Abstract
Background
Considering the poor survival rate of patients with esophageal cancers, mainly due to the disease effects and surgical co morbidities, we have aimed to introduce a new method of Transhiatal Esophagectomy (THE) without mediastinal manipulation for lower third esophageal and cardial cancers. It has suggested that using this technique would decrease mentioned complications.
Methods
In this prospective study, patients with esophageal cancer who referred for surgical treatment have enrolled and undergone to new method of THE, without mediastinal manipulation. Pre and post-operative morbidities as well as the duration of procedure, duration of hospital and ICU stay have recorded. All patients have followed up or 4-40 months.
Results
In this study 53 patients with mean age of 55.2+/-10.3 years have undergone esophagectomy, and then in 50 of them the new method has performed. Median operative time and volume of blood loss was 120 minutes and 130 ml, respectively. Median duration of hospital and ICU stay was 7 and 1 day, respectively. There were no Pre-operative mortalities, arrhythmia, hemodynamic instability and mediastinal vessels injury. The most common co morbidities have related to our new method were mediastinal pleura injury, anastomotic leaks and anastomotic narrowing with 20%, 16% and 10% reported rate, respectively.
Conclusion
The findings of current study have indicated that transhiatal esophagectomy without mediastinal manipulation, has represented a safe and effective method for treatment of lower third esophageal and cardial cancers due to its potential advantages of decreased blood loss, being a less traumatic procedure, minimal cardiopulmonary complications and low rate of hospital mortality.
Keywords: Transhiatal Esophagectomy, arrhythmia, hypotension, morbidity
Introduction
Esophageal carcinoma has been one of the most common gastrointestinal cancers. It would be a devastating disease and has considered as the sixth leading causes of morbidity and mortality worldwide [1, 2].It has estimated that 450000 people worldwide have affected by the disease and its incidence rate has shown an increasing trend during last decades [3].
Reported 5-year survival for the disease has ranged from 15% to 25% [4].The survival rate in Iran and most developing countries were less than their counterparts in developed countries [5, 6].
Surgery would be the most common and important treatment approach in this group of patients which provided proper disease free survival and quality of life as most of the patients have diagnosed in progressive or metastatic stages of the cancer [7].
There were two main surgical options for resection of esophageal carcinoma including transthoracic (TTE) and transhiatal esophagectomy (THE) and combination of the two methods [8]. Depending to the location of the tumor and preference of the surgeon one of the options should be selected. There were many evidences which indicated the superiority of transhiatal esophagectomy than traditional esophagectomy [9, 10].
Though THE would be a wildly used but some complication related to the method have reported. However, mediastinal manipulation during THE might result in arrhythmia and hypotension [11].
Then, several minimally invasive transhiatal (MIE) techniques have developed to reduce the comorbidities of THE. Different MIE methods have aimed to minimize mentioned complications in combination with the advantages of transhiatal esophagectomy [12, 13].
There were many controversies regarding the advantages of various MIE methods and as reported in a recent review study, there would be no evidence that MIE could be a better alternative for other conventional esophagectomy techniques [14].
Considering the lower survival rate of patients with esophageal cancer and surgical co morbidities, in this study we have aimed to introduce a new method of THE without mediastinal manipulation for lower third esophageal and cardial cancers. It has suggested that using this technique would decrease mentioned complications.
Materials and Methods
In this prospective study, patients with esophageal cancer who has referred to al-Zahra hospital, affiliated to Isfahan University of Medical Sciences, for surgical treatment from 2011-2014 have enrolled.
The diagnosis and staging of the cancer has performed according to the AJCC classification [15]. Patients with lower third esophageal and cardial cancers have included. Pre-operative upper GI endoscopy and CT scan of chest and abdomen with IV contrast have performed for clinical staging of the malignancy. Evaluation of cardiopulmonary system has done for all patients. Patients with definite cardiac arrhythmia , CHF , FEV1 < 2 lit or history of recent cardiac MI have excluded .In addition patients with serum albumin <3.5gr/dl and Hb<10mg/dl have excluded also.
After describing the method of the surgery, written informed consent has obtained from each patient.
All selected patients have undergone the new method, transhiatal esophagectomy without mediastinal manipulation. Details of the method have explained bellow. Pre and post-operative morbidities as well as the duration of procedure, duration of hospital and ICU stay have recorded. All patients have followed up or 4-40 months.
Surgical technique
After induction of general anesthesia, patients have placed in supine position. Head has placed in hyperextended position and turned to the right and stabilized with an O-ring padded foam protector. The skin has prepped from the left ear to the pubis and laterally to the mid axillary lines .An upper midline incision has made from the xiphoid to the umbilical region.
The stomach has completely released based on the right gastroepiploic artery without any manipulation on pylori. A nasogastric tube has inserted .Hiatus has widened or opened and cardial region and lower third esophageal tumor has released by gentle finger dissection. Vagus nerves have cut.
The cervical esophagus has released with the NG tube in it and then cut from thoracic inlet with 360 degree and then the distal part of the esophagus has fixed to the NG tube.
The abdominal end of NG tube has pulled above through gastroesophasieal junction for the lower third esophageal cancers and through fundus for cardial cancer.
Then, the fixed esophagus has exverted with a gentle traction on the NG tube. After resection the esophagus or esophagus and cardial region stomach has repaired and pulled up via posterior mediastinum as gastric tube. Finally anastomosis has performed in the neck (Figure1 and 2).
Figure 1.
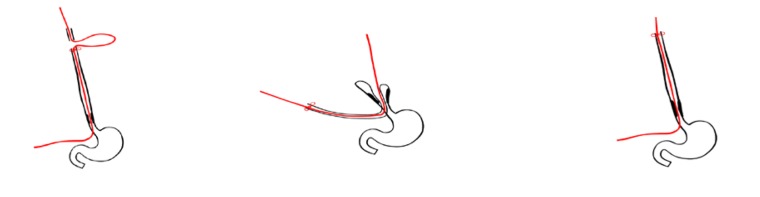
The new method of surgery, transhiatal esophagectomy without mediastinal manipulation.
Figure 2.
The new method of surgery, transhiatal esophagectomy without mediastinal manipulation.
Statistical analysis
Data has analyzed by using SPSS version 18 (SPSS Inc., Chicago, IL, U.S.A.). Mean/median has calculated for continuous variables. Frequencies have calculated for descriptive statistics.
Results
During this study 53 patients (30 men and 23 women) have undergone esophagectomy. Mean age of patients was 55.2+/- 10.3 years. All patients had stage III esophageal cancer at lower part of esophagus (16 patients) and cardial (37 patients).The histopathology of esophageal cancer at lower part of esophagus and cardial were squamus cell carcinoma and adenocarcinoma, respectively.
In selected 53 patients, 50 have undergone the new modified transhiatal esophagectomy. Reminder 3 patients have undergone transhiatal esophagectomy, because we have needed mediastinal manipulation for releasing and resection of esophagus.
Pre and post-operative complications, duration of hospital and intensive care unit stay and operative time have presented in Table1.
Table 1.
Pre and post-operative complications, duration of hospital stay and operative time in patients whose have undergone transhiatal esophagectomy without manipulation in mediastinum.
| Hospitalization[median(range)] | |
| -Duration of hospital stay(days) | 7 (5-10) |
| -Duration of ICU stay(days) | 1 (1-3) |
|
| |
| Operation | |
| - Operative time(min) | 115 (90-120) |
| -Volume of blood loss(ml) | 130 (100-150) |
|
| |
| Pre and post-operative complications | |
| - Arrhythmia | 0 (0%) |
| - Hemodynamic instability | 0 (0%) |
| - Meditational vessels injury | 0 (0%) |
| - Mediastinal pleura injury | 10 (20%) |
| - Anastomotic leaks | 8 (16%) |
| - Anastomotic narrowing | 5 (10%) |
| - Chyle leak | 0 (0%) |
For 10 patients with mediastinal pleura injury, we have used tube thoracostomy and managed them conservatively. There was not any mortality for these cases.
Patients with post-operative anastomotic leaks have managed conservatively.
During follow up, anastomotic narrowing has reported in 5 patients who have managed using balloon dilatation.
Discussion
In this study we have reported a new modified transhiatal esophagectomy without mediastinal manipulation in Isfahan. Our findings have indicated that the new introduced method had no operative mortality and less related co morbidity.
As mentioned different minimally invasive esophagectomy methods have introduced in order to minimize post-operative morbidity. Different studies have indicated that minimally invasive esophagectomy have improved the short term outcomes of the procedure, whereas they have not shown significant superior effect for long term and oncologic outcomes to TTE or THE. However, the methods had their own complications and also have considered as a high cost procedure [16-18].
In this study, we have introduced our new experience with a modified THE, with minimal or without mediastinal manipulation in order to provide better outcome for patients with lower comorbidities and low cost.
In this study, the rate of primary and post-operative morbidity was 0%, which was similar to the results of some minimally invasive esophagectomy methods and also better than many others [19, 20].
The duration of hospital stay and ICU stay in our introduced procedure has ranged between 5-10 days and 1-3 days, respectively. Our results were similar to the results of many minimally invasive esophagectomies such as robotically assisted laparoscopic transhiatal esophagectomy and laparoscopic transhiatal esophagectomy [21, 22]. Our results were similar to the results of Rizvi et al. in Pakistan [23].
One of the advantages of this method was the short operative time. It was shorter than many reported operative time for minimally invasive esophagectomy methods. The reported ranges were between 200-350 minutes. In our previous report regarding the outcomes of THE, mean of operative time was 106 minutes [24].
Median of blood loss was 130 ml (100-150ml).It was lower than TTE and THE and higher than minimally invasive esophagectomy methods. Mean of blood loss in our previous experience from THE was 506 ml [24].
We have not found any cases with arrhythmia, hemodynamic instability and mediastinal vessels injury. In a recent study in Pakistan 1.96% of patients undergone minimally invasive esophagectomy have reported arrhythmia [23]. In a Robotically assisted laparoscopic transhiatal esophagectomy method 2 out of 18 patients have reported arrhythmia. Rate of arrhythmia from THE in our center was 50. 8% during and 11.2% after mediastinal manipulation [24].
The most common co morbidities related to our new method were mediastinal pleura injury, anastomotic leaks and anastomotic narrowing with 20%, 16% and 10% reported rate, respectively. In the study of Rezvi et al. anastomotic leaks and anastomotic narrowing has seen in 5.88% and 9.80% of patients. In a robot-assisted transhiatal esophagectomy, the rate of anastomotic stricture (n=7), and anastomotic leak (n=10), was 67.5% and 25%, respectively. The comparison of our findings with the others has indicated that though they have considered as major complications of the method, but the rate would be lower than that reported by other surgical approaches.
The limitation of current study was small sample size of patients. It could justified by the fact that the method was our first experience and it has considered as pilot study.
The findings of current study has indicated that transhiatal esophagectomy without mediastinal manipulation has represented a safe and effective method for treatment of lower third esophageal and cardial cancers, due to its potential advantages of decreased blood loss, a less traumatic procedure , and minimal cardiopulmonary complications and low rate of hospital mortality.
Conclusion
Considering the low survival rate due to the nature and pre-operative complications of esophageal cancer, the best method for resection would be T.H.E for locally advanced lower third and cardial tumor but manipulation of mediastinal structure during esophagectomy causes arrhythmia and hypotension that might be dangerous. To reduce these complications, we have explained this new method that have examined on 50 patients. This method would be easy and safe, and then we have not found such as this complications.
Acknowledgments
There is no acknowledgment.
Footnotes
Conflicts of Interest
There is no conflict of interest in this article.
REFERENCES
- 1.Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381(9864):400–12. doi: 10.1016/S0140-6736(12)60643-6. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 3.Lepage C, Rachet B, Jooste V, Faivre J, Coleman MP. Continuing rapid increase in sophageal adenocarcinoma in England and Wales. . Am J Gastroentero. 2008;103:2694–99. doi: 10.1111/j.1572-0241.2008.02191.x. [DOI] [PubMed] [Google Scholar]
- 4.Pennathur A, Farkas A, Krasinskas AM. Esophagectomy for T1 esophageal cancer: outcomes in 100 patients and implications for endoscopic therapy. Ann Thorac Surg. 2009;87:1048–55. doi: 10.1016/j.athoracsur.2008.12.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mir MR, Rajabpour MV, Delarestaghi MM, Hadji M, Harirchi I, Mir P, Mir A, Lashkari M, Zendehdel K. Short- and long-term survival of esophageal cancer patients treated at the Cancer Institute of Iran. Dig Surg. 2013;30(4-6):331–6. doi: 10.1159/000354854. [DOI] [PubMed] [Google Scholar]
- 6.Harirchi I, Kolahdoozan S, Hajizadeh S, Safari F, Sedighi Z, Nahvijou A, Mir MR, Mousavi SM, Zendehdel K. Esophageal cancer in Iran; a population-based study regarding adequacy of cancer surgery and overall survival. Eur J Surg Oncol. 2014;40(3):352–7. doi: 10.1016/j.ejso.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Pennathur A, Luketich JD. Resection for esophageal cancer:strategies for optimal management. Ann Thorac Surg. 2008;85:751–56. doi: 10.1016/j.athoracsur.2007.11.078. [DOI] [PubMed] [Google Scholar]
- 8.Pennathur A, Zhang J, Chen H, Luketich JD. The “best operation”for esophageal cancer? Ann Thorac Surg. 2010;89:2163–67. doi: 10.1016/j.athoracsur.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davies AR, Forshaw MJ, Khan AA, Noorani AS, Patel VM, Strauss DC, Mason RC. Transhiatal esophagectomy in a high volume institution. World J Surg Oncol. 2008;6:88. doi: 10.1186/1477-7819-6-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang AC, Ji H, Birkmeyer NJ, Orringer MB, Birkmeyer JD. Outcomes after transhiatal and transthoracic esophagectomy for cancer. Ann Thorac Surg. 2008;85(2):424–9. doi: 10.1016/j.athoracsur.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Nikbakhsh N, Amri P, Shakeri A, Shakeri A. Changes in blood pressure and heart rhythm during transhiatal esophagectomy. Caspian J Intern Med. 2012;3(4):541–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Mallipeddi MK, Onaitis MW. The contemporary role of minimally invasive esophagectomy in esophageal cancer. Curr Oncol Rep. 2014;16(3):374. doi: 10.1007/s11912-013-0374-9. [DOI] [PubMed] [Google Scholar]
- 13.Sundaram A, Geronimo JC, Willer BL, Hoshino M, Torgersen Z, Juhasz A, Lee TH, Mittal SK. Survival and quality of life after minimally invasive esophagectomy: a single-surgeon experience. Surg Endosc. 2012;26(1):168–76. doi: 10.1007/s00464-011-1850-7. [DOI] [PubMed] [Google Scholar]
- 14.Herbella FA, Patti MG. Minimally invasive esophagectomy. World J Gastroenterol. 2010;16(30):3811–5. doi: 10.3748/wjg.v16.i30.3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rice TW, Blackstone EH, Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol. 2010;17(7):1721–4. doi: 10.1245/s10434-010-1024-1. [DOI] [PubMed] [Google Scholar]
- 16.D'Journo XB, Thomas PA. Current management of esophageal cancer. J Thorac Dis. 2014;6(Suppl 2):S253. doi: 10.3978/j.issn.2072-1439.2014.04.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoppo T, Jobe BA, Hunter JG. Minimally invasive esophagectomy: the evolution and technique of minimally invasive surgery for esophageal cancer. World J Surg. 2011;35(7):1454–63. doi: 10.1007/s00268-011-1049-z. [DOI] [PubMed] [Google Scholar]
- 18.Dhamija A, Dhamija A, Hancock J, McCloskey B, Kim AW, Detterbeck FC, Boffa DJ. Minimally invasive oesophagectomy more expensive than open despite shorter length of stay. Eur J Cardiothorac Surg. 2014;45(5):904–9. doi: 10.1093/ejcts/ezt482. [DOI] [PubMed] [Google Scholar]
- 19.Galvani CA, Gorodner MV, Moser F, Jacobsen G, Chretien C, Espat NJ, Donahue P, Horgan S. Robotically assisted laparoscopic transhiatal esophagectomy. Surg Endosc. 2008;22(1):188–95. doi: 10.1007/s00464-007-9441-3. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen NT, Hinojosa MW, Smith BR, Chang KJ, Gray J, Hoyt D. Minimally invasive esophagectomy: lessons learned from 104 operations. Ann Surg. 2008;248(6):1081–91. doi: 10.1097/SLA.0b013e31818b72b5. [DOI] [PubMed] [Google Scholar]
- 21.Dunn DH, Johnson EM, Morphew JA, Dilworth HP, Krueger JL, Banerji N. Robot-assisted transhiatal esophagectomy: a 3-year single-center experience. Dis Esophagus. 2013;26(2):159–66. doi: 10.1111/j.1442-2050.2012.01325.x. [DOI] [PubMed] [Google Scholar]
- 22.Maas KW, Biere SS, Scheepers JJ, Gisbertz SS, van-der-Peet DL, Cuesta MA. Laparoscopic versus open transhiatal esophagectomy for distal and junction cancer. Rev Esp Enferm Dig. 2012;104(4):197–202. doi: 10.4321/s1130-01082012000400005. [DOI] [PubMed] [Google Scholar]
- 23.Rizvi FH, Rizvi SS, Syed AA, Khattak S, Khan AR. Minimally invasive esophagectomy for esophageal cancer: the first experience from Pakistan. Int J Surg Oncol. 2014;2014:864705. doi: 10.1155/2014/864705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tabatabaie SA , Hashemi SM,, Mohajeri Gh,Ahmadinejad M, Goharian V, Kolahdoozan M.,Sehhat S, Davarpanah AH. Incidence of Hypotension and Type of Arrhythmia in Transhiatal Esophagectomy and Evaluation of Related Factors. Iranian Journal of Surgery. 2009;16(4):59–68. [Google Scholar]



