Abstract
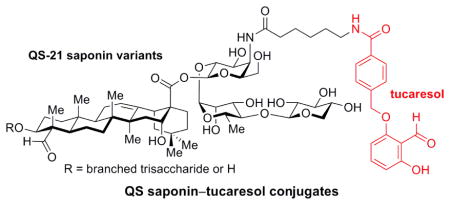
Immunoadjuvants are used to potentiate the activity of modern subunit vaccines that are based on molecular antigens. An emerging approach involves the combination of multiple adjuvants in a single formulation to achieve optimal vaccine efficacy. Herein, to investigate such potential synergies, we synthesized novel adjuvant conjugates based on the saponin natural product QS-21 and the aldehyde tucaresol via chemoselective acylation of an amine at the terminus of the acyl chain domain in QS saponin variants. In a preclinical mouse vaccination model, these QS saponin–tucaresol conjugates induced antibody responses similar to or slightly higher than those generated with related QS saponin variants lacking the tucaresol motif. The conjugates retained potent adjuvant activity, low toxicity, and improved activity–toxicity profiles relative to QS-21 itself and induced IgG subclass profiles similar to those of QS-21, indicative of both Th1 cellular and Th2 humoral immune responses. This study opens the door to installation of other substituents at the terminus of the acyl chain domain to develop additional QS saponin conjugates with desirable immunologic properties.
Keywords: Immunoadjuvant, Vaccine, QS-21, Tucaresol, Saponin conjugate, Natural product, Carbohydrates
Graphical abstract
1. Introduction
Modern vaccines based on homogeneous subunit antigens offer significant advantages over classical vaccines based on whole pathogens, enabling more precise targeting of the immune response and improved safety.1 However, such subunit vaccines are poorly immunogenic and require coadministration of an immunoadjuvant to potentiate the immune response and achieve optimal efficacy.2 Aluminum salts have been used as adjuvants in a number of vaccines, but are relatively weak immunopotentiators.3 Thus, more effective adjuvants are required to realize the full potential of subunit vaccines.
Accordingly, there is considerable current interest in using combinations of adjuvants in the same formulation to achieve complementary or even synergistic enhancement of immune responses.4 Several such Adjuvant Systems (AS) have been developed by GlaxoSmithKline5 and one, AS04, a combination of aluminum salts and monophosphoryl lipid A (MPL), was approved as part of the Cervarix vaccine for human papilloma virus.6 QS-21, a saponin natural product extracted from the bark of the South American tree Quillaja saponaria (QS),7 is one of the most potent adjuvants currently under clinical investigation (Figure 1). It has been used as an adjuvant in numerous vaccine clinical trials,8 either alone or in combinations with MPL (AS01, AS02).5 Notably, this includes the RTS,S/AS01 malaria vaccine, which has demonstrated promising early efficacy in a Phase 3 clinical trial in African children.9 However, the natural product suffers from several inherent limitations, including local and systemic dose-limiting toxicities,7,10 low-yielding purification from the natural source (<0.001% yield),7 chemical heterogeneity,11,12,13 hydrolytic instability (t90 shelf life = 24 d),14 and an enigmatic mechanism of action.15
Figure 1.
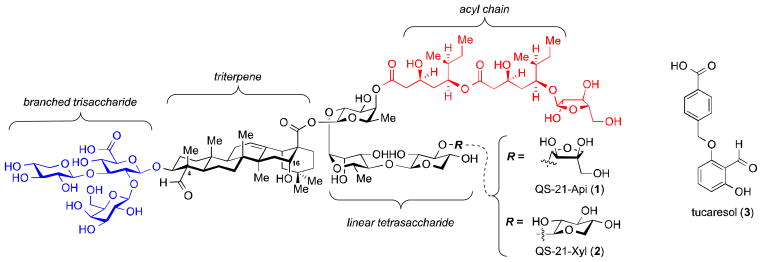
Chemical structures of the saponin adjuvant QS-21 (1/2, ≈2:1 apiose/xylose) and the aldehyde-containing adjuvant tucaresol (3).
To address these limitations, we have previously developed an efficient, flexible semisynthetic route to QS-21 and a wide variety of QS saponin variants. QS-21 is comprised of four structural domains: a branched trisaccharide, a quillaic acid triterpene, a linear tetrasaccharide, and a glycosylated acyl chain (Figure 1). The natural product actually consists of two isomers at the terminal sugar in the linear tetrasaccharide domain (QS-21-Api, 1 and QS-21-Xyl, 2).12 Following completion of the total syntheses of both isomers of QS-21,16,17 we prepared semisynthetic, amide-based acyl chain variants that overcame the hydrolytic instability issues and showed improved activity–toxicity ratios compared to the natural product.18 Stepwise truncation of the right-hand linear tetrasaccharide domain revealed that a trisaccharide is sufficient for optimal activity and could be accessed with considerably increased synthetic efficiency compared to the tetrasaccharide.19 Further modifications in the acyl chain domain also identified a 6-aminohexanoic amide variant that was adjuvant-inactive but provided a terminal amine that could undergo chemoselective acylation with restoration of adjuvant activity.19 More recently, the entire left-hand branched trisaccharide domain was found to be dispensable for adjuvant activity in QS saponin variants.20 Molecular editing in the triterpene domain revealed that the C4-aldehyde substituent is also dispensable for adjuvant activity while the C16-hydroxyl substituent enhances activity.20
Schiff-base formation between amino groups on T cells and carbonyl groups on the surface of antigen presenting cells is known to be an important event in the induction of immune responses.21 Aldehyde-containing adjuvants can substitute for these natural carbonyl groups forming imines with amino groups on T cell surface receptor(s) and providing a B7–CD28-independent co-stimulatory signal that leads to T-cell activation and Th1 immunity.22,23 One such aldehyde is tucaresol (3), which augments antigen-specific humoral and cellular immune responses22,24 and has undergone Phase I/II clinical trials in vaccines for chronic hepatitis B, HIV, and malignant melanoma.23,25 Although the C4-aldehyde substituent in the triterpene core of QS-21 has been proposed analogously to react covalently with an unidentified cell surface protein target,26 our recent finding that this aldehyde is dispensable for adjuvant activity in semisynthetic QS saponin variants has called this mechanism into question.20 Thus, we wondered whether the aldehyde-based activity of tucaresol might further potentiate the activity of novel QS saponin variants, either in combination or as a covalently-linked conjugate. Herein, we report the design and synthesis of two novel QS saponin–tucaresol conjugates to investigate this possibility. These covalent conjugates, as well as equimolar combinations of related QS saponin variants and tucaresol, were evaluated in a mouse vaccination model. The tucaresol-containing conjugates and combinations induced antibody responses similar to or slightly higher than those of the related QS saponin variants alone, with similar IgG subclass profiles. The conjugates also retained the decreased toxicity and improved activity–toxicity profiles of the related QS saponin variants compared to QS-21 itself, indicating that the QS saponins are amenable to significant structural modifications at the site of conjugation.
2. Results and discussion
2.1. Design and synthesis of saponin–tucaresol adjuvant conjugates
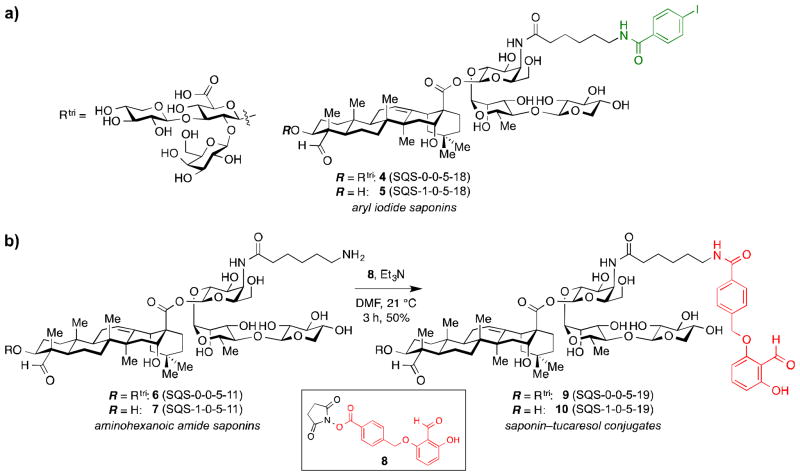
We envisioned that QS saponin adjuvants and tucaresol could be tested both as combinations of discrete molecules and as covalently-linked unimolecular conjugates. We have previously established aryl iodide variant 4 (SQS-0-0-5-18) as a potent adjuvant with low toxicity in a mouse preclinical vaccination model (Figure 2a).20 We have also demonstrated that a larger, fluoresceinyl substituent is tolerated at the terminus of the acyl chain (not shown).19 Thus, we envisioned that tucaresol could be attached analogously to the terminal amino group of 6-aminohexanoic amide variant 6 (SQS-0-0-5-11)19 by amidation of its carboxylic acid functionality. Modification of tucaresol at this position with retention of adjuvant activity has recently been demonstrated via lipidation.27 Tucaresol (3) was readily synthesized in three steps starting from commercially available material.28 Activation of the tucaresol carboxylic acid (EDCI/NHS), followed by coupling of the corresponding NHS ester 8 to saponin amine 6 (SQS-0-0-5-11), prepared as previously described,19 afforded the saponin–tucaresol conjugate 9(SQS-0-0-5-19) (Figure 2b).
Figure 2.
(a) Chemical structures of adjuvant-active aryl iodide saponins 4 (SQS-0-0-5-18) and 5 (SQS-1-0-5-18).20 (b) Synthesis of saponin–tucaresol conjugates 9 (SQS-0-0-5-19) and 10 (SQS-1-0-5-19).
We have demonstrated previously that the branched trisaccharide domain is not required for potent adjuvant activity in several QS saponin variants such as aryl iodide 5 (SQS-1-0-5-18) (Figure 2a).20 Thus, we also synthesized the corresponding saponin–tucaresol conjugate 10 (SQS-1-0-5-19), which lacks the entire branched trisaccharide domain. Amine precursor 7 (SQS-1-0-5-11), prepared as previously described,20 was acylated with tucaresol NHS ester 8 as above, to afford the structurally simplified saponin–tucaresol conjugate 10.
2.2. Immunologic evaluation of saponin–tucaresol adjuvant conjugates
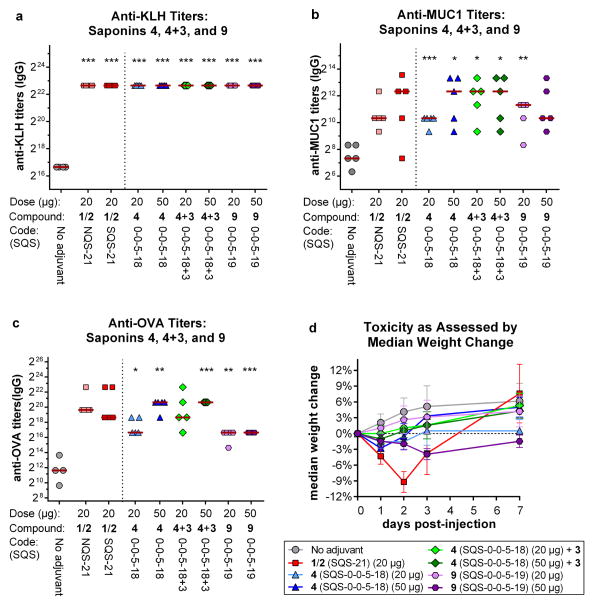
We evaluated these saponin–tucaresol conjugates, as well as equimolar combinations of the discrete molecules, for immunostimulatory activity using an established mouse vaccination model involving a multiple antigen formulation comprised of MUC1 peptide, a clinically relevant antigen in prostate and breast cancers, conjugated to the highly immunogenic KLH carrier protein (MUC1–KLH), and ovalbumin (OVA), an established immunogen commonly used to study antibody responses. Groups of five mice (C57BL/6J, female, 8–10 weeks of age) were vaccinated with this three-component vaccine of MUC1–KLH (2.5 μg MUC1 equivalent) and OVA (20 μg), with coadministration of the adjuvant of interest (saponins and saponin–tucaresol conjugates at 20 and 50 μg; tucaresol at 3.1 and 7.8 μg, representing same molar equivalents as present in the covalent conjugates) or without adjuvant (negative control). Synthetic QS-21 (SQS-21, 2:1 mixture of 1 and 2) and the related aryl iodide saponins 4 (SQS-0-0-5-18) and 5 (SQS-1-0-5-18) were used as positive controls. Mice were vaccinated by subcutaneous injections at 1-week intervals (days 0, 7, and 14), plus a booster on day 73. Mouse sera were collected on day 80 and antibody titers against KLH, MUC1, and OVA were determined by ELISA. As a general assessment of overall toxicity, weight loss of mice was monitored at 0, 1, 2, 3, and 7 days after the first vaccination, during which time acute toxicity of QS-21 is readily observed.
In an initial control experiment, tucaresol alone (250 μg) was inactive.29 The equimolar combination of tucaresol (3) with aryl iodide saponin variant 4 (SQS-0-0-5-18) induced antibody titers against all antigens that were comparable to those of NQS-21 and SQS-21 and significantly higher than those of the negative control (except OVA at the lower dose), but these were similar to (KLH) or only slightly higher than (MUC1 and OVA) those elicited by aryl iodide 4 alone (Figure 3a–c). Mice vaccinated with saponin–tucaresol conjugate 9 (SQS-0-0-5-19) also generated antibody titers against all antigens that were similar to those of NQS-21 and SQS-21, and higher than those of the no-adjuvant control, but these titers were also similar to (KLH) or slightly lower than (MUC1 and OVA) those induced in mice vaccinated with aryl iodide 4 (SQS-0-0-5-18), alone or in combination with tucaresol. Overall, the addition of equimolar tucaresol (3) to aryl iodide 4 (SQS-0-0-5-18) increased antibody responses marginally compared with 4 alone while covalent attachment of tucaresol to the saponin in 9 did not result in increased antibody titers relative to 4.
Figure 3.
Immunologic evaluation of saponin–tucaresol conjugate 9 (SQS-0-0-5-19) and of equimolar combinations of aryl iodide saponin 4 (SQS-0-0-5-18) and tucaresol (3) with a three-component vaccine comprised of MUC1–KLH and OVA for (a) anti-KLH titers (IgG), (b) anti-MUC1 titers (IgG), and (c) anti-OVA titers (IgG). Antibody titers shown for KLH with all adjuvants represent the maximum dilution tested (6,533,600-fold). Horizontal bars indicate median titers; statistical significance compared to no-adjuvant negative control was assessed using two-tailed unpaired Student T-test with CI = 95%: * p ≤ 0.05, ** p < 0.01, *** p < 0.001. (d) Toxicity assessment based on median weight loss over one week after the first vaccine injection. Error bars
As with the related aryl iodide 4 (SQS-0-0-5-18), the saponin–tucaresol conjugate 9 (SQS-0-0-5-19) was considerably less toxic than SQS-21, as judged by mouse weight loss, although some progressive weight loss was observed at the higher dose at timepoints where mice in other cohorts were already recovering (Figure 3d). Tucaresol itself was also not toxic at the doses used, with the combination of tucaresol (3) and aryl iodide saponin 4 leading to weight losses comparable to those induced by aryl iodide saponin 4 alone.
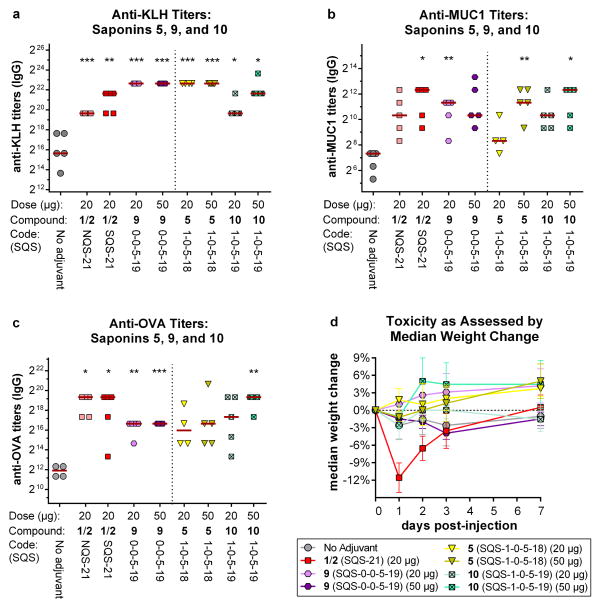
In the corresponding series lacking the branched trisaccharide domain, the saponin–tucaresol conjugate 10 (SQS-1-0-5-19) elicited, at the higher dose, antibody titers comparable to NQS-21 and SQS-21 for all antigens and, in the case of MUC1 and OVA, somewhat higher than those of the branched trisaccharide-containing conjugate 9 (SQS-0-0-5-19) (Figure 4a–c). The MUC1 and OVA titers were also slightly higher than those obtained with the aryl iodide 5 (SQS-1-0-5-18) at corresponding doses. The truncated conjugate 10 again showed low toxicity as judged by mouse weight loss, considerably less than SQS-21, and generally comparable to aryl iodide 5 (Figure 4d).
Figure 4.
Immunologic evaluation of saponin–tucaresol conjugate 10 (SQS-1-0-5-19), lacking the branched trisaccharide domain, with a three-component vaccine comprised of MUC1–KLH and OVA for (a) anti-KLH titers (IgG), (b) anti-MUC1 titers (IgG), and (c) anti-OVA titers (IgG). Data for the branched-trisaccharide containing conjugate 9 (SQS-0-0-5-19) is from the separate experiment shown in Figure 3, shown here for comparison. Horizontal bars indicate median titers; statistical significance compared to no-adjuvant negative control was assessed using two-tailed unpaired Student T-test with CI = 95%: * p ≤ 0.05, ** p < 0.01, *** p< 0.001. (d) Toxicity assessment based on median weight loss over one week after the first vaccine
Antibody subtyping of the anti-OVA IgG isotypes elicited by both saponin–tucaresol conjugates 9 (SQS-0-0-5-19) and 10 (SQS-1-0-5-19) revealed a bias toward the IgG1 and IgG2b subclasses (Table 1). Branched trisaccharide-containing conjugate 9 elicited slightly higher IgG2a and slightly lower IgG2b antibody levels than its aryl iodide congener 4 (SQS-0-0-5-18). Meanwhile, the truncated conjugate 10 produced slightly higher IgG1 and IgG2b titers than its aryl iodide counterpart 5 (SQS-1-0-5-18), and the IgG2b levels were also higher than the branched trisaccharide-containing conjugate 9. Production of other mouse IgG subtypes, such as IgG3, was low or negligible in all cases. The mouse IgG1 subclass is associated with Th2 responses (humoral immunity), whereas the IgG2b, together with the IgG2a, are related to Th1 responses (cellular immunity) and known to induce potent immunotherapeutic effector functions,30 including complement-dependent cytotoxicity and antibody-dependent cellular toxicity. Similar subtyping results were obtained with SQS-21, suggesting that, despite the considerable structural differences between these synthetic variants and QS-21, they elicit both Th1 and Th2 immunity, a distinctive characteristic of QS-21 itself.
Table 1.
IgG isotyping of anti-OVA antibodies resulting from mouse vaccinations with MUC1–KLH (2.5 μg), and OVA (20μg) in the presence of various saponin adjuvants.a
| adjuvant | IgG1 | IgG2a | IgG2b | IgG3 |
|---|---|---|---|---|
| 1/2 (SQS-21) | +++ | +/− | ++ | − |
| 4 (SQS-0-0-5-18) | +++ | − | ++ | − |
| 5 (SQS-1-0-5-18) | ++ | − | +/− | − |
| 9 (SQS-0-0-5-19) | +++ | +/− | + | − |
| 10 (SQS-1-0-5-19) | +++ | − | ++ | − |
Isotype titer levels: − = 0; +/− = 1–80; + = 81–160; ++ = 161–1280; +++ = >1280
3. Conclusion
Taken together, these results indicate that conjugation of the aldehyde-containing adjuvant tucaresol (3) to semisynthetic QS saponin adjuvants leads to similar or slightly increased antibody responses in a mouse vaccination model compared to closely-related QS saponin variants that lack the tucaresol motif. Slight differences in IgG subtype profiles were also observed in both series. The saponin–tucaresol conjugates 9 (SQS-0-0-5-19) and 10 (SQS-1-0-5-19) retain potent adjuvant activity, comparable to that of the natural product QS-21, providing further evidence that the terminus of the acyl chain domain is amenable to considerable structural modifications. This is consistent with the adjuvant activity of other QS saponin variants that we have reported previously having aryl iodide (4, SQS-0-0-5-18 and 5, SQS-1-0-5-18)20 and fluoresceinyl19 substituents at this position. It should be noted that other anionic fluorescent substituents are not well-tolerated at this position.19 While it is possible that these anionic groups may compromise interactions with a putative molecular target, they also introduce negative charge, which may alternatively lead to changes in biodistribution or subcellular localization. Moreover, we have now demonstrated that both the aryl iodides 4 and 5 and the saponin–tucaresol conjugates 9 and 10 induce anti-OVA IgG subclasses that are predominantly IgG1 and IgG2b, similar to those elicited by QS-21 itself, and indicative of induction of both Th2 and Th1 responses, respectively. Overall, these results raise the possibility of conjugating other non-anionic moieties via convenient chemoselective acylation of amines 6 (SQS-0-0-5-11) and 7 (SQS-1-0-5-11) to develop additional saponin probes and conjugates that may be useful for mechanism-of-action studies, tuning of desired immune responses to various subunit antigen vaccines, and even direct conjugation with antigens to generate novel unimolecular subunit vaccines..
4. Experimental
4.1. General synthetic materials and methods
1H NMR and 13C NMR spectra were recorded on a Bruker Avance III instrument; chemical shifts are expressed in parts per million (δ scale) downfield from tetramethylsilane, and are referenced to residual proton in the NMR solvent, (CD3)2SO: δ 2.50 for 1H NMR, δ 39.9 for 13C NMR; CDCl3: δ 7.26 for 1H NMR, δ 77.0 for 13C NMR; CD3OD: δ 3.31 for 1H NMR, δ 49.2 for 13C NMR. Data are presented as follows: chemical shift, multiplicity (s = singlet, bs = broad singlet, d = doublet, t = triplet, q = quartet, m = multiplet and/or multiple resonances), coupling constant in Hertz (Hz), integration. RP-HPLC purifications and analyses were carried out on a Waters 2545 binary gradient HPLC system equipped with a Waters 2996 photodiode array detector, and absorbances were monitored at wavelengths of 210–600 nm.
Reactions were performed in a roundbottom flask fitted with a rubber septum under a positive pressure of Ar. Air- and moisture-sensitive liquids and solutions were transferred via syringe. Flash column chromatography was performed using 230–400 mesh silica gel. Thin-layer chromatography was performed using glass plates pre-coated to a depth of 0.25 mm with 230–400 mesh silica gel impregnated with a fluorescent indicator (254 nm). Et3N was distilled from CaH at 760 Torr under N2. All other reagents were obtained from commercial vendors and were used without further purification unless noted otherwise.
Tucaresol (3) was synthesized as previously described, and the spectral data was found to be in agreement with prior reported characterization of tucaresol.28 Amine precursors 6 and 7 were synthesized as previously described.19,20
4.2. Synthesis of N-hydroxysuccinimidyl ester of tucaresol (8)
Tucaresol (3) (40 mg, 0.15 mmol, 1.0 equiv) was dissolved in DMF (1.8 mL) and Et3N (60 μL, 0.44 mmol, 3.0 equiv) was added via syringe. EDC (42 mg, 0.22 mmol, 1.5 equiv) and NHS (34 mg, 0.29 mmol, 2.0 equiv) were then added gradually, and the reaction was stirred at 21 ºC for 22 h. The mixture was diluted with EtOAc (50 mL) and washed with water (0.05% TFA) (2 × 10 mL). The organic layer was dried (Na2SO4), filtered, and concentrated by rotary evaporation. Purification by silica flash chromatography (1:1 hexanes/EtOAc) gave tucaresol NHS ester 8 (25 mg, 50% yield) as a white solid.
TLC: Rf 0.30 (1:1 hexanes/EtOAc). 1H NMR (500 MHz, CDCl3) δ11.98 (s, 1H, OH), 10.45 (s, 1H, CHO), 8.18 (d, J = 8.2 Hz, 2H, ArH), 7.57 (d, J = 8.1 Hz, 2H, ArH), 7.40 (t, J = 8.4 Hz, 1H, ArH), 6.58 (d, J = 8.5 Hz, 1H, ArH), 6.38 (d, J = 8.3 Hz, 1H, ArH), 5.25 (s, 2H, OCH2), 2.92 (br s, 4H, -CH2CH2-). 13C NMR (151 MHz, CDCl3) δ 193.9, 169.1, 161.8, 161.4, 142.6, 138.9, 131.1, 128.1, 127.2, 117.0, 115.7, 115.1, 76.0, 25.7. HRMS (ESI) m/z: Calcd for C19H15NO7Na (M+Na)+ 392.0746, found 392.0764.
4.3. General procedure for the synthesis of saponin–tucaresol conjugates (9 and 10)
To a solution of the saponin amine (6 or 7) (6.6 or 3.4 μmol, 10.0 or 3.5 mg, 1.0 equiv) in DMF (2.0 or 1.2 mL), Et3N (0.36 or 0.19 mmol, 50 or 26 μL, 55 equiv) was added via syringe and the mixture stirred at 21 °C for 10 min. Tucaresol NHS ester 8 (30 or 15.3 μmol, 11.0 or 5.6 mg, 4.5 equiv) in DMF (2.0 or 1.2 mL) was added dropwise and the reaction stirred at 21 °C for 3 h. The contents were diluted with CH3CN in water (20%, 8 mL or 30%, 6 mL) and purified directly by HPLC on an XBridge Prep BEH300 C18 column (5 μm, 10 × 250 mm) using a linear gradient of CH3CN/water (0.05% TFA, 20–95% over 30 min, or 40–65% over 18 min), at a flow rate of 5 mL/min. Saponin–tucaresol conjugate 9 (SQS-0-0-5-19) (5.7 mg, 50%) or 10 (SQS-1-0-5-19) (2.1 mg, 48%) was obtained as a white powder after lyophilization.
4.3.1. Saponin–tucaresol conjugate 9
HPLC: tret = 11.93 min, λmax = 277 nm. 1H NMR (600 MHz, CD3OD) characteristic resonances: δ 10.42 (s, 1H), 9.44 (s, 1H), 7.88–7.82 (m, 2H), 7.61–7.55 (m, 2H), 7.46 (t, J = 8.4 Hz, 1H), 6.62 (d, J = 8.3 Hz, 1H), 6.52 (d, J = 8.4 Hz, 1H), 5.36 (d, J = 1.4 Hz, 1H), 5.34 (d, J = 7.5 Hz, 1H), 5.31–5.26 (m, 3H), 4.81 (d, J = 7.2 Hz, 1H), 4.58 (d, J = 7.7 Hz, 1H), 4.49 (s, 1H), 4.47 (d, J = 7.7 Hz, 1H), 4.44 (d, J = 7.3 Hz, 1H), 4.33 (d, J = 2.5 Hz, 1H), 3.96–3.88 (m, 4H), 3.88–3.75 (m, 7H), 3.73 (dd, J = 11.3, 5.8 Hz, 1H), 3.71–3.62 (m, 3H), 3.57–3.51 (m, 2H), 3.25–3.16 (m, 5H), 2.93 (dd, J = 14.6, 4.0 Hz, 1H), 2.40–2.27 (m, 3H), 1.39 (s, 3H), 1.31 (d, J = 6.1 Hz, 1H), 1.16 (s, 3H), 0.99 (s, 3H), 0.94 (s, 3H), 0.87 (s, 3H), 0.74 (s, 3H). 13C NMR (151 MHz, CD3OD) δ 211.15, 195.65, 178.40, 177.08, 169.96, 164.84, 163.05, 158.97, 144.97, 141.54, 139.90, 135.81, 131.77, 128.83, 128.70, 128.42, 123.30, 112.38, 111.06, 107.25, 105.11, 104.96, 104.10, 103.93, 103.58, 101.66, 95.63, 86.74, 84.51, 79.66, 78.37, 76.84, 76.40, 76.32, 75.54, 75.41, 75.08, 75.06, 74.77, 73.74, 72.40, 72.08, 71.26, 71.13, 70.95, 69.06, 67.46, 67.32, 62.29, 61.84, 56.42, 52.67, 50.14, 50.00, 49.72, 48.15, 48.09, 42.88, 42.41, 41.20, 41.04, 39.36, 37.25, 36.70, 33.64, 33.54, 32.26, 31.48, 30.36, 27.72, 27.35, 26.98, 25.92, 24.97, 24.64, 21.63, 18.55, 17.87, 16.52, 11.13. HRMS (ESI) m/z: Calcd for C85H122N2O37Na (M+Na)+ 1785.7624, found 1785.7561.
4.3.2. Saponin–tucaresol conjugate 10
HPLC: tret = 12.98 min, λmax = 277 nm. 1H NMR (600 MHz, CD3OD) characteristic resonances: δ 10.42 (s, 1H), 9.30 (s, 1H), 7.88–7.83 (m, 2H), 7.60–7.55 (m, 2H), 7.46 (t, J = 8.4 Hz, 1H), 6.62 (d, J = 8.4 Hz, 1H), 6.52 (d, J = 8.4 Hz, 1H), 5.40 (s, 1H), 5.34 (d, J = 7.2 Hz, 1H), 5.31–5.26 (m, 3H), 4.52–4.46 (m, 2H), 4.37 – 4.31 (m, 1H), 3.97–3.89 (m, 3H), 3.69 (t, J = 6.6 Hz, 1H), 3.56 (t, J = 9.5 Hz, 1H), 3.25–3.16 (m, 3H), 2.93 (dd, J = 14.0, 4.0 Hz, 1H), 2.41–2.27 (m, 3H), 1.40 (s, 3H), 1.32 (d, J = 6.3 Hz, 3H), 1.01 (s, 3H), 1.00 (s, 3H), 0.94 (s, 3H), 0.87 (s, 3H), 0.76 (s, 3H). 13C NMR (151 MHz, CD3OD) δ 208.94, 195.64, 177.09, 169.97, 164.83, 163.05, 144.92, 141.52, 139.89, 135.82, 128.83, 128.69, 128.41, 123.33, 117.57, 115.06, 112.37, 111.06, 107.10, 104.95, 104.08, 101.39, 95.72, 84.18, 78.31, 76.45, 76.29, 75.06, 74.81, 74.41, 72.99, 72.35, 72.03, 71.25, 71.22, 68.99, 67.46, 61.85, 56.95, 52.68, 50.15, 50.00, 49.72, 48.15, 42.93, 42.53, 41.25, 41.04, 39.66, 37.13, 36.69, 36.63, 33.77, 33.53, 32.13, 31.48, 30.37, 27.72, 27.34, 27.15, 26.98, 24.99, 24.63, 22.04, 18.49, 17.89, 16.48, 9.64. HRMS (ESI) m/z: Calcd for C68H96N2O22Na (M+Na)+ 1315.6352, found 1315.6376.
4.4. Biological material and methods
4.4.1. Preparation of MUC1– KLH conjugate
MUC1 peptide containing 33 amino acids: CHGVTSAPDTRPAPGSTAPPAHGVTSAPDTRPA–OH, (synthesized at MSKCC’s Microchemistry Core facility) was covalently conjugated to KLH (Sigma Chemical Co., St Louis, MO) using an MBS (m-maleimidobenzoyl-N-hydroxysuccinimide ester) linker as previously described.31 Briefly, 5 mg MBS in 70 μl DMF (Sigma Chemical Co., St Louis, MO) was added to 9 mg KLH in 1.0 ml 0.01 M phosphate buffer, pH 7.0. After 1 hour incubation at room temperature, the MBS activated KLH was separated using a Sephadex G 15 column equilibrated with 0.1 M phosphate buffer (pH 6.0), and stirred with 5 mg MUC1 peptide for 2 h at room temperature. The unconjugated peptide was separated using a Centriprep 30. The epitope ratio of MUC1:KLH was 1367:1 (calculated based on the initial amount of peptide and KLH, the amount of unconjugated peptide in the filtrate, and a KLH molecular weight of 8.6×106 Da).
4.4.2. Mouse vaccination
Groups of five mice (C57BL/6J, female, 6–8 weeks old) were vaccinated three times with indicated combinations of MUC1-KLH (2.5 μg equivalent of MUC1), and/or OVA (20 μg, Sigma Chemical Co., St Louis, MO) in 100 μL phosphate buffered saline either alone (without adjuvant), with natural or synthetic QS-21 (NQS-21 or SQS-21), or with other saponins at indicated doses. Vaccines were administered subcutaneously to each mouse on days 0, 7, 14, and 73. Mice were bled 7 days after the third and fourth vaccinations.
4.4.3. Measurement of immunological response and toxicity
The presence of antibodies was tested by an enzyme-linked immunosorbent assay (ELISA). ELISAs were performed to determine antibody response against MUC1, OVA, and/or KLH as described previously.31 The ELISA plates were coated with either MUC1 antigen at 0.1 μg/well in carbonate buffer (pH 10), OVA antigen, at 0.1 μg/well in carbonate buffer (pH 10), or KLH at 0.1 μg/well in carbonate buffer (pH 10). The MUC1, OVA or KLH coated plates were incubated at 4 ºC overnight. ELISA plates were washed, blocked with 1% human serum albumin (HSA) in phosphate-buffered saline containing 0.05% Tween 20. Serially diluted pre- and post-vaccination sera in PBS with 1% HSA were added to wells of the coated plate with appropriate controls and incubated for 1 h at room temperature. After wash, goat anti-mouse IgM or IgG conjugated with alkaline phosphatase (AP) (Southern Biotechnology Associates, Inc., Birmingham, AL) was added to each well. Absorbance was measured at 405 nm. The titer was defined as the highest serum dilution that showed an absorbance of 0.1 or greater over that of the pre-sera. As standard initial assessment of overall toxicity, the weight loss of the mice was monitored at 0, 1, 2, 3 and 7 days after the first vaccination.
4.4.4. IgG isotyping
IgG subclasses were determined by using subclass-specific antibodies conjugated with AP (Southern Biotech, Birmingham, AL, USA). Flat-bottomed ELISA plates (96 wells, Nunc, Rochester, NY, USA) were pre-coated with OVA antigen, at 0.1 μg per well in carbonate buffer. Mouse sera diluted at 1:20 in 1% HSA (Grifols Biologicals, Los Angeles, CA, USA) were added with positive and negative controls. These wells were probed using class-specific IgG antibodies such as IgG 1, IgG2a, IgG2b, and IgG3, conjugated with AP at 1:1000 dilutions, respectively. The samples were measured at the end of 10 minutes at 405 nm followed by substrate solution. Samples were considered positive if the absorbance was above 0.1 OD at 405 nm.
Supplementary Material
Acknowledgments
This work is dedicated to the memory of our mentor and colleague, Prof. David Y. Gin (1967–2011). We thank Prof. Samuel J. Danishefsky for helpful discussions, and Dr. George Sukenick, Dr. Hui Liu, Hui Fang, and Dr. Sylvi Rusli (MSKCC NMR Analytical Core Facility) for expert mass spectral analyses. Financial support was provided by the European Commission (Marie Curie International Outgoing Fellowship to A.F.-T.), NIH (R01 AI085622 to J.S.L. and D.Y.G., R01 GM058833 to D.S.T. and D.Y.G., CCSG P30 CA008748 in support of the Clinical Grade Production Facility and the Center of Comparative Medicine and Pathology), William and Alice Goodwin and the Commonwealth Foundation for Cancer Research, and the Experimental Therapeutics Center of MSKCC.
Abbreviations
- AS
adjuvant systems
- MPL
monophosphoryl lipid A
- QS
Quillaja Saponaria
- EDCI
N-(3-dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride
- NHS
N-hydroxysuccinimide
- KLH
keyhole limpet hemocyanin
- MUC1
mucin-1
- OVA
ovalbumin
- MBS
m-maleimidobenzoyl-N-hydroxysuccinimide ester
- HSA
human serum albumin
- AP
alkaline phosphatase
Footnotes
The authors declare competing financial interests: J. R. G., P. O. L., G. R., and D. Y. G. are founders of and have financial interests in Adjuvance Technologies, Inc.
NMR spectra for saponin–tucaresol conjugates 9 and 10. Supplementary data associated with this article can be found, in the online version.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and notes
- 1.(a) Moyle PM, Toth I. ChemMedChem. 2013;8:360. doi: 10.1002/cmdc.201200487. [DOI] [PubMed] [Google Scholar]; (b) Koff WC, Burton DR, Johnson PR, Walker BD, King CR, Nabel GJ, Ahmed R, Bhan MK, Plotkin SA. Science. 2013;340:1232910. doi: 10.1126/science.1232910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.(a) Coffman RL, Sher A, Seder RA. Immunity. 2010;33:492. doi: 10.1016/j.immuni.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]; (b) Leroux-Roels G. Vaccine. 2010;28(Suppl 3):C25. doi: 10.1016/j.vaccine.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 3.(a) Lindblad EB. Immunol Cell Biol. 2004;82:497. doi: 10.1111/j.0818-9641.2004.01286.x. [DOI] [PubMed] [Google Scholar]; (b) Marrack P, McKee AS, Munks MW. Nat Rev Immunol. 2009;9:287. doi: 10.1038/nri2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mutwiri G, Gerdts V, van Drunen Littel-van den Hurk S, Auray G, Eng N, Garlapati S, Babiuk LA, Potter A. Expert Rev Vaccines. 2011;10:95. doi: 10.1586/erv.10.154. [DOI] [PubMed] [Google Scholar]
- 5.Garcon N, Chomez P, Van Mechelen M. Expert Rev Vaccines. 2007;6:723. doi: 10.1586/14760584.6.5.723. [DOI] [PubMed] [Google Scholar]
- 6.Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Skinner SR, Hedrick J, Jaisamrarn U, Limson G, Garland S, Szarewski A, Romanowski B, Aoki FY, Schwarz TF, Poppe WA, Bosch FX, Jenkins D, Hardt K, Zahaf T, Descamps D, Struyf F, Lehtinen M, Dubin G HPV PATRICIA Study Group. Lancet. 2009;374:301. doi: 10.1016/S0140-6736(09)61248-4. [DOI] [PubMed] [Google Scholar]
- 7.Kensil CR, Patel U, Lennick M, Marciani D. J Immunol. 1991;146:431. [PubMed] [Google Scholar]
- 8.Ragupathi G, Gardner JR, Livingston PO, Gin DY. Exp Rev Vaccines. 2011;10:463. doi: 10.1586/erv.11.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The RTS,S Clinical Trials Partnership. New Engl J Med. 2011;365:1863. [Google Scholar]
- 10.Kensil CR, Kammer R. Expert Opin Invest Drugs. 1998;7:1475. doi: 10.1517/13543784.7.9.1475. [DOI] [PubMed] [Google Scholar]
- 11.Soltysik S, Bedore DA, Kensil CR. Ann N Y Acad Sci. 1993;690:392. doi: 10.1111/j.1749-6632.1993.tb44041.x. [DOI] [PubMed] [Google Scholar]
- 12.Jacobsen NE, Fairbrother WJ, Kensil CR, Lim A, Wheeler DA, Powell MF. Carbohydr Res. 1996;280:1. doi: 10.1016/0008-6215(95)00278-2. [DOI] [PubMed] [Google Scholar]
- 13.Kamstrup S, San Martin R, Doberti A, Grande H, Daalsgard K. Vaccine. 2000;18:2244. doi: 10.1016/s0264-410x(99)00560-5. [DOI] [PubMed] [Google Scholar]
- 14.Cleland JL, Kensil CR, Lim A, Jacobsen NE, Basa L, Spellman M, Wheeler DA, Wheeler DA, Wu J-Y, Powell MF. J Pharm Sci. 1996;85:22. doi: 10.1021/js9503136. [DOI] [PubMed] [Google Scholar]
- 15.Pink JR, Kieny M-P. Vaccine. 2004;22:2097. doi: 10.1016/j.vaccine.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 16.(a) Wang P, Kim YJ, Navarro-Villalobos M, Rohde BD, Gin DY. J Am Chem Soc. 2005;127:3256. doi: 10.1021/ja0422007. [DOI] [PubMed] [Google Scholar]; (b) Kim YJ, Wang P, Navarro-Villalobos M, Rohde BD, Derryberry J, Gin DY. J Am Chem Soc. 2006;128:11906. doi: 10.1021/ja062364i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deng K, Adams MM, Damani P, Livingston PO, Ragupathi G, Gin DY. Angew Chem, Int Ed. 2008;47:6395. doi: 10.1002/anie.200801885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adams MM, Damani P, Perl N, Won A, Hong F, Livingston PO, Ragupathi G, Gin DY. J Am Chem Soc. 2010;132:1939. doi: 10.1021/ja9082842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chea EK, Fernández-Tejada A, Damani P, Adams MM, Gardner JR, Livingston PO, Ragupathi G, Gin DY. J Am Chem Soc. 2012;134:13448. doi: 10.1021/ja305121q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fernández-Tejada A, Chea EK, George C, Pillarsetty N, Gardner JR, Livingston PO, Ragupathi G, Lewis JS, Tan DS, Gin DY. Nature Chem. 2014;6:635. doi: 10.1038/nchem.1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.(a) Rhodes J. J Immun. 1989;143:1482. [PubMed] [Google Scholar]; (b) Gao XM, Rhodes J. J Immun. 1990;144:2883. [PubMed] [Google Scholar]; (c) Rhodes J. J Immun. 1990;145:463. [PubMed] [Google Scholar]
- 22.Rhodes J, Chen H, Hall SR, Beesley JE, Jenkins DC, Collins P, Zheng B. Nature. 1995;377:71–75;. doi: 10.1038/377071a0. [DOI] [PubMed] [Google Scholar]
- 23.(a) Chen H, Rhodes J. J Mol Med. 1996;74:497. doi: 10.1007/BF00204975. [DOI] [PubMed] [Google Scholar]; (b) Rhodes J. Clin Exp Immunol. 2002;130:363. doi: 10.1046/j.1365-2249.2002.02016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charo J, Sundbäck M, Wasserman K, Ciupitu A-MT, Mirzai B, van der Zee R, Kiessling R. Infect Immun. 2002;70:6652. doi: 10.1128/IAI.70.12.6652-6657.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gori A, Trabattoni D, Bandera A, Saresella M, Marchetti G, Gazzola L, Biasin M, Rhodes J, McDade H, Panebianco R, Galli M, Moroni M, Ferrante P, Thomas N, Franzetti F, Bray D, Clerici M. Antivir Ther. 2004;9:603. [PubMed] [Google Scholar]
- 26.Marciani DJ. Drug Discov Today. 2003;8:934–943. doi: 10.1016/s1359-6446(03)02864-2. [DOI] [PubMed] [Google Scholar]
- 27.Collins KC, Schlosburg JE, Lockner JW, Bremer PT, Ellis BA, Janda KD. Chem Commun. 2014;50:4079. doi: 10.1039/c4cc00682h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zacharie B, Attardo G, Barriault N, Penney C. J Chem Soc, Perkin Trans 1. 1997:2925. [Google Scholar]
- 29.In preliminary experiments, tucaresol alone (250 μg) did not induce antibody titers significantly higher than the no-adjuvant negative control in mouse vaccinations with OVA (20 μg).
- 30.Nimmerjahn F, Ravetch JV. Science. 2005;310:1510. doi: 10.1126/science.1118948. [DOI] [PubMed] [Google Scholar]
- 31.Gilewski T, Adluri R, Ragupathi G, Zhang S, Yao T-J, Panageas K, Moynahan M, Houghton AN, Norton L, Livingston PO. Clin Cancer Res. 2000;6:1693. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.