Abstract
In January 2005, a train derailment on the premises of a textile mill in South Carolina released 42 to 60 tons of chlorine gas in the middle of a small town. Medical records and autopsy reports were reviewed to describe the clinical presentation, hospital course, and pathology observed in persons hospitalized or deceased as a result of chlorine gas exposure. Eight persons died before reaching medical care; of the 71 persons hospitalized for acute health effects as a result of chlorine exposure, 1 died in the hospital. The mean age of the hospitalized persons was 40 years (range, 4 months-76 years); 87% were male. The median duration of hospitalization was 4 days (range, 1-29 days). Twenty-five (35%) persons were admitted to the intensive care unit; the median length of stay was 3 days. Many surviving victims developed significant pulmonary signs and severe airway inflammation; 41 (58%) hospitalized persons met Po2/Fio2 criteria for acute respiratory distress syndrome or acute lung injury. During their hospitalization, 40 (57%) developed abnormal x-ray findings, 74% of those within the first day. Hypoxia on room air and Po2/Fio2 ratio predicted severity of outcome as assessed by the duration of hospitalization and the need for intensive care support. This community release of chlorine gas caused widespread exposure and resulted in significant acute health effects and substantial health care requirements. Pulse oximetry and arterial blood gas analysis provided early indications of outcome severity.
1. Introduction
Chlorine is one of the most common toxic inhalants. At room temperature, it is a yellow-green gas, more than twice as heavy as air, and moderately water-soluble. It has a detectable odor even at low concentrations and is a potent eye, skin, and respiratory irritant [1]. Chlorine reacts with water in the mucous membranes and airways to form hydrochloric and hypochlorous acids leading to acute inflammation of the conjunctiva, nasal mucosa, pharynx, larynx, trachea, and bronchi. The oxidation of functional groups in cell components and the generation of free oxygen radicals are also thought to cause cellular injury [1]. Exposure to higher concentrations may result in the development of pneumonitis, pulmonary edema, respiratory failure, and death [2].
Chlorine is also among the most commonly manufactured and widely used chemicals in the United States. Much of the 13 to 14 million tons produced each year is transported by rail, often through densely populated areas, for use at tens of thousands of sites around the country. New federal regulations on the transport of rail cargo aim to avert a deliberate attack on a chlorine storage tank, which the Department of Homeland Security (DHS) included as 1 of its 15 National Planning Scenarios. If such an attack took place in an urban setting, an estimated 100,000 hospitalizations would occur [3]. The intentional use of chlorine gas to cause widespread casualties has recently become a reality in Iraq, where there have been 9 terrorist attacks using chlorine gas since January 2007.
At 2:40 am on January 6, 2005, a freight train carrying three 90-ton tanker cars of chlorine was inadvertently switched onto an industrial spur, where it collided with a parked locomotive in the center of Graniteville, SC, a town of 7,000 persons located approximately 15 miles from Augusta, GA. The collision ruptured 1 tank, releasing between 42 and 60 tons of chlorine, which became a cloud of dense gas that stayed close to the ground and spread across the premises of a large textile mill. Within minutes, chlorine gas infiltrated mill buildings, where approximately 180 persons were working the night shift. Some workers fled outdoors, only to encounter more chlorine gas; others tried unsuccessfully to shelter in place. A short time later, workers and residents began arriving at local health care facilities.
Although occupational exposures and accidental releases in the United States occur with some frequency [4], the typical clinical presentation and course of acute chlorine gas exposure in a large group of hospitalized persons has not been well described. The objective of this investigation was to characterize hospitalizations for chlorine inhalation injury resulting from this large-scale accidental release of chlorine gas in a community. We describe the range and severity of clinical presentations, the duration of hospitalizations, and current patterns of clinical treatment. Complete details about the event, including the environmental behavior of the chlorine gas, the exposures of workers and community members, and the resulting emergency medical response and epidemiologic investigation, are described in another report [5].
2. Methods
2.1. Study design
Immediately after the chlorine release, the South Carolina Department of Health and Environmental Control (DHEC) began a rapid epidemiologic assessment to determine the health impact and target resources to the affected community. Active case finding among physicians and health care facilities in the surrounding areas was accomplished by instituting mandatory reporting of persons treated for chlorine-related symptoms. Emergency department logs, which included basic demographic information, were requested from hospitals in South Carolina and Georgia.
We reviewed the medical records of all persons hospitalized for chlorine gas exposure during January 6 to 10, for information about demographic characteristics; clinical presentation; physical examinations; laboratory, pulmonary, and radiographic studies; and medical treatment and diagnoses. We excluded 1 person who was initially hospitalized 25 days after the event. We also reviewed the reports of autopsies conducted on all deaths.
The Human Subjects Committee at the US Centers for Disease Control and Prevention approved this investigation.
2.2. Statistical analysis
We used the Kaplan-Meier estimator to describe and analyze factors associated with duration of hospitalization—the time (in days) from hospital admission to hospital discharge. Differences in duration of hospitalization across groups stratified by Po2/Fio2 category and presence of hypoxia on room air (<90% or >90% oxygen saturation on pulse oximetry) were tested using a log-rank test. χ2 tests compared the proportions of persons requiring intensive care unit (ICU) support across groups stratified by Po2/Fio2 category and the presence of hypoxia on room air.
Statistical analyses used Stata v8.2 (Stata Corp, College Station, TX) and SAS v9.1 (SAS Institute Inc, Cary, NC).
3. Results
We identified 71 persons who, within 5 days of the release, were hospitalized at 9 hospitals in South Carolina and Georgia for exposure to chlorine. Two of these hospitals received single patients as transfers from other hospitals. Eight persons died at the scene, and 1 died in hospital on the first day of hospitalization. Overall, a total of 597 persons were identified who had sought medical care at least once in hospital emergency departments (EDs) or private clinics. Additional information about health effects on these persons and the impact of the event on area health care facilities is included in another report [5].
Sixty-three (89%) persons were hospitalized on the day of the accident, 7 (10%) the day after, and 1 (1%) on the fifth day. Twenty-five persons (35%) were admitted to an ICU, where 1 died. Six (67%) hospitals admitted 1 or more persons to their ICU. Of the 24 who survived, the median length of ICU admission was 3 days (interquartile range [IQR] = 2-5.5). A total of 7 (10%) persons were intubated at 1 of 3 hospitals during their hospitalization; they spent a median of 6 days (IQR = 3-12) on the ventilator. The 70 who were discharged alive spent a median of 4 days in the hospital (IQR = 2-6) with a range of 1 to 29. The total number of hospital inpatient days was 346; of these, a total of 118 were intensive care days.
3.1. Demographic characteristics
Table 1 summarizes the demographic characteristics of the persons who as a result of chlorine gas exposure were hospitalized, died, or died while in hospital. Most of those hospitalized were men (87%), white (59%), and mill workers (62%), as were those who died. The mean age of hospitalized persons was 39 years; only 1 person younger than 18 was hospitalized. No demographic characteristic—including age, preexisting disease, or tobacco use—was significantly associated with the duration of hospitalization or the need for ICU support.
Table 1. Demographic characteristics of persons hospitalized and deceased as a result of chlorine exposure.
| Variable | No. (%) unless noted otherwise | |
|---|---|---|
|
| ||
| Hospitalized (N = 71) a |
Deceased (N = 8) |
|
| Age (y) | ||
| Mean (SD) | 39.6 (±14.1) | 42.4 (±14.2) |
| Range | 4 mo-76 y | 22-58 y |
| <18 y | 1 (1) | – |
| Sex | ||
| No. (%) male | 62 (87) | 8 (100) |
| Race | ||
| White | 42 (59) | 7 (87) |
| Black | 22 (31) | 1 (12) |
| Hispanic | 5 (7) | – |
| Other | 1 (1) | – |
| Unknown | 1 (1) | – |
| Occupation | ||
| Mill worker | 44 (62) | 6 (75) |
| Emergency medical services | 3 (4) | – |
| Railroad employee | 2 (3) | – |
| Health care worker | 1 (1) | – |
| Other | 9 (13) | 2 (25) |
| Unknown | 12 (17) | – |
| Tobacco use | ||
| Never | 27 (38) | – |
| Current | 35 (49) | 3 (37) b |
| Former | 6 (9) | – |
| Unknown | 3 (4) | 5 (62) |
| Preexisting disease | ||
| Hypertension | 19 (27) | |
| Asthma or COPD | 15 (21) | |
| Diabetes | 6 (8) | |
| Cardiomegaly c | 4 (6) | 7 (87) |
COPD indicates chronic obstructive pulmonary disease.
One person who died in hospital is included in the hospitalized group. This person represents a ninth death from the event.
Current smoking determined by evidence of cotinine in postmortem laboratory analysis.
The determination of cardiomegaly among those who died—including the person who died in the hospital—was made during postmortem examination of the heart (weight, thickness of walls). In all hospitalized persons this was reported as a radiographic finding.
3.2. Autopsy findings
Of those who died at the scene, the primary cause of death was asphyxia; in the other person the cause of death was listed as lactic acidosis and acute respiratory failure. Reported findings included congested lungs, pulmonary edema, and tracheal and bronchial erythema. Reports in 3 cases stated that the tracheobronchial tree contained a slight Chlorine gas health effects and treatment amount of frothy fluid, reddened mucosa, and purplish red and firm parenchyma. Cardiomegaly was detected during the autopsies of 8 (89%) of 9 deceased persons.
3.3. Clinical presentation and physical examinations
All 71 (100%) of those who were hospitalized presented with at least 1 pulmonary complaint. Twenty-two (31%) had cardiac complaints, 9 (13%) ocular, 11 (15%) otorhinolaryngeal, 10 (14%) gastrointestinal, and 1 (1%) dermatologic.
Table 2 summarizes the time course of principal physical findings noted during the initial physical examination in the ED and the examination at hospital admission, which occurred an average of 4 hours later. At the time of the 2 examinations, the majority of persons (>90%) had at least 1 significant pulmonary finding. The most common and persistent physical finding was wheeze; no other pulmonary findings were noted in more than half of the hospitalized persons at either examination or overall. Prevalent delayed signs include 18 (29%) persons with rales/crackles, 11 (17%) with wheeze, and 11 (17%) with ocular problems. Tachypnea (>20 breaths per minute), tachycardia (>100 beats per minute), and hypertension (systolic pressure >140 mm Hg, and/or diastolic pressure >90 mm Hg) were frequently observed, affecting between 68% and 86% of persons during at least 1 examination. In most of the persons in whom the conditions were observed, tachypnea and tachycardia persisted across examinations. Eight (13%) persons developed tachycardia and 10 (16%) developed hypertension after their ED examination.
Table 2. Distribution and acute time course of significant physical findings noted during physical examinations (n = 63) a.
| No. (%) | |||
|---|---|---|---|
|
| |||
| Immediate and persistent b | Immediate and resolved c | Delayedd | |
| Findings | |||
| Pulmonary | |||
| Wheeze | 29 (46) | 13 (21) | 11 (17) |
| Rales/crackles | 7 (11) | 6 (10) | 18 (29) |
| Cough | 6 (10) | 14 (22) | 3 (5) |
| Decreased breath sounds | 3 (5) | 13 (21) | 6 (10) |
| Rhonchi | 4 (6) | 8 (13) | 2 (3) |
| Labore breathingd | 3 (5) | 3 (5) | 1 (2) |
| Retractions | 1 (2) | – | 3 (5) |
| Ear, nose, and throat | 3 (5) | 10 (16) | 3 (5) |
| Ocular | 4 (6) | 13 (21) | 11 (17) |
| Dermatologic | – | 7 (11) | 2 (3) |
| Vital signs | |||
| Tachypnea | 29 (46) | 21 (33) | 4 (6) |
| Tachycardia | 27 (43) | 10 (16) | 8 (13) |
| Hypertension | 18 (29) | 15 (24) | 10 (16) |
A total of 63 persons had information available on physical examinations in both the ED and upon hospital admission. Percentages are calculated using the number with available information. An average of 4 hours elapsed between examinations.
Immediate and persistent: finding noted during examination in the ED and upon hospital admission.
Immediate and resolved: finding noted during examination in the ED but not upon hospital admission.
Delayed: finding only noted at examination upon hospital admission.
When their oxygen saturation was initially measured, 44 (62%) persons were on room air. Those who were hypoxic on room air, with an oxygen saturation lower than 90%, were hospitalized for a median duration of 6 days—3 times as long as those who were not hypoxic (P <.001) (Fig. 1). Only 2 (9%) of 22 persons receiving oxygen therapy when their oxygen saturations were measured were hypoxic; 1 of them died. The remaining 20 had a median length of stay of 4 (IQR = 2-6) days. We did not identify any persons with delayed hypoxia.
Fig. 1.
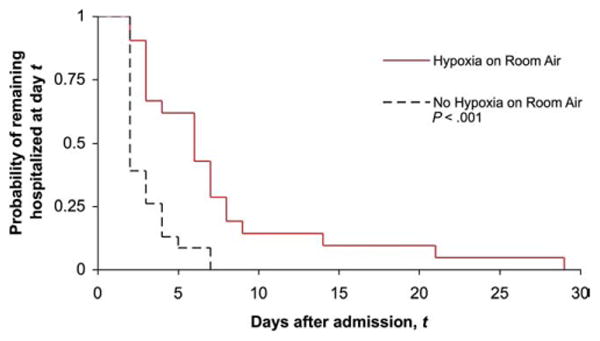
Kaplan-Meier curves illustrating probability of remaining hospitalized at time t after admission for groups stratified by presenting oxygen saturation (n = 44).
3.4. Arterial blood gas analyses, oxygenation indices, and outcomes
Table 3 summarizes values derived from the initial arterial blood gas (ABG) analysis. Among the 55 who had an ABG measurement, those with acid–base disorders had a longer median length of stay in the hospital and greater need for ICU support. Twelve (22%) of the 55 had a Po2/Fio2 ratio between 200 and 300, meeting the criteria for acute lung injury, and 29 (53%) had a ratio less than 200, meeting the criteria for acute respiratory distress syndrome (ARDS). There was an inverse relationship between the Po2/Fio2 ratio and the duration of hospital stay (P <.001; see Fig. 2) and the percentage admitted to the ICU (P = .023).
Table 3. Initial ABG values, acid–base disorders, length of stay, and intensive care requirements.
| Category | Number (%) | Length of stay, median (days) | Intensive care, number (%) |
|---|---|---|---|
| ABG analysis not performed | 16 (23) | 2 | 4 (25) |
| ABGa | 55 (77) | 5 | 21 (38) |
| pH | |||
| Mean (SD) | 7.32 (0.11) | ||
| Range | 6.73-7.55 | ||
| Acidemia | 33 (60) | 6 | 14 (42) |
| Hypercarbia | 9 (16) | 6 | 6 (67) |
| Metabolic acidosis | 9 (16) | 8 | 6 (67) |
| Respiratory acidosis | 25 (45) | 4 | 10 (40) |
| Hypoxemia | 10 (18) | 3 | 5 (50) |
| Po2/Fio2 | |||
| >300 (normal) | 14 (26) | 3 | 3 (21) |
| 200-300 (ALI) | 12 (22) | 5.5 | 2 (17) |
| <200 (ARDS) | 29 (53) | 6 | 16 (55) |
ALI indicates acute lung injury.
Acid–base disorder criteria: acidemia (pH <7.35), hypercarbia (Pco2 >55), metabolic acidosis (pH <7.35 and HCO3 <22), respiratory acidosis (pH <7.35 and Pco2 >45), hypoxemia (Po2 <60). Percentages calculated based on those receiving an ABG analysis.
Fig. 2.
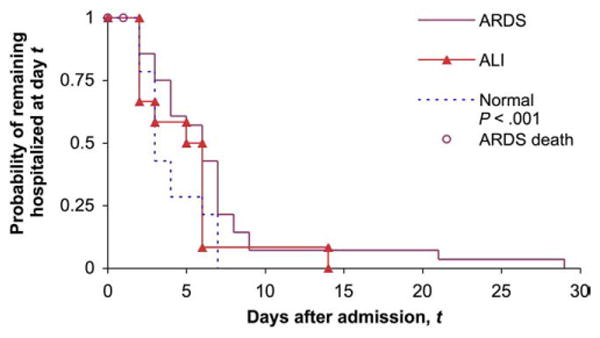
Kaplan-Meier curves illustrating probability of remaining hospitalized at time t after admission for groups stratified by presenting Po2/Fio2 ratio (n = 55).
3.5. Radiography and pulmonary investigations
Table 4 summarizes written interpretations of significant findings in radiology reports on all x-rays taken during the hospitalizations. Just less than three quarters of those who developed an abnormal finding did so within the first day of the admission, and nearly all remaining persons developed a significant finding by the end of the second day of hospitalization. Four had documented computed tomo-graphic scans of the chest; these revealed atelectasis, parenchymal densities, pulmonary edema, and bilateral consolidation. Of the 29 persons meeting the oxygenation criteria for ARDS, radiologic changes were evident in 25 (89%) of 28. Of these, 18 (72%) were noted to have infiltrates, 15 (60%) pulmonary edema, and 3 (12%) atelectasis. Bronchoscopy was performed on 4 (6%) persons and spirometry on 8 (11%) persons at least once during their hospitalization; all pulmonary function assessments demonstrated a restrictive and/or obstructive pattern.
Table 4. Chest radiograph abnormalities and day of development (n = 70).
| Category | No. (%) |
|---|---|
| Abnormal finding | 40 (57) |
| Infiltrates | 26 (37) |
| Edema | 25 (36) |
| Atelectasis | 4 (6) |
| Pneumonitis | 3 (4) |
| Cardiomegaly | 3 (4) |
| Hospital day with first abnormal finding, n = 38 a | |
| 1 | 28 (74) |
| 2 | 8 (21) |
| 3 | 1 (3) |
| 4 | 1 (3) |
Two persons with cardiomegaly had no other abnormal finding. They have been excluded from the second half of the table.
3.6. Hospital medications, discharge medications, and discharge diagnoses
Table 5 summarizes the medications that hospitalized persons received while admitted; the percentage who received each medication differed across the 4 facilities that admitted the majority (86%) of the hospitalizations. We observed similar variability across hospitals in the medications prescribed at discharge and in discharge diagnoses. The most commonly prescribed medication, inhaled β-agonists, was ordered for 67% of the hospitalized persons, followed by ipratropium bromide (44%), inhaled corticosteroids (30%), and oral corticosteroids (20%). Overall, the cohort of hospitalized persons received a combined total of 47 unique discharge diagnoses. A total of 48 (68%) persons received a diagnosis that specified chlorine exposure.
Table 5. Medications administered during hospitalization and the range of percentages of patients receiving them at the 4 hospitals that treated the most patients a.
| Medication | No. (%) | % Receiving treatment (range) |
|---|---|---|
| Oxygen | 67 (96) | 95-100 |
| Nebulized or inhaled β2-agonist | 65 (93) | 87-100 |
| Intravenous corticosteroids | 63 (90) | 66-100 |
| Ipratropium bromide | 50 (71) | 61-94 |
| Oral corticosteroids | 32 (46) | 17-61 |
| Antibiotics | 29 (41) | 11-61 |
| Inhaled corticosteroids | 20 (29) | 26-42 |
| Intravenous NaHCO3 | 8 (11) | 0-25 |
| Nebulized NaHCO3 | 2 (3) | 0-4 |
Sixty-one (86%) persons were hospitalized at one of the 4 hospitals.
4. Discussion
This report describes the presentation, treatment, and hospital course of persons exposed to chlorine gas, a common toxicant and potential terrorist agent, during a recent accidental release in a community. The strength of this report is the large size of the cohort relative to previous accounts. The resulting variation in the individuals, treatments, practitioners, and health care facilities provide insight into what could be expected in a large-scale event.
During this release, most of the deaths from acute chlorine exposure occurred within the first hours after exposure. Many surviving victims developed significant pulmonary findings suggestive of severe airway inflammation. In most patients, this quickly resolved during hospitalization, suggesting that with appropriate supportive care, patients critically ill after chlorine exposure can often be discharged within a relatively short period. By describing clinical findings from two sequential physical examinations, our report provides new information about the time course of specific signs and symptoms that can be expected to occur in a large population as a result of acute chlorine exposure.
The findings from this investigation are generally consistent with studies of persons affected by other acute chlorine gas exposures. Similar patterns of presenting complaints and physical findings have been described among hospitalized persons [2,6-9]. However, rates of significant findings during physical examination—such as wheeze and the proportion with abnormal x-rays findings—are higher in this population than in most previous reports [2,6]. This population also had decreased levels of oxygena-tion and a different profile of acid–base disorders compared with groups evaluated after other events [6,10]. The different clinical presentation and course in this group suggests that these persons had more severe health effects, possibly resulting from a more severe exposure. Indeed, the longer duration of hospitalizations and greater need for intensive care in this group compared with previously described populations supports this hypothesis [6,11]. We did not observe significant differences in the clinical presentations or outcomes of persons who reported preexisting pulmonary disease when compared with those who did not. However, the prevalence of cardiomegaly among persons who were fatally poisoned has not previously been described and warrants further investigation.
Our investigation also provides information about variability in the typical treatment of chlorine toxicity and the potential quantity of health care resources that may be required after future chlorine gas releases. Although very few treatments have a well-defined role in the treatment of acute chlorine toxicity, some treatments, such as intravenous corticosteroids and inhaled ipratropium bromide, were widely administered during these hospitalizations. Our review of the literature suggests that therapy with nebulized sodium bicarbonate [12-15] might enhance outcomes and should be considered in future mass chlorine exposures [16]. In this sample of patients hospitalized for chlorine exposure about 10% required mechanical ventilation. This suggests that if a large-scale chlorine exposure were to occur in the future, the need for mechanical ventilators may be substantial. Accordingly, provision of mechanical ventilators for a large number of victims should be an integral component of emergency planning [17]. Our report also suggests that more uniform reporting and coding on discharge summaries of the suspected chemical would improve the ability of future investigators to revisit and learn from cases related to particular exposures.
Although most of those exposed to chlorine gas recover within months and experience little or no residual dysfunction [1,2], a number of follow-up studies have suggested the potential for chlorine gas exposure to cause permanent loss of lung function or lead to the development of persistent, nonspecific bronchial hyperresponsiveness [11,18,19]. As a result, persons hospitalized and affected during this event may be able to shed light on any long-term health effects resulting from chlorine exposure. Accordingly, the DHEC has established a registry of persons potentially exposed to chlorine gas and/or traumatic stress during the event. Persons registered with the DHEC are offered free standardized medical screenings with referral for follow-up care when necessary. These screenings include physical examinations, pulmonary function testing and assessment of nonspecific bronchial hyperresponsiveness, analysis of exhaled breath condensate and exhaled nasal nitric oxide, and evaluation for posttraumatic stress disorder. In addition, investigators at the University of South Carolina Arnold School of Public Health are developing models of ambient chlorine concentrations after the release so that the magnitude of exposures and their specific health effects can be better understood.
4.1. Limitations
Although we attempted to identify everyone who received medical care for health effects resulting from chlorine exposure, it is possible that not everyone who was hospitalized was included in this investigation. It is also possible that the proportion and severity of those who were admitted (both to hospitals and to ICUs) was influenced by the mass casualty nature of the event and the capacities of area health care facilities. In different circumstances, less severely injured persons or a higher proportion of exposed persons would likely also have been hospitalized. For similar reasons, the variation observed across facilities in the treatment of hospitalized persons may reflect differences in the number or severity of people presenting to the hospitals. However, average duration of hospitalization resulting from this exposure did not differ significantly across the 4 hospitals receiving the majority of patients. Our study is also limited to information noted and found in the medical record and by the variability among physicians in the recognition or interpretation of physical signs, radiographic evidence, or other outcome variables. Finally, without knowledge of baseline medical status, it is difficult to determine the extent to which significant findings during the hospital stay represent the effects of chlorine exposure or the exacerbation of preexisting conditions.
5. Conclusions
This investigation of persons hospitalized because of this South Carolina chlorine gas release includes the largest number of chlorine-related hospitalizations in the recent medical literature. As a result, it provides information about the typical clinical presentation, treatment, and hospital course likely to result from future chlorine gas releases. In this investigation, pulse oximetry and ABG analysis provided early indications of the severity of acute health effects and health care requirements. Ongoing efforts by the DHEC to quantify the levels of chlorine exposure and monitor this population for long-term health effects will contribute to our understanding of the public health impact of chlorine gas releases.
Acknowledgments
We acknowledge the support and assistance of numerous people including Kris Bisgard, Randolph Daley, Drew Gerald, Robin Lee, David Mannino, Vuon Nguyen, Stephen Redd, Veleta Rudnick, Julie Wang, Claire Youngblood, and the health care professionals and staff at participating hospitals in South Carolina and Georgia.
Footnotes
This investigation was funded entirely by the US Centers for Disease Control and Prevention and the South Carolina Department of Health and Environmental Control.
References
- 1.Winder C. The toxicology of chlorine. Environ Res. 2001;85:105–14. doi: 10.1006/enrs.2000.4110. [DOI] [PubMed] [Google Scholar]
- 2.Das R, Blanc PD. Chlorine gas exposure and the lung: a review. Toxicol Ind Health. 1993;9:439–55. doi: 10.1177/074823379300900304. [DOI] [PubMed] [Google Scholar]
- 3.The Homeland Security Council. Planning Scenarios: Executive Summaries. 2004 [Google Scholar]
- 4.Horton DK, Berkowitz Z, Kaye WE. The public health consequences from acute chlorine releases, 1993-2000. J Occup Environ Med. 2002;44:906–13. doi: 10.1097/00043764-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Wenck MA, Van Sickle D, Drociuk D, et al. Rapid assessment of exposure to chlorine released from a train derailment and resulting health impact. Public Health Rep. 2007;122:784–92. doi: 10.1177/003335490712200610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guloglu C, Kara IH, Erten PG. Acute accidental exposure to chlorine gas in the Southeast of Turkey: a study of 106 cases. Environ Res. 2002;88:89–93. doi: 10.1006/enrs.2001.4324. [DOI] [PubMed] [Google Scholar]
- 7.Joyner RE, Durel EG. Accidental liquid chlorine spill in a rural community. J Occup Med. 1962;4:152–4. [PubMed] [Google Scholar]
- 8.Weill H, George R, Schwarz M, Ziskind M. Late evaluation of pulmonary function after acute exposure to chlorine gas. Am Rev Respir Dis. 1969;99:374–9. [PubMed] [Google Scholar]
- 9.Hedges JR, Morrissey WL. Acute chlorine gas exposure. JACEP. 1979;8:59–63. doi: 10.1016/s0361-1124(79)80038-6. [DOI] [PubMed] [Google Scholar]
- 10.Ploysongsang Y, Beach BC, DiLisio RE. Pulmonary function changes after acute inhalation of chlorine gas. South Med J. 1982;75:23–6. doi: 10.1097/00007611-198201000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz DA, Smith DD, Lakshminarayan S. The pulmonary sequelae associated with accidental inhalation of chlorine gas. Chest. 1990;97:820–5. doi: 10.1378/chest.97.4.820. [DOI] [PubMed] [Google Scholar]
- 12.Bosse GM. Nebulized sodium bicarbonate in the treatment of chlorine gas inhalation. J Toxicol Clin Toxicol. 1994;32:233–41. doi: 10.3109/15563659409017956. [DOI] [PubMed] [Google Scholar]
- 13.Douidar SM. Nebulized sodium bicarbonate in acute chlorine inhalation. Pediatr Emerg Care. 1997;13:406–7. doi: 10.1097/00006565-199712000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Sexton JD, Pronchik DJ. Chlorine inhalation: the big picture. J Toxicol Clin Toxicol. 1998;36:87–93. doi: 10.3109/15563659809162593. [DOI] [PubMed] [Google Scholar]
- 15.Vinsel PJ. Treatment of acute chlorine gas inhalation with nebulized sodium bicarbonate. J Emerg Med. 1990;8:327–9. doi: 10.1016/0736-4679(90)90014-m. [DOI] [PubMed] [Google Scholar]
- 16.Aslan S, Kandis H, Akgun M, Cakir Z, Inandi T, Gorguner M. The effect of nebulized NaHCO3 treatment on “RADS” due to chlorine gas inhalation. Inhal Toxicol. 2006;18:895–900. doi: 10.1080/08958370600822615. [DOI] [PubMed] [Google Scholar]
- 17.Hick JL, O'Laughlin DT. Concept of operations for triage of mechanical ventilation in an epidemic. Acad Emerg Med. 2006;13:223–9. doi: 10.1197/j.aem.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 18.Leroyer C, Malo JL, Infante-Rivard C, Dufour JG, Gautrin D. Changes in airway function and bronchial responsiveness after acute occupational exposure to chlorine leading to treatment in a first aid unit. Occup Environ Med. 1998;55:356–9. doi: 10.1136/oem.55.5.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lemière C, Malo JL, Boutet M. Reactive airways dysfunction syndrome due to chlorine: sequential bronchial biopsies and functional assessment. Eur Respir J. 1997;10:241–4. doi: 10.1183/09031936.97.10010241. [DOI] [PubMed] [Google Scholar]


