Abstract
Objective
To explore the factor structure of the Kessler Foundation Neglect Assessment Process (KF-NAP), and evaluate the prevalence and clinical significance of spatial neglect among stroke survivors.
Design
Inception cohort.
Setting
Inpatient rehabilitation facility (IRF).
Participants
121 participants with unilateral brain damage from their first stroke were assessed within 72 hours of admission to an IRF, and 108 were assessed again within 72 hours before IRF discharge.
Interventions
Usual and standard IRF care.
Main Outcome Measures
During each assessment session, occupational therapists measured patients’ functions with the KF-NAP, Functional Independence Measure (FIM™) and Barthel Index (BI).
Results
The KF-NAP showed excellent internal consistency with a single-factor structure. The exploratory factor analysis revealed the KF-NAP to be unique from both the FIM and BI even though all three scales were correlated. 67.8% of the participants at admission and 47.2% at discharge presented with symptoms of spatial neglect (KF-NAP > 0). Participants showing the disorder at IRF admission were hospitalized longer than those showing no symptoms. Among those presenting with symptoms, the regression analysis showed that the KF-NAP scores at admission negatively predicted FIM scores at discharge, after controlling for age, FIM at admission, and length of stay.
Conclusions
The KF-NAP uniquely quantifies symptoms of spatial neglect by measuring functional difficulties that are not captured by the FIM or BI. Using the KF-NAP to measure spatial neglect, we found the disorder persistent after inpatient rehabilitation, and replicated previous findings showing that spatial neglect adversely affects rehabilitation outcome even after prolonged IRF care.
Keywords: spatial neglect, stroke rehabilitation outcome, functional assessment
Spatial neglect is a disorder of spatial attention, affecting perception and mental representation of spatial information, and planning and execution of motor action. It is common after a brain injury such as stroke, occurring in approximately 50% of right brain-damaged and 30% of left brain-damaged survivors (Table 1).1-7 Individuals with spatial neglect demonstrate a failure or slowness to respond, orient, or initiate action towards contra-lesional stimuli.8 Therefore, spatial neglect disrupts mobility and navigation (walking,9 wheelchair ambulation,10 and driving),11 reading,12 and social interactions.13 Patients with this disorder have poorer rehabilitation outcomes, experience greater safety risk during hospitalization, and are hospitalized longer as compared to those without spatial neglect.14, 15
Table 1.
Prevalence of spatial neglect following stroke with unilateral brain damage
| Report* (ordered chronically) | Neglect prevalence (out of a given sample size) | Neglect assessment | Setting | Country | |
|---|---|---|---|---|---|
| Right-brain stroke | Left-brain stroke | ||||
| Gainotti et al., 1972 | 42% (n=114) | 31% (n=108) | Confrontation examination | Outpatient clinic | Italy |
| Denes et al., 1982 | 33% (n=24) | 21% (n=24) | Figure copying | Geriatric hospital | Italy |
| Fullerton et al., 1986 | 49% (n=88) | 25% (n=117) | Postural examination, cancellation tests, drawing | General hospital | Ireland |
| Stone et al., 1993 | 82% (n=69) | 65% (n=102) | Object pointing, reading, cancellation tests, coin selection, figure copying | General hospital | UK |
| McGlone et al., 1997 | 62% (n=71) | 31% (n=67) | Figure copying & drawing, line bisection, cancellation tests | General hospital | Canada |
| Kalra et al., 1997 | 43% (n=75) | 21% (n=70) | Confrontation examination, line bisection, cancellation tests, figure copying & drawing | General hospital | UK |
| Ringman et al., 2004 | 43% (n=356) | 20% (n=394) | Confrontation examination | Acute care hospital | USA |
| Present study | 76% (n=85) | 47% (n=36) | Kessler Foundation Neglect Assessment Process (KF-NAP) | Acute inpatient rehabilitation | USA |
| Overall | 51% (N=881) | 29% (N=918) | |||
Note: Reports were selected for their inclusion of both left and right-brain-damaged stroke survivors.
Conventional detection of spatial neglect uses visual/sensory examination or paper-and-pencil tests. One example is a cancellation task, which requires crossing out all targets (e.g., the letter “A”) embedded among non-targets (e.g., “E” and “Z”) on a piece of paper, such as the Bells Test16 or Star Cancellation.17 These assessments are widely available in the clinical setting, but create two challenges: (1) functional performance of daily activities related to spatial neglect is poorly captured, and (2) they may under-diagnose auditory, proprioceptive, or motor-intentional symptoms of spatial neglect.18 To address these deficiencies, our group developed the Kessler Foundation Neglect Assessment Process (KF-NAP™)19, 20 based upon the Catherine Bergego Scale (CBS).21, 22 The CBS comprehensively examines functional performance in personal (body surface), peri-personal (within arm's reach), and extra-personal spaces (beyond arm's reach), as well as performance in perceptual, mental imagery and motor domains. Thus, the CBS can capture the heterogeneity of spatial neglect and is more sensitive than paper-and-pencil tests19, 23 to problems in activities of daily living (ADLs).
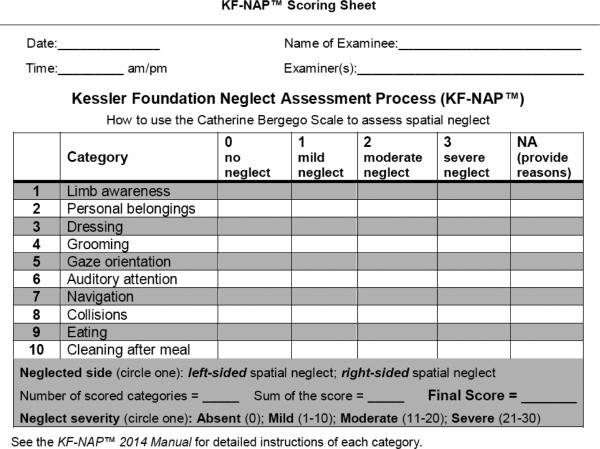
We found that additional instructions were needed for reliable CBS administration, and developed the KF-NAP, which provides detailed administration instructions and a scoring chart for the ten original CBS categories of behavior (Figure 1).19, 20 We modified some CBS category labels to better convey the purpose of an observation, to include right-sided neglect symptoms, or to shorten the wording. For example, “knowledge of left limbs” on the CBS22 is revised to “limb awareness” on the KF-NAP. The 2012 version included one page of instructions to reduce ambiguity and increase reliability.19 The KF-NAP 2014 Manual provides more detailed scoring and observation information.20 The examiner is instructed to provide the patients with verbal prompts to initiate or perform certain behavior/actions, such as “I cannot find your reading glasses. Can you tell me where they are?”, “Show me how you would put this coat on.”, “Show me how you wash your face”, “Show me how to get to the therapy gym”. Clearly, none of the prompts include spatial cues suggesting locations or directions. Even when the patient asks for item(s), the examiner must give a neutral answer. For example, if the patient asks: “Where is the coffee?” during a meal (in the observation category of “eating”) the examiner may answer: “It is on the tray. Can you find it?”
Figure 1.
Scoring chart of the Kessler Foundation Neglect Assessment Process (KF-NAP™ 2014 Scoring Chart)
Additionally, the KF-NAP specifies the environment where the observation takes place and observation of left vs. right asymmetric performance. However, rather than testing functional ability in a specific situation, the KF-NAP emphasizes direct observation of spontaneous behavior and awareness for right versus left space during ADLs. The main objective is to allow patients to spontaneously explore the environment, move their eyes/head and initiate actions. It is important that both sides of space are assessed, so that the examiner can compare performance on the right versus left before scoring. Another distinction is that all ten categories are observed during one session, which was not stressed in the original CBS. Depending on the category, patients are rated immediately during or immediately after the observation. Thus, it is based on direct observation, rather than summarized impressions from large amounts of behavior.
Standardizing an observational assessment may change its properties. We conducted the present study to demonstrate KF-NAP's psychometric properties, its clinical feasibility, and its uniqueness in measuring ADL difficulties specific to spatial neglect. We assessed stroke survivors with unilateral brain damage in an acute inpatient rehabilitation facility (IRF), using the KF-NAP and two common functional outcome measures — the Functional Independence Measure (FIM™)24 and the Barthel Index (BI).25 We had three objectives:
To determine the internal consistency and factor structure of the KF-NAP.
To examine whether the KF-NAP uniquely measures ADL deficits that the FIM or BI does not.
To evaluate the prevalence of spatial neglect and examine how the severity of spatial neglect predicts functional independence at the time of IRF discharge.
Methods
This study was approved by the Institutional Review Boards of the authors’ organizations. A consecutive sample of 121 stroke survivors (July 2012 – March 2014) met inclusion criteria, gave informed consent, and completed the first assessment within 72 hours of admission to three campuses of an IRF. Inclusion criteria were first stroke, unilateral brain damage, and adult (18 to 99 years old). Due to unexpected early discharge, 13 participants were not reassessed within 72 hours of IRF discharge. Participating patients had no previous neurological damage or psychiatric conditions.
Following a certification procedure established in 2012, two occupational therapists (OTs) per IRF campus were trained to use the KF-NAP to competency standards for observing and scoring. They screened patients’ eligibility, and scheduled and administered both assessment sessions (40-60 minutes per session), during which they measured patients’ function with the KF-NAP, FIM, and BI. OTs were instructed to assess the same patient both at admission and at discharge. However, due to busy clinical duties, it was tolerated when occasionally one OT performed the admission assessment and the other performed the discharge assessment.
Kessler Foundation Neglect Assessment Process (KF-NAP™)
The KF-NAP19, 20 consists of 10 categories: limb awareness, personal belongings, dressing, grooming, gaze orientation, auditory attention, navigation, collisions, eating, and cleaning after meal. Each is scored from 0 to 3, with higher scores indicating more severe neglect. The final score is the sum of all category scores, ranging from 0 to 30. If a category is impossible to score due to the patient's condition (e.g., not able to use a wheelchair, eating restrictions), it is not included in the final score. In this case, the final score is calculated by averaging scores in the valid categories: (sum score ÷ number of scored categories) × 10 = final score.22
Of the participants, 112 were scored in all KF-NAP categories. Five participants missed one category (3 collisions, 1 eating, and 1 auditory attention), 3 missed 2 (2 missed both eating and cleaning after meal; 1 missed both navigation and collisions), and 1 patient missed 3 (collisions, eating and cleaning after meal). Of the 108 participants completing the discharge assessment, 104 were scored in all categories: 3 missed 2 (2 missed both eating and cleaning after meal; 1 missed both navigation and collisions), and 1 missed 3 (collisions, eating and cleaning after meal). Overall, the most commonly omitted categories were, with the omission rate in parentheses (all vs. participants with KF-NAP > 0): collisions (3.1% vs. 5.3%), eating (3.1% vs. 5.3%), cleaning after meal (2.6% vs. 4.5%), navigation (.9% vs. 1.5%), and auditory attention (.4% vs. .8%).
Functional Independence Measure (FIM™)
The FIM24, 26 consists of 18 items assessing level of independence. The motor domain includes 13 items in the categories of self care, bladder and bowel management, transfers, and mobility; and the cognition domain includes 5 items in comprehension, expression, social interaction, problem solving, and memory. OTs scored each FIM item using the instructions in the Patient Assessment Instrument (IRF-PAI) Training Manual.27 Each item is scored from 1 to 7, with higher scores indicating better function. Final scores ranged from 18 to 126.
Barthel Index (BI)
The BI25, 28 consists of 10 items. The range of scores is different for each item: feeding (0,5,10), bathing (0,5), grooming (0,5), dressing (0,5,10), bowels (0,5,10), bladder (0,5,10), toilet use (0,5,10), transfers – bed to chair and back (0,5,10,15), mobility on level surfaces (0,5,10,15), and stairs (0,5,10). The total score is the sum of the 10 items and ranges from 0 to 100, with higher scores indicating better function.
Data Analyses
Because all the continuous variables were distributed in a non-normal fashion, we report medians and inter-quartile ranges (IQR). All analyses were performed with STATA/SE 12.1.
Objective 1: Reliability and factor structure of KF-NAP
We examined internal consistency with Cronbach's alpha among those with admission KF-NAP scores greater than zero (n=82). In regards to factor structure, the KF-NAP categories were based on the CBS, for which Azouvi et al. reported one underlying factor,23 but Goedert et al. found two.18 To examine the factor structure, we included patients with KF-NAP greater than zero at admission and no missing items (n=73). Following a confirmatory factor analysis in which the previously-reported one and two-factor solutions performed similarly (see Supplementary Data), we performed an exploratory factor analysis with an oblique promax rotation, because this rotation method is appropriate when latent factors are likely correlated.29, 30 We retained factors with eigenvalues (λ) greater than 1.0 that were not also produced by parallel analysis of random data structures with 50 repetitions.30, 31
Objective 2: Uniqueness of KF-NAP
Many studies choose FIM or BI as the functional outcome measure because they share similar factor structures.32 The KF-NAP may capture neglect-specific ADL performance not captured by the FIM or BI. To examine this hypothesis, we performed an exploratory factor analysis with oblique promax rotation, using all items from the KF-NAP, FIM, and BI. We reverse-coded KF-NAP so that higher scores indicate better function on all scales. We used the same factor retention principles as in Objective 1.
Objective 3: Prevalence of spatial neglect and its impact on functional outcome at IRF discharge
Some clinicians assume that spatial neglect will resolve completely during inpatient hospitalization. We calculated the percent of patients with spatial neglect at admission and discharge. Additionally, we examined whether neglect severity at admission predicted rehabilitation outcome (FIM scores) at discharge, using a linear regression analysis, controlling for age, side of stroke, admission FIM, and length of IRF stay.
Results
Of 121 participants (68 females, 53 males), the median age was 70 years, 36 participants had left brain stroke, and 85 had right brain stroke. Participants were admitted to IRF a median of 6 days post stroke. There was no significant difference in sex ratio, age, handedness, ethnicity or race between participants who had spatial neglect (KF-NAP > 0) and those who had no symptoms (Table 2).
Table 2.
Demographic and clinical information of study participants at admission
| All N=121 | No spatial neglect (KF-NAP = 0) n=39 | Spatial neglect present (KF-NAP > 0) n=82 | p value (Comparison between groups) | ||
|---|---|---|---|---|---|
| Sex | Male | 53 | 16 | 37 | .411a |
| Female | 68 | 23 | 45 | ||
| Age | Years; median | 70 | 69 | 71 | .816b |
| (IQR) | (61-81) | (58-82) | (61-80) | ||
| Handedness | Left | 12 | 4 | 8 | 1.000c |
| Right | 108 | 35 | 73 | ||
| Ambidextrous | 1 | 0 | 1 | ||
| Ethnicity | Hispanic | 11 | 6 | 5 | .096a |
| Non-Hispanic | 110 | 33 | 77 | ||
| Race | White | 78 | 20 | 58 | .090c |
| Black | 22 | 8 | 14 | ||
| Asian | 3 | 2 | 1 | ||
| Other (including those identifying “Hispanic” as race) | 17 | 8 | 9 | ||
| Unknown | 1 | 1 | 0 | ||
| Lesioned hemisphere | Left | 36 | 19 | 17 | .002a |
| Right | 85 | 20 | 65 | ||
| Time post stroke | Days; median (IQR) | 6 (4-9) | 5 (4-9) | 7 (4-9) | .458 b |
| Length of stay | Days; median (IQR) | 20 (12-25) | 13 (9-18) | 22.5 (16-27) | < .001b |
Note
Fisher's exact
U test
Freeman-Halton test
Objective 1: Reliability and Factor Structure of KF-NAP
Cronbach's alpha was .96, indicating excellent internal consistency. The factor analysis suggested a one-factor solution with an eigenvalue of 6.86 (Table 3), accounting for 94.0% of the variance. The extracted second factor had an eigenvalue of only .37, and parallel analysis produced a second factor with a greater eigenvalue (λ = .45), suggesting this second factor resulted from noise in the data.
Table 3.
Rotated factor loading pattern of the KF-NAP at admission (n = 73)
| Factor 1 (λ=6.86) | |
|---|---|
| Grooming | .77a |
| Eating | .68a |
| Dressing | .53b |
| Auditory attention | .33a |
| Cleaning after meal | .33a |
| Personal belongings | .28a |
| Limb awareness | .25b |
| Collisions | .25b |
| Gaze orientation | .07a |
| Navigation | −.02b |
Note
Items loading onto separate factors in the prior study of acute patients using the CBS,16 without the KF-NAP process.
Items loading onto separate factors in the prior study of acute patients using the CBS,16 without the KF-NAP process.
Objective 2: Uniqueness of KF-NAP
The FIM, BI, and KF-NAP were all inter-correlated (see Table 4), with all Bonferroni-corrected pairwise comparisons reaching significance. However, factor analysis revealed that the KF-NAP accounted for additional variance in patients’ performance (11.6%) not captured by the FIM or BI (Table 5). The KF-NAP items loaded onto a single factor (factor loadings greater than 0.40) that was distinct from two other factors containing subsets of FIM and BI items.
Table 4.
Pairwise Spearman correlation coefficients (ρ) among KF-NAP, Motor FIM (mFIM), Cognitive FIM (cFIM), FIM, and BI
| Admission (n=82) | Discharge (n=51) | |||||||
|---|---|---|---|---|---|---|---|---|
| KF-NAP | mFIM | cFIM | FIM | KF-NAP | mFIM | cFIM | FIM | |
| mFIM | −.61 | −.65 | ||||||
| cFIM | −.43 | .53 | −.47 | .54 | ||||
| FIM | −.62 | .96 | .72 | −.65 | .98 | .68 | ||
| BI | −.56 | .93 | .53 | .91 | −.58 | .90 | .49 | .88 |
Note: All the p values < .00001
Table 5.
Rotated factor loading pattern of the reverse-coded KF-NAP, FIM, and BI at admission (n = 73)
| Item | Factor # (λ) % of variance | 1 (λ=17.99) 55.5% | 2 (λ=3.74) 11.6% | 3 (λ=2.87) 8.9% |
|---|---|---|---|---|
| FIM Transfers: Toilet | 1.00* | .07 | −.03 | |
| FIM Transfers: Tub, Shower | .85* | .06 | −.04 | |
| FIM Toileting | .85* | −.06 | −.03 | |
| FIM Dressing-Lower Body | .79* | .17 | .15 | |
| FIM Transfers: Bed, Chair, Wheelchair | .67* | .02 | −.06 | |
| BI Toilet Use | .62* | .04 | .08 | |
| BI Transfers | .59* | .04 | .04 | |
| BI Mobility | .59* | −.03 | .02 | |
| FIM Stairs | .51* | .01 | −.03 | |
| BI Dressing | .49* | .01 | .15 | |
| FIM Bathing | .48* | −.03 | .20 | |
| FIM Walk/Wheelchair | .45* | .00 | −.01 | |
| KF-NAP Gaze orientation | .06 | .92* | −.06 | |
| KF-NAP Navigation | .01 | .90* | .08 | |
| KF-NAP Dressing | .07 | .88* | −.01 | |
| KF-NAP Personal belongings | .05 | .88* | −.03 | |
| KF-NAP Collisions | .02 | .76* | −.04 | |
| KF-NAP Grooming | .11 | .75* | .00 | |
| KF-NAP Eating | −.12 | .72* | −.05 | |
| KF-NAP limb awareness | −.04 | .56* | .03 | |
| KF-NAP Auditory attention | .04 | .54* | .01 | |
| KF-NAP Cleaning after meals | −.04 | .51* | .11 | |
| FIM Dressing-Upper Body | .40 | .02 | .67* | |
| FIM Expression | −.01 | −.03 | .14 | |
| FIM Grooming | .15 | .05 | .05 | |
| FIM Social Interaction | .02 | .03 | .04 | |
| FIM Problem Solving | .07 | .05 | .04 | |
| BI Bathing | −.04 | .03 | .02 | |
| BI Bowels | .08 | −.02 | .01 | |
| FIM Memory | −.01 | −.04 | .00 | |
| FIM Bladder Management | .14 | .02 | −.01 | |
| BI Grooming | .02 | −.08 | −.03 | |
| BI Bladder | .04 | −.02 | −.03 | |
Note
The factor loading that was the highest and with the value greater than .40 of a given item
Objective 3a: Prevalence of Spatial Neglect
At IRF admission, 67.8% of participants (n=82) showed symptoms of spatial neglect (Table 6), and their median KF-NAP score was 7 (IQR = 3-16). Among the 36 left brain-damaged participants, 17 had KF-NAP scores greater than zero, suggesting the presence of spatial neglect (median = 5, IQR = 2-7). Of the 85 right brain-damaged participants, 65 had positive KF-NAP scores (median = 8.9, IQR = 3-16). The presence of spatial neglect was more frequent after right than left brain damage (76.5% vs. 47.2%, Fisher's exact test: p = .002). However, side of stroke did not predict severity of spatial neglect (two-sample U test: p = .138).
Table 6.
Prevalence of spatial neglect.
| No neglect | Mild neglect | Moderate neglect | Severe neglect | Presence of spatial neglect | |
|---|---|---|---|---|---|
| KF-NAP score | 0 | 1 - 10 | 11 - 20 | 21 - 30 | 1 - 30 |
| Admission | |||||
| Left-brain stroke (n=36) | 19 (52.8%) | 13 | 1 | 3 | 17 (47.2%) |
| Right-brain stroke (n=85) | 20 (23.5%) | 35 | 19 | 11 | 65 (76.5%) |
| Total (N=121) | 39 (32.2%) | 48 | 20 | 14 | 82 (67.8%) |
| Discharge | |||||
| Left-brain stroke (n=34) | 25 (73.5%) | 6 | 3 | 0 | 9 (26.5%) |
| Right-brain stroke (n=74) | 32 (43.2%) | 30 | 10 | 2 | 42 (56.8%) |
| Total (N=108) | 57 (52.8%) | 36 | 13 | 2 | 51 (47.2%) |
At IRF discharge (Table 6), 47.2% of participants (n=51/108) showed symptoms of spatial neglect (KF-NAP > 0, median = 6, IQR = 3-12). Of the 34 left brain-damaged patients, 9 were discharged with symptoms of spatial neglect (median KF-NAP = 5, IQR = 3-13), as were 42 of the 74 right brain-damaged patients (median = 6, IQR = 2-11). Presence of spatial neglect remained more frequent after right than left brain damage at IRF discharge (56.8% vs. 26.5%, Fisher's exact test: p = .004), but severity of spatial neglect was again not predicted by side of stroke (p = .833).
In patients with spatial neglect at admission (n = 74), KF-NAP improved an average of .2 points per day over the hospitalization period, a rate significantly greater than zero (Kolmogorov-Smirnov test: p < .001). There was no difference in KF-NAP improvement between left and right brain-damaged participants (U test: p = .648).
Objective 3b: Clinical Impact of Spatial Neglect
Those with spatial neglect at admission (i.e., KF-NAP > 0) had lower admission FIM than those without neglect (median = 56 vs. 82; U test: p < .001). The same pattern emerged at IRF discharge (median = 88.5 vs. 112; U test: p < .001). However, patients with spatial neglect stayed almost 10 days longer in inpatient rehabilitation (Table 2). Thus, the presence of spatial neglect adversely affected rehabilitation outcomes.
We further examined whether severity, in addition to the presence, of spatial neglect impacted rehabilitation outcomes. Using a linear regression model, we found that greater neglect severity (KF-NAP score) at admission predicted lower FIM discharge scores (square-root transformed; b = −.033, SE = .015, 95% CI = [−.063, −.003], β = −.23, p = .033) after controlling for age, side of stroke, admission FIM, and length of stay. Thus, initial severity of spatial neglect predicted functional independence after inpatient rehabilitation.
Discussion
The KF-NAP provides comprehensive and clear observational methods for assessment and scoring of the CBS,19, 20 measuring patients’ symptoms of spatial neglect while performing ADLs.21, 22 In the present study, we found excellent internal consistency and a single-factor structure in the KF-NAP, consistent with one study23 but not another18 in both of which the CBS was examined without reporting a standardized assessment process. Thus, the process of the KFNAP may increase consistency among the observational categories. The majority (> 94%) of the participants were scored in all KF-NAP categories by OTs, suggesting excellent feasibility of using the assessment within the therapists’ clinical routines. Omissions in scoring occurred less than 5% of time, and were likely to involve assessment of collisions, eating, cleaning after meal, navigation, or auditory attention. Since the KF-NAP measures one single factor, occasional missing observations should not diminish its validity; we recommend, however, that clinicians observe all categories to optimize its applicability.
Importantly, we found that the KF-NAP is different from the FIM or the BI but significantly correlated with them. All these assessment tools help examine deficits during ADLs but have different emphasis. The FIM measures burden of care, and the BI measures the assistance that patients need in daily life function. The FIM and BI both measure general functions, which may be affected by spatial neglect, but they do not provide specific information on whether poor functional performance is affected by spatial neglect. The KF-NAP measures patients’ awareness of body-environment spatial relations during ADLs. Thus, the KF-NAP measures ADL performance deficits that are not captured by the FIM or BI.
Using the KF-NAP score to determine the presence of spatial neglect, we found the prevalence of the disorder to be high: 67.8% at admission and 47.2% at IRF discharge. It is not clear whether the decrease from admission to discharge is due to spontaneous stroke recovery, the effect of rehabilitation therapies, or a combination of the two. However, it is important to note that even after rehabilitation, a large proportion of patients were discharged with symptoms of spatial neglect. The present findings are consistent with reports of patients and caregivers that patients encounter difficulties with everyday tasks and community participation.33, 34 Thus, continued outpatient treatment for people with spatial neglect is desirable.
Lastly, consistent with previous research,14, 15 we found that spatial neglect and its severity predict poor rehabilitation outcomes even after prolonged IRF stay. This has important fiscal and policy implications, in that spatial neglect can seriously hamper motor and functional improvement. Early detection and timely treatment may reduce its impact.
Study Limitations
While our findings suggest the potential of using KF-NAP as part of ADL assessment in clinical settings, there are a few limitations. OTs performed all the KF-NAP, FIM, and BI assessments in this study. However, in most IRFs, the FIM is assessed by a multi-disciplinary team including OTs, physical therapists, speech and language pathologists, and nurses. It is likely that the KF-NAP can also be administered by professionals from different disciplines who receive proper training. A study examining intra-rater reliability of examiners from multiple disciplines using KF-NAP may be warranted.
Another possible limitation is selection bias. It took 21 months to enroll and assess 121 study participants in the hosting IRF system, which admits more than 1,200 stroke survivors annually. Patients with multiple strokes and bilateral brain damage were not represented in the study. OTs also recruited two times more right than left brain-damaged stroke survivors. As a result, we were not able to separately examine the KF-NAP's psychometric properties for left vs. right brain-damage, because the sample of left stroke survivors was too small. Thus, a larger-scale study better representing the stroke population, including equal numbers of right and left brain-damaged stroke survivors, is needed.
Conclusions
The KF-NAP is a clinically feasible method to observe spatial neglect systematically during activities of daily living. With excellent internal consistency and a single-factor structure, the KF-NAP can be a standard process for measuring spatial neglect using the CBS items. Using the KF-NAP as the measure of spatial neglect, we found that spatial neglect is persistent after inpatient care is completed and adversely affects rehabilitation outcome even after prolonged IRF care.
Supplementary Material
Acknowledgments
The authors thank stroke survivors for participating in the study, and the occupational therapists (Gretchen March, Sharon Holman, Courtney Silviotti, Yamiley Lemoine, Shira Schwarz, and Lindsay Comardo) for helping with participant recruitment and data collection.
Financial support: Healthcare Foundation of New Jersey (PI: Barrett), National Institutes of Health (NIH/NICHD/NCMRR, K24HD062647, PI: Barrett), and the National Institute on Disability, Independent Living and Rehabilitation Research (H133G120203, PI: Barrett).
List of Abbreviations
- ADL
Activity of daily living
- BI
Barthel Index
- CBS
Catherine Bergego Scale
- FIM
Functional Independence Measure
- IQR
Interquartile range
- IRF
Inpatient rehabilitation facility
- KF-NAP
Kessler Foundation Neglect Assessment Process
- OT
Occupational therapist
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Previous presentation of the data: Results of the present study were partially presented in the 2014 annual conference of the American Congress of Rehabilitation Medicine.
References
- 1.Gainotti G, Messerli P, Tissot R. Qualitative analysis of unilateral spatial neglect in relation to laterality of cerebral lesions. J Neurol Neurosurg Psychiatry. 1972;35(4):545–50. doi: 10.1136/jnnp.35.4.545. doi: 10.1136/jnnp.35.4.545. PubMed PMID: MEDLINE:5049813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denes G, Semenza C, Stoppa E, Lis A. Unilateral spatial neglect and recovery from hemiplegia: a follow-up study. Brain. 1982;105(Pt 3):543–52. doi: 10.1093/brain/105.3.543. doi: 10.1093/brain/105.3.543. PubMed PMID: MEDLINE:7104665. [DOI] [PubMed] [Google Scholar]
- 3.Fullerton KJ, McSherry D, Stout RW. Albert test: A neglected test of perceptual neglect. Lancet. 1986;1(8478):430–2. doi: 10.1016/s0140-6736(86)92381-0. PubMed PMID: ISI:A1986A147100013. [DOI] [PubMed] [Google Scholar]
- 4.Stone SP, Halligan PW, Greenwood RJ. The incidence of neglect phenomena and related disorders in patients with an acute right or left-hemisphere stroke. Age Ageing. 1993;22(1):46–52. doi: 10.1093/ageing/22.1.46. doi: 10.1093/ageing/22.1.46. PubMed PMID: WOS:A1993KJ97600010. [DOI] [PubMed] [Google Scholar]
- 5.McGlone J, Losier BJ, Black SE. Are there sex differences in hemispatial visual neglect after unilateral stroke? Neuropsychiatry Neuropsychol Behav Neurol. 1997;10(2):125–34. PubMed PMID: ISI:A1997WY13900008. [PubMed] [Google Scholar]
- 6.Kalra L, Perez I, Gupta S, Wittink M. The influence of visual neglect on stroke rehabilitation. Stroke. 1997;28(7):1386–91. doi: 10.1161/01.str.28.7.1386. PubMed PMID: WOS:A1997XK48200016. [DOI] [PubMed] [Google Scholar]
- 7.Ringman JM, Saver JL, Woolson RF, Clarke WR, Adams HP. Frequency, risk factors, anatomy, and course of unilateral neglect in an acute stroke cohort. Neurology. 2004;63(3):468–74. doi: 10.1212/01.wnl.0000133011.10689.ce. PubMed PMID: ISI:000223229100012. [DOI] [PubMed] [Google Scholar]
- 8.Heilman KM, Watson RT, Valenstein E. Neglect and related disorders. In: Heilman KM, Valenstein E, editors. Clinical Neuropsychology. 5th ed. Oxford University; New York: 2012. pp. 296–348. [Google Scholar]
- 9.Tromp E, Dinkla A, Mulder T. Walking through doorways: An analysis of navigation skills in patients with neglect. Neuropsychol Rehabil. 1995;5(4):319–31. PubMed PMID: ISI:A1995RX45400003. [Google Scholar]
- 10.Buxbaum LJ, Palermo MA, Mastrogiovanni D, Read MS, Rosenberg-Pitonyak E, Rizzo AA, et al. Assessment of spatial attention and neglect with a virtual wheelchair navigation task. J Clin Exp Neuropsychol. 2008;30(6):650–60. doi: 10.1080/13803390701625821. doi: 10.1080/13803390701625821. PubMed PMID: ISI:000257469300004. [DOI] [PubMed] [Google Scholar]
- 11.Akinwuntan AE, Feys H, De Weerdt W, Baten G, Arno P, Kiekens C. Prediction of driving after stroke: A prospective study. Neurorehabil Neural Repair. 2006;20(3):417–23. doi: 10.1177/1545968306287157. doi: 10.1177/1545968306287157. PubMed PMID: WOS:000239898900008. [DOI] [PubMed] [Google Scholar]
- 12.Galletta EE, Campanelli L, Maul KK, Barrett AM. Assessment of neglect dyslexia with functional reading materials. Top in Stroke Rehabil. 2014;21(1):75–86. doi: 10.1310/tsr2101-75. doi: 10.1310/tsr2101-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tham K, Kielhofner G. Impact of the social environment on occupational experience and performance among persons with unilateral neglect. Am J Occup Ther. 2003;57(4):403–12. doi: 10.5014/ajot.57.4.403. PubMed PMID: WOS:000184216600005. [DOI] [PubMed] [Google Scholar]
- 14.Wee JYM, Hopman WM. Comparing consequences of right and left unilateral neglect in a stroke rehabilitation population. Am J Phys Med Rehabil. 2008;87(11):910–20. doi: 10.1097/PHM.0b013e31818a58bd. doi: 10.1097/PHM.0b013e31818a58bd. PubMed PMID: ISI:000260340900006. [DOI] [PubMed] [Google Scholar]
- 15.Wilkinson D, Sakel M, Camp S-J, Hammond L. Patients with hemispatial neglect are more prone to limb spasticity, but this does not prolong their hospital stay. Arch Phys Med Rehabil. 2012;93:1191–5. doi: 10.1016/j.apmr.2012.01.010. doi: 10.1016/j.apmr.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Gauthier L, Dehaut F, Joanette Y. The bells test: A quantitative and qualitative test for visual neglect. J Clin Exp Neuropsychol. 1989;11(2):49–54. PubMed PMID: ISI:A1989AA11700001. [Google Scholar]
- 17.Halligan PW, Cockburn J, Wilson BA. The behavioural assessment of visual neglect. Neuropsychol Rehabil. 1991;1(1):5–32. [Google Scholar]
- 18.Goedert KM, Chen P, Botticello A, Masmela JR, Adler U, Barrett AM. Psychometric evaluation of neglect assessment reveals motor-exploratory predictor of functional disability in acute-stage spatial neglect. Arch Phys Med Rehabil. 2012;93:137–42. doi: 10.1016/j.apmr.2011.06.036. doi: 10.1016/j.apmr.2011.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen P, Hreha K, Fortis P, Goedert KM, Barrett AM. Functional assessment of spatial neglect: A review of the Catherine Bergego Scale and an introduction of the Kessler Foundation Neglect Assessment Process. Top in Stroke Rehabil. 2012;19(5):423–35. doi: 10.1310/tsr1905-423. doi: 10.1310/tsr1905-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen P, Hreha K, Pitteri M. Kessler Foundation Neglect Assessment Process: KF-NAP 2014 Manual. Kessler Foundation; West Orange, New Jersey, USA: 2014. [Google Scholar]
- 21.Bergego C, Azouvi P, Samuel C, Marchal F, Louis-Dreyfus A, Jokic C, et al. Validation d'une echelle d'evaluation fonctionnelle de l'heminegligence dance la vie quotidienne: l'echelle C.B. Annales de Readaptation et de Medecine Physique. 1995;38:183–9. [Google Scholar]
- 22.Azouvi P, Marchal F, Samuel C, Morin L, Renard C, LouisDreyfus A, et al. Functional consequences and awareness of unilateral neglect: Study of an evaluation scale. Neuropsychol Rehabil. 1996;6(2):133–50. doi: 10.1080/713755501. PubMed PMID: ISI:A1996UH13800003. [Google Scholar]
- 23.Azouvi P, Olivier S, de Montety G, Samuel C, Louis-Dreyfus A, Tesio L. Behavioral assessment of unilateral neglect: Study of the psychometric properties of the Catherine Bergego Scale. Arch Phys Med Rehabil. 2003;84(1):51–7. doi: 10.1053/apmr.2003.50062. doi: 10.1053/apmr.2003.50062. PubMed PMID: ISI:000180370100008. [DOI] [PubMed] [Google Scholar]
- 24.Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994;75(2):127–32. [PubMed] [Google Scholar]
- 25.Mahoney FI, Barthel D. Functional evaluation: The Barthel Index. Md State Med J. 1965;14:56–61. [PubMed] [Google Scholar]
- 26.Ottenbacher KJ, Hsu YW, Granger CV, Fiedler RC. The reliability of the functional independence measure: A quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–32. doi: 10.1016/s0003-9993(96)90184-7. doi: 10.1016/s0003-9993(96)90184-7. PubMed PMID: WOS:A1996VX89800002. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Medicare & Medicaid Services The Inpatient Rehabilitation Facility - Patient Assessment Instrument (IRF-PAI) Training Manual. 2012.
- 28.Duffy L, Gajree S, Langhorne P, Stott DJ, Quinn TJ. Reliability (Inter-rater Agreement) of the Barthel Index for Assessment of Stroke Survivors Systematic Review and Meta-analysis. Stroke. 2013;44(2):462–8. doi: 10.1161/STROKEAHA.112.678615. doi: 10.1161/strokeaha.112.678615. PubMed PMID: WOS:000313754800038. [DOI] [PubMed] [Google Scholar]
- 29.Schmitt TA. Current Methodological Considerations in Exploratory and Confirmatory Factor Analysis. Journal of Psychoeducational Assessment. 2011;29(4):304–21. doi: 10.1177/0734282911406653. PubMed PMID: WOS:000293797800002. [Google Scholar]
- 30.Henson RK, Roberts JK. Use of exploratory factor analysis in published research -Common errors and some comment on improved practice. Educational and Psychological Measurement. 2006;66(3):393–416. doi: 10.1177/0013164405282485. PubMed PMID: WOS:000237628100003. [Google Scholar]
- 31.Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: A tutorial on parallel analysis. Organizational Research Methods. 2004;7(2):191–205. doi: 10.1177/1094428104263675. PubMed PMID: WOS:000220465500004. [Google Scholar]
- 32.Hobart JC, Lamping DL, Freeman JA, Langdon DW, McLellan DL, Greenwood RJ, et al. Evidence-based measurement - Which disability scale for neurologic rehabilitation? Neurology. 2001;57(4):639–44. doi: 10.1212/wnl.57.4.639. PubMed PMID: WOS:000170623900012. [DOI] [PubMed] [Google Scholar]
- 33.Oh-Park M, Hung C, Chen P, Barrett AM. Severity of spatial neglect during acute inpatient rehabilitation predicts community mobility post stroke [published online ahead of print date] PM&R; 2014. [January 9, 2014]. http://www.sciencedirect.com/science/article/pii/S193414821400015X. Epub 01/09/2014. doi: 10.1016/j.pmrj.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nijboer T, van de Port I, Schepers V, Post M, Visser-Meily A. Predicting functional outcome after stroke: The influence of neglect on basic activities in daily living. Front Hum Neurosci. 2013;7(182):e00182. doi: 10.3389/fnhum.2013.00182. doi: 10.3389/fnhum.2013.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.