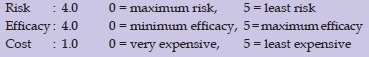
Abstract
Context:
Xanthelasma palpebrarum is the most common form of xanthomas. Albeit a benign entity, it is cosmetically disturbing and a frequently recurring dermatologic referral. Although the classical treatment option remains surgical excision, alternatively, chemical cauterization, cryosurgery and electrofulguration have all been tried in the past with mixed results. The use of laser systems such as carbon dioxide laser, Erb:YAG laser, Q-switched Nd:YAG laser, diode laser, pulsed dye laser and KTP laser have become popular in the treatment of these lesions. Recent literature suggests minimal pigmentary changes and scarring with the use of ultrapulse carbon dioxide laser treatment of these lesions.
Aim:
To study and evaluate the effectiveness of ultrapulse carbon dioxide laser ablation for treatment of xanthelasma palpebrarum.
Materials and Methods:
10 patients presenting with bilateral xanthelasma palpebrarum, new and with recurrence were studied for results after a single treatment with ultrapulse carbon dioxide laser (10,600 nm; 100-200 Hz; 200-400 μsec). The follow-up time was 9 months.
Results:
All lesions were treatable with a single-laser treatment session. Two patients (20%) developed recurrence during the follow-up period. Side effects included post inflammatory hyperpigmentation in two patients (20%), but no visible scarring was observed.
Conclusions:
The ultrapulse carbon dioxide laser is an effective and safe therapeutic alternative in treatment of xanthelasma palpebrarum.
KEYWORDS: Ultrapulse carbon dioxide laser, xanthelasma palpebrarum, xanthomas
REC Review:
INTRODUCTION
Xanthelasma palpebrarum, a form of plane xanthoma, is the most common of the xanthomas. Clinically, it is characterised by flat, yellowish lesions over and around eyelids, but most commonly over the medial canthus. Although the presence of xanthelasma warrants investigation for hyperlipidaemia, the latter is present in only about one-half of the patients with these lesions.[1] Although a benign entity, it is cosmetically disturbing.
Surgical excision has been the treatment of choice for decades. However, this normally effective measure bears a considerable risk of side effects, especially an ectropion, which could lead to additional procedures, such as, full thickness skin grafting.[2] Other modalities like cryosurgery, electrofulguration, radiofrequency and chemical cautery have yielded mixed results with frequent recurrences and multiple sessions.[3] The use of various ablative and non-ablative lasers has become popular. Ten patients were treated with a single treatment session of ultrapulse carbon dioxide laser (10,600 nm; 100-200 Hz; 200-400 μs). This mode delivers high energy in very short impulses allowing controlled and safe ablation of thin skin layers of this region, thereby minimising adverse sequelae and recurrence.
MATERIALS AND METHODS
Ten patients (6 female and 4 male), aged between 42 and 65 yrs (mean age 58.3 years) with bilateral xanthelasmas were enrolled for the study. Lesions over one eye (upper and lower eyelid) was counted as single lesion count and lesions measuring 1 cm or more were included. Four patients had been treated before, one with electrofulguration and three with trichloroacetic acid. After informed consent, patients were treated with a single treatment session with ultrapulse carbon dioxide laser (10,600 nm; 100-200 Hz; 200-400 μs). A continuously adjustable variable spot-size handpiece (spot diameter 1-2 mm) and continuous exposure mode was used. The patients were advised to keep their eyes closed during the entire procedure, which were taped with micropore for added protection. Before lasing, the lesions were infiltrated with 2% Lignocaine with adrenaline (1:10,000) via standard insulin syringe attached with a 30-G needle. Charred tissue was gently removed with a normal saline soaked gauze piece to expose the planes. Total removal of yellowish fatty tissue and appearance of underlying pink tissue was taken as endpoint of therapy. On an average, 4-7 passes were made for the macroscopic removal of the lesions under 2.5x magnification. Post-operatively, 2% mupirocin ointment was applied and patient was asked to continue topical application of the same till scabbing, which typically occurred by 5th to 7th day. Patients were instructed to keep the area clean and dry for the same duration and advised to follow strict sun protective measures thereafter. Patients were reviewed at day seven, 1 month, 6 months and finally at 9 months after the treatment session.
Patients were tested for pathologic serum lipids, i.e., total cholesterol, HDL cholesterol, LDL cholesterol and triglycerides, (normal values: Total cholesterol: 200-239 mg/dl borderline high; HDL cholesterol: <40 mg/dl low; LDL cholesterol: 130-159 mg/dl borderline high; triglycerides: 30-200 mg/dl).[4] A combined increase of triglycerides and total cholesterol was considered as mixed hyperlipidaemia. Pathological lipoprotein levels were classified in the Fredrickson scheme.[5] Patients with pathological lipid values were referred to Medicine outpatient department where they were counselled for dietary adjustments and/or drug treatment. Before and after clinical photographs were taken with Sony Cybershot DSC-T100 and Nikkon DSLR D3000 cameras.
RESULTS
All 20 lesions in 10 patients were removed with a single ultrapulse carbon dioxide laser (10,600 nm) treatment session [Figures 1a–4b]. Only two patients (20%) developed recurrence during the follow-up period of 9 months. Both these patients had been treated earlier by different modalities in the past. Side effects seen included post inflammatory hyperpigmentation in two patients (20%). However, there were no other complications, like hematomas, bleeding, infections, scarring or ectropions.
Figure 1.
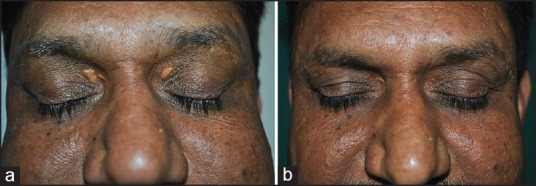
(a) Before ablation. (b) Follow up at 9 months
Figure 4.

(a) Before ablation (the patient had been treated with 30% TCA cautery in the past with recurrence). (b) Follow up at 9 months
Figure 2.

(a) Before ablation. (b) Follow up at 9 months
Figure 3.

(a) Before ablation. (b) Follow up at 9 months
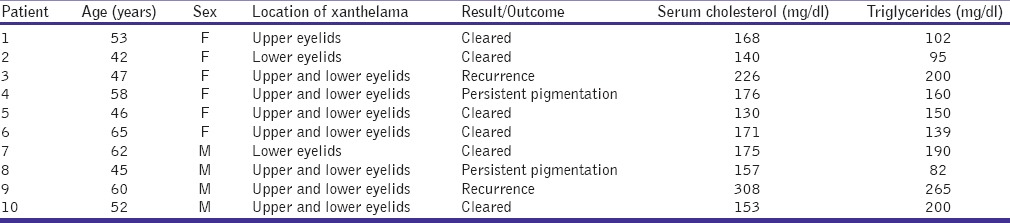
Patient clinical and lipid profile are shown in Table 1. Both serum cholesterol and serum triglycerides were raised in one patient, consistent with Frederickson type III hyperlipidaemia. Incidentally, this was one of the two cases with recurrence.
Table 1.
Patient profile
DISCUSSION
Xanthomas are plaques or nodules consisting of abnormal lipid deposition and foam cells. They do not represent a disease but rather serve as cutaneous markers of different lipoprotein disorders or may arise without an underlying metabolic disorder. Xanthelasma is a form of plane xanthoma. It is more frequent in women and its prevalence increases with age. Although sometimes associated with type II hypercholesterolaemia and type III dysbetalipoprotienaemia, xanthelasma also occur in normolipidaemic patients with monoclonal gammopathies or as familial cases.[5] Clinically, it is characterised by the appearance of a flat, raised yellowish plaque most often situated in and around the medial canthus with a tendency to spread to upper and lower eyelids. Xanthelasma plaques may subsequently become confluent and thickened. Histologically, xanthelasma differs from other xanthomas by its more superficial location in the middle and superficial layers of the dermis. It is composed of foamy histiocytes arranged around dermal capillaries. Intrahistiocytic vacuoles contain esterified cholesterol.[2]
Although a benign lesion, it is a frequent cosmetic referral to the dermatology, ophthalmology and reconstructive surgery outpatient departments. The ‘classical’ treatment option for xanthelasma palpebrarum is surgical excision. But excision almost always leads to scars, which might, at times, cause an ectropion. Furthermore, the revision of the scar can require a skin graft procedure. Very extensive lesions may not be operable at all. Furthermore, for the treatment of relapses, the surgical approach may not be repeatable.[2] Other alternatives include chemical cautery with varying percentages of trichloroacetic acid, but multiple sessions and frequent recurrences are a norm. Also, the depth of penetration of chemicals cannot be controlled and hence pose a danger for conjunctival and scleral injury. Post-inflammatory hypopigmentation and recurrence is a common side effect of cryosurgery using liquid nitrogen.[3] Low-voltage radiofrequency ablation has also been tried with mixed results.[6]
Carbon dioxide laser is the gold standard in ablative lasers. The chromophore for the carbon dioxide laser beam (10,600 nm) is the water present in biological tissues. Upon absorption, it effects a non-selective thermal damage and ablation of target tissue. Ultrapulse mode offers additional advantage of delivering high energy over extremely short pulses, well within the thermal relaxation time of the surrounding tissue, vaporising a thin layer of tissue with every pass. Fitzpatrick et al. have shown that by a single ultrapulse CO2 laser treatment of 250 mJ impulses, the skin is ablated to a depth of up to 60 microns. A second consecutive laser application increases the depth of the damage to ~130 microns; a third leads to thermal destruction of skin structures to a depth of up to 316 microns.[2] This property aids in layer by layer ablation of superficial epithelial growths. This ensures precise and controlled ablation of xanthelasma lesions and hence minimal adverse sequelae like scarring and ectropion.
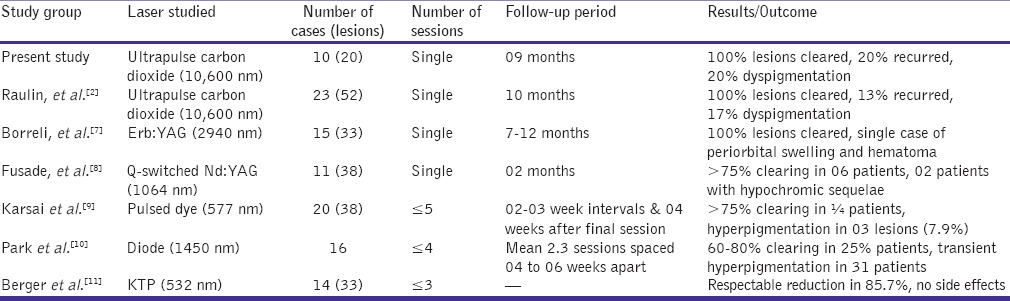
Other ablative and non-ablative lasers which have been tried in photoablation of xanthelasmas include Erb:YAG laser,[7] Q-switched Nd:Yag lasers,[8] pulsed dye lasers,[9] diode lasers[10] and KTP lasers.[11] While pulsed dye laser lasers are effective in early vascular lesions, they fare poorly in established xanthelasmas. Diode lasers have been tried on the basis of their efficacy in ablation of sebaceous glands in acne patients. Q-switched Nd;Yag lasers offer some benefit in yellowish pigmented xanthelasmas. Most of these lasers require multiple sessions with varying rates of clearance of lesions and that of recurrence. Table 2 compares the relative effectiveness in treating xanthelasmas by different laser systems. The recurrences in two of our patients could be explained by superficial and incomplete ablation of the lesions as well as an adverse lipid profile in at least one case. Post inflammatory hyperpigmentation in two of the patients could be because of failure to observe sun-protective measures and/or inherent tendency to post inflammatory hyperpigmentation in skin type IV of our patients.
Table 2.
Comparison of studies on lasers for ablation of xanthelasmas
CONCLUSIONS
In conclusion, ultrapulse carbon dioxide laser is a safe and effective alternative for ablation of xanthelasma palperarum, which additionally offers the advantage of a single treatment session and low rates of recurrence, when compared to contemporary conventional treatments. However, more extensive studies with higher sample size, comparative studies with established modalities and longer follow up periods is required to establish it as standard of care for management of this ubiquitous entity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Massengale WT, Hodari KT, Nesbitt LT., Jr . Xanthomas. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Dermatology. Amsterdam: Elsevier; 2012. pp. 1552–3. [Google Scholar]
- 2.Raulin C, Schoenermark MP, Werner S, Greve B. Xanthelasma palpebrarum: Treatment with the ultrapulsed CO2 laser. Lasers Surg Med. 1999;24:122–7. doi: 10.1002/(sici)1096-9101(1999)24:2<122::aid-lsm7>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 3.Dewan SP, Kaur A, Gupta RK. Effectiveness of cryosurgery in xanthelasma palpebrarum. Indian J Dermatol Venereol Leprol. 1995;61:4–7. [PubMed] [Google Scholar]
- 4.Kratz A, Pesce MA, Fink DJ. Appendix: Laboratory values of clinical importance. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al., editors. Harrison's Principles of Internal Medicine. 16th ed. New York: McGraw Hill; 2008. pp. A–7. 10. [Google Scholar]
- 5.White LE. Xanthomatoses and lipoprotien disorders. In: Wolff K, Goldsmith LA, Katz SI, Gilchrist BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in General Medicine. 7th ed. New York: McGraw Hill; 2008. p. 1272. [Google Scholar]
- 6.Dincer D, Koc E, Erbil AH, Kose O. Effectiveness of low-voltage radiofrequency in the treatment of xanthelasma palpebrarum: A pilot study of 15 cases. Dermatol Surg. 2010;36:1973–8. doi: 10.1111/j.1524-4725.2010.01770.x. [DOI] [PubMed] [Google Scholar]
- 7.Borelli C, Kaudewitz P. Xanthelasma palpebrarum: Treatment with the Erbium: YAG laser. Lasers Surg Med. 2001;29:260–4. doi: 10.1002/lsm.1117. [DOI] [PubMed] [Google Scholar]
- 8.Fusade T. Treatment of xanthelasma palpebrarum by 1064-nm Q-switched Nd: YAG laser: A study of 11 cases. Br J Dermatol. 2008;158:84–7. doi: 10.1111/j.1365-2133.2007.08194.x. [DOI] [PubMed] [Google Scholar]
- 9.Karsai S, Czarnecka A, Raulin C. Treatment of xanthelasma palpebrarum using a pulsed dye laser: A prospective clinical trial in 38 cases. Dermatol Surg. 2010;36:610–7. doi: 10.1111/j.1524-4725.2010.01514.x. [DOI] [PubMed] [Google Scholar]
- 10.Park EJ, Youn SH, Cho EB, Lee GS, Hann SK, Kim KH, et al. Xanthelasma palpebrarum treatment with a 1,450-nm-diode laser. Dermatol Surg. 2011;37:791–6. doi: 10.1111/j.1524-4725.2011.01945..x. [DOI] [PubMed] [Google Scholar]
- 11.Berger C, Kopera D. KTP-Laser-Koagulation bei Xanthelasma palpebrarum. J Dtsch Dermatol Ges. 2005;3:775–9. doi: 10.1111/j.1610-0387.2005.05746.x. [DOI] [PubMed] [Google Scholar]


