use of directly administered antiretroviral therapy, provision of opioid substitution therapy and integrating substance abuse treatment into HIV clinical care settings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156:817–33. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Altice FL, Maru DS, Bruce RD, Springer SA, Friedland GH. Superiority of directly administered antiretroviral therapy over self-administered therapy among HIV-infected drug users: a prospective, randomized, controlled trial. Clin Infect Dis. 2007;45:770–8. doi: 10.1086/521166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hart JE, Jeon CY, Ivers LC, et al. Effect of directly observed therapy for highly active antiretroviral therapy on virologic, immunologic, and adherence outcomes: a meta-analysis and systematic review. J Acquir Immune Defic Syndr. 2010;54:167–79. doi: 10.1097/QAI.0b013e3181d9a330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Macalino GE, Hogan JW, Mitty JA, et al. A randomized clinical trial of community-based directly observed therapy as an adherence intervention for HAART among substance users. AIDS. 2007;21:1473–7. doi: 10.1097/QAD.0b013e32811ebf68. [DOI] [PubMed] [Google Scholar]
- 61.Berg KM, Litwin A, Li X, Heo M, Arnsten JH. Directly observed antiretroviral therapy improves adherence and viral load in drug users attending methadone maintenance clinics: A randomized controlled trial. Drug Alcohol Depend. 2011;113(2–3):192–9. doi: 10.1016/j.drugalcdep.2010.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lucas GM, Mullen BA, Galai N, et al. Directly Administered Antiretroviral Therapy for HIV-Infected Individuals in Opioid Treatment Programs: Results from a Randomized Clinical Trial. PLoS One. 2013;8:e68286. doi: 10.1371/journal.pone.0068286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63**.Tran BX, Ohinmaa A, Duong AT, et al. Cost-effectiveness of integrating methadone maintenance and antiretroviral treatment for HIV-positive drug users in Vietnam’s injection-driven HIV epidemics. Drug Alcohol Depend. 2012;125:260–6. doi: 10.1016/j.drugalcdep.2012.02.021. This study provides empiric evidence and cost-effectiveness for providing both opioid substitution therapy along with directly administered antiretroviral therapy in a low or middle income country. [DOI] [PubMed] [Google Scholar]
- 64.Altice FL, Bruce RD, Lucas GM, et al. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56:S22–32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Springer SA, Qiu J, Saber-Tehrani AS, Altice FL. Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One. 2012;7:e38335. doi: 10.1371/journal.pone.0038335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2003;22:223–8. [PubMed] [Google Scholar]
- 67.Palepu A, Tyndall MW, Joy R, et al. Antiretroviral adherence and HIV treatment outcomes among HIV/HCV co-infected injection drug users: The role of methadone maintenance therapy. Drug Alcohol Depend. 2006 doi: 10.1016/j.drugalcdep.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 68.Uhlmann S, Milloy MJ, Kerr T, et al. Methadone maintenance therapy promotes initiation of antiretroviral therapy among injection drug users. Addiction. 2010;105:907–13. doi: 10.1111/j.1360-0443.2010.02905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hicks PL, Mulvey KP, Chander G, et al. The impact of illicit drug use and substance abuse treatment on adherence to HAART. AIDS Care. 2007;19:1134–40. doi: 10.1080/09540120701351888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kapadia F, Vlahov D, Wu Y, et al. Impact of drug abuse treatment modalities on adherence to ART/HAART among a cohort of HIV seropositive women. American Journal of Drug & Alcohol Abuse. 2008;34:161–70. doi: 10.1080/00952990701877052. [DOI] [PubMed] [Google Scholar]
- 71.Feelemyer JP, Des Jarlais DC, Arasteh K, Phillips BW, Hagan H. Changes in quality of life (WHOQOL-BREF) and addiction severity index (ASI) among participants in opioid substitution treatment (OST) in low and middle income countries: an international systematic review. Drug Alcohol Depend. 2014;134:251–8. doi: 10.1016/j.drugalcdep.2013.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72*.Bachireddy C, Soule MC, Izenberg JM, Dvoryak S, Dumchev K, Altice FL. Integration of health services improves multiple healthcare outcomes among HIV-infected people who inject drugs in Ukraine. Drug Alcohol Depend. 2014;134:106–14. doi: 10.1016/j.drugalcdep.2013.09.020. This study provides evidence that integrating addiction, HIV and tuberculosis treatment in a middle income country improves treatment outcomes for all three conditions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Korthuis PT, Tozzi MJ, Nandi V, et al. Improved quality of life for opioid-dependent patients receiving buprenorphine treatment in HIV clinics. J Acquir Immune Defic Syndr. 2011;56(Suppl 1):S39–45. doi: 10.1097/QAI.0b013e318209754c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lucas GM, Chaudhry A, Hsu J, et al. Clinic-based treatment of opioid-dependent HIV-infected patients versus referral to an opioid treatment program: A randomized trial. Ann Intern Med. 2010;152:704–11. doi: 10.1059/0003-4819-152-11-201006010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sulkowski MS. Hepatitis C virus infection in HIV-infected patients. Curr HIV/AIDS Rep. 2004;1:128–35. doi: 10.1007/s11904-004-0019-6. [DOI] [PubMed] [Google Scholar]
- 76.Friedland G. Infectious disease comorbidities adversely affecting substance users with HIV: hepatitis C and tuberculosis. J Acquir Immune Defic Syndr. 2010;55(Suppl 1):S37–42. doi: 10.1097/QAI.0b013e3181f9c0b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Anderson JP, Tchetgen Tchetgen EJ, Lo Re V, 3rd, et al. Antiretroviral therapy reduces the rate of hepatic decompensation among HIV- and hepatitis C virus-coinfected veterans. Clin Infect Dis. 2014;58:719–27. doi: 10.1093/cid/cit779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Butt A, Kara C, Corey K, Chung R, Butler J. HCV Viremia and the Risk of Acute Myocardial Infarction at Various Lipid Levels. Conference on Retroviruses and Opportunistic Infections; Boston, MA. 2014; p. Abstract 685. [Google Scholar]
- 79.Erqou S, Mohanty A, Murtaza Kasi P, Butt AA. Predictors of Mortality among United States Veterans with Human Immunodeficiency Virus and Hepatitis C Virus Coinfection. ISRN gastroenterology. 2014;2014:764540. doi: 10.1155/2014/764540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mallet V, Thiébaut S, Yazdanpanah Y, et al. HCV Accelerates Non-Liver Mortality in HIV-Infected Patients: A Nationwide Cohort Study. Conference on Retroviruses and Opportunistic Infections; Boston, MA. 2014; p. Abstract 690. [Google Scholar]
- 81.Hernando V, Perez-Cachafeiro S, Lewden C, et al. All-cause and liver-related mortality in HIV positive subjects compared to the general population: differences by HCV co-infection. J Hepatol. 2012;57:743–51. doi: 10.1016/j.jhep.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 82.Andreoni M, Giacometti A, Maida I, Meraviglia P, Ripamonti D, Sarmati L. HIV-HCV co-infection: epidemiology, pathogenesis and therapeutic implications. European review for medical and pharmacological sciences. 2012;16:1473–83. [PubMed] [Google Scholar]
- 83.Aspinall EJ, Corson S, Doyle JS, et al. Treatment of hepatitis C virus infection among people who are actively injecting drugs: a systematic review and meta-analysis. Clin Infect Dis. 2013;57(Suppl 2):S80–9. doi: 10.1093/cid/cit306. [DOI] [PubMed] [Google Scholar]
- 84.Rotman Y, Liang TJ. Coinfection with hepatitis C virus and human immunodeficiency virus: virological, immunological, and clinical outcomes. J Virol. 2009;83:7366–74. doi: 10.1128/JVI.00191-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Feeney ER, Chung RT. Antiviral treatment of hepatitis C. BMJ. 2014;348:g3308. doi: 10.1136/bmj.g3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zeremski M, Martinez AD, Talal AH. Editorial commentary: Management of hepatitis C Virus in HIV-infected patients in the era of direct-acting antivirals. Clin Infect Dis. 2014;58:880–2. doi: 10.1093/cid/cit804. [DOI] [PubMed] [Google Scholar]
- 87.Molina JM, Orkin C, Iser DM, et al. All-oral therapy with sofosbuvir plus ribavirin for the treatment of HCV genotypes 1, 2, 3 and 4 infection in patients co-infected with HIV (PHOTON-2). AIDS 2014: 20th International AIDS Conference; Melbourne, Australia. 2014; p. Abstract MOAB0105LB. [Google Scholar]
- 88.Sulkowski M, Eron JJ, Wyles D, et al. TURQUOISE-I: safety and efficacy of ABT-450/r/ombitasvir, dasabuvir, and ribavirin in patients co-infected with hepatitis C and HIV-1. AIDS 2014: 20th International AIDS Conference; Melbourne, Australia. 2014; p. Abstract MOAB0104LB. [Google Scholar]
- 89.Ford N, Kirby C, Singh K, et al. Chronic hepatitis C treatment outcomes in low- and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ. 2012;90:540–50. doi: 10.2471/BLT.11.097147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hill A, Khoo S, Fortunak J, Simmons B, Ford N. Minimum costs for producing hepatitis C direct-acting antivirals for use in large-scale treatment access programs in developing countries. Clin Infect Dis. 2014;58:928–36. doi: 10.1093/cid/ciu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.World Health Organization (WHO) Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. Geneva, Switzerland: 2013. [Accessed July 27, 2013]. at: http://www.who.int/hiv/pub/guidelines/arv/download/en/index.html. [PubMed] [Google Scholar]
- 92.Getahun H, Gunneberg C, Sculier D, Verster A, Raviglione M. Tuberculosis and HIV in people who inject drugs: evidence for action for tuberculosis, HIV, prison and harm reduction services. Curr Opin HIV AIDS. 2012;7:345–53. doi: 10.1097/COH.0b013e328354bd44. [DOI] [PubMed] [Google Scholar]
- 93.Getahun H, Baddeley A, Raviglione M. Managing tuberculosis in people who use and inject illicit drugs. Bull World Health Organ. 2013;91:154–6. doi: 10.2471/BLT.13.117267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94*.Grenfell P, Baptista Leite R, Garfein R, de Lussigny S, Platt L, Rhodes T. Tuberculosis, injecting drug use and integrated HIV-TB care: a review of the literature. Drug Alcohol Depend. 2013;129:180–209. doi: 10.1016/j.drugalcdep.2012.11.013. An excellent review examining the prevalence of TB among PWUD and the models of care for people coinfected with HIV and TB. [DOI] [PubMed] [Google Scholar]
- 95.Baussano I, Williams BG, Nunn P, Beggiato M, Fedeli U, Scano F. Tuberculosis Incidence in Prisons: A Systematic Review. PLoS Med. 2010;7:e1000381. doi: 10.1371/journal.pmed.1000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dara M, Chadha SS, Vinkeles Melchers NV, et al. Time to act to prevent and control tuberculosis among inmates. Int J Tuberc Lung Dis. 2013;17:4–5. doi: 10.5588/ijtld.12.0909. [DOI] [PubMed] [Google Scholar]
- 97.Lawn SD, Kerkhoff AD, Vogt M, Wood R. Clinical significance of lipoarabinomannan detection in urine using a low-cost point-of-care diagnostic assay for HIV-associated tuberculosis. AIDS. 2012;26:1635–43. doi: 10.1097/QAD.0b013e3283553685. [DOI] [PubMed] [Google Scholar]
- 98.Lawn SD, Mwaba P, Bates M, et al. Advances in tuberculosis diagnostics: the Xpert MTB/RIF assay and future prospects for a point-of-care test. Lancet Infect Dis. 2013;13:349–61. doi: 10.1016/S1473-3099(13)70008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N. Xpert(R) MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev. 2014;1:CD009593. doi: 10.1002/14651858.CD009593.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Al-Darraji HAA, Razak H, Ng KP, Altice FL, Kamarulzaman A. The Diagnostic Performance of a Single GeneXpert MTB/RIF Assay in an Intensified Tuberculosis Case Finding Survey among HIV-infected Prisoners in Malaysia. PloS One. 2013;9:e73717. doi: 10.1371/journal.pone.0073717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Morozova O, Dvoryak S, Altice FL. Methadone treatment improves tuberculosis treatment among hospitalized opioid dependent patients in Ukraine. Int J Drug Policy. 2013;24:e91–8. doi: 10.1016/j.drugpo.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Selwyn PA, Feingold AR, Iezza A, et al. Primary care for patients with human immunodeficiency virus (HIV) infection in a methadone maintenance treatment program. Ann Intern Med. 1989;111:761–3. doi: 10.7326/0003-4819-111-9-761. [DOI] [PubMed] [Google Scholar]
- 103.O’Connor PG, Shi JM, Henry S, Durante AJ, Friedman L, Selwyn PA. Tuberculosis chemoprophylaxis using a liquid isoniazid-methadone admixture for drug users in methadone maintenance. Addiction. 1999;94:1071–5. doi: 10.1046/j.1360-0443.1999.947107112.x. [DOI] [PubMed] [Google Scholar]
- 104.Zahari MM, Hwan Bae W, Zainal NZ, Habil H, Kamarulzaman A, Altice FL. Psychiatric and substance abuse comorbidity among HIV seropositive and HIV seronegative prisoners in Malaysia. Am J Drug Alcohol Abuse. 2010;36:31–8. doi: 10.3109/00952990903544828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Buckingham E, Schrage E, Cournos F. Why the Treatment of Mental Disorders Is an Important Component of HIV Prevention among People Who Inject Drugs. Advances in preventive medicine. 2013;2013:690386. doi: 10.1155/2013/690386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Iskandar S, Kamal R, De Jong CA. Psychiatric comorbidity in injecting drug users in Asia and Africa. Curr Opin Psychiatry. 2012;25:213–8. doi: 10.1097/YCO.0b013e3283523d66. [DOI] [PubMed] [Google Scholar]
- 107.Saber-Tehrani AS, Bruce RD, Altice FL. Pharmacokinetic drug interactions and adverse consequences between psychotropic medications and pharmacotherapy for the treatment of opioid dependence. Am J Drug Alcohol Abuse. 2011;37:1–11. doi: 10.3109/00952990.2010.540279. [DOI] [PubMed] [Google Scholar]
- 108.Novick A. Stigma and AIDS: three layers of damage. J Gay Lesbian Med Assoc. 1997;1:53–60. [Google Scholar]
- 109.Earnshaw VA, Jin H, Wickersham J, Kamarulzaman A, John J, Altice FL. Exploring intentions to discriminate against patients living with HIV/AIDS among future healthcare providers in Malaysia. Tropical medicine & international health : TM & IH. 2014;19:672–9. doi: 10.1111/tmi.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jin H, Earnshaw VA, Wickersham JA, et al. An assessment of health-care students’ attitudes toward patients with or at high risk for HIV: implications for education and cultural competency. AIDS Care. 2014;26:1223–8. doi: 10.1080/09540121.2014.894616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lim T, Zelaya C, Latkin C, et al. Individual-level socioeconomic status and community-level inequality as determinants of stigma towards persons living with HIV who inject drugs in Thai Nguyen, Vietnam. J Int AIDS Soc. 2013;16:18637. doi: 10.7448/IAS.16.3.18637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Levi-Minzi MA, Surratt HL. HIV stigma among substance abusing people living with HIV/AIDS: implications for HIV treatment. AIDS Patient Care STDS. 2014;28:442–51. doi: 10.1089/apc.2014.0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Marsicano E, Dray-Spira R, Lert F, Aubriere C, Spire B, Hamelin C. Multiple discriminations experienced by people living with HIV in France: results from the ANRS-Vespa2 study. AIDS Care. 2014;26(Suppl 1):S97–s106. doi: 10.1080/09540121.2014.907385. [DOI] [PubMed] [Google Scholar]


