Abstract
The gastrointestinal tract constitutes a physiological interface integrating nutrient and microbiota-host metabolism. Conjugated linoleic acids (CLA) have been reported to contribute to decreased body weight and fat accretion. The modulation by dietary CLA of stomach proteins related to energy homeostasis or microbiota may be involved, although this has not been previously analysed. This is examined in the present study, which aims to underline the potential mechanisms of CLA which contribute to body weight regulation. Adult mice were fed either a normal fat (NF, 12% kJ content as fat) or a high-fat (HF, 43% kJ content as fat) diet. In the latter case, half of the animals received daily oral supplementation of CLA. Expression and content of stomach proteins and specific bacterial populations from caecum were analysed. CLA supplementation was associated with an increase in stomach protein expression, and exerted a prebiotic action on both Bacteroidetes/Prevotella and Akkermansia muciniphila. However, CLA supplementation was not able to override the negative effects of HF diet on Bifidobacterium spp., which was decreased in both HF and HF+CLA groups. Our data show that CLA are able to modulate stomach protein expression and exert a prebiotic effect on specific gut bacterial species.
Introduction
Obesity is currently growing at an epidemic rate, considered a major health threat around the world, and resulting in an increased risk of diabetes mellitus type II, some types of cancer, fatty liver disease, hypertension, cardiovascular disease and increased mortality. Despite large research efforts on the effects of diet, exercise, education, surgery or drug therapies, there is still no long-term solution to efficiently prevent or counteract obesity [1].
Dietary conjugated linoleic acids (CLA) refer to a mixture of geometric and positional isomers of linoleic acid with conjugated double bonds found mainly in ruminant meat and dairy products [2]. Growing research has shown that the isomers cis-9, trans-11-CLA and trans-10, cis-12-CLA in particular have a major role in the regulation of body weight and body fat in both animal [3–9] and human [10–13] studies,
The present study was carried out to further characterise the effects of CLA on body weight management, by addressing certain aspects that to our knowledge have not been studied before. The gastrointestinal tract is the largest endocrine of the body and is responsible for the conversion of food into energy, is metabolically highly active and home to trillions of microbes [14, 15]. The stomach is one of the first sites in the gastrointestinal tract that responds to food intake. It synthesises proteins which have an important role in energy balance and have been shown to be modulated by diet [16–21]. Another interesting component is caecum content, which harbours a large amount of bacteria that carry out a number of functions involved in energy regulation, such as the processing of non-digestible polysaccharides, metabolism of proteins, synthesis of vitamins and production of energy [22–25]. Emerging evidence suggests that the gut microbiota may be involved in obesity [26–28], and that high-fat diet in particular could contribute to the modulation of this bacterial community [29–33]. Therefore, the role of food in modifying gut microbiota towards a more beneficial profile is of great interest [34].
Overall, this highlights the importance of the interplay between food and the different components of the gastrointestinal tract. The aim was to study the potential of CLA in the regulation of both stomach protein expression and specific gut bacterial species in obese mice under a HF diet.
Materials and Methods
Animals
Male C57BL/6J mice from Charles River (Barcelona, Spain) weighing 21 ± 0.1 g (5 weeks-old) were housed under standard conditions in cages in groups of 4–5 and kept in a 12-h light:dark cycle at 22°C with food and water ad libitum. Cages were Makrolon type III (Tecniplast, Biosis Biologic Systems S.L.) and bedding was Ultrasorb fir shavings (Panlab S.L.U). Bedding was changed weekly. After reception, animals were allowed to acclimatize for a week and divided into groups ensuring equal weight average. Food was changed twice a week, and intake and body weight were recorded every three days throughout the experiment [35]. The animal protocol followed in this study was reviewed and approved by the Bioethical Committee of the University of the Balearic Islands (approval 13th February 2006) and University guidelines for the use and care of laboratory animals were strictly followed. All efforts were made to minimize suffering.
Mice were divided into three treatment groups (n = 8). All diets were prepared by Research Diets (Inc, New Brunswick) and presented as pellets to the animals. Detailed composition of these diets can be found in S1 Table. Mice received one of the following diets for 54 days: a standard normal-fat diet (NF), containing 12% kJ content as fat, used as control, or a high-fat diet (HF), which contained 43% kJ content as fat. Diets were based on the standard rodent diet AIN-76A. Therefore, both diets contained equal proportion of protein (20% kJ content) and carbohydrate was used to adjust the energy content. Thus, NF diet contained 40% (w/w) of sucrose and HF 35% (w/w). Then, a daily dose of CLA was given to half of the animals receiving the HF diet. Tonalin (kindly provided by Cognis) was used as the CLA supplement, providing 6 mg of CLA/day (21.4 nmol/isomer/day), given as an oral gavage. Tonalin TG 80, derived from safflower oil, is composed of triacylglycerols containing approximately 80% CLA with a 50:50 ratio of the active CLA isomers cis-9, trans-11 and trans-10, cis-12. At the end of the experiment, body weight did not differ between HF and CLA group, whereas body fat was statistically lower in CLA animals. Complete set of data, including weight of animals, body fat (day 40) and estimated food intake have been previously published [35].
Sacrifice and sample collection
Sacrifice of all animals was carried out within the animal facilities, at the beginning of the light cycle and after 10h of food deprivation. Animals were anaesthetized with an intraperitoneal injection made up of a mixture of xilacine (10 mg/kg body weight) and ketamine (100 mg/kg body weight). Organs and samples of interest were excised and weighed (stomach and caecum). Stomach was opened and the inside was scraped to collect the mucosa. Caecum was also cut open and content collected. All tissues were rinsed with saline containing 0.1% diethyl pyrocarbonate (Sigma, Madrid, Spain) and snap-frozen at -80°C.
Quantification of gastric leptin and ghrelin
Stomach mucosa was homogenized at 4°C in 1:3 (w/v) PBS (mM: 137 NaCL, 2.7 KCl, 10 phosphate buffer, pH 7.4) and centrifuged at 7000 x g for 2min at 4°C. Total protein was determined after 5-fold dilution of the supernatant with PBS using the Bradford method [36]. Gastric leptin was determined in the initial homogenate with a mouse leptin enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Minneapolis, MN). Ghrelin determination in stomach was carried out according to [37]. Stomach homogenate was mixed with 10 volumes 1 M acetic acid containing 20 mM HCl, boiled for 20 min and centrifuged at 7000 x g for 2 min at 4°C. The supernatant was lyophilized and resuspended in PBS. Ghrelin concentration in stomach was then determined using a mouse ghrelin enzyme immunosorbent assay (EIA) kit (Phoenix Europe, Karlsruhe, Germany).
RNA isolation, retrotranscription and real-time qPCR
Total RNA extraction from stomach was carried out with Tripure Reagent (Roche Diagnostic Gmbh, Mannheim, Germany) according to the manufacturer’s instructions. Isolated RNA was quantified using NanoDrop ND-1000 spectrophotometer (NanoDrop Technologies Inc., Wilmington, DE, USA) and its integrity was confirmed using agarose gel electrophoresis.
Samples were retrotranscribed and real-time PCR was carried out for the analysis of stomach proteins. Briefly, 0.25 μg of total RNA (in a final volume of 5 μl) were denatured at 65°C for 10 min and then reverse-transcribed to cDNA using MuLV reverse transcriptase (Applied Biosystems, Madrid, Spain) at 20°C for 15 min, 42°C for 30 min and a final step of 5 min at 95°C in a thermal cycler (Applied Biosystems 2720 Thermal Cycler, Madrid, Spain).
Each PCR was performed with diluted cDNA template, forward and reverse primers (5μM each) and Power SYBR Green PCR Master Mix (Applied Biosystems, CA, USA). Primers were designed and obtained from Sigma Aldrich Química SA (Madrid, Spain) and sequences are described in Table 1. Real-time PCR was performed using the Applied Biosystems StepOnePlus Real-Time PCR Systems (Applied Biosystems) with the following template: 10 min at 95°C followed by a total of 42 temperature cycles (15 s at 95°C and 1 min at 60°C). In order to verify the purity of the products amplified, a melting curve was produced after each run according to the manufacturer's instructions. The threshold cycle (Ct) was calculated by the instrument's software (StepOne Software v2.0), and the relative expression of each gene was calculated as a percentage of NF mice using the 2−ΔΔCt method [38]. Beta-actin was used as the reference gene.
Table 1. Nucleotide sequences of primers used for qPCR amplification in mouse stomach.
| Mouse genes | Forward primer (5’ to 3’) | Reverse primer (3’ to 5’) | Amplicon size (pb) |
|---|---|---|---|
| Beta-actin | tacagcttcaccaccacagc | tctccagggaggaagaggat | 120 |
| Leptin | ttgtcaccaggatcaatgaca | gacaaactcagaatggggtgaag | 186 |
| Ghrelin | cagaaagcccagcagagaaa | gaagggagcattgaacctga | 144 |
| Mboat4 | ttgtgaagggaaggtggag | gagagcagggaaaaagagca | 115 |
| Retn | ttccttttcttccttgtccctg | ctttttcttcacgaatgtccc | 246 |
| Gpr39 | ctgctgattggctttgtatgg | cggttggagaggttcgtg | 188 |
| Gcg | tctgacgagatgagcacca | tgactggcacgagatgttg | 136 |
| Gcgr | gcacccgaaactacatcca | acacgccctctaccagca | 231 |
| Sst | accccagactccgtcagtt | agcctcatctcgtcctgct | 169 |
| Sstr | catcgtcaacatcgtcaacc | catcctccacaccgtatcct | 194 |
Forward and reverse sequences designed for qPCR amplification in stomach samples of mice.
Bacterial profiling by qPCR
Total bacterial DNA was extracted from approximately 50 mg of caecal samples using the E.Z.N.A. Stool DNA kit (Omega Biotek, GA, USA). DNA concentration was determined using a NanoDrop ND-1000 spectrophotometer (NanoDrop Technologies Inc., Wilmington, DE, USA) and its integrity confirmed by agarose gel. Assessment of the presence and relative amount of bacterial species was determined by measuring DNA abundance of the 16S rRNA gene sequences by qPCR with the Applied Biosystems StepOnePlus Real-Time PCR System (Applied Biosystems), following previously described protocols [39, 40]. Specific primers for Clostridium coccoides, Clostridium leptum and Lactobacillus spp. (Firmicutes representatives); Bacteroides/Prevotella (Bacteroidetes); Bifidobacterium spp. (Actinobacteria); Akkermansia muciniphila (Verrucomicrobia); Enterobacteriaceae (Proteobacteria); and Total Bacteria were obtained from Sigma (Madrid, Spain). Total Bacteria refers to a broad-range universal primer that recognizes the conserved region of the 16S rRNA encoding gene for a wide range of bacterial species, and was used to normalize the assay to total bacterial DNA. Sequences are described in Table 2. The threshold cycle was calculated using the 2−ΔΔCt method [38], and relative bacterial content and fold change (FC) were calculated (Log22−ΔΔCt). Values were normalized with the average of the NF group.
Table 2. Sequence of primers used for bacterial profiling in caecum content.
| Phylum | Bacterial Species | Forward primer (5’ to 3’) | Reverse primer (3’ to 5’) |
|---|---|---|---|
| Proteobacteria | Enterobacteriaceae | cattgacgttacccgcagaagaagc | ctctacgagactcaagcttgc[ 39 ] |
| Actinobacteria | Bifidobacterium spp. | cgcgtcyggtgtgaaag | ccccacatccagcatcca[ 39 ] |
| Firmicutes | Clostridium coccoides | actcctacgggaggcagc | gcttcttagtcargtaccg[ 39 ] |
| Clostridium leptum | gcacaagcagtggagt | cttcctccgtttgtcaa[ 39 ] | |
| Lactobacillus spp. | gaggcagcagtagggaatcttc | ggccagttactacctctatccttcttc[ 39 ] | |
| Bacteroidetes | Bacteroides/Prevotella | tcctacgggaggcagcagt | caatcggagttcttcgtg[ 39 ] |
| Verrucomicrobia | Akkermansia muciniphila | cagcacgtgaaggtggggac | ccttgcggttggcttcagat[ 40 ] |
| Housekeeping | |||
| Total Bacteria | Total bacteria | actcctacgggaggcag | gtattaccgcggctgctg[ 39 ] |
Forward and reverse sequences for qPCR amplification in mouse caecal content.
Statistical analysis
Data are presented as means ± SEM. Equality of variances between groups was assessed by Levene’s test. When homogeneity of variances was assumed, one-way ANOVA was used to determine the significance of the different parameters between groups. If there was a significant difference, a Bonferroni test was used to determine where the difference lay and to correct for multiple testing. When homogeneity of variances was not assumed, data were log transformed. Linear relationships between key variables were tested using Pearson's correlation coefficients. Threshold of significance was set at P<0.05. The analysis was performed using the SPSS program for Windows version 21.0 (SPSS, Chicago, IL, USA).
Results
CLA supplementation modulates the expression of regulatory proteins in the stomach
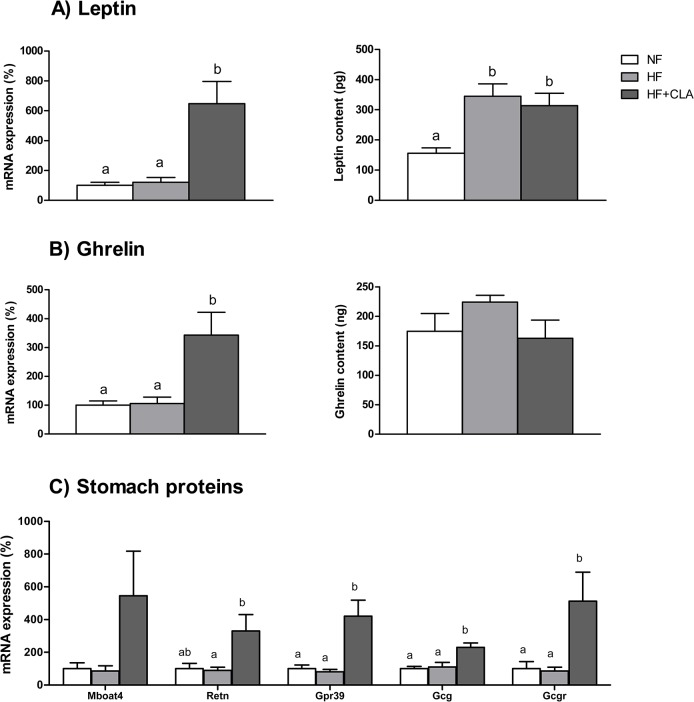
Expression of proteins associated to energy metabolism and regulation of food intake was determined in mouse stomach. Leptin mRNA expression in the HF group was not altered, however leptin protein was increased in these animals (2-fold vs. NF, p = 0.003). On the other hand, supplementation with CLA caused a 6-fold higher expression of leptin mRNA (in comparison with NF, p = 0.001), which was in accordance with higher content of gastric leptin (2-fold, p = 0.014 vs. NF) (Fig 1A). CLA-fed animals also exhibited increased ghrelin mRNA expression (3-fold, p = 0.006 vs.NF), but no changes were seen amongst groups regarding ghrelin protein (Fig 1B).
Fig 1. Effect of CLA supplementation on mRNA expression and protein levels of gastric proteins in mice.
Expression of stomach proteins were analysed in mice after 54 days of supplementation with CLA. (A) Leptin mRNA (%) expression was increased by CLA, and protein content (pg) was higher in both HF and CLA groups. (B) Ghrelin mRNA (%) expression was also higher in CLA animals, whereas protein levels (ng) did not show significant differences amongst groups. (C) Gastric resistin (Retn), G protein-coupled receptor 39 (Gpr39), glucagon (Gcg) and glucagon receptor (Gcgr) expression increased by CLA supplementation, whereas ghrelin o-acyltransferase (Mboat4) did not. Data are the mean ± SEM of 8 animals/group. Letters indicate differences amongst groups; one-way ANOVA followed by Bonferroni test (p<0.05).
Furthermore, CLA supplementation was associated to increased expression of all stomach proteins analysed and statistical significance was attained in the case of resistin (Retn) (3-fold, p = 0.026), G protein-coupled receptor 39 (Gpr39) (4-fold, p = 0.001), Glucagon (Gcg) (2-fold, 0.001) and Glucagon Receptor (Gcgr) (5-fold, p = 0.011) (Fig 1C).
Caecum microbiota is modulated by CLA
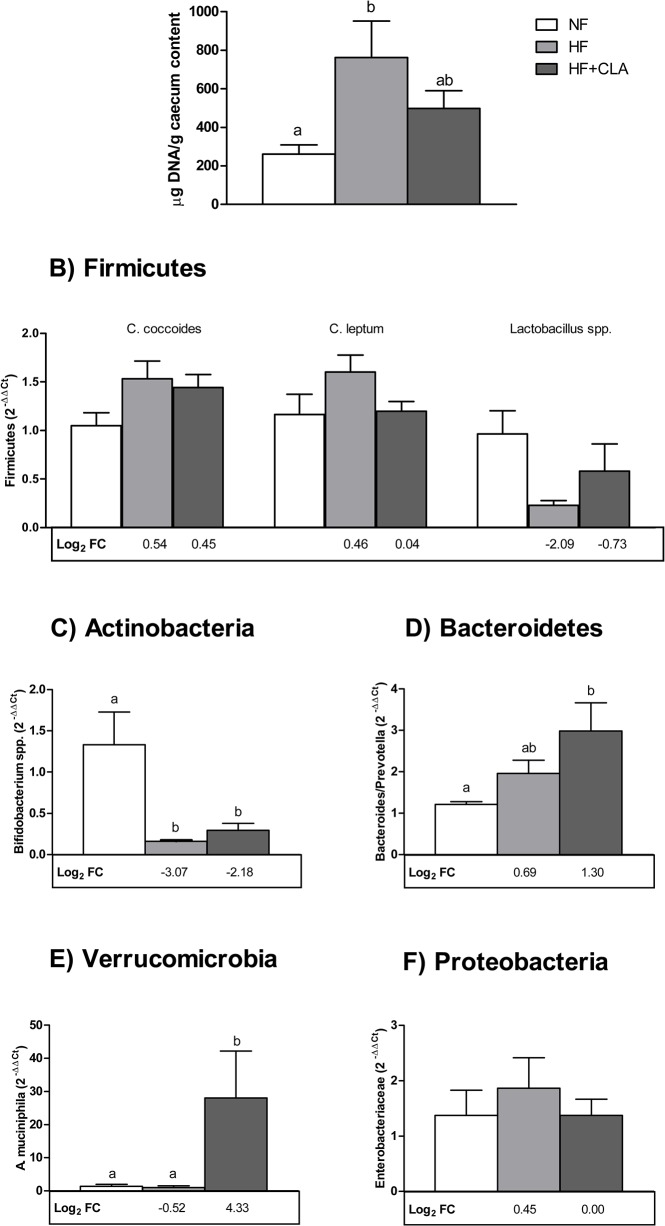
To further look into the effect of CLA, caecum content of mice was analysed in order to determine bacterial species potentially associated to obesity and energy metabolism. A significant increase in bacterial DNA caecum content was observed in mice fed a HF diet (3-fold vs. NF, p = 0.032), which decreased with CLA supplementation and showed no differences compared to NF animals (Fig 2A). This was accompanied by differences in gut microbiota composition.
Fig 2. DNA levels of representative bacterial species in mice caecum are altered by diet.
Bacterial species from caecum content was analysed in all groups. (A) Bacterial DNA levels in caecum content (μg bacterial DNA/g caecum content) was increased significantly by HF diet. DNA abundance of 16S rRNA gene of representative bacterial species (B) Firmicutes, (C) Actinobacteria, (D) Bacteroidetes, (E) Verrucomicrobia and (F) Proteobacteria was analysed in mouse caecum and normalised with the average of the NF group (2−ΔΔCt). Fold change respect to NF group was calculated (Log2 FC) and is indicated below each column. Data are mean ± SEM of 6–8 animals/group. Letters indicate differences amongst groups; one-way ANOVA followed by Bonferroni test (p<0.05). When homogeneity of variances was not assumed, data were log transformed.
No statistically significant changes were found concerning the Firmicutes content under the different dietary treatments (Fig 2B). HF feeding was mainly associated to a decrease in Bifidobacterium spp. (p = 0.009 vs. NF; with a fold change (Log2 FC) of -3.07). CLA supplementation did not counteract this reduction, presenting similar values (p = 0.034 vs. NF; -2.18 Log2 FC) (Fig 2C). In contrast, animals receiving CLA showed a significant increase in two bacterial species of interest: Bacteroides/Prevotella (p = 0.021 vs. NF; 1.30 Log2 FC) (Fig 2D) and A. muciniphila, which dramatically increased compared to both NF (p = 0.014; 4.33 Log2 FC) and HF (p = 0.002) (Fig 2E). No significant changes on Enterobacteriaceae profile were seen (Fig 2F).
Caecum microbiota correlates with body weight and body fat
We next tested the hypothesis that abundance of specific bacterial species in mouse caecum contents could be associated to modulation of body weight and body fat. On one hand, C. coccoides (r = .433, p = 0.044) and C. leptum (r = .488, p = 0.021), both belonging to the Firmicutes’ group, showed positive correlations with body weight. Bacteroides/Prevotella also showed a positive correlation (r = .581, p = 0.006) with body weight. On the other, body fat was negatively correlated with Bifidobacterium spp. (r = -.547, p = 0.008). The correlation matrix is presented in Table 3.
Table 3. Correlations between bacterial species in caecum contents with body weight and body fat of mice.
| Bacterial Species | Body Weight | Body Fat | |||
|---|---|---|---|---|---|
| R | P | R | P | ||
| Clostridium coccoides | .433* | 0.044 | .415 | 0.055 | |
| Clostridium leptum | .488* | 0.021 | .165 | 0.464 | |
| Bacteroidetes | .581** | 0.006 | .203 | 0.378 | |
| Bifidobacterium spp. | -.407 | 0.060 | -.547** | 0.008 | |
Linear relationships were tested using Pearson’s correlation coefficients (R). Significant correlations are marked as follows:
* = p<0.05,
** = p<0.01.
Discussion
The present study provides evidence that CLA supplementation under a HF diet has a noticeable effect on particular sites of the gastrointestinal tract in mouse, by increasing gastric protein expression and by promoting a prebiotic effect on gut microbiota. Considering that the gastrointestinal tract integrates the interplay of food, microbiota and metabolic effects on the host, these results may be relevant for the development of weight management strategies, since CLA are compounds used for the reduction of fat mass in humans [10–13].
Gut hormones are secreted in the stomach in response to food intake and play a key role in signalling food intake to the brain [41]. Leptin and ghrelin constitute two of the most studied proteins involved in energy metabolism, both being secreted in relevant amount by the gastric mucosa [42–47]. In accordance with leptin mRNA levels, higher gastric protein content was also observed, which is in accordance with the increased plasma leptin levels described in these animals [35]. It has been previously described that high-fat feeding stimulates the gastric leptin signalling pathway [44], an effect which would not be counteracted by CLA and would contribute to partially explain why no differences were seen regarding food intake in this experimental set up [35]. On the other hand, ghrelin gene is a gut orexigenic hormone which is mainly regulated by feeding [48], and although mRNA expression increased with CLA, protein ghrelin levels were not changed. The discrepancies observed between mRNA expression and protein levels would be associated to the presence of diurnal rhythms described for both ghrelin and leptin in the gastric environment which allow for a better metabolic control[49]. In addition to these main gastric proteins, we analysed ghrelin o-acyltransferase (Mboat4), resistin and Gpr39, as well as glucagon, somatostatin and their receptors, proteins which are also involved in energy balance and have been described in the gastric mucosa [50–56], although their potential in weight management has not been thoroughly studied. In this context, Mboat4 was of particular interest as it is the enzyme responsible for the acylation of ghrelin [56] and is activated by dietary lipids which act as acylation substrates [57]. Interestingly, all of the proteins analysed showed increased expression with CLA supplementation, suggesting that CLA isomers are specifically sensed by the genes encoding gastric proteins which respond to food cues.
Additionally to the abovementioned effects, CLA promoted changes in the gut microbiota of the lower part of the gastrointestinal tract. In recent years, it has been proposed that in obese states there is an increased ratio of Firmicutes to Bacteroidetes as well as a loss of bacterial diversity [26–28] although currently more focus is being put on bacterial species for host metabolism characterization as new data emerge (discussed in a recent review [58]). Neither CLA supplementation nor HF diet alone was associated with changes amongst bacterial species in the Firmicutes’ phylum. However, HF feeding lowered Bifidobacterium spp., in accordance with previous animal studies [59–62], a reduction which was not counteracted by CLA. Considering supplementation was not able to re-establish normal body weight [35], a positive association with body weight was found for both C. coccoides and C. leptum, in agreement with the potential adverse role of these bacterial species on obesity [33, 63, 64], as well as a negative correlation with Bifidobacterium spp., an association which has also been previously found in both animal models and human studies [60–63].
In contrast, CLA induced a prebiotic effect in supplemented animals. Bacteroides/Prevotella is a bacterial species known to use dietary polysaccharides in a prebiotic fashion [65]. A remarkable increase was found under CLA supplementation suggesting that CLA was able to confer a prebiotic effect. This is supported by a very high induction of A. muciniphila growth by CLA. The presence of this mucin-degrading bacterial species, which resides in the mucus layer, is associated to a healthy mucosa and is generally reduced in obese states [66–68]. Everard et al. [69] have recently demonstrated that oligofructose restores A. muciniphila content in obese animals, and this is associated with an improvement of their metabolic profile. Therefore, the increased caecal content of A. muciniphila found under CLA supplementation suggests that this compound was exerting a prebiotic action on this bacterial species too. To our knowledge, this is the first evidence of a CLA-prebiotic effect favouring the specific growth of potentially beneficial bacterial species in the gut. However, this increase in both Bacteroides/Prevotella and A. muciniphila was not enough to allow a full recovery since these animals remain obese [35]. We cannot rule out that a higher CLA dose and/or longer treatment, which is generally associated with a leaner phenotype [70], would cause an even higher increase in A. muciniphila content and have more significant effects on metabolic parameters. This would fit with the lower induction of A. muciniphila found in the present study in comparison with others [69, 71].
Overall, our data show that gastrointestinal tract is a first site for action of the bioactive isomers of CLA, able to modulate gastric responses as well as microbiota-host metabolism. We cannot rule out the potential interplay between gastric environment and bacterial growth associated to food cues accompanying CLA intake. However, CLA induced the expression of genes encoding gastric proteins related with regulation of energy balance and exerted a prebiotic effect on selected bacterial species. Growth of potentially beneficial bacterial species, specifically Bacteroidetes/Prevotella and A. muciniphila, suggests CLA confers a prebiotic effect, which could contribute to a healthier metabolic profile. Further and thorough research of how specific dietary treatments influence specific physiological components, such as the gastrointestinal tract, will help elucidate their impact on specific conditions such as obesity, and develop efficient body weight management strategies.
Supporting Information
Composition of normal and high fat diets used throughout the experiment.
(DOCX)
Acknowledgments
We thank Sarah Laraichi (Laboratory of Calorimetry and Materials, Faculty of Sciences, Abdelmalek Essaâdi University, 93030 Tétouan, Morocco) for her help with the animal care and sample collection during her stay in our lab.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the grant AGL2012-33692 and the EU-funded project (BIOCLAIMS FP7-244995). The authors' group receives financial support from Instituto de Salud Carlos III, Centro de Investigación Biomédica en Red Fisiopatología de la Obesidad y Nutrición, CIBERobn. Authors belong to the Nutrigenomics-group, awarded as “Group of Excellence” of CAIB and supported by “Direcció General d’Universitats, Recerca i Transferència del Coneixement” of Regional Government (CAIB) and FEDER funds (EU). AC is supported by a PhD fellowship by Conselleria d'Educació, Cultura i Universitats, Govern de les Illes Balears, a project which is cofinanced by the European Social Fund. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14. Epub 2011/08/30. 10.1016/S0140-6736(11)60813-1 . [DOI] [PubMed] [Google Scholar]
- 2. Trigueros L, Pena S, Ugidos AV, Sayas-Barbera E, Perez-Alvarez JA, Sendra E. Food ingredients as anti-obesity agents: a review. Crit Rev Food Sci Nutr. 2013;53(9):929–42. Epub 2013/06/19. 10.1080/10408398.2011.574215 . [DOI] [PubMed] [Google Scholar]
- 3. Park Y, Albright KJ, Liu W, Storkson JM, Cook ME, Pariza MW. Effect of conjugated linoleic acid on body composition in mice. Lipids. 1997;32(8):853–8. Epub 1997/08/01. . [DOI] [PubMed] [Google Scholar]
- 4. Takahashi Y, Kushiro M, Shinohara K, Ide T. Dietary conjugated linoleic acid reduces body fat mass and affects gene expression of proteins regulating energy metabolism in mice. Comp Biochem Physiol B Biochem Mol Biol. 2002;133(3):395–404. Epub 2002/11/15. . [DOI] [PubMed] [Google Scholar]
- 5. West DB, Blohm FY, Truett AA, DeLany JP. Conjugated linoleic acid persistently increases total energy expenditure in AKR/J mice without increasing uncoupling protein gene expression. J Nutr. 2000;130(10):2471–7. Epub 2000/10/04. . [DOI] [PubMed] [Google Scholar]
- 6. West DB, Delany JP, Camet PM, Blohm F, Truett AA, Scimeca J. Effects of conjugated linoleic acid on body fat and energy metabolism in the mouse. Am J Physiol. 1998;275(3 Pt 2):R667–72. Epub 1998/09/05. . [DOI] [PubMed] [Google Scholar]
- 7. Zabala A, Fernandez-Quintela A, Macarulla MT, Simon E, Rodriguez VM, Navarro V, et al. Effects of conjugated linoleic acid on skeletal muscle triacylglycerol metabolism in hamsters. Nutrition. 2006;22(5):528–33. Epub 2006/02/07. 10.1016/j.nut.2005.10.005 . [DOI] [PubMed] [Google Scholar]
- 8. Kanaya N, Chen S. Conjugated linoleic acid reduces body weight gain in ovariectomized female C57BL/6J mice. Nutr Res. 2010;30(10):714–21. Epub 2010/11/09. 10.1016/j.nutres.2010.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Park Y, Albright KJ, Storkson JM, Liu W, Pariza MW. Conjugated linoleic acid (CLA) prevents body fat accumulation and weight gain in an animal model. J Food Sci. 2007;72(8):S612–7. Epub 2007/11/13. 10.1111/j.1750-3841.2007.00477.x . [DOI] [PubMed] [Google Scholar]
- 10. Smedman A, Vessby B. Conjugated linoleic acid supplementation in humans—metabolic effects. Lipids. 2001;36(8):773–81. Epub 2001/10/11. . [DOI] [PubMed] [Google Scholar]
- 11. Blankson H, Stakkestad JA, Fagertun H, Thom E, Wadstein J, Gudmundsen O. Conjugated linoleic acid reduces body fat mass in overweight and obese humans. J Nutr. 2000;130(12):2943–8. Epub 2000/12/09. . [DOI] [PubMed] [Google Scholar]
- 12. Thom E, Wadstein J, Gudmundsen O. Conjugated linoleic acid reduces body fat in healthy exercising humans. J Int Med Res. 2001;29(5):392–6. Epub 2001/12/01. . [DOI] [PubMed] [Google Scholar]
- 13. Gaullier JM, Halse J, Hoivik HO, Hoye K, Syvertsen C, Nurminiemi M, et al. Six months supplementation with conjugated linoleic acid induces regional-specific fat mass decreases in overweight and obese. Br J Nutr. 2007;97(3):550–60. Epub 2007/02/23. 10.1017/S0007114507381324 . [DOI] [PubMed] [Google Scholar]
- 14. Martins dos Santos V, Muller M, de Vos WM. Systems biology of the gut: the interplay of food, microbiota and host at the mucosal interface. Curr Opin Biotechnol. 2010;21(4):539–50. Epub 2010/09/08. 10.1016/j.copbio.2010.08.003 . [DOI] [PubMed] [Google Scholar]
- 15. Hernandez E, Bargiela R, Diez MS, Friedrichs A, Perez-Cobas AE, Gosalbes MJ, et al. Functional consequences of microbial shifts in the human gastrointestinal tract linked to antibiotic treatment and obesity. Gut Microbes. 2013;4(4):306–15. Epub 2013/06/21. 10.4161/gmic.25321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Erdmann J, Lippl F, Schusdziarra V. Differential effect of protein and fat on plasma ghrelin levels in man. Regul Pept. 2003;116(1–3):101–7. Epub 2003/11/06. . [DOI] [PubMed] [Google Scholar]
- 17. Greenman Y, Golani N, Gilad S, Yaron M, Limor R, Stern N. Ghrelin secretion is modulated in a nutrient- and gender-specific manner. Clin Endocrinol (Oxf). 2004;60(3):382–8. Epub 2004/03/11. . [DOI] [PubMed] [Google Scholar]
- 18. Wadden D, Cahill F, Amini P, Randell E, Vasdev S, Yi Y, et al. Serum acylated ghrelin concentrations in response to short-term overfeeding in normal weight, overweight, and obese men. PLoS One. 2012;7(9):e45748 Epub 2012/10/03. 10.1371/journal.pone.0045748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sun B, Purcell RH, Terrillion CE, Yan J, Moran TH, Tamashiro KL. Maternal high-fat diet during gestation or suckling differentially affects offspring leptin sensitivity and obesity. Diabetes. 2012;61(11):2833–41. Epub 2012/07/04. 10.2337/db11-0957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhao Z, Sakata I, Okubo Y, Koike K, Kangawa K, Sakai T. Gastric leptin, but not estrogen and somatostatin, contributes to the elevation of ghrelin mRNA expression level in fasted rats. J Endocrinol. 2008;196(3):529–38. Epub 2008/03/04. 10.1677/JOE-07-0300 . [DOI] [PubMed] [Google Scholar]
- 21. Scarpace PJ, Zhang Y. Leptin resistance: a prediposing factor for diet-induced obesity. Am J Physiol Regul Integr Comp Physiol. 2009;296(3):R493–500. Epub 2008/12/19. 10.1152/ajpregu.90669.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Backhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101(44):15718–23. Epub 2004/10/27. 10.1073/pnas.0407076101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cani PD, Delzenne NM. Interplay between obesity and associated metabolic disorders: new insights into the gut microbiota. Curr Opin Pharmacol. 2009;9(6):737–43. Epub 2009/07/25. 10.1016/j.coph.2009.06.016 . [DOI] [PubMed] [Google Scholar]
- 24. Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–31. Epub 2006/12/22. 10.1038/nature05414 . [DOI] [PubMed] [Google Scholar]
- 25. Murphy EF, Cotter PD, Healy S, Marques TM, O'Sullivan O, Fouhy F, et al. Composition and energy harvesting capacity of the gut microbiota: relationship to diet, obesity and time in mouse models. Gut. 2010;59(12):1635–42. Epub 2010/10/12. 10.1136/gut.2010.215665 . [DOI] [PubMed] [Google Scholar]
- 26. Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI. Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A. 2005;102(31):11070–5. Epub 2005/07/22. 10.1073/pnas.0504978102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Backhed F, Fraser CM, Ringel Y, Sanders ME, Sartor RB, Sherman PM, et al. Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe. 2012;12(5):611–22. Epub 2012/11/20. 10.1016/j.chom.2012.10.012 . [DOI] [PubMed] [Google Scholar]
- 28. Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541–6. Epub 2013/08/30. 10.1038/nature12506 . [DOI] [PubMed] [Google Scholar]
- 29. Cotillard A, Kennedy SP, Kong LC, Prifti E, Pons N, Le Chatelier E, et al. Dietary intervention impact on gut microbial gene richness. Nature. 2013;500(7464):585–8. Epub 2013/08/30. 10.1038/nature12480 . [DOI] [PubMed] [Google Scholar]
- 30. David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–63. Epub 2013/12/18. 10.1038/nature12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhang C, Zhang M, Wang S, Han R, Cao Y, Hua W, et al. Interactions between gut microbiota, host genetics and diet relevant to development of metabolic syndromes in mice. Isme J. 2010;4(2):232–41. Epub 2009/10/30. 10.1038/ismej.2009.112 . [DOI] [PubMed] [Google Scholar]
- 32. Zhang C, Zhang M, Pang X, Zhao Y, Wang L, Zhao L. Structural resilience of the gut microbiota in adult mice under high-fat dietary perturbations. Isme J. 2012;6(10):1848–57. Epub 2012/04/13. 10.1038/ismej.2012.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Parks BW, Nam E, Org E, Kostem E, Norheim F, Hui ST, et al. Genetic control of obesity and gut microbiota composition in response to high-fat, high-sucrose diet in mice. Cell Metab. 2013;17(1):141–52. Epub 2013/01/15. 10.1016/j.cmet.2012.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Brownawell AM, Caers W, Gibson GR, Kendall CW, Lewis KD, Ringel Y, et al. Prebiotics and the health benefits of fiber: current regulatory status, future research, and goals. J Nutr. 2012;142(5):962–74. Epub 2012/03/30. 10.3945/jn.112.158147 . [DOI] [PubMed] [Google Scholar]
- 35. Laraichi S, Parra P, Zamanillo R, El Amarti A, Palou A, Serra F. Dietary supplementation of calcium may counteract obesity in mice mediated by changes in plasma fatty acids. Lipids. 2013;48(8):817–26. Epub 2013/06/05. 10.1007/s11745-013-3798-y . [DOI] [PubMed] [Google Scholar]
- 36. Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–54. Epub 1976/05/07. . [DOI] [PubMed] [Google Scholar]
- 37. Sanchez J, Oliver P, Palou A, Pico C. The inhibition of gastric ghrelin production by food intake in rats is dependent on the type of macronutrient. Endocrinology. 2004;145(11):5049–55. Epub 2004/07/31. 10.1210/en.2004-0493 . [DOI] [PubMed] [Google Scholar]
- 38. Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29(9):e45 Epub 2001/05/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Parnell JA, Reimer RA. Prebiotic fibres dose-dependently increase satiety hormones and alter Bacteroidetes and Firmicutes in lean and obese JCR:LA-cp rats. Br J Nutr. 2012;107(4):601–13. Epub 2011/07/20. 10.1017/S0007114511003163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sonoyama K, Ogasawara T, Goto H, Yoshida T, Takemura N, Fujiwara R, et al. Comparison of gut microbiota and allergic reactions in BALB/c mice fed different cultivars of rice. Br J Nutr. 2010;103(2):218–26. Epub 2009/09/24. 10.1017/S0007114509991589 . [DOI] [PubMed] [Google Scholar]
- 41. Neary MT, Batterham RL. Gut hormones: implications for the treatment of obesity. Pharmacol Ther. 2009;124(1):44–56. Epub 2009/06/30. 10.1016/j.pharmthera.2009.06.005 . [DOI] [PubMed] [Google Scholar]
- 42. Cammisotto P, Bendayan M. A review on gastric leptin: the exocrine secretion of a gastric hormone. Anat Cell Biol. 2012;45(1):1–16. Epub 2012/04/27. 10.5115/acb.2012.45.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Date Y, Kojima M, Hosoda H, Sawaguchi A, Mondal MS, Suganuma T, et al. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology. 2000;141(11):4255–61. Epub 2000/11/23. 10.1210/endo.141.11.7757 . [DOI] [PubMed] [Google Scholar]
- 44. Sanchez J, Priego T, Oliver P, Palou A, Pico C. The intake of a hyperlipidic diet stimulates the gastric leptin signalling pathway in female rats. Genes Nutr. 2007;2(1):135 Epub 2008/10/14. 10.1007/s12263-007-0033-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cinti S, de Matteis R, Ceresi E, Pico C, Oliver J, Oliver P, et al. Leptin in the human stomach. Gut. 2001;49(1):155 Epub 2001/07/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Oliver P, Pico C, De Matteis R, Cinti S, Palou A. Perinatal expression of leptin in rat stomach. Dev Dyn. 2002;223(1):148–54. Epub 2002/01/23. 10.1002/dvdy.1233 . [DOI] [PubMed] [Google Scholar]
- 47. Palou A, Pico C. Leptin intake during lactation prevents obesity and affects food intake and food preferences in later life. Appetite. 2009;52(1):249–52. Epub 2008/10/18. 10.1016/j.appet.2008.09.013 . [DOI] [PubMed] [Google Scholar]
- 48. Bednarek MA, Feighner SD, Pong SS, McKee KK, Hreniuk DL, Silva MV, et al. Structure-function studies on the new growth hormone-releasing peptide, ghrelin: minimal sequence of ghrelin necessary for activation of growth hormone secretagogue receptor 1a. J Med Chem. 2000;43(23):4370–6. Epub 2000/11/23. . [DOI] [PubMed] [Google Scholar]
- 49. Sanchez J, Oliver P, Pico C, Palou A. Diurnal rhythms of leptin and ghrelin in the systemic circulation and in the gastric mucosa are related to food intake in rats. Pflugers Arch. 2004;448(5):500–6. Epub 2004/04/27. 10.1007/s00424-004-1283-4 . [DOI] [PubMed] [Google Scholar]
- 50. McKee KK, Tan CP, Palyha OC, Liu J, Feighner SD, Hreniuk DL, et al. Cloning and characterization of two human G protein-coupled receptor genes (GPR38 and GPR39) related to the growth hormone secretagogue and neurotensin receptors. Genomics. 1997;46(3):426–34. Epub 1998/01/27. 10.1006/geno.1997.5069 . [DOI] [PubMed] [Google Scholar]
- 51. Nogueiras R, Pfluger P, Tovar S, Arnold M, Mitchell S, Morris A, et al. Effects of obestatin on energy balance and growth hormone secretion in rodents. Endocrinology. 2007;148(1):21–6. Epub 2006/09/30. 10.1210/en.2006-0915 . [DOI] [PubMed] [Google Scholar]
- 52. Nogueiras R, Gallego R, Gualillo O, Caminos JE, Garcia-Caballero T, Casanueva FF, et al. Resistin is expressed in different rat tissues and is regulated in a tissue- and gender-specific manner. FEBS Lett. 2003;548(1–3):21–7. Epub 2003/07/30. . [DOI] [PubMed] [Google Scholar]
- 53. Kumar U, Grant M. Somatostatin and somatostatin receptors. Results Probl Cell Differ. 2010;50:137–84. Epub 2009/10/28. 10.1007/400_2009_29 . [DOI] [PubMed] [Google Scholar]
- 54. Dunphy JL, Taylor RG, Fuller PJ. Tissue distribution of rat glucagon receptor and GLP-1 receptor gene expression. Mol Cell Endocrinol. 1998;141(1–2):179–86. Epub 1998/09/02. . [DOI] [PubMed] [Google Scholar]
- 55. Katayama T, Shimamoto S, Oda H, Nakahara K, Kangawa K, Murakami N. Glucagon receptor expression and glucagon stimulation of ghrelin secretion in rat stomach. Biochem Biophys Res Commun. 2007;357(4):865–70. Epub 2007/04/28. 10.1016/j.bbrc.2007.04.001 . [DOI] [PubMed] [Google Scholar]
- 56. Sakata I, Yang J, Lee CE, Osborne-Lawrence S, Rovinsky SA, Elmquist JK, et al. Colocalization of ghrelin O-acyltransferase and ghrelin in gastric mucosal cells. Am J Physiol Endocrinol Metab. 2009;297(1):E134–41. Epub 2009/04/30. 10.1152/ajpendo.90859.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kirchner H, Gutierrez JA, Solenberg PJ, Pfluger PT, Czyzyk TA, Willency JA, et al. GOAT links dietary lipids with the endocrine control of energy balance. Nat Med. 2009;15(7):741–5. Epub 2009/06/09. 10.1038/nm.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Guinane CM, Cotter PD. Role of the gut microbiota in health and chronic gastrointestinal disease: understanding a hidden metabolic organ. Therap Adv Gastroenterol. 2013;6(4):295–308. Epub 2013/07/03. 10.1177/1756283X13482996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. An HM, Park SY, Lee do K, Kim JR, Cha MK, Lee SW, et al. Antiobesity and lipid-lowering effects of Bifidobacterium spp. in high fat diet-induced obese rats. Lipids Health Dis. 2011;10:116 Epub 2011/07/13. 10.1186/1476-511X-10-116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Cani PD, Neyrinck AM, Fava F, Knauf C, Burcelin RG, Tuohy KM, et al. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia. 2007;50(11):2374–83. Epub 2007/09/08. 10.1007/s00125-007-0791-0 . [DOI] [PubMed] [Google Scholar]
- 61. Cano PG, Santacruz A, Trejo FM, Sanz Y. Bifidobacterium CECT 7765 improves metabolic and immunological alterations associated with obesity in high-fat diet-fed mice. Obesity (Silver Spring). 2013. Epub 2013/02/19. 10.1002/oby.20330 . [DOI] [PubMed] [Google Scholar]
- 62. Neyrinck AM, Possemiers S, Druart C, Van de Wiele T, De Backer F, Cani PD, et al. Prebiotic effects of wheat arabinoxylan related to the increase in bifidobacteria, Roseburia and Bacteroides/Prevotella in diet-induced obese mice. PLoS One. 2011;6(6):e20944 Epub 2011/06/23. 10.1371/journal.pone.0020944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Santacruz A, Collado MC, Garcia-Valdes L, Segura MT, Martin-Lagos JA, Anjos T, et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr. 2010;104(1):83–92. Epub 2010/03/09. 10.1017/S0007114510000176 . [DOI] [PubMed] [Google Scholar]
- 64. Nadal I, Santacruz A, Marcos A, Warnberg J, Garagorri JM, Moreno LA, et al. Shifts in clostridia, bacteroides and immunoglobulin-coating fecal bacteria associated with weight loss in obese adolescents. Int J Obes (Lond). 2009;33(7):758–67. Epub 2008/12/04. 10.1038/ijo.2008.260 . [DOI] [PubMed] [Google Scholar]
- 65. Sonnenburg ED, Zheng H, Joglekar P, Higginbottom SK, Firbank SJ, Bolam DN, et al. Specificity of polysaccharide use in intestinal bacteroides species determines diet-induced microbiota alterations. Cell. 2010;141(7):1241–52. Epub 2010/07/07. 10.1016/j.cell.2010.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Derrien M, Vaughan EE, Plugge CM, de Vos WM. Akkermansia muciniphila gen. nov., sp. nov., a human intestinal mucin-degrading bacterium. Int J Syst Evol Microbiol. 2004;54(Pt 5):1469–76. Epub 2004/09/25. 10.1099/ijs.0.02873-0 . [DOI] [PubMed] [Google Scholar]
- 67. Derrien M, Van Baarlen P, Hooiveld G, Norin E, Muller M, de Vos WM. Modulation of Mucosal Immune Response, Tolerance, and Proliferation in Mice Colonized by the Mucin-Degrader Akkermansia muciniphila. Front Microbiol. 2011;2:166 Epub 2011/09/10. 10.3389/fmicb.2011.00166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lukovac S, Belzer C, Pellis L, Keijser BJ, de Vos WM, Montijn RC, et al. Differential Modulation by Akkermansia muciniphila and Faecalibacterium prausnitzii of Host Peripheral Lipid Metabolism and Histone Acetylation in Mouse Gut Organoids. MBio. 2014;5(4). Epub 2014/08/15. 10.1128/mBio.01438-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Everard A, Belzer C, Geurts L, Ouwerkerk JP, Druart C, Bindels LB, et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci U S A. 2013;110(22):9066–71. Epub 2013/05/15. 10.1073/pnas.1219451110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Parra P, Palou A, Serra F. Moderate doses of conjugated linoleic acid reduce fat gain, maintain insulin sensitivity without impairing inflammatory adipose tissue status in mice fed a high-fat diet. Nutr Metab (Lond). 2010;7:5 Epub 2010/02/26. 10.1186/1743-7075-7-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Shin NR, Lee JC, Lee HY, Kim MS, Whon TW, Lee MS, et al. An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet-induced obese mice. Gut. 2014;63(5):727–35. Epub 2013/06/28. 10.1136/gutjnl-2012-303839 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Composition of normal and high fat diets used throughout the experiment.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.