Abstract
The ‘behavioural immune system’ is composed of mechanisms that evolved as a means of facilitating behaviours that minimized infection risk and enhanced fitness. Recent empirical research on human populations suggests that these mechanisms have unique consequences for many aspects of human sociality—including sexual attitudes, gregariousness, xenophobia, conformity to majority opinion and conservative sociopolitical attitudes. Throughout much of human evolutionary history, these consequences may have had beneficial health implications; but health implications in modern human societies remain unclear. This article summarizes pertinent ways in which modern human societies are similar to and different from the ecologies within which the behavioural immune system evolved. By attending to these similarities and differences, we identify a set of plausible implications—both positive and negative—that the behavioural immune system may have on health outcomes in contemporary human contexts. We discuss both individual-level infection risk and population-level epidemiological outcomes. We also discuss a variety of additional implications, including compliance with public health policies, the adoption of novel therapeutic interventions and actual immunological functioning. Research on the behavioural immune system, and its implications in contemporary human societies, can provide unique insights into relationships between fitness, sociality and health.
Keywords: behavioural immune system, infection, sociality, conformity, xenophobia, health
1. Introduction
For many millions of years, parasites—and the infectious diseases that they cause—have imposed substantial selection pressures on populations from which contemporary humans are descended. As a consequence, sophisticated defences against infection evolved. The most obvious adaptations of this sort are immunological mechanisms that promote resistance to infection (e.g. the mechanisms that define humans' innate and adaptive immune systems). Less obvious perhaps are strategies of behavioural defence against infection.
There exist many behavioural strategies of anti-parasite defence, observed across a wide range of species ([1–6]; see also Meunier [7]). These strategies include specific behavioural tendencies that are stimulated by existing infections and that help to promote recovery from those infections (e.g. inhibition of motor activity, ingestion of medicinal plants [8–10]). In addition, many animals also engage in prophylactic behaviours that minimize the risk of infection in the first place. Some of these behaviours might be considered reactive, in the sense that they are avoidant responses to infectious entities in the immediate perceptual environment—such as when social insects abandon a nest after a parasite outbreak, bullfrog tadpoles avoid swimming near other tadpoles infected with intestinal parasites and chimpanzees avoid touching fellow chimpanzees stricken by polio [2,11,12]. Other behavioural strategies are more proactive. Even under conditions in which there is no perceptual evidence of infectious agents in the immediate environment, organisms may engage in behaviours that proactively manage a latent infection risk, thereby reducing the likelihood that this latent risk becomes manifest in ways that would require reactive avoidance. Examples include ants' use of antibiotic resins to line their nests [13] and, as we discuss in greater detail below, humans' efforts to maintain existing cultural norms [14]. Collectively, these strategies have been likened to a kind of ‘social immune system’ [2] or ‘behavioural immune system’ [5,15,16].
We focus here on human behaviour. Within the psychological sciences especially, there has been a recent surge of research on prophylactic behavioural defences against infectious diseases. This burgeoning body of research has yielded novel insights not only about human behavioural decision-making but also about affective and cognitive phenomena (e.g. the experience of disgust [17–19]) that facilitate or inhibit specific behavioural responses. We limit our focus to implications pertaining directly to human sociality—attitudes and behavioural tendencies that govern a person's responses to and interactions with other people—and on the further implications that these attitudes may have for health outcomes in contemporary human populations.
In exploring these implications, we focus on two conceptually related but distinct behavioural strategies that reflect the underlying workings of the ‘behavioural immune system’ in human populations. One strategy (avoidance of social interactions that pose a potential infection risk) is primarily a form of reactive avoidance, while the other strategy (conformity and maintenance of cultural norms) is more proactive in nature [20]. Both strategies have been linked empirically to a broad range of specific attitudinal outcomes within the domain of human sociality. These diverse social outcomes have a wide range of further implications for human health—some of which are subtle and non-obvious, and most of which have yet to receive rigorous empirical attention.
This article is organized as follows: we first describe each of these two strategies in turn. In doing so, we summarize key pieces of empirical evidence documenting specific implications that these strategies have for individuals' social attitudes. We then turn our attention to the identification of plausible hypotheses regarding further implications that these social attitudes may have for human health outcomes in the modern world. Some of these implications are likely to be positive, others less so. We draw special attention to social attitudes that are likely to have had positive effects on health (and fitness) outcomes throughout much of human evolutionary history but which, ironically, may have negative implications for health outcomes in many modern human societies.
2. Avoidance of social interactions that pose a potential infection risk
One way to avoid infection is to avoid contact with organisms that infect. This may seem straightforward, yet many parasites are so small as to be imperceptible. Consequently, to avoid contact with them, their presence must be inferred indirectly, often on the basis of perceptual cues signalling the consequences that parasite infestation has for other entities (e.g. the distinctive odour of organic matter being devoured by bacteria, or the symptomatic appearance of a conspecific that is already infected). Like many other animals, people are sensitive to indirect perceptual cues of parasite presence, and strategically avoid contact with objects or people characterized by these cues [21–23].
(a). Implications for appearance-based prejudices, xenophobia, sexual attitudes and gregariousness
Although perceptual cues may be probabilistically predictive of the presence of parasites, even diagnostic cues are potentially fallible. For example, facial blemishes are common symptoms of infection; nevertheless, some healthy people have blemishes while some sick people do not. Perceivers are therefore likely to make occasional errors in their behavioural decisions—either false-positive errors (responding avoidantly to things that pose no actual infection risk) or false-negative errors (failing to avoid things that actually do pose an infection risk). Throughout much of human evolutionary history, it is likely that the fitness costs associated with false-negative errors were, on average, higher than the fitness costs of false-positive errors. In accordance with the ‘smoke detector principle’ of adaptive error-management [24,25], it is likely that appraisal mechanisms evolved to systematically limit the likelihood of the more costly false-negative errors—with the inevitable consequence that people make many false-positive errors instead. Consequently, people respond avoidantly not only to entities that do pose an infection risk but also to objectively non-infectious entities that simply share superficial similarities to infectious things [22]. In the social domain, this over-generalization bias contributes to prejudicial attitudes toward people whose physical appearances superficially mimic symptoms of infection, or who just appear anomalous in some way (e.g. individuals who are disfigured, disabled or obese [23,26]).
In addition to superficial perceptual cues, people also employ other kinds of information—including group stereotypes and other acquired beliefs—to identify categories of people who might pose a potential infection risk, so as to selectively avoid contact with those people. For instance, subjectively ‘foreign’ peoples tend to be stereotypically associated with a variety of dangers, and one of those dangers is the threat of infection [27]. There are several reasons why this is so, including a perceived link between exotic peoples and exotic parasites, and the greater potential for outsiders to violate local behavioural norms that serve as buffers against parasite transmission (a topic we explore more fully in the following section, below). Consequently, the strategic avoidance of potentially infectious conspecifics may sometimes manifest in xenophobia [26].
The avoidance strategy may manifest not only in avoidant attitudes toward specific categories of people who are perceived to pose an infection risk but also in more avoidant attitudes toward specific kinds of social interactions that are perceived to increase one's vulnerability to infection. For example, because sexual promiscuity is associated with increased risk of contracting sexually transmitted diseases [28], the avoidance strategy may have inhibitory implications for individuals' attitudes toward sexual promiscuity. A cost/benefit analysis suggests that these inhibitory implications are likely to occur especially among women—because the reproductive benefits of promiscuity are generally lower among women than men, and because many sexually transmitted diseases impose greater costs on female fertility than on male fertility [29].
Interpersonal interactions need not be sexually intimate in order to increase the risk of disease transmission. Many infectious diseases can be transmitted in the course of casual interpersonal interaction, with the consequence that individuals who interact socially with greater numbers of other people are more vulnerable to infection. Therefore, the avoidance strategy may manifest in a reduced dispositional tendency toward gregariousness.
(b). Context-contingent responses
Importantly, however, while these behavioural manifestations of avoidance may have had the specific benefit of reducing the risk of infection, they may have been substantially costly in other ways (especially in group-living primate species). Among humans and other big-brained animals, these kinds of cost/benefit problems have been largely solved by the evolution of behavioural flexibility [30]. Thus, in humans, the avoidance strategy is characterized not only by mechanisms that facilitate the avoidance of interactions that pose a potential infection risk, but also by additional mechanisms that modulate these avoidant responses in a context-contingent manner. People are sensitive to contextual cues providing information about the potential benefits and potential costs of behavioural avoidance, and the psychological mechanisms underlying the avoidance strategy are activated or inhibited accordingly. The potential benefits of behavioural avoidance are most likely to accrue (and to outweigh the potential costs) under conditions in which individuals are most vulnerable to infection. Therefore, under conditions in which available information implies that an individual is relatively invulnerable to infection, avoidant responses are likely to be relatively muted; but, under conditions in which individuals are—or merely perceive themselves to be—more vulnerable to potential infection, they are likely to exhibit more strongly avoidant attitudes to entities and actions that appear to pose some infection risk.
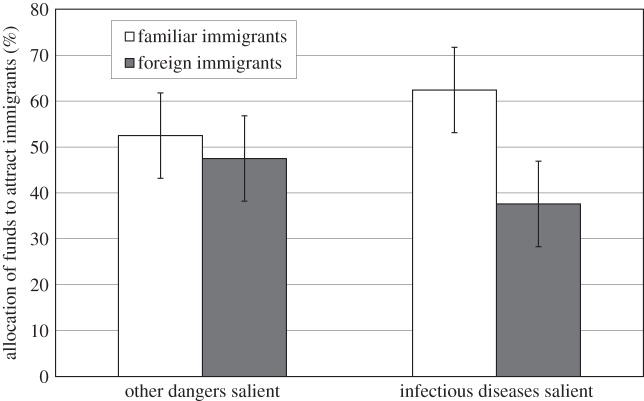
This general principle of context-contingent flexibility has important—and empirically-documented—implications for xenophobia, sexual attitudes and gregarious dispositions more generally. For example, although there may be a general human tendency toward xenophobia, this tendency manifests especially strongly under conditions in which people perceive that they are more vulnerable to infection [31–33]. In one illustrative experiment [31], participants completed a measure assessing xenophobic attitudes toward foreign peoples shortly after watching one of two brief slide shows—one that made salient the threat posed specifically by infectious diseases, and another (in a control condition) that made salient other kinds of life-threatening dangers. Results showed that, compared with the control condition, when the threat posed by infectious diseases was salient people expressed especially xenophobic attitudes (figure 1).
Figure 1.
Results from an experiment testing the effect that the psychological salience of infectious diseases has on xenophobia [31]. Canadian participants first watched a brief slide show. In one experimental condition, the content of the slide show made salient the threat posed specifically by infectious diseases; in a control condition, the slide show made salient other life-threatening dangers (e.g. electrocution). After the slide show, participants indicated preferences for the allocation of government funds to recruit immigrants from various countries, some of which were subjectively familiar (e.g. Poland, Taiwan) and some that were subjectively foreign (e.g. Mongolia, Peru). Xenophobia is indicated by a relative preference to recruit familiar immigrants rather than foreign immigrants. Results revealed that when the threat posed by infectious diseases was temporarily salient, people exhibited more strongly xenophobic attitudes.
Similar findings have been found in experiments assessing sexual attitudes and sexual behaviour. One study [34] revealed that when the threat posed by infectious diseases was made temporarily salient (compared with a condition in which other threats were salient), women consequently endorsed more restricted attitudes regarding sexual behaviour (e.g. preferring relatively fewer lifetime sexual partners). Another study showed that after being exposed to an incidental disgust-eliciting olfactory cue, both men and women reported stronger intentions to use condoms during sexual intercourse [35].
This context-contingent flexibility is also found in dispositional tendencies toward gregariousness in general. Following experimental manipulations designed to make the threat of infectious disease temporarily salient, people report lower levels of extraversion and also exhibit more avoidant motor responses toward other people [36].
In addition to the results of laboratory experiments documenting the causal influence of infection-connoting contexts on temporary changes in individuals' attitudes and actions, conceptually analogous correlations have been found in cross-national comparisons. Compared with people living in countries that historically have had relatively low levels of disease-causing parasites, people living in countries with historically higher levels of parasite prevalence report more restricted sexual attitudes, lower levels of extraversion, and more xenophobic responses to ethnic out-groups [37–39].
3. Infectious disease, conformity and maintenance of cultural norms
Until the advent of germ theory and other scientific advances in the nineteenth and twentieth centuries, the causes of infectious diseases were deeply mysterious [40,41]. And until the development of modern biomedical interventions and public health practices, the prevention of infection depended substantially on superstitious adherence to local rituals and other cultural norms. Research in medical anthropology suggests that, in pre-industrial human societies, ‘most conventions pertaining to subsistence and social behaviour operate as prescriptions to avoid illness’ [42, p. 36].
(a). Implications for conformist attitudes
If indeed local cultural norms have historically provided buffers against the transmission of infectious diseases, then any violation of these norms is likely to have increased individuals' risk of infection. Individuals' capacity to learn local norms, and their capacity to conform their own behaviour to normative standards, are likely to have served as important means of limiting infection risk. Importantly, infection risk would have been affected not only by an individual's own conformist tendencies but also by the conformist tendencies of other individuals within the local social group. Consequently, attitudinal tendencies to reward conformity behaviour in others—and to respond harshly to non-conformists—would also have helped to protect against the latent risk of infection.
The infection-reducing benefits of these conformist attitudes may be realized most strongly in behavioural domains that have the most direct implications for exposure to parasites (e.g. food preparation, personal hygiene, mating). Therefore, as a means of preventing infection, one might expect people to be especially inclined to conform—and to encourage others to conform—in those domains. But this behavioural strategy is unlikely to be limited to just those domains. Given the adaptive tendency for risk-avoidant responses to over-generalize [24,25], conformist attitudes in any domain may, to some extent, reflect an underlying motive to avoid infection.
(b). Context-contingent responses
Although conformity (by self or others) may have been beneficial as a means of reducing the spread of infectious diseases in pre-industrial societies, it may also have been associated with costs as well. Consequently, just as the avoidance strategy is engaged in a flexible, context-contingent manner, so too is the conformity strategy. Under conditions in which available information implies that an individual is relatively invulnerable to infection, conformist attitudes are likely to be relatively muted; but under conditions in which individuals are—or merely perceive themselves to be—more vulnerable to potential infection, they are likely to show a stronger tendency to conform to local norms, and also to more strongly encourage others to conform.
Much empirical research reveals that people exhibit more conformist attitudes under conditions in which they perceive that they are more vulnerable to infection. The most obvious manifestation emerges on individuals' own tendency toward behavioural conformity: when people perceive that they are more vulnerable to infection, they more readily conform to local norms [14,43]. In one illustrative experiment [14], participants were exposed to an experimental manipulation that made salient their vulnerability either to infectious diseases, or to other dangers, or to no dangers at all. Shortly thereafter they completed a measure assessing conformity to majority opinion. Results showed that, compared with the control conditions (including the condition in which other dangers were salient), people were especially likely to conform when the threat posed by infectious diseases was especially salient (figure 2). Thus, while other threats may also facilitate conformity [44], the perceived threat of infection appears to have an especially potent effect in promoting conformity behaviour.
Figure 2.
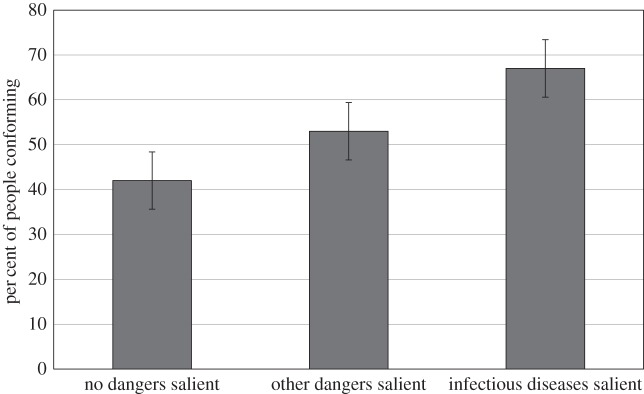
Results from an experiment testing the effect that the psychological salience of infectious diseases has on conformity to majority opinion [14]. Participants first engaged in a recall task in which they recalled and described events from their own lives. In one condition, they recalled events that made them feel vulnerable to infectious diseases; in another condition, they recalled events that made them feel vulnerable to other dangers; in a third condition they recalled non-threating events. Afterwards, they engaged in a behavioural decision-making task that assessed conformity to majority opinion. Results revealed that when their vulnerability to infectious diseases was temporarily salient, an especially high percentage of people conformed to majority opinion.
Conceptually similar effects have been found on general dispositions and attitudes. Under conditions in which people perceive that they are more vulnerable to infection, they are less open to new experiences and new ideas, they more strongly support conformist actions by others, they express greater dislike for non-conformists, and they make harsher moral judgements about people who violate social norms [14,36,45]. There are implications also for conservative political attitudes, which are characterized by attitudinal defence of cultural traditions. When people experience disgust, or in some other way are led to perceive that they are more vulnerable to infection, they express more conservative political attitudes [46]. In one experiment [47], people entering a public building were recruited to complete a brief questionnaire assessing political attitudes. They were randomly assigned to do so in one of two different locations. In one condition (a control condition) they were asked to ‘step over to the wall to complete the questionnaire’, and they proceeded to report their political attitudes in a location that offered no apparent reminders of infectious diseases. In the other condition, they were asked to ‘step over to the hand-sanitizer dispenser to complete the questionnaire’, and proceeded to report their political attitudes while standing next to an anti-bacterial hand-sanitizer dispenser—a perceptual reminder of the threat posed by bacterial infections. In the latter condition (compared with the control condition), people endorsed more conservative political attitudes.
These effects of perceived vulnerability on conformist attitudes are complemented by conceptually analogous correlations observed in cross-national comparisons. In countries that have historically had higher levels of parasite prevalence, people show greater tendencies toward behavioural conformity, impose stronger conformity pressures on others, more strongly endorse moral values pertaining to group loyalty and purity, and also more strongly endorse collectivistic values [48–50]. These outcomes manifest not only in the attitudes and actions of individuals but also are institutionalized in the form of more authoritarian government policies [51,52].
4. These social attitudes may have positive health implications in modern societies
The empirical research summarized above reveals that the avoidance strategy and the conformity strategy both have important consequences for social attitudes and behaviour. Although conceptually distinct, these various consequences are likely to have had functionally beneficial implications for health outcomes (and for fitness) within ancestral populations characterized by substantial burdens of infectious diseases. It remains unclear, however, whether these same behavioural consequences have positive implications for health outcomes in modern human societies.
(a). Evidence bearing on individual health outcomes
With one exception, there is a rather limited body of empirical research addressing the effects that avoidant and conformist social attitudes have on contemporary human health outcomes. Sexual behaviour is the one relevant domain of behaviour that has attracted sustained research attention. Evidence reveals that individuals who are more inclined to use condoms and who have more restricted (e.g. less promiscuous) attitudes towards mating are less likely to contract sexually transmitted diseases and, consequently, may be less likely to develop additional health problems too [53–55]. Outside of the sexual domain, scant evidence exists that these behavioural strategies have beneficial effects for individuals' health outcomes in contemporary human societies. One recent study [56] found no evidence that incidence of illness was predicted by sensitivity to disgust (the emotional experience associated with behavioural avoidance of infectious things). A few additional studies have focused more directly on avoidant social attitudes and provide some preliminary evidence that these attitudes may be associated with beneficial health outcomes. One study found that people who reported engaging in more parasite-avoidant behaviour (including unwillingness to have contact with potentially infectious people) also reported being in generally better health [57]. There is also some evidence that people who are less gregarious also report better health outcomes, including reduced incidence of infectious diseases; but these effects are modest in size and are qualified by other variables [58,59]. To our knowledge, there is no compelling evidence linking psychological phenomena such as xenophobia, conformity or political conservatism to reduced rates of infection.
The paucity of directly relevant empirical evidence is perhaps unsurprising, given that it is only recently that psychological research has revealed that the behavioural immune system has implications for gregariousness, xenophobia, conformity and other conceptually related attitudes. It will be important for future research to rigorously test whether these social outcomes might actually have positive health implications in contemporary human populations. In doing so, it will be useful to examine effects of individuals' attitudes not only on their own health outcomes but also on population-level epidemiological outcomes too.
(b). Potential implications for epidemiological outcomes
In order to identify plausible linkages between individual-level behavioural decisions and population-level epidemiological outcomes, it is useful to refer to the basic reproduction number (R0) employed in many epidemiological models [60]. R0 represents the average number of secondary cases produced by an infectious individual during the period of time in which that individual is infectious. For diseases that spread via direct or indirect social contact, R0 is typically computed as a function of three parameters: (i) the average length of time that infected individuals remain infectious; (ii) the number of susceptible people that individuals have contact with per unit of time; and (iii) the probability that the infection will actually be transmitted per contact. Although the first of those parameters may not be meaningfully affected by social behaviour, the latter two parameters are likely to be affected—with further implications for R0 and, consequently, for epidemiological outcomes.
For instance, drawing on empirical results reviewed above, one might predict that (compared with circumstances in which people are relatively unconcerned with disease) when people perceive some increased vulnerability to disease, they will have reduced numbers of sexual partners and may also be more inclined to use condoms during sexual intercourse. The first of these behavioural outcomes reduces potential opportunities for transmission of sexually transmitted infections; the second reduces the probability of transmission per opportunity. Jointly, the logical implication is a lower value for R0 and, consequently, a slower rate of infection within the susceptible population.
A similar predictive calculus applies to the epidemiological implications of gregariousness. When people perceive some increased vulnerability to disease, they may interact with relatively fewer people, which reduces potential opportunities for transmission of diseases that are transmitted via interpersonal interaction. This leads to a lower value for R0 and a slower rate of infection within the population.
Xenophobia also has potential epidemiological implications—not so much for the speed of spread within a particular ethnic or cultural population, but for the potential that a disease might spread more widely to additional ethnic or cultural populations as well. People who perceive themselves to be more vulnerable to infection not only express more exclusionary attitudes toward foreigners, they also are less likely to engage in behaviours—such as international air travel—that put them in contact with foreign peoples [61]. This in turn makes it more likely that a disease outbreak may be contained within an ethnic or cultural population, rather than spreading to additional ethnic or cultural populations.
Positive implications for epidemiological outcomes may also follow from the effects that infection risk has on conformity behaviour and authoritarian attitudes. If indeed existing cultural traditions—such as those governing food preparation—do serve as useful barriers against disease transmission, then conformity to those norms would be expected to reduce R0 and inhibit rates of infection. Authoritarian attitudes typically imply willingness to obey the commands of authority figures. Obedience of this sort may lead to greater compliance with government-mandated policies or laws that are often enacted as emergency measures during times of epidemic outbreaks and are designed to retard or contain the spread of infection. Of course, these positive implications of conformity and obedience are predicated upon the assumption that the relevant norms and policies are ‘good’ ones—that they actually do retard or contain the spread of infection. This assumption does not always hold; and when it does not, then increased tendencies toward conformity and obedience may not reduce infection rates at all, and may instead contribute to more dire epidemiological outcomes. One such example occurred when South African government officials persisted in supporting traditional but dubious dietary remedies (e.g. beetroot, garlic, beer) as a treatment for AIDS, while opposing effective antiretroviral therapies [62].
This last example illustrates the possibility that, in modern societies, the health implications of the behavioural immune system may not always be positive. In the following section, we explore this theme more fully, and identify specific negative health outcomes that might plausibly follow from the social attitudes associated with anti-parasite defence.
5. These social attitudes may also have negative health implications in modern societies
Human behavioural strategies of anti-parasite defence are dependent upon many different underlying neural mechanisms, some of which are evolutionarily ancient (and are common across many mammal species [63]) and others that are likely to have evolved relatively recently (some of which may even be unique to humans). Regardless of their relative antiquity, one thing is clear: these mechanisms evolved under ecological circumstances that are different from the circumstances that characterize many modern human populations. Two differences are especially relevant. First, in most parts of the modern world, people live longer lives now than they did in ancestral populations. Second, recent technological advances are such that, in many modern populations (especially within economically developed countries), infectious diseases pose a much less potent threat to human health than they did even a hundred years ago [64]. Thus, while evolved behavioural strategies for parasite-avoidance might still offer the same specific health benefit (reduced risk of contracting infectious diseases) that they provided throughout much of human history, these behaviours may be associated with different kinds of health problems—especially problems that are more likely to manifest as one ages—that matter greatly in modern societies. Furthermore, as we discuss more fully below, there may be negative effects even on infection risk.
This theme—that psychological mechanisms adapted to ancestral ecologies may not be adaptive, or even healthy, in modern ones—is not specific to the behavioural immune system. Indeed, the ‘mismatch’ between adaptations and contemporary human ecologies is an important principle in the field of evolutionary medicine [65,66]. A well-known example is the gustatory affection that humans have for fats and sugars. In ancestral ecologies characterized by short lifespans and scarcity of food supplies, the disposition to devour fats and sugars is likely to have had benefits that outweighed costs. In modern human ecologies characterized by long lifespans and an abundance of readily available processed foods, this same disposition contributes to morbid obesity, diabetes, heart disease and other serious health problems.
Perhaps an even more topical example lies in research linking human perception to immunological defences. Recent experiments reveal that the visual perception of infection-connoting stimuli leads to more vigorous immunological responses to infection [67–69]. For instance, one study [67] found that, compared with a control condition (in which perceivers saw photos connoting the threat of interpersonal violence), when perceivers saw photos depicting other people suffering from infectious diseases, their white blood cells produced more pro-inflammatory cytokines in response to a bacterial stimulus. Exaggerated pro-inflammatory responses can have obvious immediate health benefits (by helping to prevent infections from becoming established). Less obviously, however, there is the potential for long-term health costs—because persistent activation of immunological responses can lead to detrimental effects on individuals' immune functioning later in life [70]. Any such long-term costs were unlikely to have had much impact on health and fitness under ecological circumstances in which lifespans were relatively short. But in modern societies in which lifespans are longer, these long-term negative consequences for individuals' health outcomes may be non-trivial.
Similarly, behavioural anti-parasite defence strategies adapted to ancestral ecologies may also have negative implications for health outcomes in modern societies. In the following paragraphs, we revisit some of the attitudinal phenomena reviewed above and identify potential negative implications that they may have for individual- and population-level health outcomes in the modern world.
(a). Potential health costs of reduced gregariousness
Consider first the inhibiting effects that the perceived threat of infection has on gregariousness. This response may help prevent infection under conditions in which contact with other people actually poses a substantial risk of contracting debilitating infections. But this health benefit may be negligible in many contemporary societies characterized by technological advances in public health (which reduce the likelihood of contracting infections) and medical care (which reduces the likelihood that an infection actually becomes debilitating). Furthermore, the infection-specific costs of social interaction must be weighed against the broader health benefits associated with social interaction—benefits that are especially likely to be realized within modern populations characterized by long lifespans. Individuals who are less gregarious have smaller networks of friends, which puts them at greater risk for loneliness and insufficient social support in times of need—both of which are associated with poorer health outcomes ([71–74]; see also Hawkley & Capitanio [75]). Especially relevant perhaps is the fact that people who are socially disconnected experience greater cumulative stress over the course of their lives. In the words of Cacioppo et al. [71, p. 72] ‘this stress contributes to wear and tear on individual organs (e.g. the heart) and deterioration of regulatory mechanisms (e.g. homeostasis) in the brain and body. As a consequence, the health of lonely individuals fails sooner than the health of nonlonely individuals’. Cumulative stress may have been a relatively minor health concern (and have had negligible implications for reproductive fitness) in ancestral populations. But, in many modern societies—in which the objective risk of contact with truly dangerous parasites is small but individuals' subjective sense of vulnerability to infection remains easily aroused, and in which people live relatively long lives—the potential for long-term negative health consequences cannot be so easily dismissed.
(b). Potential health costs of xenophobic attitudes
Xenophobic attitudes can also have costs that—within modern human societies—may outweigh the benefits with which they were presumably associated in ancestral ecologies. These costs are likely to emerge even (and perhaps especially) under conditions in which infectious diseases do pose a serious health threat. There are several reasons. One reason arises from tendency to blame foreigners and ethnic out-group members for novel disease outbreaks [76]. There are many examples, both classic (many Europeans blamed Jews for outbreaks of the Black Death in Europe during the fourteenth century [77]) and contemporary (e.g. scapegoating of Chinese immigrants for outbreaks of SARS in North America [78]). Xenophobic explanations may be psychologically appealing to people terrified of diseases with mysterious origins, but (as illustrated by the examples identified above) these explanations are often wrong. Indeed, because people tend to be ‘satisficers’ [79] when it comes to explanations, these appealing-but-erroneous explanations may reduce efforts to seek further explanations that might actually be accurate, and so may actually inhibit the discovery of effective solutions to disease outbreaks.
Xenophobic explanations sometimes take the form of conspiracy theories (e.g. black Africans blaming AIDS on the white governments of non-African countries [62,80]) that, like the disease outbreaks they attempt to explain, can spread rapidly within cultural populations [81]. Individuals' belief in conspiracy theories is trait-like: people who believe in any one conspiracy theory tend to believe also in other conspiracy theories [82]. Consequently, to the extent that people attribute disease outbreaks to the shady dealings of foreign governments, they may also be more likely to distrust their own local governments as well. In the modern world, local government programmes provide real health benefits and real buffers against disease (e.g. government-mandated vaccination programmes). Distrust of these programmes can lead to a failure to take part in them [83,84], with negative health consequences for oneself and also for others.
Xenophobia may also promote distrust of aid provided by foreign nations and transnational non-governmental organizations. This attitude can have problematic health implications especially within developing nations, given that these nations are especially likely to be offered aid from foreign governments and from transnational organizations that provide useful resources for combating infectious diseases and other health problems. In 2003, for instance, distrust of Western governments led three states in northern Nigeria to boycott a polio vaccination programme sponsored by the World Health Organization [85]. More broadly, to the extent that people—or their local government representatives—are distrustful of subjectively ‘foreign’ medical resources, the potential benefits of those resources are likely to be underutilized.
(c). Potential health costs of conformist attitudes
Individuals' access to beneficial health resources may also be inhibited by conformist attitudes. The anti-parasite benefits of conformity are predicated upon ecological circumstances characterizing pre-industrial societies, within which epidemiological knowledge was minimal and adherence to existing behavioural rituals provided a principle means of minimizing parasite transmission [42]. These benefits are negligible in many contemporary societies—especially those within which there exist better buffers against disease transmission (e.g. public health infrastructure) and many additional means of limiting the health costs associated with infection when it does occur (e.g. antibiotic medications and other medical intervention strategies). Within these societal contexts, individuals who adhere to old-fashioned rituals and norms may experience poorer health outcomes than individuals who more willingly accept, and adopt, newer and better ways of doing things. Conformist attitudes also inhibit scientific and technological innovation [86], and thus may limit the likelihood that individuals will discover new strategies for preventing infection, treating infection or for minimizing health problems more generally. One ironic, and troubling, implication is that many people who are most likely to benefit from new strategies—individuals living in ecologies in which parasites are most prevalent—may be attitudinally disinclined to seek out or adopt such strategies.
(d). Further implications for population-level health outcomes
Xenophobic and conformist attitudes may not only prove costly to individuals' own health outcomes, but may have negative population-wide health implications too. Some of these population-level outcomes follow from the mathematical logic of epidemiology. For instance, whether motivated by xenophobia or by the psychological appeal of conforming to existing traditions, if individuals fail to avail themselves of effective new strategies for the prevention of infection (e.g. vaccines), this behavioural decision increases the likelihood that they will become infected and, consequently, will transmit the infection to others. The resulting increase in R0 implies a faster rate of infection within the population and, potentially, the emergence of otherwise preventable epidemics.
Additional population-level health consequences follow from the fact that, in many modern societies, individuals' attitudes influence the laws and public policies created by governments. Recall that the perceived threat of infection can lead individuals to endorse more conservative political attitudes [46]. To the extent that these perceptions are shared widely within a population (as they may be whenever infectious diseases receive wide coverage in popular media), one potential implication is the election of more conservative politicians and the formation of governments with more conservative political platforms. These platforms inform the passage of policies, budgets and laws that can have enduring effects on population-wide health outcomes. The exact nature of those enduring health outcomes may depend on exactly how conservatism manifests within the local political context, and on whatever the existing health-relevant cultural traditions might be. In contexts in which long-standing healthcare programmes and policies are generally effective in serving the health needs of the populace, conservation of those programmes and policies may have generally positive consequences for public health. However, in other contexts—in which traditional programmes and policies do a relatively ineffective job of serving public healthcare needs—conservative political ideologies may inhibit the passage of novel healthcare policies that could otherwise provide health benefits to substantial numbers of people.
6. Concluding comments
Human behavioural decision-making is governed by a nervous system that evolved over many millions of years, under ecological circumstances that are similar to, but different from, the circumstances under which most people live today. Among the similarities is the presence of disease-causing parasites. Among the differences are the species of parasites themselves, the magnitudes of the health threats posed by these parasites and the means available to mitigate those threats. Because of the similarities, behavioural strategies that served an infection-avoidance function in the evolutionary past may still serve that function and, consequently, have positive implications for human health outcomes. But, because of the differences, these behavioural strategies can also have negative implications for health outcomes in the modern world. In terms of their net impact on human health, the benefits of these behavioural strategies are most likely to exceed their costs within contemporary contexts under which the health costs posed by infectious diseases are relatively high and under which other means of mitigating that threat are largely unavailable. By contrast, under ecological conditions in which the risk of contracting a debilitating infection is relatively low and there exist effective means of treating such infections if they do occur, the potential health benefits of those behavioural strategies may be outweighed by their costs.
Although there is a substantial body of recent empirical research linking the behavioural immune system to specific aspects of human social cognition and behaviour [5], there remains a real need for empirical research that rigorously tests hypotheses about the further consequences for actual health outcomes of various kinds. By identifying some of these plausible implications, we hope that this article may help motivate such research.
Funding statement
Much of the research summarized in this article, along with the preparation of the article itself, was supported by research grants from the Social Sciences and Humanities Research Council of Canada.
Author's contributions
M.S., D.R.M. and A.B. contributed to the development of the contents of this article and to the review of relevant scholarly literatures. M.S. did the primary writing. All authors gave final approval for publication.
Conflict of interests
We have no competing interests.
References
- 1.Altizer S, et al. 2003. Social organization and parasite risk in mammals: integrating theory and empirical studies. Annu. Rev. Ecol. Evol. Syst. 34, 517–547. ( 10.1146/annurev.ecolsys.34.030102.151725) [DOI] [Google Scholar]
- 2.Cremer S, Armitage SAO, Schmid-Hempel P. 2007. Social immunity. Curr. Biol. 17, R693–R702. ( 10.1016/j.cub.2007.06.008) [DOI] [PubMed] [Google Scholar]
- 3.Freeland WJ. 1976. Pathogens and the evolution of primate sociality. Biotropica 8, 12–24. ( 10.2307/2387816) [DOI] [Google Scholar]
- 4.Hart BL. 1990. Behavioral adaptations to pathogens and parasites: five strategies. Neurosci. Biobehav. Rev. 14, 273–294. ( 10.1016/S0149-7634(05)80038-7) [DOI] [PubMed] [Google Scholar]
- 5.Schaller M. 2011. The behavioural immune system and the psychology of human sociality. Phil. Trans. R. Soc. B 366, 3418–3426. ( 10.1098/rstb.2011.0029) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevensen RJ, Case TI, Oaten MJ. 2011. Proactive strategies to avoid infectious disease. Phil. Trans. R. Soc. B 366, 3361–3363. ( 10.1098/rstb.2011.0170) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meunier J. 2015. Social immunity and the evolution of group living in insects. Phil. Trans. R. Soc. B 370, 20140102 ( 10.1098/rstb.2014.0102) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dantzer R, Kelley KW. 2007. Twenty years of research on cytokine-induced sickness behavior. Brain Behav. Immun. 21, 153–160. ( 10.1016/j.bbi.2006.09.006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hart BL. 2011. Behavioural defences in animals against pathogens and parasites: parallels with the pillars of medicine in humans. Phil. Trans. R. Soc. B 366, 3406–3417. ( 10.1098/rstb.2011.0092) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huffman MA. 2003. Animal self-medication and ethno-medicine: exploration and exploitation of the medicinal properties of plants. Proc. Nutr. Soc. 62, 371–381. ( 10.1079/PNS2003257) [DOI] [PubMed] [Google Scholar]
- 11.Kiesecker JM, Skelly DK, Beard KH, Preisser E. 1999. Behavioral reduction of infection risk. Proc. Natl Acad. Sci. USA 96, 9165–9168. ( 10.1073/pnas.96.16.9165) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodall J. 1986. Social rejection, exclusion, and shunning among the Gombe chimpanzees. Ethol. Sociobiol. 7, 227–239. ( 10.1016/0162-3095(86)90050-6) [DOI] [Google Scholar]
- 13.Chapuisat M, Oppliger A, Magliano P, Christe P. 2007. Wood ants use resin to protect themselves against pathogens. Proc. R. Soc. B 274, 2013–2017. ( 10.1098/rspb.2007.0531) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray DR, Schaller M. 2012. Threat(s) and conformity deconstructed: perceived threat of infectious disease and its implications for conformist attitudes and behavior. Eur. J. Soc. Psychol. 42, 180–188. ( 10.1002/ejsp.863) [DOI] [Google Scholar]
- 15.Tybur JM, O'Brien D. 2014. The behavioral immune system: taking stock and charting new directions. Evol. Behav. Sci. 8, 223–225. ( 10.1037/ebs0000025) [DOI] [Google Scholar]
- 16.Schaller M. In press The behavioral immune system: twelve things you need to know. In Handbook of evolutionary psychology (ed. Buss DM.), 2nd edn New York, NY: Wiley. [Google Scholar]
- 17.Curtis V, de Barra M, Aunger R. 2011. Disgust as an adaptive system for disease avoidance behaviour. Phil. Trans. R. Soc. B. 366, 389–401. ( 10.1098/rstb.2010.0117) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oaten M, Stevenson RJ, Case TI. 2009. Disgust as a disease-avoidance mechanism. Psychol. Bull. 135, 303–321. ( 10.1037/a0014823) [DOI] [PubMed] [Google Scholar]
- 19.Lieberman D, Patrick C. 2014. Are the behavioral immune system and pathogen disgust identical? Evol. Behav. Sci. 8, 244–250. ( 10.1037/ebs0000018) [DOI] [Google Scholar]
- 20.Schaller M. 2014. When and how disgust is and is not implicated in the behavioral immune system. Evol. Behav. Sci. 8, 251–256. ( 10.1037/ebs0000019) [DOI] [Google Scholar]
- 21.Kurzban R, Leary MR. 2001. Evolutionary origins of stigmatization: the functions of social exclusion. Psychol. Bull. 127, 187–208. ( 10.1037/0033-2909.127.2.187) [DOI] [PubMed] [Google Scholar]
- 22.Rozin P, Millman L, Nemeroff C. 1986. Operation of the laws of sympathetic magic in disgust and other domains. J. Pers. Soc. Psychol. 50, 703–712. ( 10.1037/0022-3514.50.4.703) [DOI] [Google Scholar]
- 23.Ryan S, Oaten M, Stevenson RJ, Case TI. 2012. Facial disfigurement is treated like an infectious disease. Evol. Hum. Behav. 33, 639–646. ( 10.1016/j.evolhumbehav.2012.04.001) [DOI] [Google Scholar]
- 24.Haselton MG, Nettle D. 2006. The paranoid optimist: an integrative evolutionary model of cognitive biases. Pers. Soc. Psychol. Rev. 10, 47–66. ( 10.1207/s15327957pspr1001_3) [DOI] [PubMed] [Google Scholar]
- 25.Nesse RM. 2005. Natural selection and the regulation of defenses: a signal detection analysis of the smoke detector principle. Evol. Hum. Behav. 26, 88–105. ( 10.1016/j.evolhumbehav.2004.08.002) [DOI] [Google Scholar]
- 26.Schaller M, Neuberg SL. 2012. Danger, disease, and the nature of prejudice(s). Adv. Exp. Soc. Psychol. 46, 1–55. ( 10.1016/B978-0-12-394281-4.00001-5) [DOI] [Google Scholar]
- 27.Markel H, Stern AM. 2002. The foreignness of germs: the persistent association of immigrants and disease in American society. Millbank Q. 80, 757–788. ( 10.1111/1468-0009.00030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson RM, May RM. 1991. Infectious diseases of humans: dynamics and control. Oxford, UK: Oxford University Press. [Google Scholar]
- 29.Glasier A, Gülmezoglu AM, Schmid GP, Moreno CG, Van Look PFA. 2006. Sexual and reproductive health: a matter of life and death. Lancet 368, 1595–1607. ( 10.1016/S0140-6736(06)69478-6) [DOI] [PubMed] [Google Scholar]
- 30.van Schaik CP. 2013. The costs and benefits of flexibility as an expression of behavioural plasticity: a primate perspective. Phil. Trans. R. Soc. B 368, 20120339 ( 10.1098/rstb.2012.0339) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Faulkner J, Schaller M, Park JH, Duncan LA. 2004. Evolved disease-avoidance mechanisms and contemporary xenophobic attitudes. Group Process. Interg. Behav. 7, 333–353. ( 10.1177/1368430204046142) [DOI] [Google Scholar]
- 32.Green EGT, Krings F, Staerklé C, Bangerter A, Clémence A, Wagner-Egger P, Bornand T. 2010. Keeping the vermin out: perceived disease threat and ideological orientations as predictors of exclusionary immigration attitudes. J. Community Appl. Soc. Psychol. 20, 299–316. ( 10.1002/casp.1037) [DOI] [Google Scholar]
- 33.Navarrete CD, Fessler DMT, Eng SJ. 2007. Elevated ethnocentrism in the first trimester of pregnancy. Evol. Hum. Behav. 28, 60–65. ( 10.1016/j.evolhumbehav.2006.06.002) [DOI] [Google Scholar]
- 34.Murray DR, Jones DL, Schaller M. 2013. Perceived threat of infectious disease and its implications for sexual attitudes. Pers. Indiv. Differ. 54, 103–108. ( 10.1016/j.paid.2012.08.021) [DOI] [Google Scholar]
- 35.Tybur JM, Bryan AD, Magnan RE, Hooper AEC. 2011. Smells like safe sex: olfactory pathogen primes increase intentions to use condoms. Psychol. Sci. 22, 478–480. ( 10.1177/0956797611400096) [DOI] [PubMed] [Google Scholar]
- 36.Mortensen CR, Becker DV, Ackerman JM, Neuberg SL, Kenrick DT. 2010. Infection breeds reticence: the effects of disease salience on self-perceptions of personality and behavioral avoidance tendencies. Psychol. Sci. 21, 440–447. ( 10.1177/0956797610361706) [DOI] [PubMed] [Google Scholar]
- 37.Schaller M, Murray DR. 2008. Pathogens, personality, and culture: disease prevalence predicts worldwide variability in sociosexuality, extraversion, and openness to experience. J. Pers. Soc. Psychol. 95, 212–221. ( 10.1037/0022-3514.95.1.212) [DOI] [PubMed] [Google Scholar]
- 38.Schaller M, Murray DM. 2010. Infectious diseases and the evolution of cross-cultural differences. In Evolution, culture, and the human mind (eds Schaller M, Norenzayan A, Heine SJ, Yamagishi T, Kameda T.), pp. 243–256. New York, NY: Psychology Press. [Google Scholar]
- 39.Letendre K, Fincher CL, Thornhill R. 2010. Does infectious disease cause global variation in the frequency of intrastate armed conflict and civil war? Biol. Rev. 85, 669–683. ( 10.1111/j.1469-185X.2010.00133.x) [DOI] [PubMed] [Google Scholar]
- 40.Barry JM. 2004. The great influenza. London, UK: Penguin. [Google Scholar]
- 41.Thagard P. 1999. How scientists explain disease. Princeton, NJ: Princeton University Press. [Google Scholar]
- 42.Fabrega H. 1997. Earliest phases in the evolution of sickness and healing. Med. Anthropol. Q. 11, 26–55. ( 10.1525/maq.1997.11.1.26) [DOI] [PubMed] [Google Scholar]
- 43.Wu B, Chang L. 2012. The social impact of pathogen threat: how disease salience influences conformity. Pers. Indiv. Differ. 53, 50–54. ( 10.1016/j.paid.2012.02.023) [DOI] [Google Scholar]
- 44.Griskevicius V, Goldstein NJ, Mortensen CR, Cialdini RB, Kenrick DT. 2006. Going along versus going alone: when fundamental motives facilitate strategic nonconformity. J. Pers. Soc. Psychol. 91, 281–294. ( 10.1037/0022-3514.91.2.281) [DOI] [PubMed] [Google Scholar]
- 45.Horberg EJ, Oveis C, Keltner D, Cohen AB. 2009. Disgust and the moralization of purity. J. Pers. Soc. Psychol. 97, 963–976. ( 10.1037/a0017423) [DOI] [PubMed] [Google Scholar]
- 46.Terrizzi JA, Shook NJ, McDaniel MA. 2013. The behavioral immune system and social conservatism: a meta-analysis. Evol. Hum. Behav. 34, 99–108. ( 10.1016/j.evolhumbehav.2012.10.003) [DOI] [Google Scholar]
- 47.Helzer EG, Pizarro DA. 2011. Dirty liberals! reminders of physical cleanliness influence moral and political attitudes. Psychol. Sci. 22, 517–522. ( 10.1177/0956797611402514) [DOI] [PubMed] [Google Scholar]
- 48.Fincher CL, Thornhill R, Murray DR, Schaller M. 2008. Pathogen prevalence predicts human cross-cultural variability in individualism/collectivism. Proc. R. Soc. B. 275, 1279–1285. ( 10.1098/rspb.2008.0094) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murray DR, Trudeau R, Schaller M. 2011. On the origins of cultural differences in conformity: four tests of the pathogen prevalence hypothesis. Pers. Soc. Psychol. Bull. 37, 318–329. ( 10.1177/0146167210394451) [DOI] [PubMed] [Google Scholar]
- 50.Van Leeuwen F, Park JH, Koenig BL, Graham J. 2012. Regional variation in pathogen prevalence predicts endorsement of group-focused moral concerns. Evol. Hum. Behav. 33, 429–437. ( 10.1016/j.evolhumbehav.2011.12.005) [DOI] [Google Scholar]
- 51.Murray DR, Schaller M, Suedfeld P. 2013. Pathogens and politics: further evidence that parasite prevalence predicts authoritarianism. PLoS ONE 8, e62275 ( 10.1371/journal.pone.0062275) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thornhill R, Fincher CL, Aran D. 2009. Parasites, democratization, and the liberalization of values across contemporary countries. Biol. Rev. 84, 113–131. ( 10.1111/j.1469-185X.2008.00062.x) [DOI] [PubMed] [Google Scholar]
- 53.Burk RD, Ho GYF, Beardsley L, Lempa M, Peters M, Bierman R. 1996. Sexual behavior and partner characteristics are the predominant risk factors for genital human papillomavirus infection in young women. J. Infect. Dis. 174, 679–689. ( 10.1093/infdis/174.4.679) [DOI] [PubMed] [Google Scholar]
- 54.Frisch M, Glimelius B, van den Brule AJC, Wohlfahrt J, Meijer CJLM, et al. 1997. Sexually transmitted infection as a cause of anal cancer. N. Engl. J. Med. 337, 1350–1358. ( 10.1056/NEJM199711063371904) [DOI] [PubMed] [Google Scholar]
- 55.Manhart LE, Koutsky L. 2002. Do condoms prevent genital HPV infection, external genital warts, or cervical neoplasia? A meta-analysis. Sex. Transm. Dis. 29, 725–735. ( 10.1097/00007435-200211000-00018) [DOI] [PubMed] [Google Scholar]
- 56.de Barra M, Islam MS, Curtis V. 2014. Disgust sensitivity is not associated with health in a rural Bangladeshi sample. PLoS ONE 9, e100444 ( 10.1371/journal.pone.0100444) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Prokop P, Fančovičová J, Fedo P. 2010. Health is associated with antiparasite behavior and fear of disease-relevant animals in humans. Ecol. Psychol. 22, 222–237. ( 10.1080/10407413.2010.496676) [DOI] [Google Scholar]
- 58.Hamrick N, Cohen S, Rodriguez MS. 2002. Being popular can be healthy or unhealthy: stress, social network diversity, and incidence of upper respiratory infection. Health Psychol. 21, 294–298. ( 10.1037/0278-6133.21.3.294) [DOI] [PubMed] [Google Scholar]
- 59.Nettle D. 2005. An evolutionary approach to the extraversion continuum. Evol. Hum. Behav. 26, 363–373. ( 10.1016/j.evolhumbehav.2004.12.004) [DOI] [Google Scholar]
- 60.Diekmann O, Heesterbeek JAP, Metz JAJ. 1990. On the definition and the computation of the basic reproduction ratio R0 in models for infectious diseases in heterogeneous populations. J. Math. Biol. 28 356–382. ( 10.1007/BF00178324) [DOI] [PubMed] [Google Scholar]
- 61.Hamamura T, Park JH. 2010. Regional differences in pathogen prevalence and defensive reactions to the ‘swine flu’ outbreak among East Asians and Westerners. Evol. Psychol. 8, 508–515. [PubMed] [Google Scholar]
- 62.Kalichman S. 2009. Denying AIDS: conspiracy theories, pseudoscience, and human tragedy. New York, NY: Copernicus Books. [Google Scholar]
- 63.Fessler DMT, Gervais M. 2010. From whence the captains of our lives: ultimate and phylogenetic perspectives on emotions in humans and other primates. In Mind the gap: tracing the origins of human universals (eds Kappeler PM, Silk JB.), pp. 261–279. Berlin, Germany: Springer. [Google Scholar]
- 64.Jones DS, Podolsky SH, Greene JA. 2012. The burden of disease and the changing task of medicine. N. Engl. J. Med. 366 2333–2338. ( 10.1056/NEJMp1113569) [DOI] [PubMed] [Google Scholar]
- 65.Williams GC, Nesse RM. 1991. The dawn of Darwinian medicine. Q. Rev. Biol. 66, 1–22. ( 10.1086/417048) [DOI] [PubMed] [Google Scholar]
- 66.Nesse RM, Dawkins R. 2010. Evolution: medicine's most basic science. In Oxford textbook of medicine (eds Warrell DA, Cox TM, Firth JD, Benz EJJ.), pp. 12–15, 5th edn Oxford, UK: Oxford University Press. [Google Scholar]
- 67.Schaller M, Miller GE, Gervais WM, Yager S, Chen E. 2010. Mere visual perception of other people's disease symptoms facilitates a more aggressive immune response. Psychol. Sci. 21, 649–652. ( 10.1177/0956797610368064) [DOI] [PubMed] [Google Scholar]
- 68.Stevenson RJ, Hodgson D, Oaten MJ, Barouei J, Case TI. 2011. The effect of disgust on oral immune function. Psychophysiology 48, 900–907. ( 10.1111/j.1469-8986.2010.01165.x) [DOI] [PubMed] [Google Scholar]
- 69.Stevenson RJ, Hodgson D, Oaten MJ, Moussavi M, Langberg R, Case TI, Barouei J. 2012. Disgust elevates core body temperature and up-regulates certain oral immune markers. Brain Behav. Immunol. 26, 1160–1168. ( 10.1016/j.bbi.2012.07.010) [DOI] [PubMed] [Google Scholar]
- 70.Segerstrom SC, Miller GE. 2004. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol. Bull. 130, 601–630. ( 10.1037/0033-2909.130.4.601) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cacioppo JT, Hawkley LC, Berntson GG. 2003. The anatomy of loneliness. Curr. Dir. Psychol. Sci. 12, 71–74. ( 10.1111/1467-8721.01232) [DOI] [Google Scholar]
- 72.Cohen S. 2004. Social relationships and health. Am. Psychol. 59, 676–684. ( 10.1037/0003-066X.59.8.676) [DOI] [PubMed] [Google Scholar]
- 73.Hawkley LC, Cole SW, Capitanio JP, Norman GJ, Cacioppo JT. 2012. Effects of social isolation on glucocorticoid regulation in social mammals. Horm. Behav. 62, 314–323. ( 10.1016/j.yhbeh.2012.05.011) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jaremka LM, Fagundes CP, Peng J, Bennett JM, Glaser R, Malarkey WB, Kiecolt-Glaser JK. 2013. Loneliness promotes inflammation during acute stress. Psychol. Sci. 24, 1089–1097. ( 10.1177/0956797612464059) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hawkley LC, Capitanio JP. 2015. Perceived social isolation, evolutionary fitness and health outcomes: a lifespan approach. Phil. Trans. R. Soc. B 370, 20140114 ( 10.1098/rstb.2014.0114) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wagner-Egger P, Bangerter A, Gilles I, Green E, Rigaud D, Krings F, Staerklé C, Clémence A. 2011. Lay perceptions of collectives at the outbreak of the H1N1 epidemic: heroes, villains and victims. Public Underst. Sci. 20, 461–476. ( 10.1177/0963662510393605) [DOI] [PubMed] [Google Scholar]
- 77.Foa A. 2000. The Jews of Europe after the black death. Berkeley, CA: University of California Press. [Google Scholar]
- 78.Eichelberger L. 2007. SARS and New York's Chinatown: the politics of risk and blame during an epidemic of fear. Soc. Sci. Med. 65 1284–1295. ( 10.1016/j.socscimed.2007.04.022) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Simon HA. 1956. Rational choice and the structure of the environment. Psychol. Rev. 63, 129–138. ( 10.1037/h0042769) [DOI] [PubMed] [Google Scholar]
- 80.Farmer P. 2006. AIDS and accusation: Haiti and the geography of blame. Berkeley, CA: University of California Press. [Google Scholar]
- 81.Franks B, Bangerter A, Bauer MW. 2013. Conspiracy theories as quasi-religious mentality: an integrated account from cognitive science, social representations theory, and frame theory. Front. Psychol. 4, 424 ( 10.3389/fpsyg.2013.00424) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wood M, Douglas KM, Sutton RM. 2012. Dead and alive: belief in contradictory conspiracy theories. Soc. Psychol. Pers. Sci. 3, 767–773. ( 10.1177/1948550611434786) [DOI] [Google Scholar]
- 83.Bogart LM, Wagner G, Galvan FH, Banks D. 2010. Conspiracy beliefs about HIV are related to antiretroviral treatment: nonadherence among African American men with HIV. J. Acquir. Immune. Defic. Syndr. 53, 648–655. ( 10.1097/QAI.0b013e3181c57dbc) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gilles I, Bangerter A, Clémence A, Green EGT, Krings F, Staerklé C, Wagner-Egger P. 2011. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur. J. Epidemiol. 26, 203–210. ( 10.1007/s10654-011-9577-2) [DOI] [PubMed] [Google Scholar]
- 85.Jegede AS. 2007. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 4, e73 ( 10.1371/journal.pmed.0040073) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Murray DR. 2014. Direct and indirect implications of disease threat for scientific and technological innovation. J. Cross Cult. Psychol. 45, 971–985. ( 10.1177/0022022114532356) [DOI] [Google Scholar]