Abstract
Background
The question of whether to recommend amputation or salvage after IIIB and IIIC tibial fractures remains unanswered. The purpose of this study is to conduct a systematic review to derive evidence-based recommendation concerning primary amputation versus limb salvage for IIIB and IIIC open tibial fractures.
Methods
Articles from Medline, Cinahl and Embase that met pre-determined criteria were included. Outcomes of interest included: hospital stay duration, complications, rehabilitation time, quality of life, limb function, pain, and return to work data. Pooling of statistical data was performed when possible.
Results
We reviewed 1,947 articles, and 28 observational studies were included. Length of hospital stay was 56.9 days for salvage patients and 63.7 days for amputees. The most common complications after salvage attempt were osteomyelitis (17.9%), nonunion (15.5%), secondary amputation (7.3%) and flap failure (5.8%). Rehabilitation time for salvaged patients was reported as time to union (10.2 months) and time to full weight-bearing (8.1 months). Pain, quality of life and limb function outcomes were assessed differently among studies and could not be combined. Percent of patients who returned to work was 63.5% for salvage patients and 73% for amputees.
Conclusions
The current literature offers no evidence to support superior outcomes of either limb salvage or primary amputation for IIIB and IIIC tibial fractures. When outcomes are similar between two treatment strategies, economic analysis that incorporates cost and preference (utility) may define an optimal treatment strategy to guide physicians and patients.
Keywords: Systematic Review, Meta-analysis, Tibial Fractures, Amputation, Limb Salvage, Outcomes
Surgeons now have over thirty years of experience with lower extremity reconstruction for patients with Gustilo IIIB and IIIC open tibial fractures. Despite the innovations in microvascular surgery and flap reconstruction, the decision between primary amputation and attempted limb salvage continues to pose a dilemma for both patients and physicians. High levels of evidence from clinical trials comparing outcomes of these two management options do not exist. The lack of these level 1 evidence studies reflects the ethical concerns of randomizing patients to these two operative choices.
Clinical decisions must still be based on the best available evidence. Good medical decisions have two parts: first, an objective estimate of the outcomes from the available treatment options and, second, an assessment of the utility (preference) of each outcome from various perspectives, including patients, physicians, and health-policy makers. Quality of care suffers when poor decisions are made by ignoring this systematic approach.1 Conflicting data following tibial trauma make this decision difficult, however. Many articles champion limb salvage with data that indicated improved quality of life,2,3 whereas others report poor outcomes following salvage such as impaired activities of daily living.4,5
Systematic reviews are rigorously designed to perform critical appraisals of available literature.6 For this reason, medicine has been using formal systematic reviews more frequently in order to obtain objective, reproducible, up-to-date, inclusive analyses that minimize bias and random error.7 These studies are particularly useful when available literature presents differing results for a particular problem. In this study, we systematically review outcomes data for primary amputation and attempted limb salvage following Type IIIB and IIIC open tibial fractures. The goals of this project are to synthesize available data to help guide the decision-making process when faced with this type of injury and to give recommendations for future investigations.
METHODS
Search Criteria
We conducted a literature search using Medline, Cinahl and Embase to identify all citations reporting tibial fractures that were treated with amputation or flap salvage. For Medline and Cinahl, the following Boolean expression of MeSH terms were employed: “(exp Tibial Fractures/ or Leg Injuries/) and (exp Amputation/ or exp Limb Salvage/ or Reconstructive Surgical Procedures/ or exp Salvage Therapy/).” In Embase, the following Boolean expression of Emtree Subject Headings was employed: “('leg injury' OR 'leg fracture' OR 'tibia fracture'/exp) AND ('limb salvage'/exp OR 'salvage therapy'/exp OR 'amputation'/exp OR 'plastic surgery' OR 'orthopedic surgery') [embase]/lim.”
Inclusion criteria
We included the highest level of evidence available, which consisted of retrospective and prospective observational studies. We only included human studies that stratified results for type IIIB or IIIC fractures because primary amputation may be considered for these injures.
Exclusion criteria
Narrative reviews, technique articles, and case series with fewer than twenty IIIB and IIIC patients were excluded.8 We also excluded studies limited to patients less than 18 years of age or limited to patients greater than 60 years of age due to the inherently different healing potential of these groups. Duplicate articles were excluded. Multiple articles from the same medical centers were thoroughly screened to ensure that no patients were included twice in our analysis. In articles that included overlapping patient sets, only data from the original series or unique data from subsequent series were extracted (Table 1).
Table 1.
Pre-determined inclusion and exclusion criteria for literature search
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Non-English articles offer large amounts of data but are often excluded because of translation difficulty. We went to great length to ensure that relevant non-English articles were included whenever possible by employing the use of expert translators.
Data Abstraction
The data were abstracted from the included articles by one of the investigators (DS) and verified by the senior author (KCC) and the statistician (MK), both of whom have substantial expertise in systematic reviews and meta-analyses.9-15 We collected data for the following variables: study design, patient demographics, mean follow-up time, duration of hospital stay, complications, rehabilitation time, quality of life, limb function, pain, and return to work outcomes.
Analyses
Meta-analysis is a quantitative method that combines and summarizes the results from multiple studies pertaining to a particular topic.16 For lower extremity trauma, meta-analysis is not feasible because the outcomes data are not reported consistently using standardized measures. In addition, most studies contain case series with no comparison group, and comparative summary measures were not available. Because standard errors were not reported in almost all the studies, pooled estimates for continuous outcome data, such as hospital length of stay, were obtained after weighting each study by the number of fractures in each series. For proportion outcomes, such as major complication rates, pooled estimates were obtained after weighting by the inverse of the variance of the individual study estimates. Tests of heterogeneity were done for proportion outcomes using a chi-square test of heterogeneity, but for continuous outcomes, the tests were not done because the variances were generally not available for individual studies. Pooled estimates were calculated even when tests of heterogeneity were significant, indicating that outcomes may not be homogeneous across the studies. For both continuous and proportion outcomes, the 95% confidence intervals for the pooled estimates were obtained based on random-effect model based estimates. This model is more realistic than a fixed-effect model and tends to give a wider 95% confidence interval of the pooled estimates from accounting for not only the within-study variability, but also the between-study variability. We used a regression analysis extended from a random effects model to assess for trends over the year of publication, that is, to estimate the extent to which year of publication explained the variability in the outcomes.17
RESULTS
Study Retrieval and Characteristics
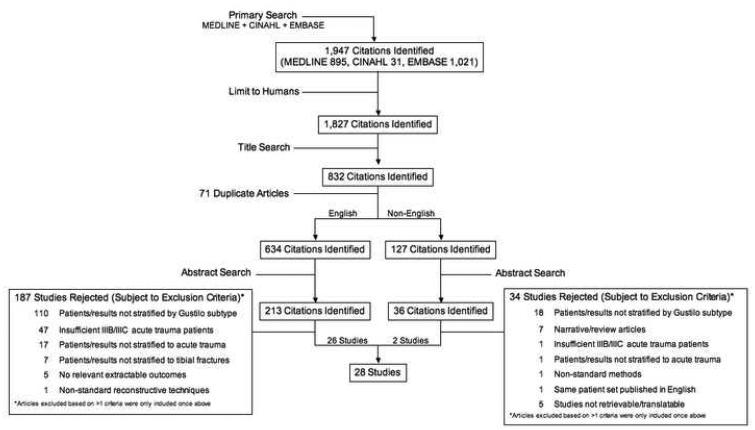
From our extensive search, 1,947 citations were identified. Of the 241 English articles selected from the title and abstract screening, 26 studies were selected on the basis of our pre-determined inclusion and exclusion criteria (Table 1). We identified 127 foreign language articles from the title screening of the original 1,947 citations. From these, 90 exclusions were made based on available translated abstracts. For the remaining 37, full articles were meticulously screened to determine if patients were stratified by Gustilo IIIB and IIIC classification. Remaining articles were then reviewed with language experts. Ultimately, we included two of these articles. A study attrition diagram of our selection process is presented in Figure 1. Of the included studies, one was prospective, 22 were retrospective, and the remaining five, though likely retrospective, did not specify the manner in which the data were collected. Eight of the 28 studies included results from both attempted limb salvage and primary amputation groups, whereas the other twenty studies reported results on patients in attempted limb salvage group only. A summary of study characteristics is included in Table 2.
Figure 1.
Study attrition diagram showing the number of references retrieved and excluded from review
Table 2.
Study and patient characteristics
| Author | Year | Country | Salvage or amputation | % Male | Mean pt age | Months of follow-up (range) |
|---|---|---|---|---|---|---|
| Arangio | 1997 | U.S.A. | Salvage | 83 | 35 | 39 (21-56) |
| Bosse | 2002 | U.S.A. | Salvage | 75 | 36 | 24 (N/A) |
| Caudle | 1987 | U.S.A. | Salvage | 86 | 36 | 71 (7-147) |
| Celikoz | 2005 | Turkey | Salvage | 100* | 22 | 25 (9-47) |
| Conroy | 2003 | U.K. | Salvage | 81 | 44 | 50 (12-96) |
| Dagum | 1999 | Canada | Both | 73 | 37 | Salvage 71 (7-147) Amputation 53 (12-82) |
| Francel | 1992 | U.S.A. | Both | 74 | 32 | 42 (N/A) |
| Georgiadis | 1993 | U.S.A. | Both | 88 | Salvage 33 Amputation 32 |
Salvage 35 (20-96) Amputation 44 (19-90) |
| Gopal | 2000 | England | Salvage | 80 | 37 | 12 minimum (or until union) |
| Gopal | 2004 | England | Salvage | 82 | 48** | 46 (15-80) |
| Graf | 1998 | Germany | Salvage | 78 | 40 | 6 (1-17) |
| Hertel | 1996 | Switzerland | Both | N/A | Salvage 22 Amputation 23 |
Salvage 83 (23-143) Amputation 83 (25-138) |
| Hertel | 1999 | Switzerland | Both | 79 | 31 | 47 (15-89) |
| Hoogendoorn | 2001 | The Netherlands |
Both | 77 | Salvage 40 Amputation 45 |
N/A |
| Keating | 2000 | Canada | Salvage | 87 | 36 | 41 (12-79) |
| Naique | 2006 | England | Salvage | 83 | 42 | 14 (8-48) |
| O'Sullivan | 1997 | Ireland | Salvage | 80 | 35 | N/A |
| Peat | 1990 | New Zealand | Salvage | N/A | 25 | Until union or amputation (~12-36) |
| Pelissier | 2003 | France | Salvage | 76 | 34 | 84 (14-180) |
| Puno | 1996 | U.S.A. | Both | 83 | 28 | 48.2 (12-116) |
| Redett | 2000 | U.S.A. | Salvage | 72 | 39 | N/A (1-84 months) |
| Robinson | 1995 | Scotland | Salvage | 76 | 41 | 38 (6-78) |
| Schandelmaier | 1997 | Germany | Salvage | 85 | 36 | 22 (12-46) for 32 of 41 pts |
| Seekamp | 1998 | Germany | Both | N/A | 38 | 4.6 |
| Trabulsy | 1994 | U.S.A. | Salvage | 69 | 27 | 16 (12-46) |
| Xu | 2006 | China | Salvage | 89 | 43 | 77 (6-12 years) |
| Yakuboff | 1990 | U.S.A. | Salvage | N/A | 28 | 26 (NA) |
| Yazar | 2006 | Taiwan | Salvage | 68 | 35 | >24 months |
Only males were included in this study as part of their selection criteria.
This is the average age of the adult group, which does not include 4 children included in their results
Patient and Injury Characteristics
All patients included in this study had IIIB or IIIC open tibial fractures resulting from acute trauma. Mean patient age ranged from 22 to 48,2,18,19 and the injuries across all reviewed articles were incurred predominantly by males (68% to 89%).20, 21 The mechanism of injury included motorcycle accidents (accounting for up to 78%),22 pedestrian accidents (up to 62%),23 and motor vehicle accidents (up to 55%).24 Other causes included industrial or agricultural accidents, falls, gunshots, domestic injuries and sports injuries.
Duration of Hospital Stay
Length of hospital stay data were available from seven studies reporting on 281 attempted limb salvage patients,2,5,21,25-28 and five studies reporting on 88 primary amputation patients.2,5,21,27,28 Limb salvage patients (12.1% of which were IIIC) had a pooled mean hospital stay of 56.9 days (range 25-129; 95% CI = 34.9, 78.9) compared to 63.7 days (range 28-101; 95% CI = 21.7, 105.8) with primary amputation patients. The length hospital stay observed in amputation patients was not statistically different from that in limb salvage patients (p = 0.97). Only one of the five amputation studies reported the percentage of IIIC fractures in the study sample (72%),2 and it is likely that extended hospital stays in the amputation group may in part be due to the larger proportion of IIIC fractures. Concomitant injuries were not discussed in all articles.
Major Clinical Complications
We defined major complications of attempted limb salvage as secondary amputation, osteomyelitis, flap failure, and nonunion (Table 3).24,25,29 Twenty-two of the included articles reported on secondary amputation rates with values ranging from 0% to 27%.29,30 The pooled secondary amputation rate was 5.1% (95% CI = 3.4, 6.9) in IIIB fractures (68 of 1,037 limbs) and 28.7% (95% CI = 11.2, 46.2) in IIIC fractures (18 of 71 limbs). The pooled rate of secondary amputation for the combined IIIB and IIIC fractures (including studies which reported results not stratified by the two fracture types) was 7.3% (105 of 1,239 limbs; 95% CI = 5.0, 9.5).4,5,8,18,20,21,23-25,28-40 Note that the test of heterogeneity was significant across individual study results for IIIB fractures (p = 0.018) as well as across individual study results for IIIC fractures (p < 0.001).
Table 3.
Synthesis of Extracted Data
| Salvaged Limbs (range), number of pts included |
Amputated Limbs (range), number of pts included |
|
|---|---|---|
| Length of Hospital Stay | ||
| Length of initial stay | 56.9 days (25-129), 281 | 63.7 days (28-101), 88 |
| Major Complications | ||
| Secondary amputation | 7.3% (0-27), 1239 | N/A |
| Osteomyelitis | 17.9% (4-56), 798 | 6% (6)*, 18 |
| Nonunion | 15.5% (0-50), 777 | N/A |
| Complete flap loss | 5.8% (0-15), 601 | N/A |
| Secondary revision | N/A | 33% (33)*, 18 |
| Other Clinical Outcomes | ||
| Superficial infection | 8% (6-13), 238 | N/A |
| Donor site morbidity | 15% (11-17), 99 | N/A |
| Rehabilitation Time | ||
| Time to union | 10.2 months (7.9-12.3), 430 | N/A |
| Time to full-weight bearing | 8.1 months (3.6-13), 176 | 6 months (6)*, 18 |
| Return to Work | ||
| Percent who returned to work | 63.5% (19-100), 432 | 73% (50-100), 59 |
| Delay until working for those who did return to work |
14.4 months (12.1-19.0), 93 | 13.6 months (10.0-15.8), 31 |
Reflects data from only 1 study
Rates of osteomyelitis in limb salvage patients were reported in 12 studies and ranged from 4% to 56%,21,32 showing heterogeneity (p < 0.001). Much of this large range is due to inconsistent diagnostic criteria for identifying osteomyelitis, which ranged from radiographic features to diagnosis based on culture results. The pooled osteomyelitis rate was 17.9% (124 of 798 reconstructed limbs; 95% CI = 12.4, 23.5).5,8,20,21,25,28,30-32,34,35,37
Complete flap loss ranged from 0%30 to 15%21 with a pooled rate of 5.8% (37 of 601 flaps; 95% CI = 2.9, 8.7) based on 9 studies. To further explore this, we analyzed the data to see if the type of flap was predictive of failure. Studies that did not state which type of flap was used were not included in this subgroup analysis. Local flaps had failure rates ranging from 0% to 10.8% with a pooled failure rate of 7.6% (6 of 64 flaps; 95% CI = 1.3, 14.0),30,32,40 and free flaps had failure rates ranging from 0% to 14.8%, with a pooled failure rate of 4.9% (21 of 413 flaps; 95% CI = 1.8, 8.0).18,20,21,24,25,30,32,35,40
Comparisons of nonunion rates with limb salvage were difficult due to inconsistent definitions and diagnostic methods. For example, one paper defined nonunion as “time to full, unprotected weight-bearing after which no further skeletal complication or reoperation occurred,”30 whereas another defined it as “motion at the site of the fracture on manual manipulation and no evidence of healing as seen on roentgenograms that were made six months after the original injury.”29 Reported values from 13 studies ranged from 0% to 50%,29,30 with a pooled rate of 15.5% (95% CI = 9.5, 21.6; 159 of 835).8,20,22-24,26,29,30,32,34,35,37,38
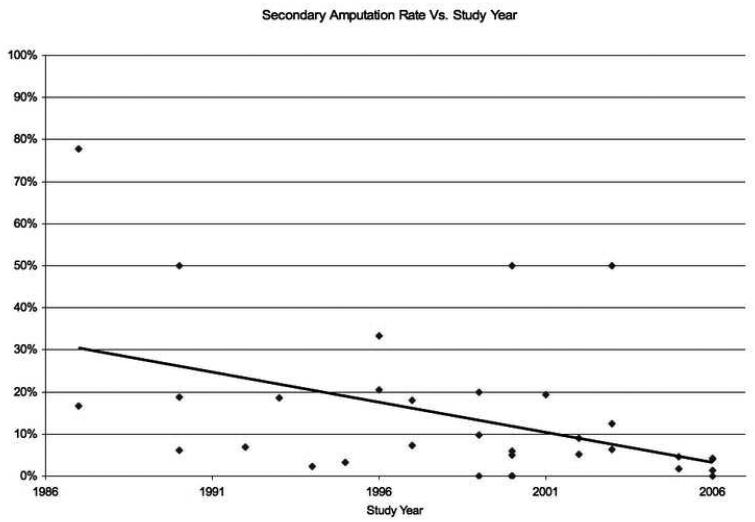
When regressed against the year of study publication, secondary amputation rate decreased significantly with time (p = 0.01, Figure 2). These are expected results because of improved operative techniques and better decision-making process in salvage attempts. No significant changes over the years in rates of osteomyelitis (p = 0.19), nonunion (p = 0.27), or complete flap loss (p = 0.29) were noted. This suggests that technique advancements in these areas have not produced tangible improvements over the time period examined.
Figure 2.
Secondary amputation rates decreased significantly with year of study (p=0.01). The two 50% outcomes at 2000 and 2003 represent small subgroups of only type IIIC patients who likely contribute to their appearance as outliers.
There was only one included study that described complications after primary amputation.21 It reported secondary revision in 6 of 18 amputated limbs and osteomyelitis in 1 of 18 amputated limbs.
Other Clinical Outcomes
Several studies reported on other complications after salvage attempts in addition to those discussed above. The most common of these include superficial infection, limb shortening and flap donor site morbidity. Unfortunately, no standardized metrics were employed in presenting these data. For example, whereas one study presents data on limb shortening greater than 20mm after reconstruction,21 another presents data only on patients with limb shortening greater than 25mm after reconstruction.34 Despite these limitations, our analyses revealed that two studies showed flap donor site morbidity in 14.7% (15 of 99 patients),21,25 and four studies showed the rate of superficial infection of the reconstructed limb in 6-13% of patients across studies, with a pooled rate of 7.9% (20 of 238 patients).8,35,39,40
Pain, Limb Function and Quality of Life Assessment
Pain was assessed by six of the included articles.2,5,21,26,28,34 Of the six studies, three did not report significant differences in pain scores between salvage and amputation groups, although all six studies noted pain in the involved limb.5,21,28 These three studies evaluated pain in different ways so it is not possible to combine the results. The fourth study found significantly increased pain in 18 primary amputees when compared to the 21 patients with limb salvage measured using visual analogue scale (p < 0.05).2 The final two studies examined only salvaged limbs.26,34
Limb function was measured with a variety of metrics including ankle range of motion, knee range of motion, walking distance and others.2,5,19,23,27,28 Two studies offered no comparison between amputation and salvage patients.19,23 A third study reported no significant difference between 9 amputees and 48 salvage patients for a composite range of motion score (no p-value reported).5 A fourth study reported significantly longer walking distance (p < 0.018) and significantly less thigh wasting (p < 0.001) for 22 salvage patients over 23 amputees.2 This study also reported no significant differences in number of hours each patient group was able to remain standing. The final study assessed limb function using the WOMAC, a validated disease-specific health outcome questionnaire used to assess lower-extremity function.28 This study reported a trend toward better physical function (p = 0.07) and less stiffness (p = 0.07) for successful salvage patients compared to primary and secondary amputees.
Assessment of quality of life was undertaken in seven of the included articles in this study.2,8,19,21,26,28,39 Three of these used the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), a self-administered questionnaire that yields two global scores – a physical component scale (PCS) and a mental component scale (MCS).19,28,39 Scores of the PCS and the MCS range from 0 (worst outcome) to 100 (best outcome) with a score 50 as the general population mean. One of these three included both salvage and amputation patients.28 No significant differences in the MCS were noted between salvage and amputation or between these groups combined as compared to the general population mean.28 Statistically significant better PCS scores were reported in 28 salvage patients than 14 patients with below-the-knee amputations (p = 0.007). The two other studies did not include an original amputee comparison group.19,39
Four other studies did not use the SF-36.2,8,21,26 As such it was impossible to directly compare their results. The first study reported quality of life based on two validated questionnaires – the Nottingham Health Profile, which measure thirteen axes of subjective health and the General Well-Being Schedule to measure psychological well-being.21 Across the thirteen axes of health from the Nottingham Health Profile, eleven showed no statistical difference between 13 limb salvage and 15 primary amputation patients. Primary amputees had significantly better outcomes than salvage patients (p < 0.05) for two axes – “recreation” and “health.” No significant differences were reported between these two groups for the General Well-Being Schedule. The second of these studies did not employ validated questionnaires and did not report any statistical results on quality-of-life measures.2 The third paper used the Fragen zur Lebenszufriedenheit™ index, a validated global life satisfaction and health index. The study reports that salvage patients have significantly lower quality of life than a control group of healthy individuals.26 The fourth paper did not employ validated questionnaires and did not include comparison between amputation and salvage groups.8
Total Rehabilitation Time
Eight studies report on time to union in salvage patients,8,20,28,30-32,34,38 and five report on time to full-weight bearing in salvage patients.21,25,30,34,39 Our analysis of the 430 salvage patients revealed a pooled mean time to union of 10.2 months (95% CI = 8.9, 11.5) with a range of 7.9 months to 12.8 months.32,34 Similarly, 176 salvage patients yielded a pooled mean of 8.1 months (95% CI = 5.6, 10.5) until full-weight bearing, with a range of 3.6 months to 13 months.21,34 These data are shown in Table 3. Rehabilitation time data for amputation patients were available only in one study with 18 patients,21 which showed a mean of 6 months before they were capable of full-weight bearing.
Return to Work
Return to work results for salvage patients varied across the eleven reporting studies.2,3,5,8,19,21,25-28,40 The data from our analysis are presented in Table 3. Combining data for the 432 salvage patients showed a pooled mean return to work rate of 63.5% (95% CI = 48.1, 78.9; range 18.8% to 100%) in patients who underwent attempted salvage. For salvage patients who did return to work, the pooled mean delay before returning to work was 14.4 months (95% CI = 9.9, 18.8; range 12.1 to 19.0 months) based on available data for 217 patients from five included studies.3,25-28 These data compare with a mean return to work rate of 73% for amputees based on a pool of 59 patients (range 50 to 100%).2,5,21,25,28 Only two studies included delay before returning to work for patients with amputation.27,28 The pooled average based on 31 patients from these two studies was 13.6 months before returning to work.
DISCUSSION
Lower extremity trauma is common. Open long bone fractures occur at a rate of 11.5 per 100,000 persons per year41 and the annual number of hospital discharges following trauma-related lower limb amputations in the United States is 3500.42 The number of lower limbs salvaged is many times greater than the number of trauma-related amputations. Because initial hospital costs are reported to be over $100,000 for each salvage attempt,21 the approach to management decisions regarding these fractures is essential.
The Lower Extremity Assessment Project (LEAP) project is the largest primary analysis of limb-threatening injuries. The project is a prospective, longitudinal, multicenter study funded by the National Institutes of Health, and it has resulted in several publications.37,43-56 We were able to include one large outcomes study from this project.37 Other LEAP publications were excluded either because they did not report on outcomes of interest for this systematic review or because results were not stratified specifically to IIIB and IIIC tibial fractures. Despite not being included, the results in the other LEAP papers for non-stratified limb-threatening injuries were compared with this paper’s results that are specific to IIIB and IIIC tibial fractures. One such study followed 460 patients with limb-threatening injuries for two years and found no significant difference in functional outcomes as measured by the Sickness Impact Profile.37 A follow-up study performed at eighty-four months reconfirmed this conclusion.51 A 2006 study reporting on return to work data at 84 months found no difference based on treatment option for 423 patients after accounting for other factors.54 That study’s overall return to work rate was 51%.
In 2007, Busse et al published a review of amputation and limb salvage.57 The analysis included a broad range of limb-threatening injuries other than just IIIB and IIIC fractures. Because this study restricted analysis to only comparative studies and excluded foreign language articles, this study ultimately examined only 9 articles with fewer than 900 distinct patients. By restricting its analysis to comparative studies only, it ignored the abundance of data that assess outcomes of salvage attempts alone.
In our systematic review, we screened over 1900 citations from three large databases, ultimately extracting data from 28 articles that collectively examined over 1300 distinct patients. Patients who undergo limb salvage versus primary amputation for IIIB and IIIC open tibial fractures are not likely to experience any difference in length of initial hospital stay. Although some studies have suggested a difference in outcomes, our analysis suggests that pain, long-term quality-of-life and limb function do not differ greatly between the patient groups. Complications following amputation are poorly characterized in the current literature, but complications of limb salvage for these fractures are quite extensive.
The present study has several limitations. As with any systematic review, our results are limited by the strength of available evidence. Because none of the available studies could ethically randomize patients, heterogeneity likely exists between the two groups in many characteristics, including patient age, gender, associated injuries, time between injury and procedure, duration of follow-up period, and presence of complications unrelated to the leg procedures. Because many included articles exclude unfavorable patients with co-morbid conditions or associated severe injuries, generalizing our results to these patient types should be considered cautiously. Lastly, because available studies did not use standardized evaluation tools and did not include full data sets for some outcomes, we were unable to perform rigorous statistical analysis. Future publications should use uniform standardized definitions of outcomes in order to allow appropriate pooling of data for meta-analysis. Despite these limitations, by including observational studies with sufficient sample sizes, our conclusions are based on the largest amount of data of the highest available evidence.
In cases when two strategies are evaluated and one is found to be clinically superior, there is no ambiguity. In cases when the results are not conclusive, a systematic review can give the best estimates of outcomes. This study evaluates all existing high level data for IIIB and IIIC tibial fractures. We have found that despite over thirty years experience and a large number of publications, there is still no clearly superior strategy for treating patients with lower limb-threatening injuries. It is unlikely that large scale outcomes studies can define the most optimal treatment strategy for IIIB and IIIC tibial injuries. Instead, decisions must be made from the standpoint of the caregiver and the patient. The pooled outcome data presented in this study can now be used to assess the cost-utility tradeoff for these decisions. We are currently undertaking a national study funded by the National Endowment of Plastic Surgery to evaluate cost and utility associated with limb salvage and amputation. Assessing the economic impact of these two strategies will provide an evidence-based approach to treating this prevalent injury by considering the overall costs of treatment and the utilities of physicians and patients in this difficult decision-making process.
Acknowledgement
We appreciate the support from the National Endowment for Plastic Surgery and a National Institute of Arthritis and Musculoskeletal and Skin Diseases Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
References
- 1.Eddy DM. Clinical decision making: from theory to practice. Anatomy of a decision. JAMA. 1990;263:441. doi: 10.1001/jama.263.3.441. [DOI] [PubMed] [Google Scholar]
- 2.Hertel R, Strebel N, Ganz R. Amputation versus reconstruction in traumatic defects of the leg: outcome and costs. J Orthop Trauma. 1996;10:223. doi: 10.1097/00005131-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Arangio GA, Lehr S, Reed JF., III Reemployment of patients with surgical salvage of open, high-energy tibial fractures: an outcome study. J. Trauma. 42:942–1997. doi: 10.1097/00005373-199705000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Yakuboff KP, Stern PJ, Neale HW. Technical successes and functional failures after free tissue transfer to the tibia. Microsurgery. 11:59–1990. doi: 10.1002/micr.1920110112. [DOI] [PubMed] [Google Scholar]
- 5.Puno RM, et al. Functional outcome of patients with salvageable limbs with grades III-B and III-C open fractures of the tibia. Microsurgery. 17:167–1996. doi: 10.1002/(SICI)1098-2752(1996)17:3<167::AID-MICR14>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 6.Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann. Intern. Med. 126:376–1997. doi: 10.7326/0003-4819-126-5-199703010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Stroup DF, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 19:283–2000. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 8.Keating JF, et al. Reamed nailing of Gustilo grade-IIIB tibial fractures. J. Bone Joint Surg. Br. 82:1113–2000. doi: 10.1302/0301-620x.82b8.10566. [DOI] [PubMed] [Google Scholar]
- 9.Kotsis SV, Chung KCA. systematic review of the outcomes of digital sympathectomy for treatment of chronic digital ischemia. J. Rheumatol. 30:1788–2003. [PubMed] [Google Scholar]
- 10.Watt AJ, Kotsis SV, Chung KC. Risk of melanoma arising in large congenital melanocytic nevi: a systematic review. Plast. Reconstr. Surg. 113:1968–2004. doi: 10.1097/01.prs.0000122209.10277.2a. [DOI] [PubMed] [Google Scholar]
- 11.Margaliot Z, Haase SC, Kotsis SV, Kim HM, Chung KC. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J. Hand Surg. [Am.] 30:1185–2005. doi: 10.1016/j.jhsa.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Margaliot Z, Chung KC. Systematic reviews: a primer for plastic surgery research, Plast. Reconstr. Surg. 120:1834–2007. doi: 10.1097/01.prs.0000295984.24890.2f. [DOI] [PubMed] [Google Scholar]
- 13.Sears ED, Burns PB, Chung KC. The outcomes of outcomes studies in plastic surgery: A systematic review of 17 years of plastic surgery and research. Plast. Reconstr. Surg. 120:2059–2007. doi: 10.1097/01.prs.0000287385.91868.33. [DOI] [PubMed] [Google Scholar]
- 14.Cavaliere CM, Chung KC. A systematic review of arthroplasty versus arthrodesis for rheumatoid wrist. Plast. Reconstr. Surg. In press. [Google Scholar]
- 15.Squitieri L, Chung KC. A systematic review of outcomes and complications of vascularized joint transfer, silicone arthroplasty and pyrocarbon arthroplasty for post-traumatic joint reconstruction of the finger. Plast. Reconstr. Surg. doi: 10.1097/PRS.0b013e31816aa0b3. In press. [DOI] [PubMed] [Google Scholar]
- 16.Cook DJ, Sackett DL, Spitzer WO. Methodologic guidelines for systematic reviews of randomized control trials in health care from the Potsdam Consultation on Meta-Analysis. J. Clin. Epidemiol. 48:167–1995. doi: 10.1016/0895-4356(94)00172-m. [DOI] [PubMed] [Google Scholar]
- 17.Hedges LV, Olgin I. Statistical Methods for Meta-Analysis. Academic Press, Inc.; 1985. [Google Scholar]
- 18.Celikoz B, et al. Subacute reconstruction of lower leg and foot defects due to high velocity-high energy injuries caused by gunshots, missiles, and land mines. Burns. 2005;31:99. doi: 10.1002/micr.20049. [DOI] [PubMed] [Google Scholar]
- 19.Gopal S, Giannoudis PV, Murray A, Matthews SJ, Smith RM. The functional outcome of severe, open tibial fractures managed with early fixation and flap coverage. J. Bone Joint Surg. Br. 86:861–2004. doi: 10.1302/0301-620x.86b6.13400. [DOI] [PubMed] [Google Scholar]
- 20.Yazar S, Lin CH, Lin YT, Ulusal AE, Wei FC. Outcome comparison between free muscle and free fasciocutaneous flaps for reconstruction of distal third and ankle traumatic open tibial fractures. Plast. Reconstr. Surg. 117:2468–2006. doi: 10.1097/01.prs.0000224304.56885.c2. [DOI] [PubMed] [Google Scholar]
- 21.Georgiadis GM, Behrens FF, Joyce MJ, Earle AS, Simmons AL. Open tibial fractures with severe soft-tissue loss. Limb salvage compared with below-the-knee amputation. J. Bone Joint Surg. Am. 75:1431–1993. doi: 10.2106/00004623-199310000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Xu YQ, et al. Repair and reconstruction of severe leg injuries: retrospective review of eighty-five patients. Chin. J. Traumatol. 9:131–2006. [PubMed] [Google Scholar]
- 23.Robinson CM, McLauchlan G, Christie J, McQueen MM, Court-Brown CM. Tibial fractures with bone loss treated by primary reamed intramedullary nailing. J. Bone Joint Surg. Br. 77:906–1995. [PubMed] [Google Scholar]
- 24.Redett RJ, Robertson BC, Chang B, Girotto J, Vaughan T. Limb salvage of lower-extremity wounds using free gracilis muscle reconstruction. Plast. Reconstr. Surg. 106:1507–2000. doi: 10.1097/00006534-200012000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Francel TJ, Vander Kolk CA, Hoopes JE, Manson PN, Yaremchuk MJ. Microvascular soft-tissue transplantation for reconstruction of acute open tibial fractures: timing of coverage and long-term functional results. Plast. Reconstr. Surg. 89:478–1992. [PubMed] [Google Scholar]
- 26.Graf PF, Wiendl M, Maurer J, Oedekoven G, Herschbach P, Henrich G. [Quality of life after complex tibial reconstruction] Unfallchirurg. 1998;101:838. doi: 10.1007/s001130050348. [DOI] [PubMed] [Google Scholar]
- 27.Seekamp A, Regel G, Ruffert S, Ziegler M, Tscherne H. [Amputation or reconstruction of IIIB and IIIC open tibial fracture. Decision criteria in the acute phase and late functional outcome] Unfallchirurg. 101:360–1998. doi: 10.1007/s001130050281. [DOI] [PubMed] [Google Scholar]
- 28.Dagum AB, Best AK, Schemitsch EH, Mahoney JL, Mahomed MN, Blight KR. Salvage after severe lower-extremity trauma: are the outcomes worth the means? Plast. Reconstr. Surg. 103:1212–1999. doi: 10.1097/00006534-199904040-00017. [DOI] [PubMed] [Google Scholar]
- 29.Caudle RJ, Stern PJ. Severe open fractures of the tibia. J. Bone Joint Surg. Am. 69:801–1987. [PubMed] [Google Scholar]
- 30.Hertel R, Lambert SM, Muller S, Ballmer FT, Ganz R. On the timing of soft-tissue reconstruction for open fractures of the lower leg. Arch. Orthop. Trauma Surg. 119:7–1999. doi: 10.1007/s004020050346. [DOI] [PubMed] [Google Scholar]
- 31.Peat BG, Liggins DF. Microvascular soft tissue reconstruction for acute tibial fractures - late complications and the role of bone grafting. Ann. Plast. Surg. 24:517–1990. doi: 10.1097/00000637-199006000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Trabulsy PP, Kerley SM, Hoffman WY. A prospective study of early soft tissue coverage of grade IIIB tibial fractures. J. Trauma. 36:661–1994. doi: 10.1097/00005373-199405000-00011. [DOI] [PubMed] [Google Scholar]
- 33.O’Sullivan ST, O’Sullivan M, Pasha N, O’Shaughnessy M, O’Connor TPF. Is it possible to predict limb viability in complex Gustilo IIIB and IIIC tibial fractures? A comparison of two predictive indices. Injury. 28:639–1997. doi: 10.1016/s0020-1383(97)00134-4. [DOI] [PubMed] [Google Scholar]
- 34.Schandelmaier P, Krettek C, Rudolf, Kohl J, Katz A, Tscherne H. Superior results of tibial rodding versus external fixation in grade 3B fractures. 342:164–1997. B.E. [PubMed] [Google Scholar]
- 35.Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J. Bone Joint Surg. Br. 2000;82:959. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 36.Hoogendoorn JM, Van der Werken C. Grade III open tibial fractures: functional outcome and quality of life in amputees versus patients with successful reconstruction. Injury. 32:329–2001. doi: 10.1016/s0020-1383(00)00250-3. [DOI] [PubMed] [Google Scholar]
- 37.Bosse MJ, et al. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N. Engl. J. Med. 2002;347:1924. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 38.Pelissier P, Boireau P, Martin D, Baudet J. Bone reconstruction of the lower extremity: complications and outcomes. Plast. Reconstr. Surg. 2003;111:2223. doi: 10.1097/01.PRS.0000060116.21049.53. [DOI] [PubMed] [Google Scholar]
- 39.Conroy J, Agarwal M, Giannoudis PV, Matthews SJ. Early internal fixation and soft tissue cover of severe open tibial pilon fractures. Int. Orthop. 2003;27:343. doi: 10.1007/s00264-003-0486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J. Bone Joint Surg. Br. 2006;88:351. doi: 10.1302/0301-620X.88B3.17120. [DOI] [PubMed] [Google Scholar]
- 41.Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29:529. doi: 10.1016/s0020-1383(98)00125-9. [DOI] [PubMed] [Google Scholar]
- 42.Pierce RO, Jr., Kernek CB, Ambrose TA. The plight of the traumatic amputee. Orthopedics. (2nd) 1993;16:793. doi: 10.3928/0147-7447-19930701-08. [DOI] [PubMed] [Google Scholar]
- 43.Pollak AN, McCarthy ML, Burgess AR. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) Study Group. J. Bone Joint Surg. Am. 2000;82-A:1681. [PubMed] [Google Scholar]
- 44.Bosse MJ, et al. A prospective evaluation of the clinical utility of the lower-extremity injury-severity scores. J. Bone Joint Surg. Am. 2001;83-A:3. doi: 10.2106/00004623-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 45.MacKenzie EJ, et al. Factors influencing the decision to amputate or reconstruct after high-energy lower extremity trauma. J. Trauma. 52:641–2002. doi: 10.1097/00005373-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 46.McCarthy ML, et al. Psychological distress associated with severe lower-limb injury . Bone Joint Surg. Am. 2003;85-A:1689. doi: 10.2106/00004623-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 47.MacKenzie EJ, et al. Functional outcomes following trauma-related lower-extremity amputation. J. Bone Joint Surg. Am. 2004;86-A:1636. doi: 10.2106/00004623-200408000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Bosse MJ, et al. The insensate foot following severe lower extremity trauma: an indication for amputation? J. Bone Joint Surg. Am. 2005;87:2601. doi: 10.2106/JBJS.C.00671. [DOI] [PubMed] [Google Scholar]
- 49.Castillo RC, et al. Use and perceived need of physical therapy following severe lower-extremity trauma. Arch. Phys. Med. Rehabil. 2005;86:1722. doi: 10.1016/j.apmr.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 50.Castillo RC, et al. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J. Orthop. Trauma. 2005;19:151. doi: 10.1097/00005131-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 51.MacKenzie EJ, et al. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J. Bone Joint Surg. Am. 2005;87:1801. doi: 10.2106/JBJS.E.00032. [DOI] [PubMed] [Google Scholar]
- 52.Smith JJ, et al. Functional outcome of bilateral limb threatening: lower extremity injuries at two years postinjury. J. Orthop Trauma. 2005;19:249. doi: 10.1097/01.bot.0000151813.10046.e4. [DOI] [PubMed] [Google Scholar]
- 53.MacKenzie EJ, Bosse MJ. Factors Influencing Outcome Following Limb-Threatening Lower Limb Trauma: Lessons Learned From the Lower Extremity Assessment Project (LEAP) J. Am. Acad. Orthop. Surg. 2006;14:S205. doi: 10.5435/00124635-200600001-00044. [DOI] [PubMed] [Google Scholar]
- 54.MacKenzie EJ, et al. Early predictors of long-term work disability after major limb trauma. J. Trauma. 2006;61:688. doi: 10.1097/01.ta.0000195985.56153.68. [DOI] [PubMed] [Google Scholar]
- 55.Archer KR, et al. Physical disability after severe lower-extremity injury. Arch. Phys. Med. Rehabil. 2006;87:1153. doi: 10.1016/j.apmr.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 56.Castillo RC, et al. Prevalence of chronic pain seven years following limb threatening lower extremity trauma. Pain. 2006;124:321. doi: 10.1016/j.pain.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 57.Busse JW, Jacobs CL, Swiontkowski MF, Bosse MJ, Bhandari M. Complex limb salvage or early amputation for severe lower-limb injury: a meta-analysis of observational studies. J. Orthop. Trauma. 2007;21:70. doi: 10.1097/BOT.0b013e31802cbc43. [DOI] [PubMed] [Google Scholar]