Abstract
Objectives: this study was aimed to test the hypothesis that ankle proprioception assessed by custom-designed proprioception testing equipment changes with ageing in men and women.
Methods: ankle proprioception was assessed in 289 participants (131 women) of the Baltimore Longitudinal Study of Aging (BLSA); the participants aged 51–95 years and were blinded during testing.
Results: the average minimum perceived ankle rotation was 1.11° (SE = 0.07) in women and 1.00° (SE = 0.06) in men, and it increased with ageing in both sexes (P < 0.001, for both). Ankle tracking performance, which is the ability to closely follow with the left ankle, a rotational movement induced on the right ankle by a torque motor, declines with ageing in both men and women (P = 0.018 and P = 0.011, respectively).
Conclusions: a simple, standardised method for assessing ankle proprioception was introduced in this study using a customized test instrument, software and test protocol. Age-associated reduction in ankle proprioception was confirmed from two subtests of threshold and tracking separately for women and men. Findings in this study prompt future studies to determine whether these age-associated differences in the threshold for passive motion detection and movement tracking are evident in longitudinal study and how these specific deficits in ankle proprioception are related to age-associated chronic conditions such as knee or hip osteoarthritis and type II diabetes and affect daily activities such as gait.
Keywords: proprioception, ageing, gait, older people
Introduction
Proprioception is defined as the perception of position and motion which is conveyed by mechanoreceptors located within several joint components and is essential for precision in motor control [1–3]. As a possible compensatory sensory apparatus, proprioception may become more important in older adults who have limited visual and/or vestibular function.
Age-associated decline in proprioception has been documented using the threshold to detection of passive motion for the ankle and knee joints [4–8]. Ankle proprioception assessment in particular has been an area of focus because of its essential role in postural control [7, 9, 10]. Modified or impaired ankle performance during customary walking has been reported in relation to normal ageing and in conditions that are known to impact lower limb somatosensation (e.g. diabetes mellitus) [11–14]. Therefore, proper assessment of ankle proprioception may be critical for designing not only rehabilitation but also pre-habilitation interventions with the aim of preventing or delaying mobility limitation and maintaining normal walking patterns in the face of advancing age and/or pathological conditions. Deficits in ankle joint movement perception have been reported previously in diabetic adults and older adults from ankle proprioception assessments conducted while standing and thus weight bearing [4, 15]. However, the importance of ankle proprioception assessment in non-weight-bearing situations cannot be underestimated, because precise ankle proprioception may be crucial in non-weight-bearing stages of the gait, i.e. the swing phase, for safe ground clearance and avoiding tripping. Poorer ankle proprioception in older adults compared with younger adults has been reported in previous studies using threshold of detecting passive ankle rotation [5] and dynamic position sensing [7], but potentially more subtle age-related differences within older adults and differences between women and men has not been examined. To expand on these scarce observations, we developed a proprioception testing apparatus and testing protocol for automated objective assessment of ankle joint proprioception for detecting threshold for perception of passive movement, passive-to-active ankle position matching and tracking tasks. We examined ankle proprioception performance of older adults to test whether ankle proprioception-related performance is worse with increasing age in the threshold, positioning and tracking tasks using this newly developed device. We also examined proprioception performance differences between men and women.
Methods
Participants
Data are from 289 cognitively intact participants (131 women) aged 51–95 in the BLSA. Participants with severe pain in lower limbs or <10° of ankle plantar flexion or dorsiflexion from neutral position (ankles at 100° with respect to tibia; Figure 1a) were excluded from testing. The BLSA protocol was approved by the appropriate Institutional Review Board (Baltimore, MD, USA), and all participants provided written consent to participate.
Figure 1.
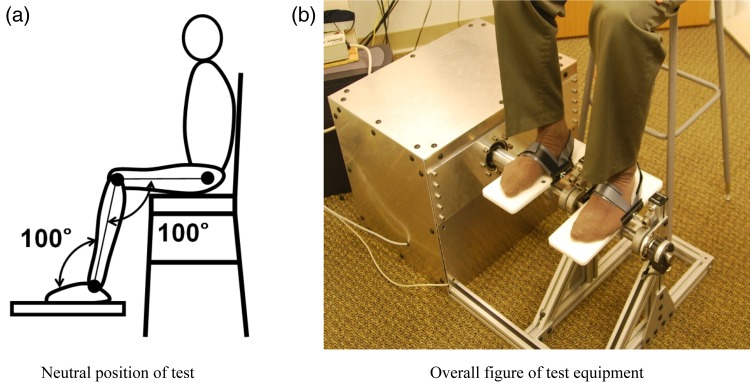
Ankle proprioception test instrument. (a) Neutral position of test; (b) overall figure of test equipment.
Ankle proprioception instrument
The measurement equipment was specifically designed and built for the BLSA and consists of two pedals (Figure 1b). The right foot pedal is moved by a motor (BALDOR, Ft Smith, AZ, USA) and the left is moved freely by the test subject (Figure 1b). Both pedals are attached to potentiometers that continuously measure angular deviation of the ankle joint from the neutral position. Custom-designed interfacing software that executes pre-set rotations in the motor-driven pedal and records the rotations for both pedals was written by LabView (version 7.1, National Instruments, USA) with a 20 Hz sampling rate.
Test protocol
Participants are seated on a height-adjustable stool with their stocking or bare feet placed on the free moving (left) and motor-driven (right) pedals with ankles at neutral position (Figure 1) to permit comfortable ankle rotation for plantar flexion and dorsiflexion of at least 10°. Participants are blindfolded, and their feet are securely strapped into the pedals. If necessary, the instrument can be immediately stopped during the test. The testing is performed in a quiet room without any distractions. Three tests are administered:
Threshold test assesses the minimal angular displacement (degrees) required for perception of passive movement in the proper direction (plantar flexion or dorsiflexion). A total of four trials are performed at an angular speed of 0.3°/s in the pre-set sequence of ankle plantar flexion, dorsiflexion, dorsiflexion, and plantar flexion. Participants hold a push button during the threshold tests which they are instructed to push it as soon as they perceive ankle movement and to indicate the direction of rotation. If they perceive the wrong rotational direction, the trial is repeated. The threshold angle required for perception of passive movement is calculated as the average of the last two trials, one in dorsiflexion and one in plantar flexion direction.
Position test measures ability to actively match the ankle angle set by the motor-driven pedal on the right side using the free moving pedal on the left side. From the neutral test position (Figure 1), participants are asked to move their left foot to match the rotation angle of the right foot that is driven by the motor. The error calculated as the absolute difference (degrees) between the left (participant driven) and right (motor driven) ankle pedals is measured after 5 s of initial setting of the motor-driven pedal. Three trials are performed in the following sequence: 5° plantar flexion, 5° plantar flexion and 5° dorsiflexion.
Tracking test evaluates the ability to track continuous passive ankle angular rotations in plantar flexion and dorsiflexion produced by the machine on the right ankle by actively rotating the free pedal of the left ankle. Participants are asked to rotate left foot to match the continuously rotating angle of the right foot. Thus, this novel test evaluates the position as well as the velocity aspect of movement. Two trials are performed with continuous repetition of plantar flexion and dorsiflexion between angles of 10°, one at a relatively slow speed (3°/s) and one at a relatively fast speed (5°/s). Waveforms were designed to generate the ankle rotation pattern using custom written software. Tracking performance is measured at each speed by calculating the cross-correlation coefficients of the ankle rotation curves obtained from the left- and right-side potentiometers.
Test–retest reliability of the three proprioception tests was examined by calculating intraclass correlation coefficients (ICCs). For reliability evaluation, the test protocol was re-administered to 27 participants 2 days following initial testing [16].
Statistical analysis
Cross-sectional associations between ankle proprioception performances and age were examined by multiple regression analysis adjusted for height and weight separately for women and men. Proprioception differences between women and men were also examined with generalised linear models (GLM) controlling for height, weight and age. Statistical analyses were performed using SAS (SAS 9.1), with significance set at P < 0.05.
Results
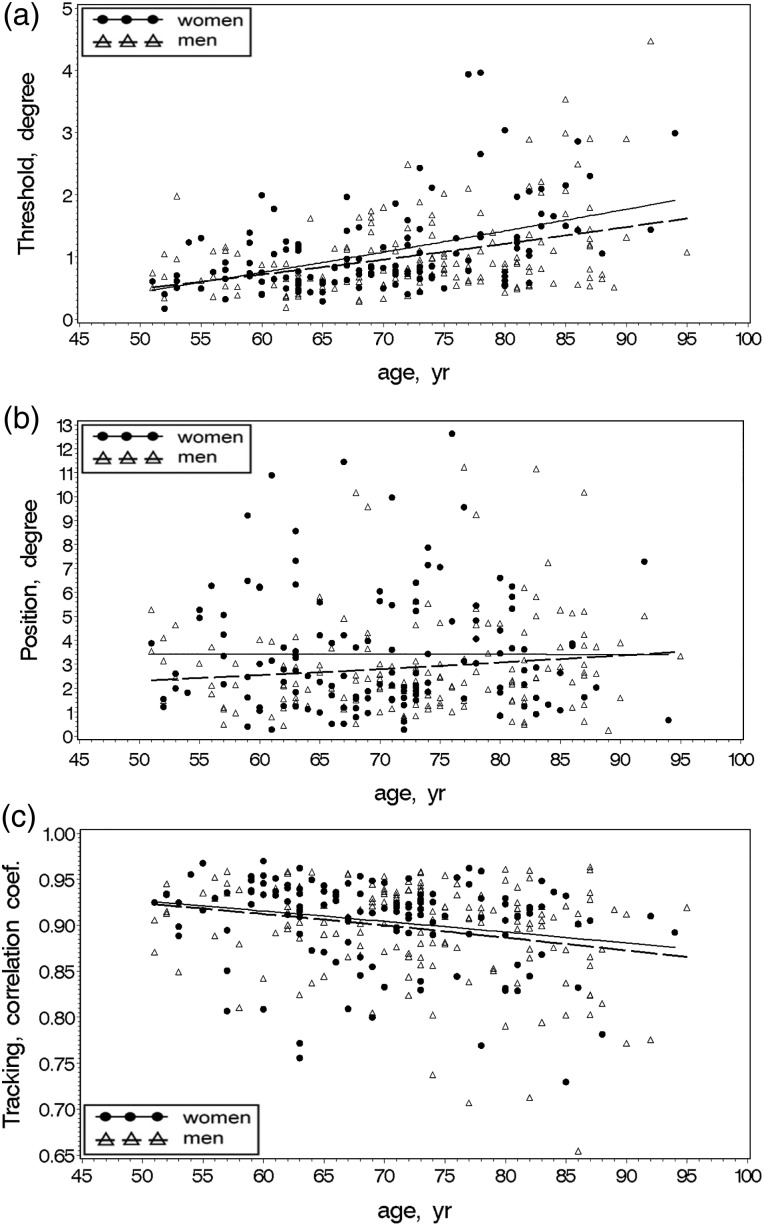
Women and men had comparable BMI, but women were younger (P = 0.004), shorter (P < 0.001) and weighed less (P = 0.001) as shown in Table 1. Repeated tasks for the same participants (N = 27) confirmed reliability of test procedures in the threshold, positioning and tracking tasks with significant correlations between same tasks with 2-day time interval (ICCs were 0.88, 0.44 and 0.65, respectively). Ankle proprioception test results with respect to age and differences between women and men are shown in the Table 2. Age-associated patterns for the threshold tests were consistent across all trials. On average, required ankle angular movement for detecting rotation in women and men was 1.11° (SE = 0.07) and 1.00° (SE = 0.06), respectively, and threshold angles for both women and men were higher with older age (P < 0.001, for both). Position matching did not vary with age for either women or men. The cross-correlation coefficients for ankle tracking performance (closer to 1 means better tracking performance) in women and men did not differ (P = 0.446) and were lower with increasing age in both women and men (P = 0.018, and P = 0.011, respectively). Age associations of tracking task performance differ between men and women, with men demonstrating age association on the slower task and women on the faster. Age associations of ankle proprioception for the threshold, position and tracking performance in women and men are depicted in Figure 2.
Table 1.
Participant characteristics
| Women (SE), N = 131 | Men (SE), N = 158 | P value | |
|---|---|---|---|
| Age, years | 70 (1) | 73 (1) | 0.004 |
| Height, m | 1.62 (0.01) | 1.74 (0.01) | <0.001 |
| Mass, kg | 71.80 (1.25) | 84.03 (1.14) | <0.001 |
| BMI, kg/m2 | 27.37 (0.39) | 27.53 (0.36) | 0.768 |
SE, standard error.
Table 2.
Age associations in ankle proprioception parameters in women and men
| Ankle proprioception variables | Age associationa |
Women and men differencesb |
|||
|---|---|---|---|---|---|
| β | P value | Mean (SE) | P value | ||
| Threshold average, degree (motor speed = 0.3°/s) |
Women | 0.036 | <0.001 | 1.11 (0.07) | 0.291 |
| Men | 0.024 | <0.001 | 1.00 (0.06) | ||
| Thresholdtest1 (3°/s, plantar flexion) |
Women | 0.063 | 0.002 | 2.48 (0.21) | 0.031 |
| Men | 0.056 | <0.001 | 1.77 (0.19) | ||
| Threshold test2 (3°/s, dorsiflexion) |
Women | 0.037 | <0.001 | 1.29 (0.11) | 0.135 |
| Men | 0.038 | <0.001 | 1.03 (0.10) | ||
| Threshold test3 (3°/s, dorsiflexion) |
Women | 0.043 | <0.001 | 1.30 (0.10) | 0.260 |
| Men | 0.039 | <0.001 | 1.28 (0.08) | ||
| Threshold test4 (3°/s, plantar flexion) |
Women | 0.029 | <0.001 | 0.93 (0.06) | 0.563 |
| Men | 0.010 | 0.016 | 0.88 (0.05) | ||
| Position average, degree (motor speed = 3°/s) |
Women | 0.001 | 0.976 | 3.51 (0.25) | 0.073 |
| Men | 0.027 | 0.124 | 2.81 (0.22) | ||
| Position test1 (5°, plantar flexion) |
Women | −0.026 | 0.342 | 2.70 (0.28) | 0.958 |
| Men | 0.015 | 0.459 | 2.68 (0.24) | ||
| Position test2 (5°, plantar flexion) |
Women | 0.045 | 0.123 | 3.25 (0.31) | 0.260 |
| Men | 0.032 | 0.159 | 2.71 (0.27) | ||
| Position test3 (5°, dorsiflexion) |
Women | −0.017 | 0.722 | 4.58 (0.45) | 0.026 |
| Men | 0.033 | 0.241 | 3.03 (0.39) | ||
| Tracking average | Women | −0.001 | 0.018 | 0.90 (0.01) | 0.446 |
| Men | −0.001 | 0.011 | 0.90 (0.00) | ||
| Tracking test1 (3°/s) |
Women | −0.001 | 0.103 | 0.92 (0.01) | 0.275 |
| Men | −0.001 | 0.004 | 0.91 (0.01) | ||
| Tracking test2 (5°/s) |
Women | −0.001 | 0.026 | 0.89 (0.01) | 0.799 |
| Men | −0.001 | 0.121 | 0.88 (0.01) | ||
Bold values indicate significant age association with P < 0.05.
β, coefficient of age association with ankle proprioception performance.
aModels are adjusted for height and mass.
bModels are adjusted for height and mass, and age.
Figure 2.
Average age associations in ankle proprioception for threshold task (a), positioning task (b) and tracking task (c) in women and men.
Discussion
The proprioception test instrument and protocol described in this study were developed to assess proprioception in the ankle joint by measuring ability to sense movement and control static and dynamic position. Partially supporting our hypothesis, ankle proprioception tests of threshold and tracking revealed poorer performance with increasing age in both women and men.
The threshold test was designed for detection of slow (0.3°/s) ankle angular movement in the sagittal plane. Previously developed ankle threshold tests have the test subject in an upright, weight-bearing position [4, 5, 15, 17]; thus, ankle rotation possibly could be detected through proprioception of any of the lower extremity joints including the hip, knee and/or ankle. Thus, detection of ankle rotation using a standing test may be less sensitive to impaired ankle proprioception [5, 18]. The threshold test performed in a seated, non-weight-bearing position, as introduced in this study, can be beneficial for assessing proprioception focussed solely on the ankle joint and can be an essential supplementary method to weight bearing or standing tests. Awareness of subtle ankle angular movement may contribute to efficient customary walking in providing a triggering cue for shock absorbing effort during initial stepping and also in assuring appropriate clearance during the swing phase. Given that weight bearing is just started or not even applied in the initial step or swing phase of gait, respectively, the critical role of ankle proprioception in the non-weight-bearing position for efficient ambulation cannot be underestimated. Thus, the finding that minimum ankle threshold angles required for detecting slow ankle angular movements are higher with increasing age has important implications for understanding the precise mechanism of gait mechanics and walking efficiency in late life and suggests a potential area of intervention for retaining mobility of older adults. Lower performance in threshold for perception of passive ankle rotation in older age in this study was consistent with a previous study using a weight-bearing standing test [4].
Unexpectedly, position test performance that captured the ability to perceive and match a pre-set static ankle position with the other ankle showed no variation with age. This lack of variation indicates that this particular approach to assessing ankle proprioception has low construct validity in addition to low test–retest reliability and would require modification before further consideration as a meaningful measure of ankle proprioception. The low test–retest reliability is consistent with this perspective. Given these issues, we cannot clearly evaluate age associations in ankle positioning performance.
In contrast, the tracking test that evaluates ability to perceive and match dynamic ankle positions continuously and simultaneously revealed a significant inverse age association for both women and men in the cross-correlation coefficients. Consistent with previous studies in ankle movement, age-associated decline in tracking performance can be interpreted as combined deterioration in the sensing and controlling of ankle angular movements of ipsilateral and contralateral sides [19, 20]. The tracking tests administered at the relatively faster speed (5°/s) and at the relatively slower speed (3°/s) revealed age associations in women and men, respectively. These results suggest that men and women may differ in tracking-related ankle proprioception tasks that could be associated with different footwear histories such as wearing high heels, for instance.
The ankle proprioception tests introduced in this study have threefold significance. First, the ease of testing due to the seated, non-weight-bearing position allows wider application of the testing protocol that is particularly important for longitudinal study. This system was designed to conduct relatively precise assessments to facilitate ascertainment of minimum potential differences or change in ankle proprioception performance over time. In addition, older adults who have or develop difficulty in standing because of balance problems or joint pain can be tested using the instrument and procedures described here. Second, by measuring proprioception in the most distal segment of the lower extremity (ankle), subtle, but more specific functional deficits, as a possible consequence of normal ageing or chronic disease can be obtained. This more narrowly focussed assessment of proprioception could be especially important for older adults with limited visual and/or vestibular function. Third, the tracking test is uniquely capable of measuring the ability to sense and control movement simultaneously which may elucidate mechanisms underlying impaired balance control associated with frequent falling highly prevalent in older adults.
This study has limitations. The ankle proprioception test instrument as currently designed has only one pedal that is motor driven, the one on the right, and one pedal that the participant can move, the one on the left. Thus, participants with the same level of proprioception who differ with regard to their dominant leg may achieve different results because of the instrument setting. Therefore, it should be noted that the reported results from this study assume symmetry in ankle activity of left and right sides. Although proprioception performance was measured from the ankle joint in a seated and non-weight-bearing position, passive and active ankle movement cannot be totally isolated from the activities of the knee and hip. Thus, existence of a small portion of other joint effects, which were not considered in this study, may have impacted the results.
In conclusion, a simple, standardised method for assessing ankle proprioception was introduced in this study using a customized test instrument, software and test protocol. Age-associated reduction in ankle proprioception was confirmed from two subtests of threshold and tracking separately for women and men. Findings in this study prompt future studies to determine whether these age-associated differences in the threshold for passive motion detection and movement tracking are evident in longitudinal study and how these specific deficits in ankle proprioception are related to age-associated chronic conditions such as knee or hip osteoarthritis and type II diabetes and affect daily activities such as gait.
Key points.
Ankle proprioception assessment.
Age-associated decline in proprioception.
Baltimore Longitudinal Study of Aging.
Conflicts of interest
None declared.
Acknowledgements
This paper was supported by the Intramural Research Program of the NIH, National Institute on Aging and Chonnam National University. Data for these analyses were obtained from the Baltimore Longitudinal Study of Aging, a study performed by the National Institute on Aging.
References
- 1.Diener HC, Dichgans J. On the role of vestibular, visual and somatosensory information for dynamic postural control in humans. Prog Brain Res 1988; 76: 253–62. [DOI] [PubMed] [Google Scholar]
- 2.Hurley MV, Scott DL, Rees J, Newham DJ. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis 1997; 56: 641–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med 1998; 25: 149–55. [DOI] [PubMed] [Google Scholar]
- 4.Deshpande N, Connelly DM, Culham EG, Costigan PA. Reliability and validity of ankle proprioceptive measures. Arch Phys Med Rehabil 2003; 84: 883–9. [DOI] [PubMed] [Google Scholar]
- 5.Gilsing MG, Van den Bosch CG, Lee SG, Ashton-Miller JA, Alexander NB, Schultz AB, Ericson WA. Association of age with the threshold for detecting ankle inversion and eversion in upright stance. Age Ageing 1995; 24: 58–66. [DOI] [PubMed] [Google Scholar]
- 6.Hurley MV, Rees J, Newham DJ. Quadriceps function, proprioceptive acuity and functional performance in healthy young, middle-aged and elderly subjects. Age Ageing 1998; 27: 55–62. [DOI] [PubMed] [Google Scholar]
- 7.Madhavan S, Shields RK. Influence of age on dynamic position sense: evidence using a sequential movement task. Exp Brain Res 2005; 164: 18–28. [DOI] [PubMed] [Google Scholar]
- 8.Skinner HB, Barrack RL, Cook SD. Age-related decline in proprioception. Clin Orthop Relat Res 1984; 184: 208–11. [PubMed] [Google Scholar]
- 9.Horak FB, Nashner LM. Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol 1986; 55: 1369–81. [DOI] [PubMed] [Google Scholar]
- 10.van Deursen RW, Sanchez MM, Ulbrecht JS, Cavanagh PR. The role of muscle spindles in ankle movement perception in human subjects with diabetic neuropathy. Exp Brain Res 1998; 120: 1–8. [DOI] [PubMed] [Google Scholar]
- 11.Ko S, Ling SM, Winters J, Ferrucci L. Age-related mechanical work expenditure during normal walking: the Baltimore Longitudinal Study of Aging. J Biomech 2009; 42: 1834–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ko SU, Stenholm S, Ferrucci L. Characteristic gait patterns in older adults with obesity-results from the Baltimore Longitudinal Study of Aging. J Biomech 2010; 43: 1104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mueller MJ, Minor SD, Schaaf JA, Strube MJ, Sahrmann SA. Relationship of plantar-flexor peak torque and dorsiflexion range of motion to kinetic variables during walking. Phys Ther 1995; 75: 684–93. [DOI] [PubMed] [Google Scholar]
- 14.Segal NA, Yack HJ, Brubaker M, Torner JC, Wallace R. Association of dynamic joint power with functional limitations in older adults with symptomatic knee osteoarthritis. Arch Phys Med Rehabil 2009; 90: 1821–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simoneau GG, Derr JA, Ulbrecht JS, Becker MB, Cavanagh PR. Diabetic sensory neuropathy effect on ankle joint movement perception. Arch Phys Med Rehabil 1996; 77: 453–60. [DOI] [PubMed] [Google Scholar]
- 16.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice, 3rd edition Upper Saddle River, NJ: Pearson/Prentice Hall, 2009. [Google Scholar]
- 17.Robbins S, Waked E, McClaran J. Proprioception and stability: foot position awareness as a function of age and footwear. Age Ageing 1995; 24: 67–72. [DOI] [PubMed] [Google Scholar]
- 18.Gurfinkel VS, Lipshits MI, Popov KE. Thresholds of kinesthetic sensation in the vertical posture. Hum Physiol 1982; 8: 439–45. [PubMed] [Google Scholar]
- 19.Ko SU, Hausdorff JM, Ferrucci L. Age-associated differences in the gait pattern changes of older adults during fast-speed and fatigue conditions: results from the Baltimore Longitudinal Study of Ageing. Age Ageing 2010; 39: 688–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwon M, Baweja HS, Christou EA. Age-associated differences in positional variability are greater with the lower limb. J Mot Behav 2011; 43: 357–60. [DOI] [PubMed] [Google Scholar]