Abstract
Tattooing is a process of implantation of permanent pigment granules in the skin. Tattoos can be decorative, medical or accidental. There has been a exponential increase in decorative tattooing as a body art in teenagers and young adults. Unfortunately there are no legislations to promote safe tattooing, hence complications are quite common. Superficial and deep local infections, systemic infections, allergic reactions, photodermatitis, granulomatous reactions and lichenoid reactions may occur. Skin diseases localised on the tattooed area, such as eczema, psoriasis, lichen planus, and morphea can be occasionally seen. When used as a camouflage technique, colour mismatch and patient dissatisfaction are common complications. On the other hand, regrets after a tattoo are also seen and requests for tattoo removal are rising. Laser tattoo removal using Q-switched lasers are the safest; however, complications can occur. Acute complications include pain, blistering, crusting and pinpoint hemorrhage. Among the delayed complications pigmentary changes, hypopigmentation and hyperpigmentation, paradoxical darkening of cosmetic tattoos and allergic reactions can be seen. Another common complication is the presence of residual pigmentation or ghost images. Scarring and textural changes are potential irreversible complications. In addition, tattoo removal can be a prolonged tedious procedure, particularly with professional tattoos, which are difficult to erase as compared to amateur tattoos. Hence the adage, stop and think before you ink holds very much true in the present scenario.
KEYWORDS: Complications, tattoo, laser tattoo removal
INTRODUCTION
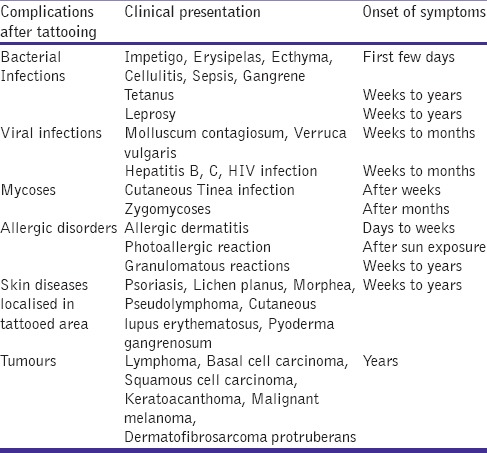
The term tattooing is derived from “tattau”, a Tahitian word which translates essentially as “to mark” and is a process of implantation of permanent pigment granules in the skin.[1] It may be done intentionally for cosmetic purposes (decorative tattoos and permanent makeup) or therapeutic purposes (medical tattoos), or introduced accidentally (traumatic tattoos), in case of abraded skin injuries. Although tattooing is an ancient practice, there has been a dramatic increase in recent times among teenagers and young adults, as a cosmetic and decorative body art form. It is also being used as a form of ‘permanent makeup’ by beauty salons. Medical therapeutic tattooing has been used as a camouflage technique in vitiligo, for breast areola reconstruction after cancer surgery, as camouflage for permanent hair loss after craniofacial surgery, and scars following plastic and reconstructive surgery. There are currently few requirements or regulations and no legislation for the safety of tattoos. Sterility of the pigments and equipment is an uncertainty as many are being performed on the roadside and in makeshift salons. Consequently, the number of reported adverse reactions after tattooing has increased. These are often seen by physicians, but are generally unknown to the public.[2] The most common skin reactions to tattooing reported in the literature include a transient acute inflammatory reaction due to trauma of the skin with needles and medical complications such as superficial and deep local infections, systemic infections, allergic contact dermatitis, photodermatitis, granulomatous and lichenoid reactions, and skin diseases localised on tattooed area, such as eczema, psoriasis, lichen planus and morphea[3,4,5,6,7] [Table 1].
Table 1.
Dermatologic disorders and complications after tattooing[7]
In addition there has been an exponential increase in patients seeking removal of tattoos for various psychosocial reasons, especially when names are tattoed and patients have a change of heart or a change of faith in case of religious symbols. Many occupations such as the armed forces prohibit the presence of tattoos and youngsters seek tattoo removal. It has been rightly sung by Jimmy Buffett, an American singer that a tattoo is a permanent reminder of a temporary feeling. Many people who get a tattoo will eventually want to get rid of it. Tattoo removal can also be a tedious prolonged procedure, particularly professional tattoos, hence there is an urgent need to caution youngsters before they get themselves a tattoo.
COMPLICATIONS OF MEDICAL TATTOOS
Tattoos by physicians are used in certain medical conditions for camouflage, like resistant vitiligo,[8] breast areola reconstruction following surgery, scar camouflage following burns or surgery and hair camouflage for permanent hair loss following radiation or craniofacial surgery. In these settings infections are less common as compared to decorative tattoos as they are carried out in sterile environments, but general complications of tattoos can still occur. The commonest complications are changes in colour, leading to colour mismatch. In vitiligo it is essential to get a good cosmetic skin-coloured tattoo matching with the surrounding normal skin. This requires a great degree of skill and often a colour mismatch leads to worsening appearance of the patch and a dissatisfied patient [Figure 1]. This is more common on the lips, exposed skin and the acral areas. The colour can fade if the pigment is placed superficially or it can appear bluish due to the Tyndall effect if it is placed too deep [Figure 2]. Tattooing should be avoided when the skin is tanned, as when the tan fades, the tattoo will appear darker than the surrounding skin. Management for a mismatched tattoo in vitiligo is skin grafting if the tattoo fades, though it is difficult to cover the tattoo adequately if it is deep in the dermis. Small patches can be excised, followed by suturing.
Figure 1.

Colour mismatch of a skin-coloured tattoo on the exposed area used as a camouflage technique for vitiligo
Figure 2.

Fading of the tattoo and bluish discolouration due to Tyndall effect on a patch of vitiligo
COMPLICATIONS OF DECORATIVE TATTOOS
These occur mainly due to the unsterile pigments that are implanted and unsterile conditions in which they are carried out. Different reactions have different times of onset as few of them appear immediately after the procedure and some may take days to weeks to years to appear [Table 1].
INFECTIONS
Tattooing involves physical injury to the skin that may promote the transdermal transmission of viral and bacterial infections, depending on the conditions of hygiene during tattooing. There are three potential origins of infections after tattooing. Firstly, use of contaminated tattoo ink. Secondly, inadequate disinfection of the skin area to be tattooed because of which resident skin bacteria can enter the skin during the tattooing process. Thirdly, during the healing process of the injured tissue after tattooing, patients often develop pruritus and burning.[9] This increases the risk of superinfection of the tattooed skin area due to scratching and therefore inoculating microorganisms.[10]
Viral diseases
Transmission of hepatitis B and C virus,[11,12] human immunodeficiency virus (HIV),[13] human papillomavirus (HPV),[14] molluscum contagiosum virus[15] and herpes simplex virus (HSV)[10] infection has been described. In a meta-analysis it was reported that there is an increased risk of infectious complications like hepatitis C when tattooing was not done in professional parlors.[11] There was no definite evidence when it was performed in professional parlours.
Bacterial infections[10,16]
Bacterial infections related to tattooing comprise infection by Streptococcus pyogenes leading to impetigo, erysipelas and even septicaemia, Staphylococcus aureus causing the rare toxic shock syndrome, skin and soft tissue infections caused by community-acquired methicillin-resistant S. aureus (CA-MRSA), treponema pallidum causing syphilis, infections with atypical mycobacteria[17] and even Mycobacterium leprae which causes leprosy. A study of 31 female patients with leprosy lesions starting over tattoo marks was reported from a leprosy endemic area from India.[18] In most cases, improper use of hygiene regimens, particularly contaminated needles are causal, but sometimes, contaminated pigments are implicated.
Fungal infections
A case of zygomycosis was observed after tattooing.[19] Severe systemic mycoses can be transmitted rarely by tattooing. A case of Candida endophthalmitis in a 40-year-old asplenic man after tattooing has been described.[20]
Allergic and foreign body reactions
Classic pigments and their degradation products used in tattooing, such as dichromate (green), cobalt (blue), cadmium (yellow) and mercury salt (red)-based pigments are responsible for these kind of reactions with permanent tattoos. In addition, contamination of pigments with nickel sulphate can cause marked allergic reactions.[16] Other potential allergen sources are organic ingredients in tattoo pigments, such as azo dyes and quinacridon.[16,20,21,22]
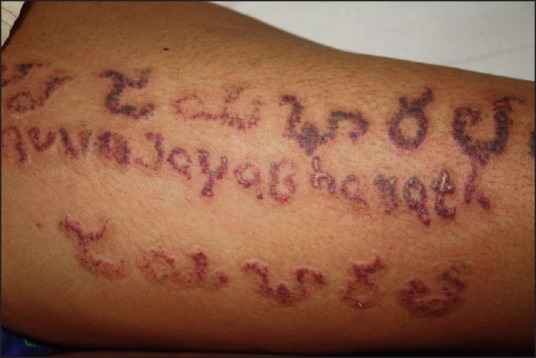
The introduction of foreign substances into the skin during tattooing can promote a toxic or an immunological response. The timing of these delayedtype hypersensitivity reactions may vary from shortly after the tattoo application up to several years later and may be triggered by retattooing.[10] Rarely generalised reactions may occur due to autosensitisation that can explain why the tattoo reactions become generalised, A localised hypersensitivity reaction stimulates the immune system causing distant skin eruptions.[23] Clinical picture is quite variable and includes eczematous, lichenoid, pseudolymphomatous lesions, contact urticaria like reactions or photoallergic reactions [Figure 3].[10,16] Patch tests unfortunately often show negative results, maybe because suitable patch test solutions are difficult to obtain owing to the low dispersing capacities of most pigments. To increase positive patch test reactions, tape stripping, late readings, and photopatch testing particularly for red pigments are recommended. The immunologic mechanisms involved are still a subject of speculation. A specific allergic pathway with a dermal-immunologic pattern is assumed, which probably bypasses the mechanisms in place in transepidermal allergen penetration. Therefore, additional intracutaneous testing, obviously including late readings, are required.[10]
Figure 3.

Photoallergic reaction in a red tattoo
On biopsy, various types of histopathologic patterns have been reported in tattoo reactions. These include lichenoid, eczematous, granulomatous and pseudolymphomatous reactions, most of which are confined to the areas of the tattoo. Granulomatous reactions after tattooing can be subdivided into two main categories: Sarcoidal granulomas and other granulomatous reactions, e.g., foreign body granulomas.[10] Sarcoidal granulomas can occur either as an isolated reaction in tattooed skin or they can represent the first visible signs of systemic sarcoidosis.[10,24]
Besides the classic patterns of reactions in tattoo intolerance or allergy, cases of morphea-like lesions and marked pseudoepitheliomatous hyperplastic lesions have been described.[25,26]
Henna tattoos mixed with p-phenylenediamine (PPD) to produce black colour can produce acute allergic contact dermatitis which may be accompanied by systemic reactions, for example, generalised lymphadenopathy and fever.[16]
Tumours
Benign lesions such as seborrheic keratosis, histiocytofibroma, epidermal cysts and milia are well known after tattooing but are rarely published.[10,27] Malignant lesions complicating tattoos include basal cell carcinoma, keratoacanthoma, squamous cell carcinoma, malignant melanoma and dermatofibrosarcoma protuberans.[10] In one case, a primary non-Hodgkin lymphoma arose in a tattoo.[28] In view of the large number of people that have tattoos and the few cases of malignant lesions that have been reported so far, at present, the association might be coincidental. Numerous factors could be involved, including intradermal injection of potentially carcinogenic substances (benzapyrene in black tattoo ink), exposure to UV radiation and genetic factors. True association is difficult to study and detect. Dark black tattoos may impede a correct clinical and dermatoscopic evaluation, and can mask the development of new melanocytic lesions or the change of existing nevi. Another problem arises when tattoos are removed by laser therapy. Tattoo pigments are phagocytosed by macrophages and are transferred to regional lymph nodes. Therefore, tattoo pigments in draining lymph nodes can be confused with metastatic changes. In case of a concurrently evident malignant melanoma, a histologic pigment analysis is recommended. Moreover, tattoos may be used to cover up suspect lesions which can cause delay in diagnosis.
Miscellaneous cutaneous complications after tattooing
Tattooing can lead to koebnerisation in patients with active psoriasis,[29,30] lichen planus and vitiligo. Tattooing can lead to reactivation of infections such as herpes simplex and herpes zoster, subacute cutaneous and discoid lupus erythematosus[31,32] and pyoderma gangrenosum.[33]
Psychosocial complications
Most tattoos are a result of peer pressure and following media personalities such as actors, sportspersons, etc. Teenagers get themselves tattooed without thinking of the consequences. Getting tattoos of the names of the current love interest leads to a lot of psychological distress if there is a change of heart. Social complications arise when religious symbols are tattooed and if patients desire a change. Dissatisfaction or boredom with an existing tattoo also leads to patients seeking tattoo removal. Feelings of low self esteem, stigmatisation and anxiety are common in patients seeking tattoo removal.[10]
Management
With the increasing incidence of tattooing as a fashion trend in society, clinicians should be able to recognise and treat those complications at the earliest and also appropriately counsel their patients on risks of tattoo placement. Thorough clinical history and examination are essential to make a diagnosis. To confirm the diagnosis, skin biopsy is mandatory, especially with a papulonodular growth within the tattoo pigment, since neoplastic conditions are not immediately recognised with clinical examination only.
Diagnostic procedures to prove allergic reactions to tattoo colours remain challenging due to the numerous and usually unknown substances in the tattoo inks. So patch testing, as performed in several studies to confirm the diagnosis of allergic reactions, might not be the appropriate approach in tattoos.[10] Allergic reactions can be treated with topical, intralesional or systemic corticosteroids. Topical tacrolimus is useful for lichenoid reactions.[34] Generalised allergic reactions have been reported to subside spontaneously after skin biopsy.[35] Bacterial infections can be confirmed by appropriate cultures and managed accordingly. Viral and fungal infections can be treated by appropriate antivirals and antifungals, respectively. Surgical removal of tumours is done depending on the site and size of the lesion with or without lymph node removal in case of metastases. Active disease needs to be treated in case of koebnerisation with appropriate therapy.
PREVENTION OF COMPLICATIONS
A majority of the complications of tattooing can be prevented by following proper guidelines. Strict aseptic precautions are important to prevent bacterial, viral and fungal infections. The instruments should be sterile and preferably all disposables should be used to prevent transmissible infections such as Hepatitis B, C and HIV infection and leprosy. There are regulations that restrict blood donation following a tattoo. The period varies from 4 months to 1 year in different counties. In India the regulation is that blood donation should be avoided within 6 months after getting a tattoo in order to avoid the risk of transmissible infections.[36] Thorough cleaning of the skin to be tattoed is mandatory to prevent resident organisms of the skin from being introduced in the dermis. The inks should be sterile and of good quality without extraneous contaminants to reduce the incidence of allergic and granulomatous reactions. The tattooing should be carried out by trained personnel, so that the pigment is placed in the proper depth. This is important especially in medical tattoos where colour matching with the surrounding normal skin is essential to achieve good cosmesis. To facilitate easy removal special tattoo inks are available which can be easily destroyed using fewer laser treatments[37] (Infinitink Freedom Inc., Cherry Hill, NJ). This contains bioresorbable dyes encapsulated in polymethylmethacrylate beads with pigments specially designed to permit targeting of the tattoo by specific laser wavelengths.
COMPLICATIONS OF TATTOO REMOVAL
Q-switched lasers have now become the standard for removal of tattoos. However complications can occur, with an incidence of about 5%.[38] On delivery of the laser in the skin, the energy that is absorbed by the pigment is converted to heat, which is the photothermal effect. There is breakage of chemical bonds inside the pigment, which is the photochemical effects. There is a mechanical destruction of the pigments due to photoacoustic effects. Small pigment particles, unknown decomposition products and newly generated chemical compounds are then removed from the skin via blood vessels or the lymphatic system. Pigments remaining in the skin may exhibit different chemical characteristics as compared to nonirradiated pigments again stimulating a reaction of the immune system. Some tattoo pigments containing metals could theoretically break down into toxic chemicals in the body when exposed to light. This has not yet been reported in vivo but has been shown in laboratory tests. It has also been shown that carcinogenic amines are generated by a laser-induced cleavage of azo dyes.[39] The complications of laser tattoo removal can be divided into immediate and delayed [Table 2].
Table 2.
Complications of laser tattoo removal
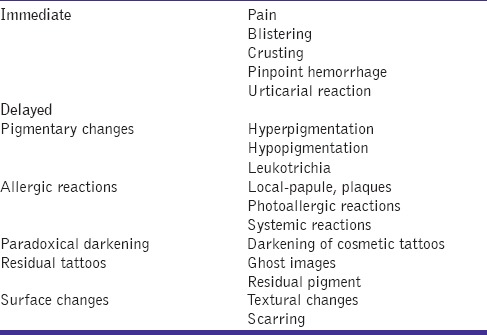
Immediate complications
These include pain, blisters [Figure 4], crusting and pinpoint haemorrhage [Figure 5]. These are more common in darker skins, using a high fluence. Pain during the laser procedure can be reduced by application of topical anesthetic cream. One report suggests that application of the laser light through a microscope glass slide can reduce the pain and blistering.[40] If crusting occurs, topical emollient or topical antibiotic should be prescribed. The patient should be advised not to pick at the crusts as this can lead to pigmentary changes. Pinpoint haemorrhage subsides spontaneously. An acute allergic reaction in the form of urticarial lesion has been reported.[41]
Figure 4.
Purpura and bruising following Q switched Nd YAG laser 1064nm (Photo courtesy Dr Sanjeev Aurangabadkar)
Figure 5.

Blistering following Q switched Nd YAG laser (Photo courtesy Dr Shenaz Arsiwala)
Delayed complications
The most common complication is pigmentary changes, either hypopigmentation [Figure 6] or hyperpigmentation. These occur 4-6 weeks after laser treatment and most of them are transient. However, longer-lasting pigmentary alterations can occur, especially in darker or tanned skin.[42] Kirby et al. reported hypopigmentation in 8% and hyperpigmentation in 22% of patients with darker skins. Leukotrichia with permanent whitening of the eyelashes has been reported following laser tattoo removal of permanent eyeliner.[43]
Figure 6.

Prlonged hypopigmentation following Q switched Nd YAG laser in darker skin (Photo courtesy Dr Shenaz Arsiwala)
Local allergic reactions, particularly to the red and yellow pigment can occur in the form of pruritic papules, nodules or scaly plaques. Rarely systemic reactions following laser treatment of allergic tattoos have been reported.[44] Photoallergic reactions can occur in the red or yellow ink. These allergic reactions may be early or delayed after several months or years following tattoo removal.[45] These allergic reactions should be treated with topical and intralesional corticosteroids.
Paradoxical darkening of tattoos can occur, particularly the light-coloured pink, tan or white-coloured tattoos, which are often used for permanent makeup.[46] This occurs due to reduction of titanium dioxide or iron oxide by the laser, turning the pigment black. Hence a small test area should be done first. When the tattoos turn black, they can be managd by further treatment with the Q-switched lasers. In removal of permanent makeup, it is sometimes wiser to treat with fractional CO2 laser or fractional Er:YAG laser to avoid paradoxical darkening.
It is sometimes difficult to remove the tattoo entirely, particularly the multicoloured professional tattoos and residual pigment can remain or there may be a ghost image. Textural changes can occur and these may be transient or permanent. Scarring can occur if a high fluence is used, particularly in dark or tanned skin, because the epidermal melanin absorbs most of the laser radiation [Figure 7]. In a large prospective study of laser tattoo removal, adverse effects were observed in only 6.2% of patients with hyperpigmentation being the commonest observed in 4.8%.[46]
Figure 7.

Hypertrophic scarring following Q switched Nd YAG laser 1064nm (Photo courtesy Dr Sanjeev Aurangabadkar)
PREVENTION OF COMPLICATIONS OF LASER TATTOO REMOVAL
The laser should be chosen according to the colour of the tattoo pigment and the patient's skin type. Generally Q-switched 1064nm Nd:YAG laser is safer in darker skin types 5-6. The spot size, the fluence and the pulse duration are important and should be carefully selected.
CONCLUSIONS
There is a need to increase awareness in the youth today regarding increased risks of tattooing when carried out in potential unsterile environments. In addition tattoo parlors should also be educated about the risks involved and the importance of using proper infection control procedures. Complications following medical tattoos are mainly due to colour mismatch, due to improper selection of pigment and improper depth of placement that can cause colour fading or bluish discolouration. Complications following decorative tattoos are mainly related to infections and allergic reactions due to failure of aseptic precautions. However, the commonest complication is patient dissatisfaction that compels them to seek removal of the tattoo. Tattoo removal is a very cumbersome procedure, and it may not always be successful, leaving a ghost image, hence the adage, think before you ink holds very much true.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Graudenz K, Greve B, Raulin C. Diffused traumatic dirt and decorative tattooing: Removal by Q-switched lasers. Hautarzt. 2003;54:756–9. doi: 10.1007/s00105-003-0493-6. [DOI] [PubMed] [Google Scholar]
- 2.Ortiz AE, Alster TS. Rising concern over cosmetic tattoos. Dermatol Surg. 2012;38:424–9. doi: 10.1111/j.1524-4725.2011.02202.x. [DOI] [PubMed] [Google Scholar]
- 3.Sanghavi SA, Dongre AM, Khopkar US. Tattoo reactions — An epidemic on the surge: A report of 3 cases. Indian J Dermatol Venereol Leprol. 2013;79:231–4. doi: 10.4103/0378-6323.107644. [DOI] [PubMed] [Google Scholar]
- 4.Piérard-Franchimont C, Hermanns JF, Piérard GE. Skin reactions to tattoo ink. Rev Med Liege. 2011;66:430–3. [PubMed] [Google Scholar]
- 5.Wenzel SM, Rittmann I, Landthaler M, Bäumler W. Adverse reactions after tattooing: Review of the literature and comparison to results of a survey. Dermatology. 2013;226:138–47. doi: 10.1159/000346943. [DOI] [PubMed] [Google Scholar]
- 6.Garcovich S, Carbone T, Avitabile S, Nasorri F, Fucci N, Cavani A. Lichenoid red tattoo reaction: Histological and immunological perspectives. Eur J Dermatol. 2012;22:93–6. doi: 10.1684/ejd.2011.1558. [DOI] [PubMed] [Google Scholar]
- 7.Bassi A, Campolmi P, Cannarozzo G, Conti R, Bruscino N, Gola M, et al. Tattoo-associated skin reaction: The importance of an early diagnosis and proper treatment. Biomed Res Int 2014. 2014 doi: 10.1155/2014/354608. 354608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaliyadan F, Kumar A. Camouflage for patients with vitiligo. Indian J Dermatol Venereol Leprol. 2012;78:8–15. doi: 10.4103/0378-6323.90940. [DOI] [PubMed] [Google Scholar]
- 9.Klügl I, Hiller KA, Landthaler M, Bäumler W. Incidence of health problems associated with tattooed skin: A nation-wide survey in German-speaking countries. Dermatology. 2010;221:43–50. doi: 10.1159/000292627. [DOI] [PubMed] [Google Scholar]
- 10.Wenzel SM, Rittmann I, Landthaler M, Bäumler W. Adverse reactions after tattooing: Review of the literature and comparison to results of a survey. Dermatology. 2013;226:138–47. doi: 10.1159/000346943. [DOI] [PubMed] [Google Scholar]
- 11.Tohme RA, Holmberg SD. Transmission of hepatitis C virus infection through tattooing and piercing: a critical review. Clin Infect Dis. 2012;54:1167–78. doi: 10.1093/cid/cir991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haley RW, Fischer RP. Commercial tattooing as a potentially important source of hepatitis C infection. Clinical epidemiology of 626 consecutive patients unaware of their hepatitis C serologic status. Medicine (Baltimore) 2000;80:134–51. doi: 10.1097/00005792-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Doll DC. Tattooing in prison and HIV infection. Lancet. 1988;1:66–7. doi: 10.1016/s0140-6736(88)91054-9. [DOI] [PubMed] [Google Scholar]
- 14.Ragland HP, Hubbell C, Stewart KR, Nesbitt LT., Jr Verruca vulgaris inoculated during tattoo placement. Int J Dermatol. 1994;33:796–7. doi: 10.1111/j.1365-4362.1994.tb00998.x. [DOI] [PubMed] [Google Scholar]
- 15.Pérez Gala S, Alonso Pérez A, Ríos Buceta L, Aragüés Montañés M, Garcia Díez A. Molluscum contagiosum on a multicoloured tattoo. J Eur Acad Dermatol Venereol. 2006;20:221–2. doi: 10.1111/j.1468-3083.2005.01363.x. [DOI] [PubMed] [Google Scholar]
- 16.Kaatz M, Elsner P, Bauer A. Body-modifying concepts and dermatologic problems: Tattooing and piercing. Clin Dermatol. 2008;26:35–44. doi: 10.1016/j.clindermatol.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Kluger N, Muller C, Gral N. Atypical mycobacteria infection following tattooing: Review of an outbreak in 8 patients in a French tattoo parlor. Arch Dermatol. 2008;144:941–2. doi: 10.1001/archderm.144.7.941. [DOI] [PubMed] [Google Scholar]
- 18.Ghorpade A. Inoculation (tattoo) leprosy: A report of 31 cases. J Eur Acad Dermatol Venereol. 2002;16:494–9. doi: 10.1046/j.1468-3083.2002.00548.x. [DOI] [PubMed] [Google Scholar]
- 19.Parker C, Kaminski G, Hill D. Zygomycosis in a tattoo, caused by Saksenaea vasiformis. Australas J Dermatol. 1986;27:107–11. doi: 10.1111/j.1440-0960.1986.tb00304.x. [DOI] [PubMed] [Google Scholar]
- 20.Alexandridou A, Reginald AY, Stavrou P, Kirkby GR. Candida endophthalmitis after tattooing in an asplenic patient. Arch Ophthalmol. 2002;120:518–9. doi: 10.1001/archopht.120.4.518. [DOI] [PubMed] [Google Scholar]
- 21.Waldmann I, Vakilzadeh F. Delayed type allergic reaction to red azo dye in tattooing. Hautarzt. 1997;48:666–70. doi: 10.1007/s001050050643. [DOI] [PubMed] [Google Scholar]
- 22.Greve B, Chytry R, Raulin C. Contact dermatitis from red tattoo pigment (quinacridone) with secondary spread. Contact Dermatitis. 2003;49:265–6. doi: 10.1111/j.0105-1873.2003.0225h.x. [DOI] [PubMed] [Google Scholar]
- 23.Litak J, Ke MS, Gutierrez MA, Soriano T, Lask GP. Generalized lichenoid reaction from tattoo. Dermatol Surg. 2007;33:736–40. doi: 10.1111/j.1524-4725.2007.33153.x. [DOI] [PubMed] [Google Scholar]
- 24.Kluger N. Cutaneous complications related to permanent decorative tattooing. Expert Rev Clin Immunol. 2010;6:363–71. doi: 10.1586/eci.10.10. [DOI] [PubMed] [Google Scholar]
- 25.Mahalingam M, Kim E, Bahwan J. Morphea-like tattoo reaction. Am J Dermatopathol. 2002;24:392–5. doi: 10.1097/00000372-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Balfour E, Olhoffer I, Leffelll D, Handerson T. Massive pseudoepitheliomatous hyperplasia: An unusual reaction to a tattoo. Am J Dermatopathol. 2003;25:338–40. doi: 10.1097/00000372-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Kluger N, Cotten H, Magana C, Pinquier L. Dermatofibroma occurring within a tattoo: Report of two cases. J Cutan Pathol. 2008;35:696–8. doi: 10.1111/j.1600-0560.2007.00882.x. [DOI] [PubMed] [Google Scholar]
- 28.Armiger WG, Caldwell EH. Primary lesion of a non-Hodgkin's lymphoma occurring in a skin tattoo: Case report. Plast Reconstr Surg. 1978;62:125–7. doi: 10.1097/00006534-197807000-00031. [DOI] [PubMed] [Google Scholar]
- 29.Punzi L, Rizzi E, Pianon M, Rossini P, Gambari PF. Tattooing-induced psoriasis and psoriatic arthritis. Br J Rheumatol. 1997;36:1133–4. doi: 10.1093/rheumatology/36.10.1133. [DOI] [PubMed] [Google Scholar]
- 30.Horner KL, Chien AJ, Edenholm M, Hornung RL. Winnie the Pooh and psoriasis too: An isomorphic response of guttate psoriasis in a tattoo. Pediatr Dermatol. 2007;24:E70–2. doi: 10.1111/j.1525-1470.2007.00445.x. [DOI] [PubMed] [Google Scholar]
- 31.La Placa M, Passarini B. Subacute cutaneous lupus erythematosus after a tattoo. Clin Exp Dermatol. 2009;34:632–3. doi: 10.1111/j.1365-2230.2008.03040.x. [DOI] [PubMed] [Google Scholar]
- 32.Jolly M. Discoid lupus erythematosus after tattoo: Koebner phenomenon. Arthritis Rheum. 2005;53:627. doi: 10.1002/art.21334. [DOI] [PubMed] [Google Scholar]
- 33.Tendas A, Niscola P, Barbati R, Abruzzese E, Cuppelli L, Giovannini M, et al. Tattoo related pyoderma/ectyma gangrenous as presenting feature of relapsed acute myeloid leukaemia: An exceptionally rare observation. Injury. 2011;42:546–7. doi: 10.1016/j.injury.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 34.Campbell FA, Gupta G. Lichenoid tattoo reaction responding to topical tacrolimus ointment. Clin Exp Dermatol. 2006;31:293–4. doi: 10.1111/j.1365-2230.2005.02012.x. [DOI] [PubMed] [Google Scholar]
- 35.Fang H, Wu P, Hsieh H. Generalized lichenoid tattoo reaction with spontaneous resolution after skin biopsy. Dermatolo Sin. 2013;31:38–40. [Google Scholar]
- 36.Guidelines for blood banks. [Last accessed on 2014 Feb 12]. available from: http://www.cdsco.nic.in/forms/list.aspx?lid=1642&Id=1 .
- 37.Kent Km, Graber EM. Laser tattoo removal: A review. Dermatol Surg. 2012;38:1–13. doi: 10.1111/j.1524-4725.2011.02187.x. [DOI] [PubMed] [Google Scholar]
- 38.Kilmer SL, Lee MS, Grevelink JM, Flotte TJ, Anderson RR. The Q-switched Nd: YAG laser effectively treats tattoos. A controlled, dose-response study. Arch Dermatol. 1993;129:971–8. [PubMed] [Google Scholar]
- 39.Vasold R, Naarmann N, Ulrich H, Fischer D, König B, Landthaler M, et al. Tattoo pigments are cleaved by laser light-the chemical analysis in vitro provide evidence for hazardous compounds. Photochem Photobiol. 2004;80:185–90. doi: 10.1562/2004-05-17-RA-170. [DOI] [PubMed] [Google Scholar]
- 40.Murphy MJ. A novel, simple and efficacious technique for tattoo removal resulting in less pain using the Q-switched Nd: YAG laser. Lasers Med Sci. 2014;29:1445–7. doi: 10.1007/s10103-014-1542-3. [DOI] [PubMed] [Google Scholar]
- 41.Kirby W, Koriakos A, Desai A, Desai T. Undesired pigmentary alterations associated with Q-switch laser tattoo removal. Skin and Aging. 2010;18:38–40. [Google Scholar]
- 42.Liu XJ, Huo MH. Permanent leukotrichia after Q-switched 1064 nm laser tattoo removal. Indian J Dermatol Venereol Leprol. 2011;77:81–2. doi: 10.4103/0378-6323.75007. [DOI] [PubMed] [Google Scholar]
- 43.Bernstein EF. A widespread allergic reaction to black tattoo ink caused by laser treatment. Lasers Surg Med. 2015;47:180–2. doi: 10.1002/lsm.22319. [DOI] [PubMed] [Google Scholar]
- 44.Bernstein EF. Laser tattoo removal. Semin Plast Surg. 2007;21:175–92. doi: 10.1055/s-2007-991186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anderson RR, Geronemus R, Kilmer SL, Farinelli W, Fitzpatrick RE. Cosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatment. Arch Dermatol. 1993;129:1010–4. doi: 10.1001/archderm.129.8.1010. [DOI] [PubMed] [Google Scholar]
- 46.Bencini PL, Cazzaniga S, Tourlaki A, Galimberti MG, Naldi L. Removal of tattoos by q-switched laser: Variables influencing outcome and sequelae in a large cohort of treated patients. Arch Dermatol. 2012;148:1364–9. doi: 10.1001/archdermatol.2012.2946. [DOI] [PubMed] [Google Scholar]


