Abstract
Background
There is controversy about the effect of Helicobacter pylori (H. pylori) eradication on the prevention of metachronous gastric cancer after endoscopic resection (ER).
Aims
The aim of this study was to systematically evaluate the effect of H. pylori eradication on the prevention of metachronous gastric lesions after ER of gastric neoplasms.
Methods
We performed a systematic search of PubMed, EMBASE, the Cochrane Library, and MEDLINE that encompassed studies through April 2014. Our meta-analysis consisted of 10 studies, which included 5881 patients who underwent ER of gastric neoplasms.
Results
When we compared the incidence of metachronous lesions between H. pylori-eradicated and non-eradicated groups, H. pylori eradication significantly lowered the risk of metachronous lesions after ER of gastric neoplasms (five studies, OR = 0.392, 95% CI 0.259 – 0.593, P < 0.001). When we compared H. pylori-eradicated and persistent groups, again, H. pylori eradication significantly lowered the incidence of metachronous lesions after ER of gastric neoplasms (six studies, OR = 0.468, 95% CI 0.326 – 0.673, P < 0.001). There was no obvious heterogeneity across the analyzed studies.
Conclusions
This meta-analysis suggests a preventive role for H. pylori eradication for metachronous gastric lesions after ER of gastric neoplasms. Thus, H. pylori eradication should be considered if H. pylori infection is confirmed during ER.
Introduction
The incidence of early gastric cancer (EGC) has been increasing as screening upper endoscopy has become widely available in Korea. The prognosis of EGC is quite favorable, with a 5 year survival rate > 95% [1]. Therefore, endoscopic resection (ER) has been a standard treatment for select cases of EGC in Korea. ER has many advantages, such as preservation of the stomach, quality of life, and reduced health costs. However, risk of metachronous gastric cancer in the remnant stomach after ER is higher than after gastrectomy [2]. The incidence of metachronous gastric cancer within 3–5 years after ER is 2.7–14.0% [3,4]. Therefore, scheduled endoscopic surveillance has been recommended to detect metachronous lesions after ER of EGC.
Helicobacter pylori (H. pylori) infection is closely related to progression to gastric dysplasia or cancer. In 1994, the International Agency for Research on Cancer (IARC), a subdivision of the World Health Organization (WHO), defined H. pylori as a group I carcinogen for gastric carcinoma [5]. However, the exact role of H. pylori infection in development of metachronous gastric lesions after ER has not been clearly elucidated. Fukase et al. reported that eradication of H. pylori after ER of EGC reduced the incidence of metachronous gastric cancer (odds ratio (OR) 0.353, 95% CI 0.161–0.775, P = 0.009), and recommended that prophylactic eradication should be pursued after ER [6]. However, Choi et al. showed that the incidence of metachronous cancer did not differ significantly between H. pylori-eradicated and control groups. This study enrolled 901 patients, who underwent ER for gastric dysplasia and cancer [7]. Thus, here lies the controversy about the effect of H. pylori eradication on prevention of metachronous gastric cancer after ER. Therefore, we aimed to systematically evaluate the effect of H. pylori eradication on prevention of metachronous gastric lesions after ER of gastric neoplasms.
Methods
Meta-analysis inclusion criteria
All relevant randomized controlled trials (RCTs) and retrospective cohort studies that compared the effects of H. pylori eradication on prevention of metachronous gastric lesions after ER of EGC were eligible for inclusion in our analysis.
Identification of appropriate studies
PubMed (1966 to April 2014), Cochrane Library (1997 to April 2014), MEDLINE (1966 to April 2014), and EMBASE (1985 to April 2014) databases were queried during our computer-aided search. Database searches used the following terms: Helicobacter pylori, H. pylori, metachronous, second, recur, gastric dysplasia, neoplasm, and gastric cancer. We also searched references manually in order to not miss relevant articles. Two reviewers (DH Jung and J-H Kim) searched the databases independently. The primary outcome measure was the incidence of metachronous gastric lesions after H. pylori eradication.
Study selection
Titles and abstracts were screened by two reviewers, and studies were chosen for meta-analysis if they were relevant. Language restrictions were not considered. If there was a disagreement, it was resolved by simultaneous review.
Data extraction and quality assessment
Reviewers used standardized data extraction forms. Extracted data included baseline patient and tumor characteristics, status of H. pylori infection and eradication, duration of follow-up, and primary outcome measures reported by the authors. All obtained data were compared in order to minimize error.
Measures of treatment effect
We compared the incidence of metachronous gastric neoplasms after ER of gastric neoplasms between H. pylori-eradicated and non-eradicated groups. We also compared the incidence of metachronous gastric neoplasms after ER of gastric neoplasms between H. pylori-eradicated and persistent groups. The results of each study were reported as a risk ratio (RR) between H. pylori-eradicated and non-eradicated or persistent groups, with a 95% confidence interval (CI).
Assessment of heterogeneity
Statistical heterogeneity among trials was assessed with χ2 and I 2 tests. The I 2 test measures the percentage of variability between studies caused by heterogeneity but not chance. As values from the I 2 test increase, heterogeneity increases. Data were pooled according to the fixed-effects and random-effects models.
Statistical analysis
The Begg’s funnel plot and Egger’s test were used to evaluate publication bias. P < 0.05 suggested a significant publication bias. Data was analyzed using CMA ver. 2.0 software (Comprehensive Meta-Analysis, Englewood, NJ, USA). Weights were assigned to individual studies based on the inverse of the variance. We used the PRISMA checklist (S1 PRISMA Checklist).
Results
Study inclusion
Our literature search yielded a total of 10 studies associated with H. pylori eradication and metachronous gastric lesions that were included in the final analysis. Fig 1 shows the search process that resulted in the final selection of eligible studies. Of the 1590 studies identified through our search strategy, 1575 studies were excluded after review of titles and abstracts. The 15 articles that were potentially relevant were reviewed carefully. Of these, three studies were excluded because they did not explore H. pylori [8–10], and one study was excluded due to an insufficient description of metachronous gastric cancer [11]. The last study was excluded because it focused on patients with dysplasia [12].
Fig 1. Flow chart for determining study inclusion.

.
Heterogeneity
There was no heterogeneity for the primary outcome between H. pylori-eradicated and non-eradicated or persistent groups. There was no significant heterogeneity between H. pylori-eradicated and non-eradicated groups (χ2 = 3.11, P = 0.539, and I 2 = 0). Similarly, there was no significant heterogeneity between H. pylori-eradicated and persistent groups (χ2 = 2.05, P = 0.842, and I 2 = 0).
Effect of H. pylori eradication on prevention of metachronous lesions after ER
Ten studies, which included 5881 patients, compared the effect of H. pylori eradication on prevention of metachronous lesions after ER of gastric neoplasm (Table 1). Among these, five studies compared the incidence of metachronous lesions between H. pylori-eradicated and non-eradicated groups [6,7,13–15]. Six studies compared the incidence of metachronous lesions between H. pylori-eradicated and persistent groups [14,16–20]. One study compared the incidence of metachronous lesions between H. pylori-eradicated and non-eradicated or persistent groups [14]. On the whole, compared with the H. pylori non-eradicated group, results showed that H. pylori eradication was significantly helpful in preventing metachronous lesions after ER of gastric neoplasms (OR = 0.392, 95% CI 0.259–0.593, P < 0.001) (Fig 2). When we compared H. pylori-eradicated and persistent groups, H. pylori eradication significantly lower the incidence of metachronous lesions after ER of gastric neoplasms (OR = 0.468, 95% CI 0.326–0.673, P < 0.001) (Fig 3). According to the Begg’s and Egger’s tests, there was no apparent publication bias on the effect of H. pylori eradication for prevention of metachronous lesions after ER between H. pylori-eradicated and non-eradicated or persistent groups (Egger’s test, P = 0.090 or 0.926, funnel plot, Fig 4).
Table 1. Characteristics of studies that evaluated the effect of Helicobacter. pylori eradication on the prevention of metachronous gastric lesions after endoscopic resection of gastric neoplasm.
| Study ID | Authors | Year | Ethnicity | Sample size (No receiving H. pylori eradication therapy) | Participant | Metachronous Recurrence | H. pylori Infection status (%) |
|---|---|---|---|---|---|---|---|
| 1 | Uemura et al.[15] | 1997 | Japanese | 132 (67) | EGC | EGC | 100 |
| 2 | Nakagawa et al.[13] | 2006 | Japanese | 2825 (2469) | EGC | EGC | 100 |
| 3 | Fukase et al.[6] | 2008 | Japanese | 505 (250) | EGC | EGC | 100 |
| 4 | Shiotani et al.[16] | 2008 | Japanese | 91 (0) | EGC | EGC | 91.0 |
| 5 | Maehata et al.[18] | 2012 | Japanese | 268 (0) | EGC | EGC | 100 |
| 6 | Choi et al.[7] | 2013 | Korean | 880 (441) | Gastric dysplasia or EGC | Gastric dysplasia or EGC | 100 |
| 7 | Seo et al.[17] | 2013 | Korean | 74 (0) | EGC | EGC | 100 |
| 8 | Kim et al.[14] | 2014 | Korean | 156 (88) | EGC | EGC | 41.7 |
| 9 | Bae et al.[19] | 2014 | Korean | 667 (N/A) | EGC | EGC | 66.2 |
| 10 | Kwon et al.[20] | 2014 | Korean | 283 (0) | EGC | Gastric dysplasia or EGC | 69.0 |
H. pylori, Helicobacter pylori
EGC, early gastric cancer
Fig 2. Forest plot showing comparisons for the effect of Helicobacter pylori eradication on metachronous gastric lesions after endoscopic resection between Helicobacter pylori-eradicated and non-eradicated groups.

Fig 3. Forest plot showing comparisons for the effect of Helicobacter pylori eradication on metachronous gastric lesions after endoscopic resection between Helicobacter pylori-eradicated and persistent groups.

Fig 4. Publication bias plot for the effect of Helicobacter pylori eradication on metachronous gastric lesions after endoscopic resection.
(A) comparison between Helicobacter pylori-eradicated and non-eradicated groups; (B) comparison between Helicobacter pylori-eradicated and persistent groups.
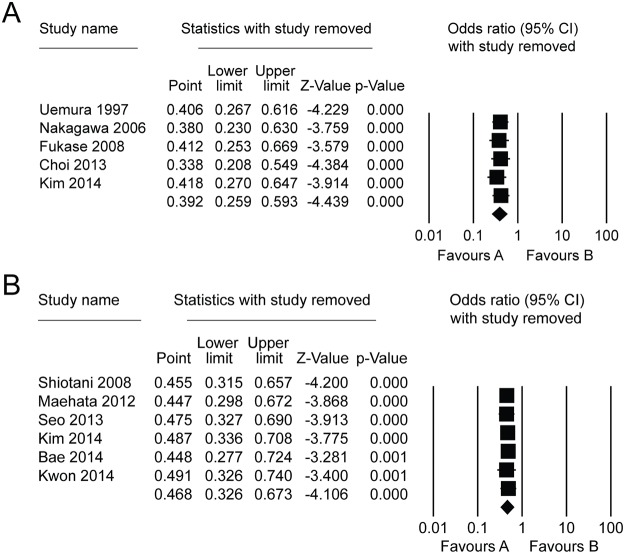
Sensitivity analysis
A sensitivity analysis showed that the results of our meta-analysis could not be obviously influenced by removing any one study (Fig 5).
Fig 5. Sensitive analysis for the effect of Helicobacter pylori eradication on metachronous gastric lesions after endoscopic resection.
(A) comparison between Helicobacter pylori-eradicated and non-eradicated groups; (B) comparison between Helicobacter pylori-eradicated and persistent groups.
Discussion
The effect of H. pylori eradication on the prevention of metachronous lesions after ER is still controversial. Thus, it may be useful to combine the results of similar published studies to arrive at a meaningful conclusion. As far as we know, this is the first meta-analysis to evaluate the association between H. pylori eradication and the incidence of metachronous lesions. Based on our findings, H. pylori eradication would be helpful for prevention of metachronous lesions after ER.
Nowadays, ER is widely used for local treatment of a gastric neoplasm. In Korea, the number of patients who have undergone ER for gastric neoplasm has increased annually because of the popularity of screening endoscopy [21]. The H. pylori infection rate in patients undergoing ER varies widely: 41.7–91.0% [14,16,19]. Our analysis suggests a preventive effect of H. pylori eradication since H. pylori eradication lowered the incidence of metachronous lesions after ER (OR = 0.392, 95% CI 0.259–0.593, P < 0.001). However, patients persistently infected after receiving H. pylori treatment were included in these groups. The study by Choi et al. showed the eradication rate of H. pylori after ER of gastric neoplasms [7]. Persistent H. pylori infection was found in 80 of 439 (18.2%) patients who received H. pylori treatment and in 373 of 441 (84.6%) patients who did not receive H. pylori treatment. We compared the effect of H. pylori treatment between H. pylori-eradicated and persistent groups. Successful H. pylori eradication was associated with a significant decrease in the incidence of metachronous lesions after ER (OR = 0.468, 95% CI 0.326–0.673, P < 0.001). This means that H. pylori eradication has a protective effect for the development of metachronous lesions. And, successful eradication of H. pylori is very important for the prevention of metachronous lesions after ER of a gastric neoplasm.
A large, prospective, randomized study in China reported that the incidence of gastric cancer was similar between patients receiving H. pylori eradication treatment and those receiving placebo. Subgroup analysis revealed that H. pylori eradication significantly inhibited development of gastric cancer in patients without a precancerous lesion [22]. However, several reports have shown that H. pylori eradication decreases the incidence of gastric cancer in high-risk patients as well [23,24]. Bae et al. reported that H. pylori eradication prevents development of metachronous lesions despite the presence of severe atrophy and intestinal metaplasia (IM) in the mucosal background [19].
Metachronous gastric cancer can develop after ER. Therefore, evaluating the risk factors associated with metachronous gastric cancer is important. Kwon et al. showed that old age and persistent H. pylori infection were independently significant risk factors for development of metachronous gastric cancer after ER of EGC [20]. Hanaoka et al. reported that extensive atrophic fundic gastritis diagnosed by autofluorescence imaging is a significant predictor for development of metachronous gastric cancer after H. pylori eradication [25]. According to Correa’s hypothesis, atrophic gastritis and IM caused by H. pylori infection are closely associated with the development of gastric cancer [26]. A meta-analysis of 12 studies inferred that H. pylori eradication significantly improved atrophic gastritis [27]. We cannot interrupt age-related atrophic changes in gastric mucosa. Thus, H. pylori eradication may be a very effective intervention strategy for promoting regression of metachronous lesions after ER.
Metachronous gastric cancers are found more frequently in patients following ER than in the gastrectomized stomach. It is caused naturally by the remnant stomach, which is preserved after ER. In addition, the surrounding non-tumorous mucosa may be at high risk of developing metachronous gastric lesions because it used to share the environment with gastric cancer [28]. Therefore, eradication of H. pylori should be recommended to promote regression of background mucosa in patients after ER of a gastric neoplasm.
Our study has some limitations. First, the ethnicity of study participants included in this meta-analysis was Korean and Japanese. The incidence of gastric cancer and H. pylori infection in Eastern Asia is higher than in other areas of the world. And, ER of gastric neoplasm is performed routinely in Korea and Japan [29–31]. Therefore, reports of an association between H. pylori eradication and metachronous recurrence after ER might be published mostly in Korea and Japan.
Secondly, our results did not segregate dysplasia and cancer. However, dysplasia was a pre-cancerous lesion as Correa’s hypothesis [26]. Therefore, to elucidate the effect of H. pylori eradication on prevention of metachronous lesions after ER is significant in patients with dysplasia or cancer.
In conclusion, the incidence of metachronous gastric cancer was higher in patients with persistent H. pylori infection than in those whose H. pylori infection was eradicated. And, eradication of H. pylori was helpful in decreasing the development of metachronous gastric cancer. Thus, eradication of H. pylori should be recommended if H. pylori infection is confirmed after ER.
Supporting Information
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1. Soetikno R, Kaltenbach T, Yeh R, Gotoda T. Endoscopic mucosal resection for early cancers of the upper gastrointestinal tract. J Clin Oncol. 2005;23: 4490–4498. [DOI] [PubMed] [Google Scholar]
- 2. Choi KS, Jung HY, Choi KD, Lee GH, Song HJ, Kim do H, et al. EMR versus gastrectomy for intramucosal gastric cancer: comparison of long-term outcomes. Gastrointest Endosc. 2011;73: 942–948. 10.1016/j.gie.2010.12.032 [DOI] [PubMed] [Google Scholar]
- 3. Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, et al. Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut. 2009;58: 331–336. 10.1136/gut.2008.165381 [DOI] [PubMed] [Google Scholar]
- 4. Nasu J, Doi T, Endo H, Nishina T, Hirasaki S, Hyodo I. Characteristics of metachronous multiple early gastric cancers after endoscopic mucosal resection. Endoscopy. 2005;37: 990–993. [DOI] [PubMed] [Google Scholar]
- 5. Schistosomes, liver flukes and Helicobacter pylori. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 7–14 June 1994. IARC Monogr Eval Carcinog Risks Hum. 1994;61: 1–241. [PMC free article] [PubMed] [Google Scholar]
- 6. Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet. 2008;372: 392–397. 10.1016/S0140-6736(08)61159-9 [DOI] [PubMed] [Google Scholar]
- 7. Choi J, Kim SG, Yoon H, Im JP, Kim JS, Kim WH, et al. Eradication of Helicobacter pylori After Endoscopic Resection of Gastric Tumors Does Not Reduce Incidence of Metachronous Gastric Carcinoma. Clin Gastroenterol Hepatol. 2013. 10.1016/j.cgh.2013.09.057 [DOI] [PubMed] [Google Scholar]
- 8. Seo JH, Park JC, Kim YJ, Shin SK, Lee YC, Lee SK. Undifferentiated Histology after Endoscopic Resection May Predict Synchronous and Metachronous Occurrence of Early Gastric Cancer. Digestion. 2010;81: 35–42. 10.1159/000235921 [DOI] [PubMed] [Google Scholar]
- 9. Boda T, Ito M, Yoshihara M, Kitamura Y, Matsuo T, Oka S, et al. Advanced method for evaluation of gastric cancer risk by serum markers: determination of true low-risk subjects for gastric neoplasm. Helicobacter. 2014;19: 1–8. 10.1111/hel.12165 [DOI] [PubMed] [Google Scholar]
- 10. Kato M, Asaka M, Ono S, Nakagawa M, Nakagawa S, Shimizu Y, et al. Eradication of Helicobacter pylori for primary gastric cancer and secondary gastric cancer after endoscopic mucosal resection. J Gastroenterol. 2007;42 Suppl 17: 16–20. [DOI] [PubMed] [Google Scholar]
- 11. Kikuchi S, Kato M, Katsuyama T, Tominaga S, Asaka M. Design and planned analyses of an ongoing randomized trial assessing the preventive effect of Helicobacter pylori eradication on occurrence of new gastric carcinomas after endoscopic resection. Helicobacter. 2006;11: 147–151. [DOI] [PubMed] [Google Scholar]
- 12. Chon I, Choi C, Shin CM, Park YS, Kim N, Lee DH. Effect of Helicobacter pylori eradication on subsequent dysplasia development after endoscopic resection of gastric dysplasia. Korean J Gastroenterol. 2013;61: 307–312. [DOI] [PubMed] [Google Scholar]
- 13. Nakagawa S, Asaka M, Kato M, Nakamura T, Kato C, Fujioka T, et al. Helicobacter pylori eradication and metachronous gastric cancer after endoscopic mucosal resection of early gastric cancer. Alimentary Pharmacology & Therapeutics. 2006;24: 214–218. [Google Scholar]
- 14. Kim YI, Choi IJ, Kook MC, Cho SJ, Lee JY, Kim CG, et al. The association between Helicobacter pylori status and incidence of metachronous gastric cancer after endoscopic resection of early gastric cancer. Helicobacter. 2014;19: 194–201. 10.1111/hel.12116 [DOI] [PubMed] [Google Scholar]
- 15. Uemura N, Mukai T, Okamoto S, Yamaguchi S, Mashiba H, Taniyama K, et al. Effect of Helicobacter pylori eradication on subsequent development of cancer after endoscopic resection of early gastric cancer. Cancer Epidemiol Biomarkers Prev. 1997;6: 639–642. [PubMed] [Google Scholar]
- 16. Shiotani A, Uedo N, Iishi H, Yoshiyuki Y, Ishii M, Manabe N, et al. Predictive factors for metachronous gastric cancer in high-risk patients after successful Helicobacter pylori eradication. Digestion. 2008;78: 113–119. 10.1159/000173719 [DOI] [PubMed] [Google Scholar]
- 17. Seo JY, Lee DH, Cho Y, Oh HS, Jo HJ, Shin CM, et al. Eradication of Helicobacter pylori reduces metachronous gastric cancer after endoscopic resection of early gastric cancer. Hepatogastroenterology. 2013;60: 776–780. 10.5754/hge12929 [DOI] [PubMed] [Google Scholar]
- 18. Maehata Y, Nakamura S, Fujisawa K, Esaki M, Moriyama T, Asano K, et al. Long-term effect of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic resection of early gastric cancer. Gastrointest Endosc. 2012;75: 39–46. 10.1016/j.gie.2011.08.030 [DOI] [PubMed] [Google Scholar]
- 19. Bae SE, Jung HY, Kang J, Park YS, Baek S, Jung JH, et al. Effect of Helicobacter pylori eradication on metachronous recurrence after endoscopic resection of gastric neoplasm. Am J Gastroenterol. 2014;109: 60–67. 10.1038/ajg.2013.404 [DOI] [PubMed] [Google Scholar]
- 20. Kwon YH, Heo J, Lee HS, Cho CM, Jeon SW. Failure of Helicobacter pylori eradication and age are independent risk factors for recurrent neoplasia after endoscopic resection of early gastric cancer in 283 patients. Aliment Pharmacol Ther. 2014;39: 609–618. 10.1111/apt.12633 [DOI] [PubMed] [Google Scholar]
- 21. Kang KJ, Lee JH. Characteristics of Gastric Cancer in Korea—with an Emphasis on the Increase of the Early Gastric Cancer (EGC). Journal of the Korean Medical Association. 2010;53: 283–289. [Google Scholar]
- 22. Wong BC, Lam SK, Wong WM, Chen JS, Zheng TT, Feng RE, et al. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004;291: 187–194. [DOI] [PubMed] [Google Scholar]
- 23. Take S, Mizuno M, Ishiki K, Nagahara Y, Yoshida T, Yokota K, et al. The effect of eradicating helicobacter pylori on the development of gastric cancer in patients with peptic ulcer disease. Am J Gastroenterol. 2005;100: 1037–1042. [DOI] [PubMed] [Google Scholar]
- 24. Takenaka R, Okada H, Kato J, Makidono C, Hori S, Kawahara Y, et al. Helicobacter pylori eradication reduced the incidence of gastric cancer, especially of the intestinal type. Aliment Pharmacol Ther. 2007;25: 805–812. [DOI] [PubMed] [Google Scholar]
- 25. Hanaoka N, Uedo N, Shiotani A, Inoue T, Takeuchi Y, Higashino K, et al. Autofluorescence imaging for predicting development of metachronous gastric cancer after Helicobacter pylori eradication. J Gastroenterol Hepatol. 2010;25: 1844–1849. 10.1111/j.1440-1746.2010.06442.x [DOI] [PubMed] [Google Scholar]
- 26. Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988;48: 3554–3560. [PubMed] [Google Scholar]
- 27. Wang J, Xu LJ, Shi RH, Huang XY, Li SWH, Huang ZH, et al. Gastric Atrophy and Intestinal Metaplasia before and after Helicobacter pylori Eradication: A Meta-Analysis. Digestion. 2011;83: 253–260. 10.1159/000280318 [DOI] [PubMed] [Google Scholar]
- 28. Bornschein J, Toth K, Selgrad M, Kuester D, Wex T, Molnar B, et al. Dysregulation of CDX1, CDX2 and SOX2 in patients with gastric cancer also affects the non-malignant mucosa. Journal of Clinical Pathology. 2013;66: 819–822. 10.1136/jclinpath-2013-201448 [DOI] [PubMed] [Google Scholar]
- 29. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61: 69–90. 10.3322/caac.20107 [DOI] [PubMed] [Google Scholar]
- 30. Lee SY. Current progress toward eradicating Helicobacter pylori in East Asian countries: Differences in the 2013 revised guidelines between China, Japan, and South Korea. World Journal of Gastroenterology. 2014;20: 1493–1502. 10.3748/wjg.v20.i6.1493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kim MY, Cho JH, Jain P, Cho JY. ESD around the world: Asia. Gastrointest Endosc Clin N Am. 2014;24: 283–293. 10.1016/j.giec.2013.11.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.