Abstract
Background:
There continues to be controversy about performing abdominoplasty concurrently with abdominal liposuction. The concern is that liposuction on the already vascularly compromised abdominal flap will lead to increased complications and flap necrosis. The central abdomen is supplied by the epigastric system. If perforator vessels from this system are spared, the blood supply to the abdomen can be spared and liposuction should be able to be safely performed on the elevated abdominal flap. The purpose of this study was to evaluate the safety of abdominoplasty with concurrent abdominal liposuction when a perforator vessel is spared.
Methods:
A standard abdominoplasty was performed, sparing one or two perforator vessels from the deep superior epigastric artery system. A retrospective chart review of 300 consecutive patients who underwent abdominoplasty surgery combined with concurrent abdominal liposuction was performed. Complications, total volume of abdominal liposuction, and results were reviewed.
Results:
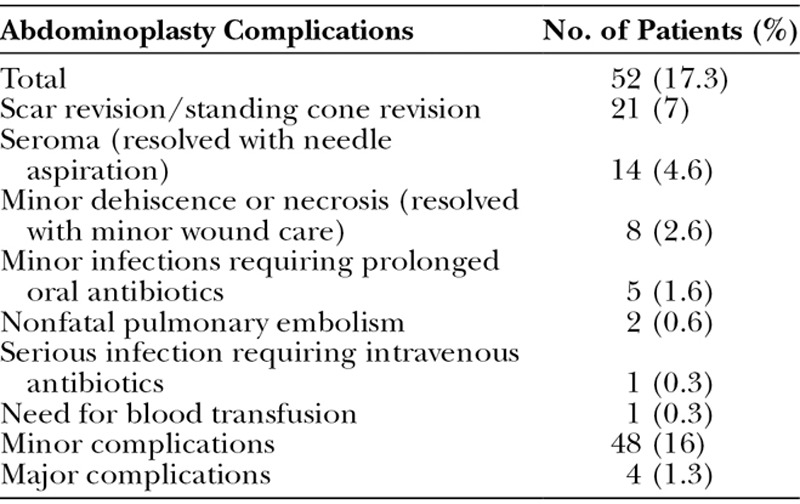
The overall complication rate was 17.3 percent (52 patients). Sixteen percent (48 patients) suffered minor complications and 1.3 percent (four patients) suffered major complications.
Conclusions:
Abdominoplasty can be combined safely with concurrent abdominal liposuction when a perforator vessel is spared. The combination of concurrent liposuction with abdominoplasty showed no increase in complication rates when a perforator vessel was spared. The perforator vessels are located consistently in a 2-cm radius located 4 cm from the midline and 6 cm from the subcostal margin. The potential advantages of abdominoplasty with concurrent liposuction include a better postoperative cosmetic result.
CLINICAL QUESTION/LEVEL OF EVIDENCE:
Therapeutic, IV.

There continues to be controversy about performing liposuction on an undermined abdominoplasty flap.1–5 Early articles warned against the combination of liposuction with abdominoplasty, and these concerns have carried over to present day. In one of the largest recent series of abdominoplasty patients (1008 consecutive patients), the authors strongly recommended against the combination of liposuction and abdominoplasty.4
Liposuction of the undermined abdominal flap has been described as far back as the late 1980s, but was often combined with warnings or recommended changes in abdominoplasty technique.5–9 Matarasso originally recommended against combining abdominoplasty with liposuction, but later revised his recommendation, saying it was safe provided that certain steps were taken.7,8 Lockwood recommended the limited undermining of the central upper portion of the abdominoplasty flap in combination with aggressive liposuction.10 With the Avelar abdominoplasty technique, there is no undermining of the central flap at all, but there is excision of the lower skin and sometimes upper skin, combined with liposuction.11 Shestak described a modified short flap abdominoplasty technique combined with aggressive liposuction but recommended a standard abdominoplasty in patients with extensive loose skin.12 In some articles, it is simply understood that lipoabdominoplasty means limited undermining of the central flap, and abdominoplasty means extensive undermining of the abdominal flap. With this technique of limited undermining of the central flap, Samra et al. noted no increase in complications when combining abdominoplasty with liposuction, even in high-risk patients.13
Traditional abdominoplasty means wide undermining and elevation of the abdominal flap up to the costal margin, also called a type IV abdominoplasty.8 This compromises the blood supply to the central abdominal flap. This was described by Matarasso, who based his work on Huger.8,14 Huger divided the abdominal vascular supply into three zones (Fig. 1). Zone I is the vascular supply to the central abdomen, which is supplied by branches of the deep and superficial superior epigastric artery system. Zone III is the vascular supply to the peripheral abdomen and is supplied by the intercostal, subcostal, and lumbar segmental perforators. Zone II is the vascular supply to the inferior abdomen, which is supplied by the deep inferior epigastric artery system, the deep circumflex iliac artery, the superficial circumflex iliac artery, and the superficial external pudendal artery. During abdominoplasty, zone II is essentially resected and discarded. In the article by Matarasso, the safe areas and unsafe areas of abdominal liposuction based on the blood supply to the abdominal flap that remains after elevation of the flap are described8 (Fig. 1). During abdominoplasty, zone II is traditionally removed and therefore irrelevant. Most of the blood supply to zone III remains after flap elevation, and this is considered a safe area for liposuction. The blood supply to zone I is transected during elevation of the abdominal flap, and liposuction in this area is not recommended. This is the central portion of the abdomen and, theoretically, this area would be the most advantageous area for liposuction if it were safe. Limited liposuction is considered safe by Matarasso in the intermediate area between zone I and zone III because branches of the marginal phrenic artery remain after elevation of the abdominal flap.
Fig. 1.
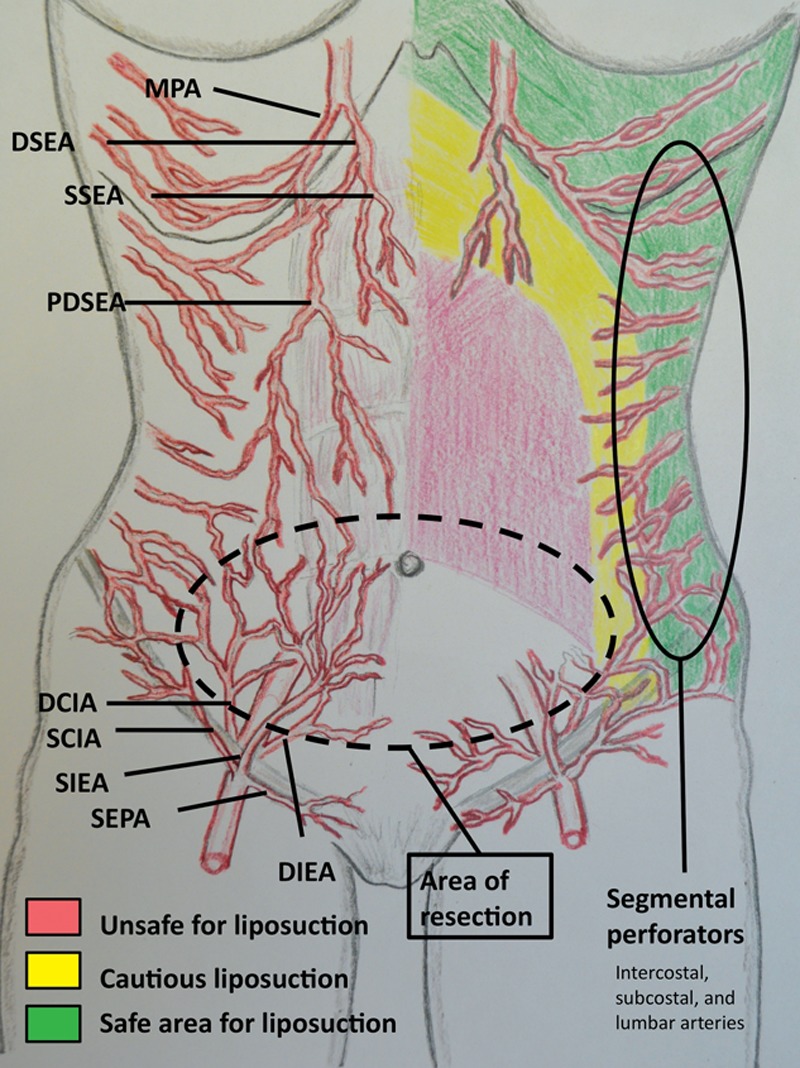
After elevation of the abdominal flap during traditional (type IV) abdominoplasty, the vascular supply to the central abdomen is compromised. The areas marked in green are supplied by the segmental perforators (subcostal, intercostal, and lumbar arteries) that are intact after abdominoplasty, and this area is safe for liposuction. The yellow area is the intermediate area where cautious liposuction can be performed. The red area is poorly supplied, and liposuction in this area is not recommended in the article by Matarasso. DIEA, deep inferior epigastric artery; SIEA, superficial inferior epigastric artery; DCIA, deep circumflex iliac artery; SIEA, superficial circumflex iliac artery; MPA, marginal phrenic artery; DSEA, deep superior epigastric artery; SSEA, superficial superior epigastric artery; PDSEA, perforator deep superior epigastric artery; SEPA, superficial external pudendal artery. (Closely adapted from Matarasso A. Liposuction as an adjunct to full abdominoplasty revisited. Plast Reconstr Surg. 2000;106:1197–1202.)
Theoretically, if the blood supply to zone I could be preserved, aggressive liposuction of the abdominal flap could proceed with impunity. We have found that consistent perforators do exist which, if spared during flap elevation, will supply zone I with sufficient vascularity to allow aggressive liposuction of the central abdominal flap after elevation (Fig. 2).
Fig. 2.
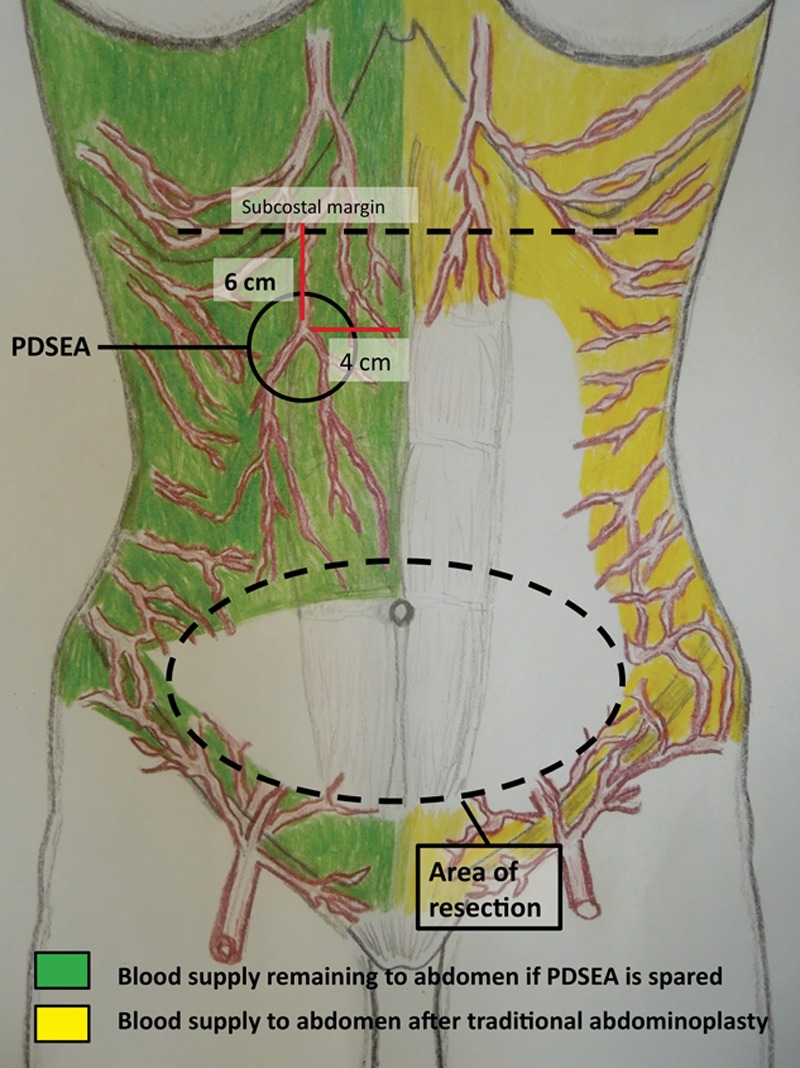
The remaining blood supply to the abdomen after flap elevation and resection of the pannus. On the left, the green area marks the remaining blood supply to the abdomen if the perforator branch of the deep superior epigastric artery (PDSEA) is spared. The location of the perforator branch of the deep superior epigastric artery is typically found in a 2-cm radius of a circle located 6 cm from the costal margin and 4 cm from the midline. Theoretically, the entire green area should be safe for liposuction. On the right, the yellow area marks the remaining blood supply to the flap if the perforator branch of the superior epigastric artery is not spared, as in traditional type IV abdominoplasty. In this case, only the yellow area is safe for liposuction, making liposuction of the central abdomen dangerous.
PATIENTS AND METHODS
A retrospective chart review of patients who underwent abdominoplasty surgery combined with concurrent abdominal liposuction was performed from 2005 to 2010. Three hundred consecutive cases were reviewed. Complications, total volume of abdominal liposuction, and results were reviewed. All subjects were patients of one surgeon. All operations were performed using the same technique, sparing at least one perforator vessel. Patients were excluded who underwent abdominoplasty without liposuction. Abdominoplasty without liposuction was performed only on extremely thin patients who would not have benefited from any liposuction. No patient was excluded from abdominal liposuction that would have benefited from concomitant liposuction, including smokers and those with abdominal scars.
Surgical Technique
A standard abdominoplasty incision is performed and carried down to the fascia. The abdominal flap is elevated to the subcostal margin, isolating the umbilicus and sparing a perforator vessel from the deep superior epigastric artery on each side of the abdomen. It is preferable, but not necessary, to spare both vessels; one vessel is sufficient. This vessel is located consistently in an area within a 2-cm radius located 6 cm below the subcostal margin and 4 cm from the abdominal midline (Fig. 3). The rectus muscles are plicated in the midline. The abdominal flap is pulled down, and excess skin is resected. The table is bent slightly to facilitate closure, but the amount of tissue resection should not be excessive so that the final closure, rather than being extremely tight, is under only moderate tension. The umbilicus is transposed in the standard fashion. The abdominal flap is then temporarily stapled closed and the abdomen, anterior flanks, and surrounding areas are infiltrated with tumescent solution using the superwet technique. Then, 4-mm cannulas are used to perform liposuction of the entire abdomen, including the subcostal region and anterior flanks in the amount the surgeon feels is necessary for optimal abdominal improvement. Laser liposuction and ultrasonic liposuction are not used. This is thought to damage the microvasculature necessary to preserve the abdominal flap blood supply. After completion of liposuction, a single drain is placed, and layered closure of the abdomen is performed. The umbilicus is transposed and the abdominal incision closed in the manner of the surgeon’s choice (layered closure).
Fig. 3.
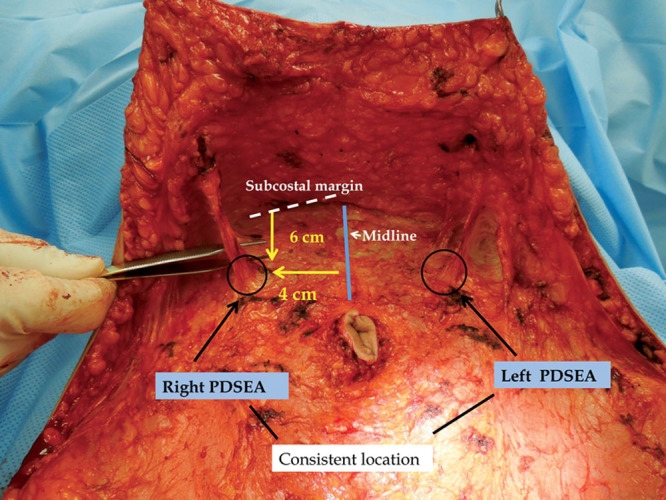
The actual location of the perforator of the deep superior epigastric artery (PDSEA) is shown on this patient during surgery after abdominal flap elevation. The artery is located within a 2-cm radius of a circle located 6 cm from the subcostal margin (dotted line) and 4 cm from the midline (solid blue line). The arteries are typically accompanied by one or two small veins and are bilateral, and consistent in location.
RESULTS
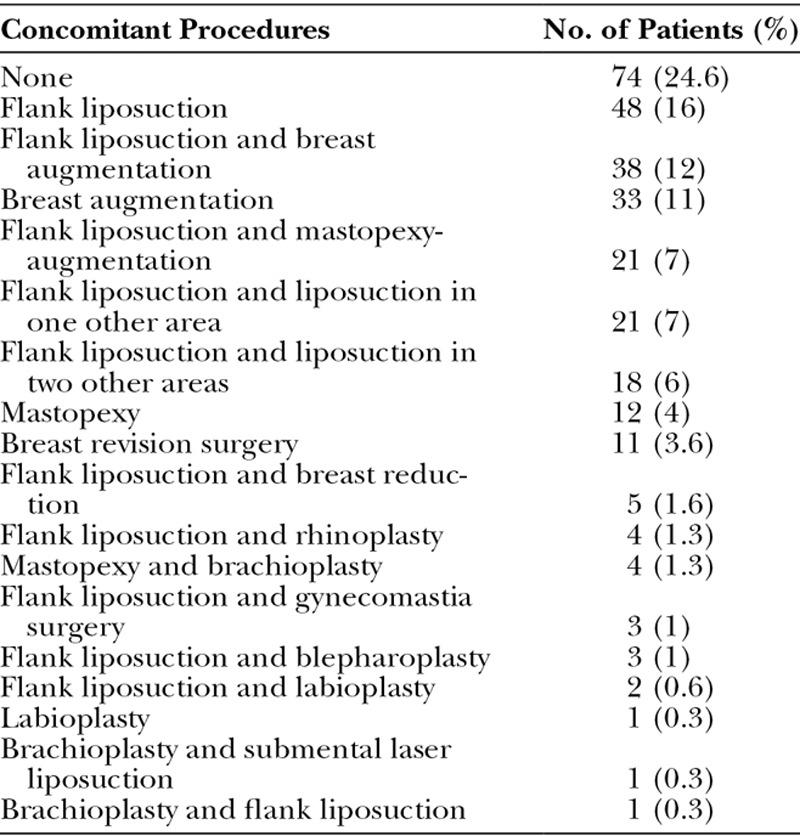
Ninety-five percent of the abdominoplasties were performed as outpatient procedures; 5 percent of patients underwent an overnight stay. In addition to abdominal liposuction, 75.3 percent (226 patients) of the abdominoplasties were combined with other operations, most commonly flank liposuction [165 patients (55 percent)] or breast operations [121 patients (40.3 percent)] (Table 1). The majority of patients had concomitant flank liposuction because the surgeon felt that flank liposuction was an important part of body contouring and recommended it for most patients. This was considered a distinct separate area because the surgeon actually performs the liposuction with the patient in the prone position, removing fat from the lower back and posterior and lateral flanks. Liposuction of the anterior flanks is usually performed as part of the abdominal liposuction. Concomitant hernia repair was performed in 17 patients (5.6 percent) and did not increase the complication rate in any way. One hundred twenty-two patients had three or more procedures (40.6 percent). Fairly aggressive abdominal liposuction was performed on the majority of patients. The average amount of abdominal liposuction aspirate was 660 cc, with a range of 75 to 2200 cc.
Table 1.
Abdominoplasty and Concomitant Procedures in the Study
Fifty-two patients had complications (17.3 percent) (Table 2). Complications were divided into major and minor complications. Only four patients (1.3 percent) had major complications. Forty-eight patients (16 percent) had minor complications. The most common complication was the need for scar or standing cone revision in 21 patients (7 percent). The most common major complication was nonfatal pulmonary embolism in two patients (0.6 percent). The second most common complication was seroma formation in 14 patients (4.6 percent). All seromas resolved with needle aspiration. Minor dehiscence or necrosis usually occurred in the central area of the abdomen along the center of the incision line were the tension is greatest. All dehiscence or necrosis was less than 2 cm wide and 4 cm long. All resolved with minor wound care. Five patients developed infection of the lower abdomen that resolved with prolonged oral antibiotics. One patient had an infection that did not resolve after 3 weeks of oral antibiotics and received intravenous vancomycin and cefazolin given on an outpatient basis for 2 weeks, with complete resolution of his infection. No positive cultures were identified on any patient. One patient was given a blood transfusion.
Table 2.
Complications
DISCUSSION
The combination of abdominoplasty with abdominal liposuction remains a controversial subject. This controversy reached its zenith in February of 2004 when, after several patient deaths, the state of Florida placed a temporary moratorium preventing the simultaneous combination of abdominoplasty with liposuction in the office setting, mandating a minimum 14-day interval between the two operations.15
This study involved 300 consecutive abdominoplasties with concurrent abdominal liposuction; 75.3 percent of the abdominoplasties were combined with other operations, most commonly flank liposuction and/or breast surgery (Table 1). The surgical technique relies on the preservation of perforator vessels to maintain blood supply to the central abdomen after flap elevation. The three zones of vascularity to the abdomen are described above (Fig. 1). Zone II is resected during standard abdominoplasty. The blood supply to zone III remains relatively intact during abdominoplasty, and liposuction has been considered safe in this area.8 The blood supply to zone I is largely transected during flap elevation. Consequently, abdominoplasty with concurrent liposuction of the central abdomen has been considered dangerous, with a high risk of flap necrosis. In our study, preservation of consistent perforators has preserved enough of the blood supply to the central abdomen to allow safe, concurrent liposuction of the elevated abdominal flap (Figs. 2 through 9).
Fig. 9.

The angle view of the same patient as in Figure 8, shown (left) before surgery and (right) 4 weeks after abdominoplasty with concurrent abdomen, flank, and back liposuction. This early result (the patient is still slightly swollen) shows that the changes present are attributable solely to surgery and not patient weight loss.
Fig. 4.

A 38-year-old patient with a preoperative body mass index of 32. (Left) the patient before surgery. (Right) The patient 9 months after abdominoplasty with concurrent abdominal, flank, and back liposuction. Notice the thighs are the same size, indicating the change was attributable solely to the surgery and not patient weight loss.
Fig. 5.
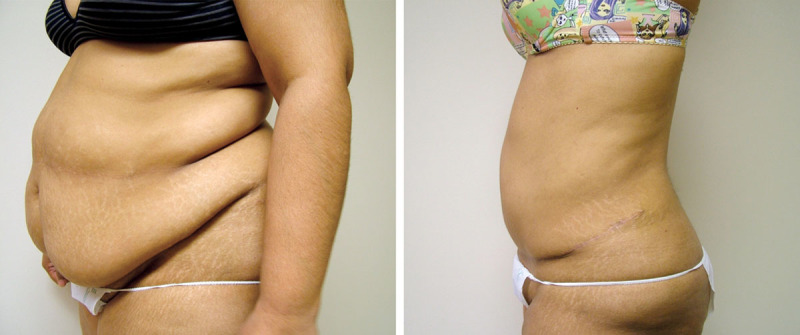
The same patient as in Figure 4 from a side view, shown (left) before surgery and (right) 9 months after abdominoplasty with concurrent abdomen, flank, and back liposuction.
Fig. 6.

A 45-year-old patient with a preoperative body mass index of 28, shown (left) before surgery and (right) 7 months after abdominoplasty combined with concurrent abdomen, flank, and mid-back liposuction. Notice a small brown spot of melasma on the central abdomen in each photograph. On the left it is in a higher location, and the same spot on the right is in a lower location, as it was moved down with the flap advancement.
Fig. 7.
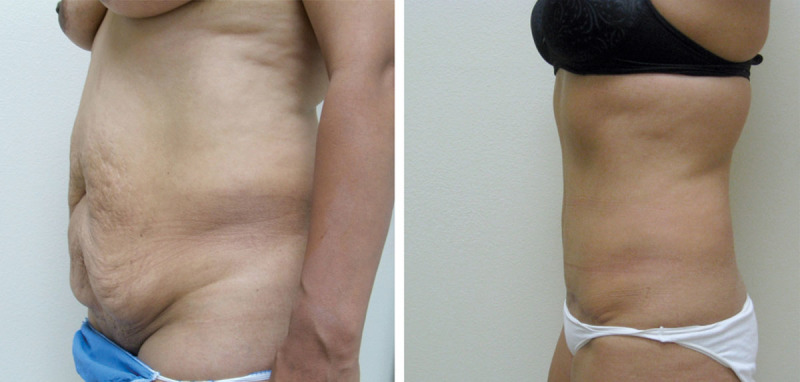
This is the same patient as in Figure 6 from a side view, shown (left) before surgery and (right) after abdominoplasty with concurrent abdomen, flank, and mid-back liposuction.
Fig. 8.

A 29-year-old patient with a preoperative body mass index of 35, shown (left) before surgery and (right) approximately 4 weeks after abdominoplasty with concurrent abdomen, flank, and back liposuction. The purpose of showing this early result is to confirm that the changes present are attributable solely to the surgery and not to patient weight loss after surgery. Note that the incisions are still erythematous and the patient is still slightly swollen after surgery.
In the past, authors recommended against concomitant abdominal liposuction with abdominoplasty.1–5 There has slowly become a partial acceptance of liposuction with abdominoplasty; however, in the majority of cases, this involves altering the abdominoplasty technique in one way or another. This has led to the evolution of a different operation entirely, sometimes called lipoabdominoplasty.12,13,16–20 Lipoabdominoplasty differs from the combination of abdominoplasty and liposuction in that the liposuction is performed first in lipoabdominoplasty, and there is limited undermining of the abdominal flap in the area above the umbilicus, thus sparing multiple perforator vessels. This new operation slowly evolved out of many surgeons’ efforts. Later, more extensive undermining was championed by Samra et al., Brauman, and others.12,13,16–20 This operation differs from traditional abdominoplasty in several ways. First, the liposuction is performed first and the flap is elevated with hydrodissection and liposuction. Second, there is typically limited undermining of the flap above the umbilicus. Third, there is usually no closure, or only segmental closure of the rectus diastasis.17 The results shown in the article by Brauman and Capocci are impressive, and this is a useful technique for body contouring.17 Avelar’s technique involves even less undermining of the superior abdominal flap, and the umbilicus is not transposed.11 His technique does involve the addition of skin excision in the inframammary area in selected cases.
The surgical technique used here relies on perforator vessels that branch off the deep superior epigastric artery to supply the central abdomen. The blood supply provided by these vessels allows for safe liposuction of the entire undermined abdominal flap. In this series, not a single incident of major flap necrosis occurred. The average amount of liposuction aspirate from the abdominal flap was 660 cc (range, 75 to 2200 cc). This is somewhat aggressive, considering that this is mainly liposuction of the original upper abdomen, as most of the lower abdomen is resected during surgery. The concept of perforator vessels for use in abdominal wall reconstruction has been described by Rohrich et al. and Hallock.21,22 It is easy to extend this concept for use in cosmetic abdominoplasty. The perforator vessels can be consistently found in a 2-cm radius located at a point 4 cm from the abdominal midline and 6 cm below the subcostal margin (Figs. 2 and 3). The preservation of these vessels gives a hearty blood supply to the elevated abdominal flap that allows for aggressive liposuction of the abdominal flap and surrounding areas. It should be noted that, most likely, these vessels are also spared in the lipoabdominoplasty techniques referenced above. Close inspection of the photographs in the article by Brauman and Capocci shows perforators in this area that have been spared.17 Although the proponents of the lipoabdominoplasty procedure do not specifically describe or search for this perforator vessel, it is likely these vessels are spared with their technique of limited superior undermining.
The argument against combining liposuction with abdominoplasty has been that this will lead to an increase in complication rates. Mayr et al. postulate that the relatively high complication rate found in standard abdominoplasty without liposuction is related to the loss of vascularity of the abdominal flap.23 Our study shows that when a perforator vessel is spared, abdominoplasty can be safely combined with liposuction, with no increase in complication rates. In fact, the complication rate in this study is lower than many involving abdominoplasty alone, and the lower complication rate may be attributable to the preservation of the central abdominal blood supply. The overall complication rate in this study of 17.3 percent and a major complication rate of just 1.3 percent compare favorably with other studies of abdominoplasty alone.24–27 In a retrospective review of 199 abdominoplasty cases, Hensel et al. reported an overall complication rate of 32 percent and a major complication rate of 1.4 percent.24 In this series, seroma rates approached 14 percent and wound infection rates were 7 percent. Interestingly, revision surgery rates were 43 percent and were used to improve the aesthetic appearance in all cases. They did not count revision surgery as a complication. In our series, we counted the need for revision surgery as a complication and considered this our most frequent complication (7 percent.) If scar/standing cone revision was removed from our complication list, our complication rate drops to 10 percent. Also, it can be assumed that a large part of the high revision surgery rate in the study by Hensel et al. involved the need for liposuction of the abdomen. This need is removed when liposuction is combined with the abdominoplasty, and presumably leads to greater patient satisfaction and a lower revision surgery rate. Neaman et al. reviewed 1080 cases and found a significant increase in complications when abdominoplasty was combined with abdominal liposuction.4 Their complication rate for abdominoplasty alone was 26.2 percent; when combined with abdominal liposuction, it jumped to 40.1 percent. Najera et al., in their retrospective cohort study of 200 abdominoplasties with and without liposuction, noted a seroma rate of 16 percent in the abdominoplasty-only group and a seroma rate of 31.2 percent in the abdominoplasty and liposuction group.27 Conversely, Stevens et al., in their retrospective review of 406 cases, did not find any difference in complication rates among patients that had abdominoplasty alone or abdominoplasty with liposuction.28 Unfortunately, in the study by Stevens et al., there was no description of the surgical technique used, other than to state “when adjunctive lipoplasty was performed, aggressive treatment of the lower abdomen was avoided to minimize interference with the blood supply to the distal flap.” They had a reference at the end of that sentence to the article by Matarasso, in which he recommended no liposuction of the central abdomen, so it can be assumed they did not perform liposuction of the central abdomen.8
The main concern with concurrent liposuction of the abdomen with abdominoplasty is ischemia and necrosis of the flap. Hunstad and Jones describe the mechanism of this complication in their article on concurrent circumferential liposuction with abdominoplasty.29 The area most at risk for this complication is a triangular area beginning at the umbilicus and extending to the suprapubic region. We did not have a single instance of this complication, attesting to the heartiness of the flap when the perforator vessels are spared. Hunstad and Jones also propose liposuction of the abdominal flap and note “a very low incidence of ischemia and necrosis,” but do not give a specific percentage. They do not specifically search for perforator vessels, but with their technique they also note that “important vascular pillars exist that must be respected, but these can be mobilized successfully with vascular preservation using a blunt dissector.”29 As with the article by Brauman and Capocci, inspection of their photographs shows that most likely the perforator vessels shown here have been spared.
Both the advocates of lipoabdominoplasty and Hunstad and Jones stress the importance of tumescent infiltration and liposuction performed before elevation of the abdominal flap. Hunstad and Jones recommend infiltration of 4 to 8 liters of tumescent fluid.28 They and Brauman feel that tumescent infiltration helps to constrict and compress the blood vessels, which is helpful in preventing vascular injury during liposuction.16,17,29 Our technique differs from theirs in that the liposuction of the abdomen is performed at the end of the operation rather than at the beginning. We believe liposuction performed after the pannus has been resected and temporarily stapled closed allows for better contouring and easier identification of standing cones. The superwet technique is used for infiltration with our technique rather than tumescent technique. Rohrich et al. have showed that there is no advantage to the tumescent technique over the superwet technique and that there is a greater risk of fluid overload with the tumescent technique.30,31
An advantage of our technique is that rectus muscle plication is made easier with standard abdominoplasty flap elevation than with limited flap undermining techniques. Brauman16 and Matarasso32 debate the merits of rectus muscle plication, and go so far as to say that it may not be necessary in the majority of patients. Brauman and Capocci later partially reverse this stance in their 2009 article recommending segmental rectus muscle placation.17 Although it is not the point of this article to debate the need for rectus muscle plication, in many patients this can be one of the most important parts of the operation, and we routinely perform rectus muscle plication in the majority of patients. Another possible advantage of more extensive abdominal flap undermining when compared with limited undermining techniques is better correction of superior abdominal fullness and easier redraping of the flap.
CONCLUSIONS
This study of 300 consecutive cases by a single surgeon shows that standard abdominoplasty can be safely combined with concurrent abdominal liposuction when perforator vessels to the abdomen are spared. The perforator vessels are located consistently in a 2-cm radius located 4 cm from the midline and 6 cm from the subcostal margin. The potential advantages of abdominoplasty with concurrent liposuction include a better postoperative cosmetic result and a possible reduction in the need for revision surgery.
Footnotes
Presented at the 63rd Annual Meeting of the California Society of Plastic Surgeons, in San Francisco, California, May 24 through 27, 2013.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.

REFERENCES
- 1.Matarasso A, Swift RW, Rankin M. Abdominoplasty and abdominal contour surgery: A national plastic surgery survey. Plast Reconstr Surg. 2006;117:1797–1808. doi: 10.1097/01.prs.0000209918.55752.f3. [DOI] [PubMed] [Google Scholar]
- 2.Rohrich RJ, Muzaffer AR. Discussion: Fatal outcomes from liposuction: Census survey of cosmetic surgeons. Plast Reconstr Surg. 2000;105:447––448. doi: 10.1097/00006534-200001000-00070. [DOI] [PubMed] [Google Scholar]
- 3.Hester TR, Jr, Baird W, Bostwick J, III, Nahai F, Cukic J. Abdominoplasty combined with other major surgical procedures: Safe or sorry? Plast Reconstr Surg. 1989;83:997–1004. doi: 10.1097/00006534-198906000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Neaman CK, Armstrong SD, Baca M, Renucci JD, Vander Woude DL. Liposuction of the flanks and abdomen during cosmetic abdominoplasty: Safe or sorry? Plast Reconstr Surg. 2010;126:71. [Google Scholar]
- 5.Dillerud E. Abdominoplasty combined with suction lipectomy: A study of complications, revisions and risk factors in 187 cases. Ann Plast Surg. 1990;25:333––338. doi: 10.1097/00000637-199011000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Matarasso A. Abdominolipoplasty. Clin Plast Surg. 1989;16:289––303. [PubMed] [Google Scholar]
- 7.Matarasso A. Liposuction as an adjunct to full abdominoplasty. Plast Reconstr Surg. 1995;95:829––836. [PubMed] [Google Scholar]
- 8.Matarasso A. Liposuction as an adjunct to full abdominoplasty revisited. Plast Reconstr Surg. 2000;106:1997––1202. doi: 10.1097/00006534-200010000-00035. [DOI] [PubMed] [Google Scholar]
- 9.Cárdenas-Camarena L, González IE. Large-volume liposuction and extensive abdominoplasty: A feasible alternative for improving body shape. Plast Reconstr Surg. 1998;102:1698––1707. doi: 10.1097/00006534-199810000-00059. [DOI] [PubMed] [Google Scholar]
- 10.Lockwood T. High lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96:603––615. doi: 10.1097/00006534-199509000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Avelar JM. Abdominoplasty without panniculus undermining and resection: Analysis and 3-year follow-up of 97 consecutive cases. Aesthet Surg J. 2002;22:16–25. doi: 10.1067/maj.2002.121961. [DOI] [PubMed] [Google Scholar]
- 12.Shestak KC. Marriage abdominoplasty expands the mini-abdominoplasty concept. Plast Reconstr Surg. 1999;103:1020–1031; discussion 1032. doi: 10.1097/00006534-199903000-00042. [DOI] [PubMed] [Google Scholar]
- 13.Samra S, Sawh-Martinez R, Barry O, Persing JA. Complication rates of lipoabdominoplasty versus traditional abdominoplasty in high-risk patients. Plast Reconstr Surg. 2010;125:683–690. doi: 10.1097/PRS.0b013e3181c82fb0. [DOI] [PubMed] [Google Scholar]
- 14.Huger WE., Jr The anatomic rationale for abdominal lipectomy. Am Surg. 1979;45:612–617. [PubMed] [Google Scholar]
- 15.Florida Board of Medicine. Emergency Rule 64b8er04-2: Moratorium on combined liposuction/abdominoplasty procedures in office surgery settings Florida Administrative Weekly. 2004;30:808. [Google Scholar]
- 16.Brauman D. Liposuction abdominoplasty: An evolving concept. Plast Reconstr Surg. 2003;121:288––298. doi: 10.1097/01.PRS.0000066371.34978.F0. [DOI] [PubMed] [Google Scholar]
- 17.Brauman D, Capocci J. Liposuction abdominoplasty: An advanced body contouring technique. Plast Reconstr Surg. 2009;124:1685–1695. doi: 10.1097/PRS.0b013e3181b98c5d. [DOI] [PubMed] [Google Scholar]
- 18.Illouz YG. A new safe and aesthetic approach to suction abdominoplasty. Aesthetic Plast Surg. 1992;16:237––245. doi: 10.1007/BF00190070. [DOI] [PubMed] [Google Scholar]
- 19.Saldanha OR, Pinto EB, Matos WN, Jr, Lucon RI, Magalhães F, Bello EM. Lipoabdominoplasty without undermining. Aesthet Surg J. 2001;1:518––526. doi: 10.1067/maj.2001.121243. [DOI] [PubMed] [Google Scholar]
- 20.Matos WN, Jr, Ribeiro RC, Marujo RA, da Rocha RP, da Silva Ribeiro SM, Carillo Jiminez VF. Classifications for indications of lipoabdominoplasty and its variations. Aesthet Surg J. 2006;26:417––431. doi: 10.1016/j.asj.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 21.Rohrich RJ, Lowe JB, Hackney FL, Bowman JL, Hobar PC. An algorithm for abdominal wall reconstruction. Plast Reconstr Surg. 2000;105:202––216. doi: 10.1097/00006534-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 22.Hallock GG. A paradigm shift for soft-tissue coverage of the zones of the abdominal wall using perforator flaps. Plast Reconstr Surg. 2012;130:590––599. doi: 10.1097/PRS.0b013e31825dc1cc. [DOI] [PubMed] [Google Scholar]
- 23.Mayr M, Holm C, Höfter E, Becker A, Pfeiffer U, Mühlbauer W. Effects of abdominoplasty on abdominal wall perfusion: A quantitative evaluation. Plast Reconstr Surg. 2004;114:1586––1594. doi: 10.1097/01.prs.0000138757.33998.ee. [DOI] [PubMed] [Google Scholar]
- 24.Hensel JM, Lehman JA, Jr, Tantri MP, Parker MG, Wagner DS, Topham NS. An outcomes analysis and satisfaction survey of 199 consecutive abdominoplasties. Ann Plast Surg. 2001;46:357–363. doi: 10.1097/00000637-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Buck DW, II, Mustoe TA. An evidence based approach to abdominoplasty. Plast Reconstr Surg. 2010;126:2189––2195. doi: 10.1097/PRS.0b013e3181f83115. [DOI] [PubMed] [Google Scholar]
- 26.van Uchelen JH, Werker PM, Kon M. Complications of abdominoplasty in 86 patients. Plast Reconstr Surg. 2001;107:1869–1873. doi: 10.1097/00006534-200106000-00037. [DOI] [PubMed] [Google Scholar]
- 27.Najera RM, Asheld W, Sayeed SM, Glickman LT. Comparison of seroma formation following abdominoplasty with or without liposuction. Plast Reconstr Surg. 2011;127:417–422. doi: 10.1097/PRS.0b013e3181f95763. [DOI] [PubMed] [Google Scholar]
- 28.Stevens WG, Cohen R, Vath SD, Stoker DA, Hirsch EM. Does lipoplasty really add morbidity to abdominoplasty: Revisiting the controversy with a series of 406 cases. Aesthet Surg J. 2005;25:353––358. doi: 10.1016/j.asj.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Hunstad JP, Jones SR. Abdominoplasty with thorough concurrent circumferential abdominal tumescent liposuction. Aesthet Surg J. 2011;31:572–590. doi: 10.1177/1090820X11412487. [DOI] [PubMed] [Google Scholar]
- 30.Trott SA, Beran SJ, Rohrich RJ, Kenkel JM, Adams WP, Jr, Klein KW. Safety considerations and fluid resuscitation in liposuction: An analysis of 53 consecutive patients. Plast Reconstr Surg. 1998;102:2220–2229. doi: 10.1097/00006534-199811000-00063. [DOI] [PubMed] [Google Scholar]
- 31.Rohrich RJ, Leedy JE, Swamy R, Brown SA, Coleman J. Fluid resuscitation in liposuction: A retrospective review of 89 consecutive patients. Plast Reconstr Surg. 2006;117:431––435. doi: 10.1097/01.prs.0000201477.30002.ce. [DOI] [PubMed] [Google Scholar]
- 32.Matarasso A. Liposuction abdominoplasty: An evolving concept (Discussion). Plast Reconstr Surg. 2003;112:299––301. doi: 10.1097/01.PRS.0000066371.34978.F0. [DOI] [PubMed] [Google Scholar]


