Abstract
Background
HIV patients on antiretroviral therapy have shown elevated incidence of dyslipidemia, lipodystrophy, and cardiovascular disease (CVD). Most studies, however, focus on cohorts from developed countries, with less data available for these co-morbidities in Ethiopia and sub-Saharan Africa.
Methods
Adult HIV-negative (n = 36), treatment naïve (n = 51), efavirenz (EFV)-treated (n = 91), nevirapine (NVP)-treated (n = 95), or ritonavir-boosted lopinavir (LPV/r)-treated (n=44) subjects were recruited from Black Lion Hospital in Addis Ababa, Ethiopia. Aortic pressure, augmentation pressure, and pulse wave velocity (PWV) were measured via applanation tonometry and carotid intima-media thickness (cIMT) and carotid arterial stiffness, and brachial artery flow-mediated dilation (FMD) were measured via non-invasive ultrasound. Body mass index, waist-to-hip circumference ratio (WHR), skinfold thickness, and self-reported fat redistribution were used to quantify lipodystrophy. CD4+ cell count, plasma HIV RNA levels, fasting glucose, total-, HDL-, and LDL-cholesterol, triglycerides, hsCRP, sVCAM-1, sICAM-1, leptin and complete blood count were measured.
Results
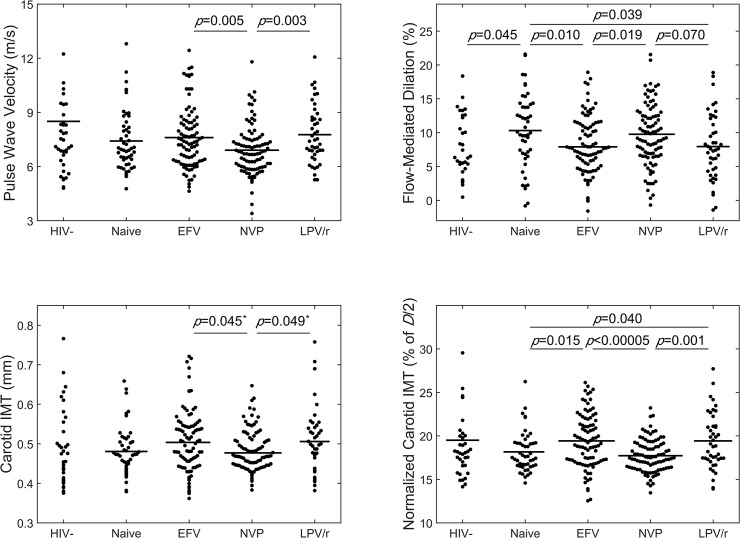
PWV and normalized cIMT were elevate and FMD impaired in EFV- and LPV/r-treated subjects compared to NVP-treated subjects; normalized cIMT was also elevated and FMD impaired in the EFV- and LPV/r-treated subjects compared to treatment-naïve subjects. cIMT was not statistically different across groups. Treated subjects exhibited elevated markers of dyslipidemia, inflammation, and lipodystrophy. PWV was associated with age, current EFV and LPV/r used, heart rate, blood pressure, triglycerides, LDL, and hsCRP, FMD with age, HIV duration, WHR, and glucose, and cIMT with age, current EFV use, skinfold thickness, and blood pressure.
Conclusions
Current EFV- or LPV/r-treatment, but not NVP-treatment, correlated with elevated markers of atherosclerosis, which may involve mechanisms distinct from traditional risk factors.
Background
People living with HIV taking highly active antiretroviral therapy (HAART) have shown elevated incidence of dyslipidemia, lipodystrophy, insulin resistance, diabetes mellitus, and cardiovascular disease (CVD)[1]; the latter includes higher prevalence of myocardial infarction [2,3] and atherosclerotic lesions [4], as well as elevated preclinical markers atherosclerosis including increased arterial stiffness [5,6] and carotid artery intima-media thickness (cIMT) [6,7], and impaired flow-mediated dilation (FMD) [8]. Of the five classes of antiretroviral drugs, protease inhibitors (PI) are the most widely implicated drug class in early on-set CVD, but nucleoside reverse transcriptase inhibitors (NRTI’s) and non-NRTI’s (NNRTI’s) have also been implicated [3,9–11].
A pressing need remains to better quantify non-AIDS related co-morbidities in people living with HIV in sub-Saharan Africa. Most studies of cardiovascular co-morbidities with HIV represent populations from developed countries; yet, 69% of all people living with HIV reside in sub-Saharan Africa [12]. Antiretroviral programs in Africa have made a tremendous impact in reducing HIV-related deaths and have been available in Ethiopia since 2005; the treatment disparities, however, between the developing world and the developed world remain great. People living with HIV in the developing world have access to fewer combinations of HAART regimens and patient adherence and clinical monitoring of CD4+ cell counts and viral loads in the developing world is well below that in the developed countries. As a result, people living with HIV in developing nations remain on first line therapy with less follow up. These treatment disparities, combined with differences in demographics, lifestyle, and nutritional status between Ethiopian and Western populations, may make this population more susceptible to non-AIDS related co-morbidities.
This paper reports a cross-sectional study to assess preclinical markers of atherosclerosis, lipodystrophy, dyslipidemia, and systemic inflammation with HIV infection and HAART in Addis Ababa, Ethiopia. We hypothesize that current efavirenz (EFV)- or ritonavir-boosted lopinavir (LPV/r)-treatment will correlate with increased arterial stiffness and cIMT and impaired FMD compared to current nevirapine (NVP)-treatment and no HAART-treatment, and that these preclinical markers will be associated with markers of lipodystrophy and inflammation.
Materials and Methods
Participant Enrollment and Baseline Data
All work was performed in accordance with the Declaration of Helsinki. All participants provided written informed consent and this study was approved by the Institutional Review Board Committees at Addis Ababa University and Georgia Institute of Technology. Eighteen- to 65-year-old HIV-negative, HIV-positive HAART naïve, and HIV-positive subjects on EFV-, NVP-, or LPV/r-containing regimens for at least two months prior to the exam were recruited from Tikur Anbessa (Black Lion) Specialized Referral Hospital in Addis Ababa, Ethiopia to participate in this study. Subjects were excluded if they had active AIDS defining illnesses or diabetes mellitus. Subjects fasted and refrained from tobacco products for at least 8 hours prior to the test and refrained from exercise in the morning of the test.
Participant age, sex, HIV-serostatus, date of first HIV-seropositive test, initial CD4+ cell count, last CD4+ cell count, and any viral load determinations, and date of initiation of current and all previous HAART regimens were obtained from the participants hospital card. Questionnaire-driven interviews were performed by the local recruiting nurse at the Black Lion Hospital HIV clinic under the direction of the research team. Self-reported personal and familial (mother, father, brothers, or sisters) history of heart attack, angina, stroke, kidney disease, diabetes, or lipid disorders and self-reported alcohol and cigarette use were recorded.
Body Composition
Body weight, body height, waist and hip circumference, and skinfold thickness (bicep, tricep, suprailiac, and sub scapula) were measured. Skinfold measurements were taken in duplicate on the right and left sides and reported as the average of these four values. The ratio of the sum of skin-fold measurements in the suprailiac and sub-scapula divided by the sum of those from the bicep and tricep was reported as the Trunk/arm ratio. Subjects were asked if they observed an ‘increase in fat’, ‘decrease in fat’, or ‘no change’ at each of the following locations: face, arms, legs, abdomen, chest, cervical fat pad, supraclavicular fat, and across their entire body.
Blood Pressure, Pulse Wave Analysis, and Pulse Wave Velocity
Brachial artery systolic (B-SBP) and diastolic (B-DBP) blood pressure were measured with a digital automatic blood pressure measurement device after the subjects rested in a supine position for at least 10 minutes. Pulse wave analysis (PWA) and pulse wave velocity (PWV) measurements were subsequently taken with a SphygmoCor CPV Clinical System (AtCor Medical) following manufacturer protocol. PWA and PWV measurements meeting the manufacturer quality control criteria were collected in triplicate and averaged.
Carotid intima-media thickness (cIMT)
Ultrasound measurements were collected using a Sonocyte Micromax portable ultrasound device with vascular software for two-dimensional imaging, color and spectral Doppler, high- frequency (10 MHz) linear transducer, and internal electrocardiogram monitor. The right and left common carotid arteries (CCA) were examined with the head in the midline position tilted slightly upward and away from the artery being imaged. The probe was placed so that the near and far walls were parallel in the acquired image and lumen diameter was maximized in the longitudinal plane. Three 6-second clips of each artery were collected and stored for analysis. cIMT was reported in systole and diastole as the average of the near and far wall measurements from three separate clips from both the right and left CCA. In addition, given that clinically relevant differences in cIMT are on the order of microns and typical standard deviations observed across broad ranges of age and both sexes can be on the order of microns, mainly due to subject-to-subject variability in the carotid artery size, a normalized measure was defined as cIMTnorm = cIMT/(D/2), where D was the measured inner diameter of the CCA. It should be noted that this normalized value of cIMT is not been shown to be associated with cardiovascular risk; however, this measure allows for the normalization of data across a broad range of common carotid artery size.
The linearized cyclic strain Δε = ΔD/D, was also reported, where ΔD is the difference between the systolic and diastolic luminal diameter and D is the diastolic luminal diameter. The Peterson’s modulus (E p), a common measure of arterial stiffness, defined as E p = PP/Δε = 1/C, where PP is the pulse pressure and C is the compliance, was reported. The medial hoop stress approximated as σθ = P(D/2)/(cIMT) = P/cIMTnorm, was also reported. P and PP in the carotid artery were approximated by the values determined for the aorta via PWA. A single analyst, blinded to the patients HIV status and HAART regimen, analyzed all images.
Flow-mediated dilation
An appropriately sized sphygmomanometer was placed on the widest part of the proximal right forearm ~1 cm distal to the antecubital fossa. Prior to inflation, three 6-second clips of the brachial artery image and EKG tracings were stored for baseline measurements. The sphygmomanometer was inflated at least 50 mmHg above the subjects’ systolic blood pressure. Five minutes after occlusion, the cuff was deflated and a 6-second clip of the brachial artery image and EKG tracing was stored at 30, 45, 60, 75, and 90 seconds after deflation. A single analyst, blinded to the patients HIV status and HAART regimen, analyzed all images. Further, FMD = (D t—D B)/D B, where D t is the brachial artery inner diameter during diastole at the time-point of interest and D B is the average of the three measurements of the brachial artery diameter during diastole at baseline.
Blood Sample Analysis
Complete blood count, total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL), low-density lipoprotein cholesterol (LDL), and glucose analysis were performed at the clinical laboratory at Black Lion Hospital. CD4+ cell count and plasma HIV RNA analysis was performed at the International Clinical Laboratory (Addis Ababa, Ethiopia). High-sensitivity C-reactive protein (hsCRP), soluble vascular cell adhesion molecule-1 (sVCAM-1) and intercellular adhesion molecule-1 (sICAM-1), and leptin analyses were performed on blood serum using commercially available ELISA kits (Life Technologies Corporation). Analysis for HIV viral load was performed on 70%, hsCRP on 80%, sVCAM-1 on 85%, sICAM-1 on 80%, and leptin on 80% of the subject pool, equally distributed among groups.
Statistical Analysis
All statistical analyses were performed using MATLAB© (MathWorks). A one-way analysis of variance (ANOVA) was performed to determine statistical significance across groups (p < 0.05) on continuous variables that satisfied Bartlett's test for equal variances and Pearson Chi-square test for normality of residuals; a Kruskal-Wallis non-parametric one-way ANOVA was performed on continuous variables that did not show equal variances or normality. For continuous variables with significance across groups, a pairwise Wilcoxon rank sum test was performed to detect differences between individual groups (p < 0.05). For categorical variables, χ2 analysis was performed to determine statistical significance across groups (p < 0.05); for those with significance across groups, a pairwise Marascuillo procedure was performed to compare differences in proportions between individual groups (p < 0.05).
Correlation analysis was performed and multivariable linear regression models were constructed to examine the association of study parameters with PWV for all HAART treated subjects. Relevant study parameters were selected for the inclusion of the initial models and the stepwisefit multivariable regression MATLAB subroutine, which eliminates (or adds) covariates in a stepwise fashion, was used with the criteria p<0.05 for removal from (or inclusion in) the final model.
Results
Participant Characteristics
CD4+ cell count was lower in all HIV-positive groups, compared to HIV-negative subjects, and lower in LPV/r-treated, compared to NVP-treated subjects (Table 1). Plasma HIV RNA levels were lower and percentages of subjects with plasma HIV RNA levels below detectable limits (<40 copies/mL) were higher in all HAART-treated groups, compared to HAART-naïve subjects. Years since first HIV diagnosis was higher in HAART-treated groups compared to HAART-naïve and in NVP- and LPV/r-treated compared to EFV-treated subjects. LPV/r-treated subjects were on HAART longer than EFV-treated subjects. EFV-treated subjects have been on their current regimen longer than LPV/r-treated, but shorter than NVP-subjects. The HAART treated groups had similar distributions of NRTI-backbone, with the exceptions that less LPV/r-treated subjects had an AZT-3TC backbone compared to NVP-treated subjects and more LPV/r-treated subjects had an NRTI-backbone other than AZT-3TC or TDF-3TC compared to EFV-treated subjects. The ‘Other’ NRTI backbones included stavudine in the NNRTI groups and didanosine, abacavir, or stavudine in the LPV/r group. More LPV/r-treated subjects had taken a previous regimen, which was expected, as LPV/r is considered a ‘second-line’ regimen. See S1 File for additional participant characteristics; namely, cigarette smoking, personal and family history of heart attack, angina, or stroke, kidney disease, diabetes, or lipid disorders, and complete blood count results.
Table 1. Baseline characteristics, body composition.
| End-point | HIV-Negative | HAART Naïve | Efavirenz (EFV) | Nevarapine (NVP) | Lopinavir/r (LPV/r) |
|---|---|---|---|---|---|
| (n=36) | (n=51) | (n=91) | (n=95) | (n=44) | |
| Demographics | |||||
| Age (yrs) | 39(29-45) | 38(32-45) | 38(34-45) | 37(32-42) | 39(35-44) |
| Male ratio [# (%)] | 8 (22%) | 14(27%) | 23 (25%) | 21(22%) | 14 (32%) |
| HIV / HAART History | |||||
| CD4+ count | 730(656-1047) | 395(182-546)A | 349(232-481)A | 390(271-534)A | 285(147-453)A,e |
| Viral Load (log10copies/mL) | -- | 3.6(2.2-4.7) | <1.6(<1.6-<1.6)B | <1.6(<1.6-<1.6)B | <1.6(<1.6-<1.6)B |
| Viral Load (% BDL) | -- | 18% | 92%B | 87% B | 81% B |
| Yrs since diagnosis | -- | 1.6(0.3-3.7) | 5.7(3.4-7.0)B | 6.0(5.6-7.4)B,d | 6.5(5.3-8.3)B,d |
| Yrs on HAART | -- | -- | 5.0(3.2-6.2) | 5.7(3.9-6.2) | 5.9(4.2-6.8)d |
| Yrs on Current Regimen | -- | -- | 2.5(1.5-4.4) | 3.8(1.9-5.7)d | 1.8(0.7-3.2)E |
| Current NRTI backbone | |||||
| TDF+3TC [# (%)] | -- | -- | 55(60%) | 38(40%) | 28(64%) |
| AZT+3TC [# (%)] | -- | -- | 35(38%) | 53(56%) | 7(16%)E |
| Other [# (%)] | -- | -- | 1(1%) | 4(4%)e | 9(20%) |
| Previous Regimen | |||||
| All [# (%)] | -- | -- | 39(43%) | 29(31%) | 40(91%)D,E |
| EFV-containing [# (%)] | -- | -- | 24(26%) | 5(5%) | 20(45%)d,e |
| NVP-containing [# (%)] | -- | -- | 15(16%) | 24(25%) | 22(50%)d,e |
| Body Composition | |||||
| BMI [kg/m2] | 22(20-26) | 22(20-26) | 21(19-24) | 23(20-25) | 22(18-25) |
| WHR [ ] | 0.82(0.77-0.86) | 0.84(0.79-0.89) | 0.86(0.81-0.91)A | 0.86(0.81-0.92)A | 0.88(0.82-1)A,b |
| Skinfold Thickness | |||||
| Tricep [mm] | 12.2(7.6-15.3) | 10.8(5.4-14.9)A | 6.7(3.9-9.5)A,B | 6.7(4.2-10.0)A,b | 8.0(5.2-10.6)A |
| Bicep [mm] | 6.1(3.3-8.8) | 6.2(3.1-9.2) | 3.1(2.4-5.8)A,B | 3.5(2.4-6.0)A,B | 4.4(2.7-8.1) |
| Suprailiac [mm] | 9.3(6.4-13.7) | 7.9(5.0-13.1) | 6.2(4.0-8.9)A,b | 7.4(4.3-10.9)A | 7.7(4.0-12.4) |
| Sub-scapula [mm] | 20.9(16.0-27.1) | 19.8(11.7-28.4) | 15.8(9.9-20.7)a,b | 18.4(11.2-28.2)d | 20.2(9.8-30.4)d |
| Trunk:arm [ ] | 1.6(1.4-2.0) | 1.8(1.4-2.2) | 2.1(1.4-2.8)a,b | 2.2(1.5-3.3)a,b | 2.1(1.5-2.6)a,b |
| Observed change in fat (% observing decrease in fat / % observing increase in fat | |||||
| Face [%] | 0%/0% | 8%/4% | 27%A,b/5% | 15%A/23% A,b,d | 36%A,b/11% |
| Arms [%] | 0%/0% | 4%/4% | 16%A/4% | 8%/13% A | 23%A/7% |
| Legs [%] | 0%/0% | 6%/2% | 22%A/5% | 17%A/20% A,b | 25%/7% |
| Abdomen [%] | 0%/0% | 4%/6% | 1%/32% A,B | 1%/29% A,B | 2%/41% A,B |
| Chest [%] | 0%/0% | 4%/0% | 2%/11% a,b | 1%/9% a,b | 0%/25% a,b |
| Buffalo hump [%] | 0%/0% | 4%/0% | 1%/7% | 0%/9% a,b | 2%/14% |
| Neck [%] | 0%/0% | 4%/0% | 3%/5% | 0%/8% | 2%/16% |
| Body [%] | 0%/8% | 20% a /14% | 14%A/32% a | 13%a/42% A,B | 16%/36% |
Continuous variables are reported as median (interquartile range). BMI = body mass index, and WHR = waist-to-hip ratio, mm = millimeters.
A, a = p<0.005 or p<0.05 versus HIV-negative controls, respectively;
B, b = p<0.005 or p<0.05 versus HAART-naive, respectively;
D, d = p<0.005 or p<0.05 versus EFV, respectively;
E, e = p<0.005 or p<0.05 versus NVP, respectively.
Body Composition and Anthropometric Measurements
No differences were observed in BMI across groups. WHR was elevated in all HAART-treated groups, compared to HIV-negative subjects and in the LPV/r-treated subjects compared to HAART-naïve subjects. Skin-fold thickness measurements yielded multiple differences between HAART treated versus HIV-negative and HAART-naïve subjects. Trunk/Arm skin-fold thickness ratio was significantly higher in all HAART-treated subjects compared to HIV-negative and HAART-naïve subjects. The self-reported fat redistribution followed these trends, with HAART-treated subjects generally reporting decreased fat in their face, arms, and legs, increased fat in the chest, buffalo hump, and neck and increased overall body fat. A significant fraction of NVP-treated subjects also reported increased fat in their face, arms, and legs. Taken together, WHR, skin-fold thickness measurements, and self-reported observations show that HAART-treated subjects in Addis Ababa, Ethiopia exhibit lipodystrophy.
Blood Pressure, Pulse Wave Analysis, and Pulse Wave Velocity
The B-SBP was lower in EFV-treated compared to NVP-treated subjects and brachial artery pulse pressure (PP) was lower in EFV-treated compared to NVP- and LPV/r-treated subjects (Table 2). Pulse wave analysis predicted that the aortic PP was higher in the NVP- and LPV/r-treated compared to the HAART-naïve and EFV-treated subjects; aortic PP was higher in HIV-negative compared to HAART-naïve subjects. PWV was significantly lower in NVP-treated compared to EFV-treated and LPV/r-treated subjects, indicating arterial stiffening of the central vasculature (Fig 1).
Table 2. Cardiovascular metrics.
| End-point | HIV-Negative | HAART Naïve | Efavirenz (EFV) | Nevarapine (NVP) | Lopinavir/r (LPV/r) |
|---|---|---|---|---|---|
| (n=36) | (n=51) | (n=91) | (n=95) | (n=44) | |
| Cardiovascular Metrics | |||||
| Heart Rate | 66(64-74) | 72(65-79) | 70(65-78) | 71(65-78) | 69(63-73) |
| Blood Pressure | |||||
| Brachial SBP [mmHg] | 120(112-132) | 112(108-123) | 112(104-123)a | 117(107-130)d | 119(105-131) |
| Brachial DBP [mmHg] | 73(68-81) | 70(66-79) | 71(63-78) | 72(67-82) | 70(66-79) |
| Brachial MP [mmHg] | 90(83-99) | 85(82-95) | 86(78-95) | 89(82-99) | 90(80-101) |
| Brachial PP [mmHg] | 46(40-54) | 43(37-49) | 42(38-46)a | 45(39-52)d | 45(38-56)d |
| Pulse Wave Analysis | |||||
| Aortic SBP [mmHg] | 110(101-121) | 103(98-114) | 103(96-113) | 109(98-122) | 112(97-123) |
| Aortic DBP [mmHg] | 75(69-82) | 71(67-81) | 72(64-79) | 73(68-83) | 71(67-81) |
| Aortic MP [mmHg] | 90(83-98) | 85(82-95) | 86(78-95) | 89(82-99) | 90(80-101) |
| Aortic PP [mmHg] | 34(30-42) | 32(26-38) | 31(28-36)a | 34(29-42)b,d | 34(31-47)b,d |
| AP [mmHg] | 8(5-13) | 8(6-14) | 8(5-11) | 10(6-14) | 10(6-16) |
| Aix | 27(15-34) | 25(20-35) | 26(20-33) | 27(20-35) | 28(21-38) |
| AIx-75 | 26(12-33) | 25(19-35) | 26(17-32) | 27(19-33) | 28(19-34) |
| Pulse Wave Velocity [m/s] | 7.1(6.3-8.4) | 7.0(6.3-8.2) | 7.4(6.3-8.4) | 6.8(6.0-7.5)D | 7.4(6.8-8.7)E |
| Baseline Diameter [mm] | 3.04(2.83-3.40) | 2.87(2.63-3.19) | 2.98(2.75-3.26) | 3.07(2.81-3.41) | 2.88(2.69-2.69) |
| Dilated Diameter [mm] | 3.29(3.07-3.56) | 3.22(2.94-2.94) | 3.22(2.99-3.51) | 3.33(3.07-3.76) | 3.20(2.91-2.91) |
| FMD [%] | 6.5(5.0-12.4) | 10.0(7.0-13.9)a | 7.7(4.8-11.2)b | 9.2(6.6-12.5)d | 7.6(4.5-12.2)b |
| Common Carotid Artery | |||||
| Diameter [mm] | 5.17(4.94-5.52) | 5.27(5.02-5.58) | 5.16(4.92-5.51) | 5.42(5.08-5.69)D | 5.21(4.90-5.49)e |
| c-IMT [mm] | 0.47(0.41-0.54) | 0.47(0.44-0.51) | 0.50(0.44-0.54) | 0.47(0.44-0.51) | 0.50(0.46-0.54) |
| c-IMT norm [%] | 18.0(16.4-19.8) | 17.6(16.6-19.3) | 19.2(17.2-21.7)b | 17.5(16.3-18.9)D | 19.0(17.4-21.1)b,E |
| Medial stress [kPa] | 55(49-60) | 55(49-61) | 50(45-58)a,b | 57(52-62)D | 51(43-59)e |
| Properties | |||||
| Modulus [kPa] | 57(42-81) | 50(43-74) | 52(43-66) | 55(47-70) | 61(51-75) |
| Compliance [MPa-1] | 20(12-24) | 20(14-24) | 19(15-23) | 18(14-22) | 17(14-20) |
| Cyclic strain [ ] | 8.3(7.4-9.8) | 7.5(6.7-9.2) | 8.0(6.8-9.5) | 8.4(7.0-10.2) | 8.8(6.9-9.7) |
| Blood Sample Analysis | |||||
| Metabolic Parameters | |||||
| Glucose [mg/dL] | 93(85-100) | 88(83-97) | 94(88-103) | 89(83-96)D | 89(83-95)D |
| TC [mg/dL] | 184(161-230) | 180(152-206) | 195(175-229)b | 201(175-239)B | 216(181-240)b |
| TG [mg/dL] | 90(74-153) | 131(104-155) | 147(109-196)A | 146(102-185)a | 208(149-242)A,B,D,E |
| HDL-c [mg/dL] | 53(46-59) | 43(39-54)A | 46(40-56)a | 49(41-60)b | 45(38-53)A,e |
| LDL-c [mg/dL] | 106(91-149) | 108(91-140) | 123(101-152) | 126(95-155) | 129(108-160)b |
| TC:HDL ratio | 3.5(3.1-4) | 4.3(3.7-4.8)a | 4.3(3.6-5.1)A | 4.2(3.4-5.2)a | 4.5(4.1-5.7)A,b,e |
| Inflammatory Markers | |||||
| hs-CRP [ug/mL] | 3.1(1.5-6.6) | 3.6(1.8-14.9) | 8.1(4.2-18.3)A,b | 3.9(2.0-14.8)d | 5.4(2.4-15.9)a |
| s-ICAM [ng/mL] | 521(454-602) | 711(574-937)A | 651(509-914)A | 657(526-914)A | 651(504-843)A |
| s-VCAM [ng/mL] | 651(548-977) | 1114(768-1952)A | 806(593-1036)B | 845(649-1083)a,b | 1011(606-1409)a |
| Lepitin [ng/mL] | 23(15-31) | 23(16-43) | 16(11-24)a,B | 18(12-27)b | 18(14-31) |
Continuous variables are reported as median (interquartile range). bpm = beats per minute, mmHg = millimeters of mergury, SBP = systolic blood pressure, DBP = diastolic blood pressure, MP = mean preasure, PP = pulse pressure, AP = augmentation pressure, AIx = augmentation index, AIx = 75 = augmentation index, normalize to a heart rate of 75 bpm, mm = millimeters, kPa = kiloPascals, TC = total cholesterol, TG = triglycerides, HDL = high density lipoprotein cholesterol, LDL = low density lipoprotein cholesterol, hs-CRP = high sensitivity C-reactive protein, sICAM = soluble intercellular adhesion molecule-1, sVCAM = soluble vascular cell adhesion molecule-1, mg = milligrams, ug = micrograms, ng = nanograms, dL = deciliter, mL = milliliters.
A, a = p<0.005 or p<0.05 versus HIV-negative controls, respectively;
B, b = p<0.005 or p<0.05 versus HAART-naive, respectively;
D, d = p<0.005 or p<0.05 versus EFV, respectively;
E, e = p<0.005 or p<0.05 versus NVP, respectively.
Fig 1. Preclinical markers of atherosclerosis are elevated in EFV-treated and LPV/r-treated subjects compared to HAART-naïve and NVP-treated.
Wilcoxon rank sum test p-values are shown. *Note: Although the pairwise Wilcoxon rank sum test showed differences in cIMT between EFV- and LPV/r-treated and NVP-treated subject, ANOVA yielded a p = 0.12, which is above the defined criteria of p<0.05 for statistical significance. When normalized to carotid artery diameter (cIMT-norm = cIMT/(D/2), where D = carotid diameter), EFV- and LPV/r-treated subjects exhibited significantly increased values compared to NVP-treated and HAART-naïve subject.
Flow-mediated dilation (FMD)
The peak FMD was observed at 60 seconds post-occlusion (not shown). FMD at 60 seconds post-occlusion was reduced in EFV-treated and LPV/r-treated compared to HAART-naïve subjects and in EVF-treated compared to NVP-treated subjects.
Carotid Artery Geometry and Properties
No significant differences in the cIMT were observed across groups. The carotid artery diameter was smaller in NVP- compared to EFV- and LPV/r-treated subjects, both in diastole and systole. When normalized to diameter, however, cIMTnorm was significantly increased in EFV- and LPV/r-treated compared to NVP-treated and HAART-naïve subjects. The medial stress was lower in EFV- and LPV/r-treated compared to NVP-treated subjects and lower in EFV-treated compared to HIV-negative and HAART-naïve subjects. No differences were observed in the Peterson modulus, compliance, or cyclic strain over the cardiac cycle across groups.
Plasma Metabolic Parameters
Fasting glucose was elevated in EFV-treated compared to NVP- and LPV/r-treated subjects. Total cholesterol was elevated in all HAART-treated groups compared to HAART-naïve subjects. Triglycerides were elevated in all HAART-treated groups compared to HIV-negative subjects and in LPV/r-treated subjects compared to all other groups. HDL was lower in HAART-naïve and EFV- and LPV/r-treated compared to HIV-negative subjects and in HAART-naïve and LPV/r-treated compared to NVP-treated subjects. LDL was higher in LPV/r-treated compared to HAART-naïve subjects. Total cholesterol to HDL ratio was elevated in all HAART-treated groups and HAART-naïve compared to HIV-negative subjects and in LPV/r-treated compared to HAART-naïve and NVP-treated subjects.
Inflammatory Markers and Adipokines
hs-CRP was elevated in EFV-treated compared to HIV-negative, HAART-naïve, and NVP-treated subjects and in LPV/r-treated compared to HIV-negative subjects. sICAM-1 was elevated in all HIV-positive groups, compared to HIV-negative subjects. sVCAM-1 was elevated in HAART-naïve, NVP-treated, and LPV/r-treated compared to HIV-negative subjects and in HAART-naïve subjects compared to EFV- and NVP-treated subjects. Leptin was lower in EFV- and NVP-treated groups compared to HAART-naïve subjects and in EFV-treated compared to HIV-negative subjects.
Correlation and Regression Analysis
Multivariable regression of data from all HAART treated subjects showed that PWV was associated with age, current EFV and LPV/r used, heart rate, B-SPB, triglycerides, LDL, and hsCRP (Table 3). FMD was associated with age, HIV duration, WHR, and glucose. cIMT was associated with age, current EFV use, skinfold thickness, and blood pressure.
Table 3. Correlation analysis and multivariable regression model for PWV, FMD, and cIMT versus key study parameters.
| Pulse Wave Velocity | Flow-mediated Dilation | Carotid Intima-media Thickness | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Correlation | Multivariable Regression Model | Correlation | Multivariable Regression Model | Correlation | Multivariable Regression Model | ||||||||||
| ρ | P | β | SE(β) | p | ρ | P | β | SE(β) | p | ρ | P | β | SE(β) | p | |
| Demographics | |||||||||||||||
| Age | 0.531 | <0.001 | 0.0425 | 0.0151 | 0.006 | -0.163 | 0.014 | -0.00137 | 0.000564 | 0.017 | 0.412 | <0.001 | 0.000240 | 7.582E-05 | 0.002 |
| Sex | 0.151 | 0.022 | — | — | — | -0.15 | 0.023 | — | — | — | 0.164 | 0.013 | — | — | — |
| HIV / HAART History | |||||||||||||||
| CD4 count | -0.154 | 0.020 | — | — | — | 0.0429 | 0.52 | — | — | — | 0.0314 | 0.64 | — | — | — |
| log10(VL) | 0.066 | 0.32 | — | — | — | -0.011 | 0.87 | — | — | — | 0.0531 | 0.42 | — | — | — |
| Year since HIV+ | 0.189 | 0.004 | — | — | — | -0.0105 | 0.87 | -0.00357 | 0.00167 | 0.035 | 0.104 | 0.12 | — | — | — |
| HAART duration | 0.228 | <0.001 | — | — | — | 0.0119 | 0.86 | — | — | — | 0.140 | 0.034 | — | — | — |
| Current EFV | 0.121 | 0.067 | 1.14 | 0.277 | <0.001 | -0.0987 | 0.14 | — | — | — | 0.0972 | 0.14 | 0.0257 | 0.0122 | 0.038 |
| Current LPV/r | 0.132 | 0.047 | 1.05 | 0.305 | <0.001 | -0.0471 | 0.48 | — | — | — | 0.0744 | 0.26 | — | — | — |
| Body Composition | |||||||||||||||
| BMI | 0.107 | 0.11 | — | — | — | 0.027 | 0.68 | — | — | — | 0.109 | 0.1 | — | — | — |
| WHR | 0.313 | <0.001 | — | — | — | -0.187 | 0.005 | -0.15 | 0.0647 | 0.023 | 0.171 | 0.009 | — | — | — |
| Trunk:Arm | 0.140 | 0.034 | — | — | — | -0.152 | 0.022 | — | — | — | 0.105 | 0.11 | 0.00138 | 0.000517 | 0.009 |
| Cardiovascular Metrics | |||||||||||||||
| Heart Rate | 0.204 | 0.002 | 0.0278 | 0.0125 | 0.028 | 0.0741 | 0.26 | — | — | — | -0.0711 | 0.28 | — | — | — |
| B-SBP | 0.567 | <0.001 | 0.0332 | 0.00662 | <0.001 | -0.147 | 0.026 | — | — | — | 0.311 | <0.001 | 6.43E-05 | 3.14E-05 | 0.043 |
| AIx75 | 0.408 | <0.001 | — | — | — | 0.0978 | 0.14 | — | — | — | 0.146 | 0.027 | — | — | — |
| PWV | -0.113 | 0.088 | — | — | — | 0.337 | <0.001 | — | — | — | |||||
| FMD | -0.113 | 0.09 | — | — | — | -0.111 | 0.093 | — | — | — | |||||
| cIMT | 0.337 | <0.001 | — | — | — | -0.111 | 0.093 | — | — | — | |||||
| Blood Sample Analysis | |||||||||||||||
| Metabolic Parameters | |||||||||||||||
| Glucose | 0.130 | 0.05 | — | — | — | -0.0671 | 0.31 | -0.000615 | 0.000288 | 0.035 | 0.0915 | 0.17 | — | — | — |
| TG | 0.145 | 0.03 | 0.0018 | 0.000888 | 0.046 | -0.084 | 0.21 | — | — | — | 0.0274 | 0.68 | — | — | — |
| HDL-c | 0.00364 | 0.96 | — | — | — | 0.0049 | 0.94 | — | — | — | 0.0954 | 0.15 | — | — | — |
| LDL-c | 0.259 | <0.001 | 0.0063 | 0.00311 | 0.046 | -0.0212 | 0.75 | — | — | — | 0.185 | 0.005 | — | — | — |
| Inflammatory Markers | |||||||||||||||
| VCAM | -0.125 | 0.06 | — | — | — | 0.0739 | 0.27 | — | — | — | -0.103 | 0.12 | — | — | — |
| ICAM | -0.113 | 0.09 | — | — | — | 0.134 | 0.042 | — | — | — | -0.118 | 0.0756 | — | — | — |
| Leptin | -0.0293 | 0.66 | — | — | — | 0.127 | 0.055 | — | — | — | -0.0282 | 0.67 | — | — | — |
| hs-CRP | 0.300 | <0.001 | 0.0209 | 0.00799 | 0.0106 | -0.0531 | 0.42 | — | — | — | 0.0820 | 0.22 | — | — | — |
| Adjusted R2 = | 0.604 | Adjusted R2 = | 0.168 | Adjusted R2 = | 0.277 | ||||||||||
ρ = Spearman Rank Correlation Coefficient, P = p-value for Spearman correlation, β = model parameters, SE(β) = standard error of model parameters, p = p-value for multivariable regression for that parameter. BMI = body mass index, WHR = waist-to-hip ratio, B-SBP = brachial artery systolic blood pressure, PWV = pulse wave velocity, FMD = flow mediated dilation, cIMT = carotid intima-media thickness, TG = triglycerides, HDL = high density lipoprotein cholesterol, LDL = low density lipoprotein cholesterol, VCAM = soluble vascular cell adhesion molecule, ICAM = souluble intercellular adhesion molecule, hsCRP = C-reactive protein.
Discussion
Preclinical Markers of Atherosclerosis
There are numerous studies that associate specific antiretroviral drugs with early onset of atherosclerosis. Protease inhibitors (PI’s) have been the most widely implicated class of antiretroviral drugs associated with atherosclerosis and have been correlated with increased c-IMT [13,14], impaired FMD [15–17], dyslipidemia [10], atherosclerosis [18,19], and myocardial infarction [20], but others have reported contradictory results [21–25]. Non-nucleoside reverse transcriptase inhibitors (NNRTIs) have been associated with elevated cholesterol levels and triglycerides [19], with EFV associated with higher total cholesterol and triglyceride levels than NVP [10]. Less is known about the association between NNRTIs and c-IMT, FMD, and arterial stiffness.
Increased arterial stiffness is a key predictor of future cardiovascular events [26] and is elevated in HIV-positive populations [5,6,27,28]. van Vonderen et al. report decreased distensibility and compliance coefficients in carotid, femoral, and brachial arteries in HIV-positive subjects, with no differences between HAART-naïve and HAART-treated subjects. In a longitudinal study, van Vonderen et al. showed a decrease in carotid arterial stiffness, but increase in femoral artery stiffness (i.e., a decrease in distensibility and compliance coefficients) after 24 months of AZT+3TC+LPV/r treatment, with similar trends in NVP+LPV/r treatment [6]. The current report shows that central arterial stiffness measured via PWV was higher in EFV- and LPV/r-treated subjects, compared to NVP-treated subjects; however, no differences were observed in the carotid artery elastic modulus, compliance, or the distensibility or compliance coefficients (not shown) across groups. Note that arterial stiffening in aorta, but not CCA’s, is consistent with recent findings in a mouse model of AZT treatment [29].
Arterial stiffness appears to increase with HAART [5,6,28] and is associated with immune cell activation and senescence [27] and may be independent of lipodystrophy [30]. In the current study, PWV was associated with EFV and LPV/r use, traditional cardiovascular risk factors (age, heart rate, B-SBP), dyslipidemia (triglycerides and LDL), and systemic inflammation (hsCRP). Taken together, the current study and previous studies from the literature suggest that both HIV infection and HAART play a role in arterial stiffening, with differing effects at different locations in the vasculature.
Impaired brachial artery FMD is a non-invasive indicator of endothelial dysfunction and is associated with elevated cardiovascular risk in the general population [31]. Impaired FMD is also widely reported in HIV-infected populations and appears to be associated with both viral RNA levels [32,33] and HAART [8,9,11,34]. Although not significantly different than pre-HAART values, Gupta et al. reports a significant decrease in FMD in EFV-treated compared to PI-treated subjects after 12-months of treatment [34]. Impaired FMD has been associated with lipodystrophy [35]; the association between FMD and dyslipidemia with HIV, however, is debatable [8]. Our data show that EFV- and LPV/r-treated subject exhibit lower FMD, compared to NVP-treated and HAART-naïve subjects. Multivariant regression shows that FMD was associated with age, duration of HIV, WHR, and fasting blood glucose levels.
Increased cIMT has been widely reported in HIV-infected populations [6,7,32,36–39], is strongly associated with all-cause death in HIV patients [40], and appears to be associated with both HIV infection and HAART regimen [36,38]. PI’s have been implicated [4] as a mediator of increased cIMT and cIMT has been associated with immune cell activation [41,42], systemic inflammation [40,42,43], and Framingham risk [44]. Our data show nominally higher cIMT in EFV- and LPV/r-treated subject; however, increased cIMT only becomes significant when normalized to D/2. Multivariant regression showed that cIMT was associated with current EFV use, traditional cardiovascular risk factors (age and B-SBP), and lipodystrophy (Trunk:Arm).
Our results show elevated markers of atherosclerosis in EFV- and LPV/r-treated subjects, compared to HAART-naïve and NVP-treated groups. However, there are several compounding factors at play that contribute to this observation. First, the years since HIV diagnosis in the HAART-treated group is nearly double that of the HIV-naïve group. however, the NVP group had a longer duration of HIV infection, compared to the EFV group. Second, more subjects in the EFV- and LPV/r-treated groups were taking an NRTI-backbone of TDF+3TC, compared to the NVP-treated group, which had more subjects taking AZT+3TC. The role of AZT in arterial stiffening, endothelial dysfunction, and cIMT is well documented [45–47]. We included TDF and AZT in early iterations of our multivariable regression model; due to their low association with arterial stiffness, cIMT, and FMD, TDF and AZT were considered key predictors of these markers and were subsequently eliminated from the final model. Clinical evidence for atherosclerosis associated with NRTIs is often indirect and difficult to define because NRTIs are typically not prescribed as monotherapy and cardiovascular effects are often attributed to other components of HAART (namely PIs). Nevertheless, recent exposure to abacavir, didanosine, and tenofovir in adult populations was associated with increased risk of heart failure [48–51]; however, these findings are controversial [52]. Abacavir has been associated with impaired FMD [53]. Experimental models, including those from our group, clearly show that AZT, induces endothelial dysfunction [45,54] and increased c-IMT and arterial stiffness [55].
Data from the literature suggest that HIV, independent of HAART, can induce cardiovascular disease [56–58]. Post-mortem analyses reveal coronary arteriopathy [59,60], pulmonary arteriopathy [60], major atherosclerotic lesions [60,61] and cerebral aneurysms [62] in HIV-positive patients not treated with HAART. A long-term multi-institution analysis concluded that cessation of HAART in HIV-positive patients increased their short-term risk of developing cardiovascular disease [56]. Viral load correlated inversely with endothelium-dependent FMD without any relation to HAART regimens [63]; thus, viral load is a significant predictor of impaired FMD [25]. HIV infected, HAART-naïve patients exhibited elevated c-IMT and impaired FMD [57] and HIV-infected children had significantly reduced FMD and increased arterial stiffness of the carotid artery compared to non-infected children, with no significant differences between HAART treated and HAART naïve subjects [64]. Lorenz et al. concluded that both HAART and HIV-infection are independent risk factors for the development of atherosclerosis in adults [65]. They show that c-IMT of the carotid bifurcation was 25% higher in HIV positive / HAART-naïve patients compared to uninfected controls, but observed significantly greater c-IMT of the carotid bifurcation and the common carotid artery due to HAART treatment in HIV positive subjects. Although c-IMT, FMD, and arterial stiffening are affected by HIV infection, it appears that HIV infection only introduces mild dyslipidemia [57,66,67].
Metabolic Disorders
Alterations in plasma lipid profiles have been reported in both HAART-naïve and HAART-treated subjects that are characterized by increased TG’s and decreased HDL; increased total cholesterol and LDL are also reported and PI-containing regimens are generally associated with a less favorable lipid profile compared to PI-sparing regimens [10,68]. Our results are consistent with these observations, with both HAART-naïve and HAART-treated subjects showing less favorable lipid profiles than HIV-negative subjects, and PI-treated subjects exhibiting worse lipid profiles than other HIV-positive groups.
HIV-associated lipodystrophy is characterized by peripheral lipoatrophy and central lipohypertrophy, and are often associated with disorders in glucose metabolism, insulin resistance, dyslipidemia, altered cytokine and adipokine production, and markers of cardiovascular disease [1,69]. Self-reported observations of fat redistribution in the present study suggest similar trends, with a significant fraction of HAART subjects reporting observed decreases in peripheral fat and an increase in central fat. In addition, NVP-treated subjects reported increase in fat in their face, arms, and legs. Skin-fold thickness measurements support these self-reports, with EFV-, NVP-, and LPV/r-treated subjects having higher Trunk/arm ratios compared to HIV-negative and HAART-naïve subjects. Note that the trunk skin-fold thickness measurement did not suggest central lipohypertrophy, as superiliac and sub-scapula values were generally lower or not significantly different in HAART-treated compared to non-HAART-treated subjects.
Inflammatory Markers & Adipokines
hsCRP is a key predictor of future cardiovascular events in the general population [70–72], is widely reported to be elevated in HIV populations [7,39,43,73–79] (noting contradictory reports [27,32,80]), and is associated with all-cause death in HIV patients [40]. Most studies show little or no HAART dependency [6,33,34,76,81] and hsCRP appears to be independent of lipodystrophy [35]. Our results show that hsCRP is elevated in EFV-treated subjects compared to HIV-negative, HAART-naïve, and NVP-treated subjects and elevated in LPV/r-treated subjects compared to HIV-negative subjects and that hsCRP is a key predictor of PWV.
sVCAM-1 and sICAM-1 are plasma biomarkers that have been associated with the initiation and progression of atherosclerosis [82] and are commonly associated with HIV infection [76,79,80,83]. Following initiation of HAART, values decrease from pre-HAART levels, but remain higher than HIV-negative controls [6,34,76,84]. Our results are consistent with these findings, with sVCAM-1 and sICAM-1 levels elevated in HAART-naïve and, to a lesser degree, in HAART-treated subjects compared to HIV-negative subjects, but no correlation between sVCAM-1 or sICAM-1 levels and PWV, FMD, or cIMT were found.
Adipokines such as adiponectin and leptin have been studied intensively for their relation to obesity, insulin resistance, and hyperglycemia and as potential proatherogenic mediators [85,86]. Low leptin and adiponectin levels are more common in persons with HIV and correlate with lipodystrophy [35,73,79,87]. Our results show reduced leptin levels with HAART treatment, but no correlation between leptin levels and PWV, FMD, or cIMT were found.
Study Limitations
This study has several limitations. The cross-sectional design of this study does not allow for a causal relationship between specific antiretroviral drugs and the markers studied. As is often the case, there were challenges in recruiting a representative HIV-negative control group. Controls were recruited by word of mouth at Black Lion hospital, and some recruits may have been referred from the Cardiac clinic. This may explain, in part, why the preclinical markers of atherosclerosis were nominally, albeit not significantly higher (except for FMD), in the controls versus NVP-treated and HAART-naïve groups. Although the normalization of the cIMT was motivated to normalize values across a broad range of patients and showed significant differences across groups, although the more traditional ‘raw’ cIMT data followed similar trends, the raw data did not show significant differences. Also, the cIMT images were taken from a single profile view, rather than the average of several orthogonal views and the FMD protocol did not include nitroglycerine to quantify the endothelial independent vasodilation. Taken together, we believe these limitations do not significantly bias the conclusions of this study.
Conclusion
This report suggests that current EFV and LPV/r may play a role in the development of HIV-associated preclinical markers of atherosclerosis. The data presented herein are consistent with previous results, in that HAART-treated subjects exhibit elevated cholesterol, TC:HDL ratio, and triglycerides and elevated markers of inflammation. What is surprising, however, is that although NVP-treated subjects have similar traditional risk factors (e.g., dyslipidemia, lipodystrophy) compared to EFV-treated subjects, NVP-treated subjects appear to be protected from elevations in preclinical markers of atherosclerosis. These data suggest that the early on-set atherosclerosis may arise from inflammatory mechanisms or mechanisms that are distinct from traditional risk factors and delineate the need for additional longitudinal studies to establish a causal relationship between EFV- and LPV/r-treatment and atherosclerosis in this population.
Supporting Information
(DOCX)
Acknowledgments
We gratefully acknowledge the support from the Fulbright Scholars Program (11–21255, RLG) American Heart Association (11GRNT7990055, RLG). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Funding from Fulbright Scholars Program (11-21255, RLG) and American Heart Association (11GRNT7990055, RLG). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Carr A, Samaras K, Thorisdottir A, Kaufmann G, Chisholm D, et al. (1999) Diagnosis, prediction, and natural course of HIV-1 protease-inhibitor-associated lipodystrophy, hyperlipidaemia, and diabetes mellitus: a cohort study. Lancet 353: 2093–2099. [DOI] [PubMed] [Google Scholar]
- 2. Mary-Krause M, Cotte L, Simon A, Partisani M, Costagliola D (2003) Increased risk of myocardial infarction with duration of protease inhibitor therapy in HIV-infected men. AIDS 17: 2479–2486. [DOI] [PubMed] [Google Scholar]
- 3. Friis-Moller N, Sabin C, Weber R, D'Arminio Monforte A, El-Sadr W, et al. (2003) Combination antiretroviral therapy and the risk of myocardial infarction. New England Journal of Medicine 349: 1993–2003. [DOI] [PubMed] [Google Scholar]
- 4. Maggi P, Lillo A, Perilli F, Maserati R, Chirianni A (2004) Colour-Doppler ultrasonography of carotid vessels in patients treated with antiretroviral therapy: a comparative study. AIDS 18: 1023–1028. [DOI] [PubMed] [Google Scholar]
- 5. Sevastianova K, Sutinen J, Westerbacka J, Ristola M, Yki-Jarvinen H (2005) Arterial stiffness in HIV-infected patients receiving highly active antiretroviral therapy. Antivir Ther 10: 925–935. [PubMed] [Google Scholar]
- 6. van Vonderen M, Hassink E, van Agtmael M, Stehouwer C, Danner S, et al. (2009) Increase in carotid artery intima-media thickness and arterial stiffness but improvement in several markers of endothelial function after initiation of antiretroviral therapy. Journal of Infectious Diseases 199: 1186–1194. 10.1086/597475 [DOI] [PubMed] [Google Scholar]
- 7. Hsue P, Lo J, Franklin A, Bolger A, Martin J, et al. (2004) Progression of atherosclerosis as assessed by carotid intima-media thickness in patients with HIV infection. Circulation 109: 1603–1608. [DOI] [PubMed] [Google Scholar]
- 8. Stein J, Klein M, Bellehumeur J, McBride P, Wiebe D, et al. (2001) Use of human immunodeficiency virus-1 protease inhibitors is associated with atherogenic lipoprotein changes and endothelial dysfunction. Circulation 104: 257–262. [DOI] [PubMed] [Google Scholar]
- 9. Shankar S, Dube M, Gorski J, Klaunig J, Steinberg H (2005) Indinavir impairs endothelial function in healthy HIV-negative men. American Heart Journal 150: 933 [DOI] [PubMed] [Google Scholar]
- 10. Fontas E, van Leth F, Sabin C, Friis-Moller N, Rickenbach M, et al. (2004) Lipid profiles in HIV-infected patients receiving combination antiretroviral therapy: are different antiretroviral drugs associated with different lipid profiles? Journal of Infectious Diseases 189: 1056–1074. [DOI] [PubMed] [Google Scholar]
- 11. Hsue PY, Hunt PW, Wu Y, Schnell A, Ho JE, et al. (2009) Association of abacavir and impaired endothelial function in treated and suppressed HIV-infected patients. AIDS 23: 2021–2027. 10.1097/QAD.0b013e32832e7140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.UNAIDS (2012) Report on the Global AIDS Epidemic.
- 13. van Wijk JP, de Koning EJ, Cabezas MC, Joven J, op't Roodt J, et al. (2006) Functional and structural markers of atherosclerosis in human immunodeficiency virus-infected patients. Journal of the American College of Cardiology 47: 1117–1123. [DOI] [PubMed] [Google Scholar]
- 14. Johnsen S, Dolan SE, Fitch KV, Kanter JR, Hemphill LC, et al. (2006) Carotid intimal medial thickness in human immunodeficiency virus-infected women: effects of protease inhibitor use, cardiac risk factors, and the metabolic syndrome. Journal of Clinical Endocrinology and Metabolism 91: 4916–4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stein JH, Klein MA, Bellehumeur JL, McBride PE, Wiebe DA, et al. (2001) Use of human immunodeficiency virus-1 protease inhibitors is associated with atherogenic lipoprotein changes and endothelial dysfunction. Circulation 104: 257–262. [DOI] [PubMed] [Google Scholar]
- 16. Shankar SS, Dube MP, Gorski JC, Klaunig JE, Steinberg HO (2005) Indinavir impairs endothelial function in healthy HIV-negative men. American Heart Journal 150: 933 [DOI] [PubMed] [Google Scholar]
- 17. Blanco JJ, Garcia IS, Cerezo JG, de Rivera JM, Anaya PM, et al. (2006) Endothelial function in HIV-infected patients with low or mild cardiovascular risk. Journal of Antimicrobial Chemotherapy 58: 133–139. [DOI] [PubMed] [Google Scholar]
- 18. Fisher SD, Miller TL, Lipshultz SE (2006) Impact of HIV and highly active antiretroviral therapy on leukocyte adhesion molecules, arterial inflammation, dyslipidemia, and atherosclerosis. Atherosclerosis 185: 1–11. [DOI] [PubMed] [Google Scholar]
- 19. Friis-Moller N, Weber R, Reiss P, Thiebaut R, Kirk O, et al. (2003) Cardiovascular disease risk factors in HIV patients—association with antiretroviral therapy. Results from the DAD study. AIDS 17: 1179–1193. [DOI] [PubMed] [Google Scholar]
- 20. Worm SW, Sabin C, Weber R, Reiss P, El-Sadr W, et al. (2010) Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) study. Journal of Infectious Diseases 201: 318–330. 10.1086/649897 [DOI] [PubMed] [Google Scholar]
- 21. Currier JS, Kendall MA, Henry WK, Alston-Smith B, Torriani FJ, et al. (2007) Progression of carotid artery intima-media thickening in HIV-infected and uninfected adults. AIDS 21: 1137–1145. [DOI] [PubMed] [Google Scholar]
- 22. Currier JS, Kendall MA, Zackin R, Henry WK, Alston-Smith B, et al. (2005) Carotid artery intima-media thickness and HIV infection: traditional risk factors overshadow impact of protease inhibitor exposure. AIDS 19: 927–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Grubb JR, Dejam A, Voell J, Blackwelder WC, Sklar PA, et al. (2006) Lopinavir-ritonavir: effects on endothelial cell function in healthy subjects. Journal of Infectious Diseases 193: 1516–1519. [DOI] [PubMed] [Google Scholar]
- 24. Nolan D, Watts GF, Herrmann SE, French MA, John M, et al. (2003) Endothelial function in HIV-infected patients receiving protease inhibitor therapy: does immune competence affect cardiovascular risk? QJM 96: 825–832. [DOI] [PubMed] [Google Scholar]
- 25. Solages A, Vita JA, Thornton DJ, Murray J, Heeren T, et al. (2006) Endothelial function in HIV-infected persons. Clinical Infectious Diseases 42: 1325–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Arnet D, Evans G, Riley W (1994) Arterial stiffness: a new cardiovascular risk factor? American Journal of Epidemiology 140: 669–682. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan RC, Sinclair E, Landay AL, Lurain N, Sharrett AR, et al. (2011) T cell activation predicts carotid artery stiffness among HIV-infected women. Atherosclerosis. [DOI] [PMC free article] [PubMed]
- 28. Seaberg EC, Benning L, Sharrett AR, Lazar JM, Hodis HN, et al. (2010) Association between human immunodeficiency virus infection and stiffness of the common carotid artery. Stroke 41: 2163–2170. 10.1161/STROKEAHA.110.583856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hansen L, Parker I, Roberts LM, Sutliff R, Platt M, et al. (2013) Azidothymidine (AZT) leads to arterial stiffening and intima-media thickening in mice. Journal of Biomechanics In Press. [DOI] [PMC free article] [PubMed]
- 30. van Vonderen M, Smulders Y, Stehouwer C, Danner S, Gundy C, et al. (2009) Carotid intima-media thickness and arterial stiffness in HIV-infected patients: the role of HIV, antiretroviral therapy, and lipodystrophy. Journal of Acquired Immune Deficiency Syndromes 50: 153–161. 10.1097/QAI.0b013e31819367cd [DOI] [PubMed] [Google Scholar]
- 31. Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, et al. (2009) Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation 120: 502–509. 10.1161/CIRCULATIONAHA.109.864801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Oliviero U, Bonadies G, Apuzzi V, Foggia M, Bosso G, et al. (2009) Human immunodeficiency virus per se exerts atherogenic effects. Atherosclerosis 204: 586–589. 10.1016/j.atherosclerosis.2008.10.012 [DOI] [PubMed] [Google Scholar]
- 33. Torriani F, Komarow L, Parker R, Cotter B, Currier J, et al. (2008) Endothelial function in human immunodeficiency virus-infected antiretroviral-naive subjects before and after starting potent antiretroviral therapy: The ACTG (AIDS Clinical Trials Group) Study 5152s. Journal of the American College of Cardiology 52: 569–576. 10.1016/j.jacc.2008.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gupta SK, Shen C, Moe SM, Kamendulis LM, Goldman M, et al. (2012) Worsening endothelial function with efavirenz compared to protease inhibitors: a 12-month prospective study. PloS one 7: e45716 10.1371/journal.pone.0045716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Masiá M, Padilla S, García N, Jarrin I, Bernal E, et al. (2010) Endothelial function is impaired in HIV-infected patients with lipodystrophy. Antiviral therapy 15: 101–110. 10.3851/IMP1491 [DOI] [PubMed] [Google Scholar]
- 36. Chironi G, Escaut L, Gariepy J, Cogny A, Teicher E, et al. (2003) Brief report: carotid intima-media thickness in heavily pretreated HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes 32: 490–493. [DOI] [PubMed] [Google Scholar]
- 37. Mercie P, Thiebaut R, Aurillac-Lavignolle V, Pellegrin J, Yvorra-Vives M, et al. (2005) Carotid intima-media thickness is slightly increased over time in HIV-1-infected patients. HIV Med 6: 380–387. [DOI] [PubMed] [Google Scholar]
- 38. Lorenz M, Stephan C, Harmjanz A, Staszewski S, Buehler A, et al. (2008) Both long-term HIV infection and highly active antiretroviral therapy are independent risk factors for early carotid atherosclerosis. Atherosclerosis 196: 720–726. [DOI] [PubMed] [Google Scholar]
- 39. Hsue P, Hunt P, Schnell A, Kalapus S, Hoh R, et al. (2009) Role of viral replication, antiretroviral therapy, and immunodeficiency in HIV-associated atherosclerosis. AIDS 23: 1059–1067. 10.1097/QAD.0b013e32832b514b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mangili A, Polak JF, Quach LA, Gerrior J, Wanke CA (2011) Markers of atherosclerosis and inflammation and mortality in patients with HIV infection. Atherosclerosis 214: 468–473. 10.1016/j.atherosclerosis.2010.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kaplan RC, Sinclair E, Landay AL, Lurain N, Sharrett AR, et al. (2011) T cell activation and senescence predict subclinical carotid artery disease in HIV-infected women. The Journal of infectious diseases 203: 452–463. 10.1093/infdis/jiq071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Longenecker C, Funderburg N, Jiang Y, Debanne S, Storer N, et al. (2013) Markers of inflammation and CD8 T-cell activation, but not monocyte activation, are associated with subclinical carotid artery disease in HIV-infected individuals. HIV Med. [DOI] [PMC free article] [PubMed]
- 43. Ross AC, O'Riordan MA, Storer N, Dogra V, McComsey GA (2010) Heightened inflammation is linked to carotid intima-media thickness and endothelial activation in HIV-infected children. Atherosclerosis 211: 492–498. 10.1016/j.atherosclerosis.2010.04.008 [DOI] [PubMed] [Google Scholar]
- 44. Falcone EL, Mangili A, Skinner S, Alam A, Polak JF, et al. (2011) Framingham risk score and early markers of atherosclerosis in a cohort of adults infected with HIV. Antiviral therapy 16: 1–8. 10.3851/IMP1682 [DOI] [PubMed] [Google Scholar]
- 45. Kline ER, Sutliff RL (2008) The role of HIV-1 proteins and antiretroviral drug therapy in HIV-1-associated endothelial dysfunction. J Investig Med 56: 752–769. 10.1097/JIM.0b013e3181788d15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hansen L, Parker I, Roberts LM, Sutliff RL, Platt MO, et al. (2013) Azidothymidine (AZT) leads to arterial stiffening and intima-media thickening in mice. J Biomech 46: 1540–1547. 10.1016/j.jbiomech.2013.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sutliff R, Dikalov S, Weiss D, Parker J, Raidel S, et al. (2002) Nucleoside reverse transcriptase inhibitors impair endothelium-dependent relaxation by increasing superoxide. American Journal of Physiology: Heart and Circulatory Physiology 283: H2363–H2370. [DOI] [PubMed] [Google Scholar]
- 48. Choi AI, Vittinghoff E, Deeks SG, Weekley CC, Li Y, et al. (2011) Cardiovascular risks associated with abacavir and tenofovir exposure in HIV-infected persons. AIDS 25: 1289–1298. 10.1097/QAD.0b013e328347fa16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kowalska JD, Kirk O, Mocroft A, Hoj L, Friis-Moller N, et al. (2010) Implementing the number needed to harm in clinical practice: risk of myocardial infarction in HIV-1-infected patients treated with abacavir. HIV medicine 11: 200–208. 10.1111/j.1468-1293.2009.00763.x [DOI] [PubMed] [Google Scholar]
- 50. Worm SW, Sabin C, Weber R, Reiss P, El-Sadr W, et al. (2010) Risk of myocardial infarction in patients with HIV infection exposed to specific individual antiretroviral drugs from the 3 major drug classes: the data collection on adverse events of anti-HIV drugs (D:A:D) study. The Journal of infectious diseases 201: 318–330. 10.1086/649897 [DOI] [PubMed] [Google Scholar]
- 51. Lundgren J, Neuhaus J, Babiker A, Cooper D, Duprez D, et al. (2008) Use of nucleoside reverse transcriptase inhibitors and risk of myocardial infarction in HIV-infected patients. AIDS 22: F17–24. 10.1097/QAD.0b013e32830fe35e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ribaudo HJ, Benson CA, Zheng Y, Koletar SL, Collier AC, et al. (2011) No risk of myocardial infarction associated with initial antiretroviral treatment containing abacavir: short and long-term results from ACTG A5001/ALLRT. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 52: 929–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hsue PY, Hunt PW, Wu Y, Schnell A, Ho JE, et al. (2009) Association of abacavir and impaired endothelial function in treated and suppressed HIV-infected patients. AIDS 23: 2021–2027. 10.1097/QAD.0b013e32832e7140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sutliff RL, Dikalov S, Weiss D, Parker J, Raidel S, et al. (2002) Nucleoside reverse transcriptase inhibitors impair endothelium-dependent relaxation by increasing superoxide. American Journal of Physiology: Heart and Circulatory Physiology 283: H2363–H2370. [DOI] [PubMed] [Google Scholar]
- 55.Hansen L, Kennedy I, Sutliff R, Platt M, Gleason R (In Preparation) AZT induces intima-medial thickening, endothelial dysfunction, and arterial stiffening in mice. [DOI] [PMC free article] [PubMed]
- 56. El-Sadr WM, Lundgren JD, Neaton JD, Gordin F, Abrams D, et al. (2006) CD4+ count-guided interruption of antiretroviral treatment. New England Journal of Medicine 355: 2283–2296. [DOI] [PubMed] [Google Scholar]
- 57. Oliviero U, Bonadies G, Apuzzi V, Foggia M, Bosso G, et al. (2009) Human immunodeficiency virus per se exerts atherogenic effects. Atherosclerosis 204: 586–589. 10.1016/j.atherosclerosis.2008.10.012 [DOI] [PubMed] [Google Scholar]
- 58. Hsue PY, Hunt PW, Schnell A, Kalapus SC, Hoh R, et al. (2009) Role of viral replication, antiretroviral therapy, and immunodeficiency in HIV-associated atherosclerosis. AIDS 23: 1059–1067. 10.1097/QAD.0b013e32832b514b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Joshi VV, Pawel B, Connor E, Sharer L, Oleske JM, et al. (1987) Arteriopathy in children with acquired immune deficiency syndrome. Pediatr Pathol 7: 261–275. [DOI] [PubMed] [Google Scholar]
- 60. Perez-Atayde AR, Kearney DI, Bricker JT, Colan SD, Easley KA, et al. (2004) Cardiac, aortic, and pulmonary arteriopathy in HIV-infected children: the Prospective P2C2 HIV Multicenter Study. Pediatric and developmental pathology: the official journal of the Society for Pediatric Pathology and the Paediatric Pathology Society 7: 61–70. [DOI] [PubMed] [Google Scholar]
- 61. Paton P, Tabib A, Loire R, Tete R (1993) Coronary artery lesions and human immunodeficiency virus infection. Res Virol 144: 225–231. [DOI] [PubMed] [Google Scholar]
- 62. Maniker AH, Hunt CD (1996) Cerebral aneurysm in the HIV patient: a report of six cases. Surg Neurol 46: 49–54. [DOI] [PubMed] [Google Scholar]
- 63. Blum A, Hadas V, Burke M, Yust I, Kessler A (2005) Viral load of the human immunodeficiency virus could be an independent risk factor for endothelial dysfunction. Clin Cardiol 28: 149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bonnet D, Aggoun Y, Szezepanski I, Bellal N, Blanche S (2004) Arterial stiffness and endothelial dysfunction in HIV-infected children. AIDS 18: 1037–1041. [DOI] [PubMed] [Google Scholar]
- 65.Lorenz MW, Stephan C, Harmjanz A, Staszewski S, Buehler A, et al. (2007) Both long-term HIV infection and highly active antiretroviral therapy are independent risk factors for early carotid atherosclerosis. Atherosclerosis. [DOI] [PubMed]
- 66. Buchacz K, Weidle P, Moore D, Were W, Mermin J, et al. (2008) Changes in lipid profile over 24 months among adults on first-line highly active antiretroviral therapy in the home-based AIDS care program in rural Uganda. Journal of Acquired Immune Deficiency Syndromes 47: 304–311. [DOI] [PubMed] [Google Scholar]
- 67.Charakida M, Donald A, Green H, Storry C (2005) Early structural and functional changes of the vasculature in HIV-infected children. Circulation. [DOI] [PubMed]
- 68. Estrada V, Portilla J (2011) Dyslipidemia related to antiretroviral therapy. AIDS reviews 13: 49–56. [PubMed] [Google Scholar]
- 69. Loonam CR, Mullen A (2012) Nutrition and the HIV-associated lipodystrophy syndrome. Nutrition research reviews 25: 267–287. 10.1017/S0954422411000138 [DOI] [PubMed] [Google Scholar]
- 70. Ridker PM, Rifai N, Rose L, Buring JE, Cook NR (2002) Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. The New England journal of medicine 347: 1557–1565. [DOI] [PubMed] [Google Scholar]
- 71. Ballantyne CM, Hoogeveen RC, Bang H, Coresh J, Folsom AR, et al. (2005) Lipoprotein-associated phospholipase A2, high-sensitivity C-reactive protein, and risk for incident ischemic stroke in middle-aged men and women in the Atherosclerosis Risk in Communities (ARIC) study. Archives of Internal Medicine 165: 2479–2484. [DOI] [PubMed] [Google Scholar]
- 72. Rost NS, Wolf PA, Kase CS, Kelly-Hayes M, Silbershatz H, et al. (2001) Plasma concentration of C-reactive protein and risk of ischemic stroke and transient ischemic attack: the Framingham study. Stroke; a journal of cerebral circulation 32: 2575–2579. [DOI] [PubMed] [Google Scholar]
- 73. Dolan SE, Hadigan C, Killilea KM, Sullivan MP, Hemphill L, et al. (2005) Increased cardiovascular disease risk indices in HIV-infected women. Journal of acquired immune deficiency syndromes (1999) 39: 44–54. [DOI] [PubMed] [Google Scholar]
- 74. Masia M, Bernal E, Padilla S, Graells ML, Jarrin I, et al. (2007) The role of C-reactive protein as a marker for cardiovascular risk associated with antiretroviral therapy in HIV-infected patients. Atherosclerosis 195: 167–171. [DOI] [PubMed] [Google Scholar]
- 75. Ross AC, Armentrout R, O'Riordan MA, Storer N, Rizk N, et al. (2008) Endothelial activation markers are linked to HIV status and are independent of antiretroviral therapy and lipoatrophy. Journal of acquired immune deficiency syndromes 49: 499–506. 10.1097/QAI.0b013e318189a794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kristoffersen U, Kofoed K, Kronborg G, Giger A, Kjaer A, et al. (2009) Reduction in circulating markers of endothelial dysfunction in HIV-infected patients during antiretroviral therapy. HIV Med 10: 79–87. 10.1111/j.1468-1293.2008.00661.x [DOI] [PubMed] [Google Scholar]
- 77. Lichtner M, Cuomo M, Rossi R, Strano S, Massetti A, et al. (2009) Increased carotid intima media thickness is associated with depletion of circulating myeloid dendritic cells in HIV-infected patients on suppressive antiretroviral treatment. Atherosclerosis 204: e1–3. 10.1016/j.atherosclerosis.2008.12.025 [DOI] [PubMed] [Google Scholar]
- 78. Neuhaus J, Jacobs DR, Baker JV, Calmy A, Duprez D, et al. (2010) Markers of inflammation, coagulation, and renal function are elevated in adults with HIV infection. The Journal of infectious diseases 201: 1788–1795. 10.1086/652749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Miller TL, Somarriba G, Orav EJ, Mendez AJ, Neri D, et al. (2010) Biomarkers of vascular dysfunction in children infected with human immunodeficiency virus-1. Journal of acquired immune deficiency syndromes (1999) 55: 182–188. 10.1097/QAI.0b013e3181e222c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Baker J, Ayenew W, Quick H, Hullsiek K, Tracy R, et al. (2010) High-density lipoprotein particles and markers of inflammation and thrombotic activity in patients with untreated HIV infection. Journal of Infectious Diseases 201: 285–292. 10.1086/649560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Calmy A, Gayet-Ageron A, Montecucco F, Nguyen A, Mach F, et al. (2009) HIV increases markers of cardiovascular risk: results from a randomized, treatment interruption trial. AIDS 23: 929–939. [DOI] [PubMed] [Google Scholar]
- 82. Galkina E, Ley K (2007) Vascular adhesion molecules in atherosclerosis. Arteriosclerosis, Thrombosis, and Vascular Biology 27: 2292–2301. [DOI] [PubMed] [Google Scholar]
- 83. Gattegno L, Bentata-Peyssare M, Gronowski S, Chaouche K, Ferriere F (1995) Elevated concentrations of circulating intercellular adhesion molecule 1 (ICAM-1) and of vascular cell adhesion molecule 1 (VCAM-1) in HIV-1 infection. Cell Adhesion and Communication 3: 179–185. [DOI] [PubMed] [Google Scholar]
- 84. Mastroianni CM, Lichtner M, Mengoni F, Agostino C, Ettorre G, et al. (2000) Changes in circulating levels of soluble cell adhesion molecules following highly active antiretroviral treatment of HIV-1-infected patients. Clinical immunology (Orlando, Fla) 95: 212–217. [DOI] [PubMed] [Google Scholar]
- 85. Matarese G, Mantzoros C, La Cava A (2007) Leptin and adipocytokines: bridging the gap between immunity and atherosclerosis. Current Pharmaceutical Design 13: 3676–3680. [DOI] [PubMed] [Google Scholar]
- 86. Takemura Y, Walsh K, Ouchi N (2007) Adiponectin and cardiovascular inflammatory responses. Current atherosclerosis reports 9: 238–243. [DOI] [PubMed] [Google Scholar]
- 87. Gougeon ML, Penicaud L, Fromenty B, Leclercq P, Viard JP, et al. (2004) Adipocytes targets and actors in the pathogenesis of HIV-associated lipodystrophy and metabolic alterations. Antiviral therapy 9: 161–177. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.