Abstract
Background:
We present the incidence and determinants of endophthalmitis between July 2010 and June 2012 at King Khaled Eye Specialist Hospital, Riyadh, Saudi Arabia. On its basis, we recommended recommendations to strengthen the infection prevention and control strategies.
Methods:
This is a retrospective review of health records type of study. The details of cases reported having endophthalmitis among those operated in 2 years of study period were studied. The incidence of endophthalmitis was calculated for different eye surgeries and epidemiological variables. The causative organisms in vitreous tap were reviewed. The visual outcomes 6 weeks following intervention/treatment of endophthalmmitis were also studied.
Results:
Of the 22,554 cases operated, 17 developed endophthalmitis. The incidence was 0.08% (95% confidence interval [CI] 0.04–0.11). The incidence of endophthlamitis among cataract surgeries was 0.12% (95% CI 0.04–0.21). Five specimens did not show any bacteria or fungus. Staphylococcus epidermis (3 cases) was the main pathogen identified. In 8 (47%) eyes, vision deteriorated in spite of treatment. In 5 (29%) eyes, it became stable and in 4 (23.5%) eyes, it improved following treatment. Signs of infection were noted in 1st week, 3 weeks and 12 weeks in 4, 6 and 5 eyes respectively. Late presentation of infection (6 months postoperatively) was reported in two eyes.
Conclusions:
A vigilant infection control unit in a large eye hospital helps in monitoring endophthalmitis related catastrophes and suggests timely preventive measures to reduce the occurrence and appropriate measures to limit visual disabilities following eye surgery related endophthalmitis.
Keywords: Cataract, endophthalmitis, infection control, ocular surgery
INTRODUCTION
In ophthalmic surgery, infection is a dreaded complication. Both causative agents and treatment are toxic to the retina and result in irreversible visual impairment. Prevention is, therefore, the best measure. Large eye hospitals have infection control units and quality management departments to ensure prompt and adequate steps to prevent and control infections during and soon after surgery. With the advent of modern antibiotics and intravitreal administration, infections are controlled quickly, and visual disabilities are lower than previously reported.1
The majority of literature on endophthalmitis relates to cataract surgery as it is the most common intraocular surgery. With lens implantation during modern cataract surgery, the risk of infection is also higher. Intravitreal injection for treating posterior segment pathologies is another procedure that could cause endophthalmitis.2,3 Studies from Saudi Arabia reviewed the outcomes of treatment of endophthalmitis with antibiotics. However, they were procedure specific and related to the outcomes.4,5,6
The infection prevention and control team of the quality management department at King Khaled Eye Specialist Hospital (KKESH) reviewed postoperative endophthalmitis cases. These cases are reported based on the event notification system. The present study estimates the incidence and determinants of postoperative endophthalmitis at KKESH and recommends measures to address the problem.
METHODS
The Institutional Review Board of KKESH approved this study. As this was a retrospective review of health information and the identity of the patients was kept confidential, written permission of patients with endophthalmitis was waived. This study was conducted between March 25, 2013 and April 15, 2013. Data from July 1, 2010 to June 30, 2012 about reported endophthalmitis cases were reviewed. Data collected from patient charts included, the cause of endophthalmitis, the surgical details and follow-up findings.
Patients who underwent surgery in the operating theaters as well as those who received intravitreal injection at KKESH constituted the denominator for calculating the incidence of endophthalmitis.
Patients, who underwent surgery at KKESH and had intraocular infection within 6 months postoperatively, were included in the present study. Cases of endophthalmitis that underwent primary surgery at institution other than KKESH were excluded from this study. Cases with a history of trauma as the underlying cause of endophthalmitis were also excluded from this study.
The hospital infection control team undertook this study with the aid of an epidemiologist. The protocol to prevent and manage infection following ocular surgery and cataract surgeries conform to international standards.7,8
On follow-up, ophthalmologists inquired about pain in and around the eye, redness and decreased vision. On examination, they noted circumcorneal congestion, aqueous flare, hypopyon, vitreous floaters, keratic precipitates on the posterior surface of cornea, painful eye movements, and other evidence of inflammation of the posterior segment of eye to define a case of endophthalmitis. Visual acuity was measured with Snellen distance vision charts held six meters from the patient. If the patient could not identify the top letter of the chart at six meters, the test was repeated at three meters. If the patient still failed to identify the top letter correctly, the optotype ‘E’ was shown at two, and one meter distances and projection of light from four directions was also tested. While reviewing the response of the treatment for endophthalmitis, similar tests were repeated.
A committee of infection prevention and control within the quality management department at KKESH constantly reviewed the endophthalmitis cases reported in the hospital. From 2007, it focused only on surgical cases from KKESH instead of all cases treated at KKESH. A standard protocol and case report form was prepared and discussed with the ophthalmologists and surgical nursing staff, recovery area nurses and clinics where the patients went for follow-up. The endophthalmitis case report form was implemented in 2010.
The demographic information included age, sex, and nationality of individuals with endophthalmitis. Presence of diabetic and blepharitis in the eye scheduled to undergo surgery was noted. The operative log-book was used to collect the data on surgery details including date, place, type of eye surgery, operating surgeon, day of surgery, presence of intraocular lens implant and glaucoma valve. Follow-up information included the time interval between surgery and the first evidence of infection in the eye, type of antibiotic treatment offered, repeat surgery, laboratory report of organism profile and the response to the treatment. The best-corrected visual acuity 6 weeks following management of endophthalmitis was considered the outcome indicator. The visual outcome was further categorized as; vision improved, remained same or deteriorated.
The operation theaters of KKESH had an average temperature of 22°C. Prior to surgery the face, lids and lid margins are painted with 5% povidone iodine solution. All cases of cataract surgery were given intracameral moxifloxacillin (0.5%), subconjunctival injection of cefazolin (100 mg in 0.5 ml) and topical ofloxacillin 0.3% eye drops as prophylaxis.
The annual incidence of endophthalmitis was calculated using the formula:
Number of endophthalmitis cases/total eye surgeries performed in the study period/2 × 100. Incidence rates by age-group, gender, year of cataract surgery were also calculated. To review the visual outcome following endophthalmitis treatment, we calculated the numbers and percentage proportion of eyes with different grades of visual disability. For continuous variables such as age, we estimated the mean, standard deviation, difference of mean and the 95% confidence interval (CI). For qualitative variables, we calculated the odds ratio or Chi-square value and ensured that it was not a chance observation. For comparison of incidence rates among variables, we estimated the difference in the percentage proportion including the 95% CI. Statistical analysis was performed using Epidata Association, Odense, Denmark, software.9
The outcome of this study was discussed with the members of KKESH infection control committee and steps to further reduce intraocular infection rates and manage cases of endophthalmitis were suggested.
RESULTS
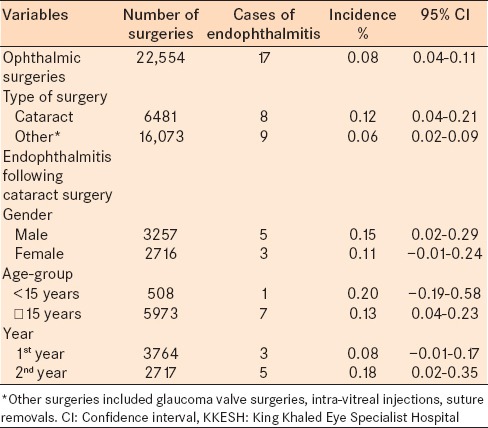
Over the 2 years of study period, 17 cases of endophthalmitis were reported. Fourteen cases underwent surgery in the major operating theatres, and three cases underwent procedures in minor surgery unit attached to clinics. During this period, 22,554 cases underwent surgery in the operation theaters both major and minor operation theaters. The incidence of postoperative endophthalmitis was 0.08% (95% CI: 0.04–0.11). The incidence of endophthalmitis among cataract surgery cases by variables is presented in Table 1.
Table 1.
Incidence of postoperative endophthalmitis at KKESH between July 2010 and June 2012
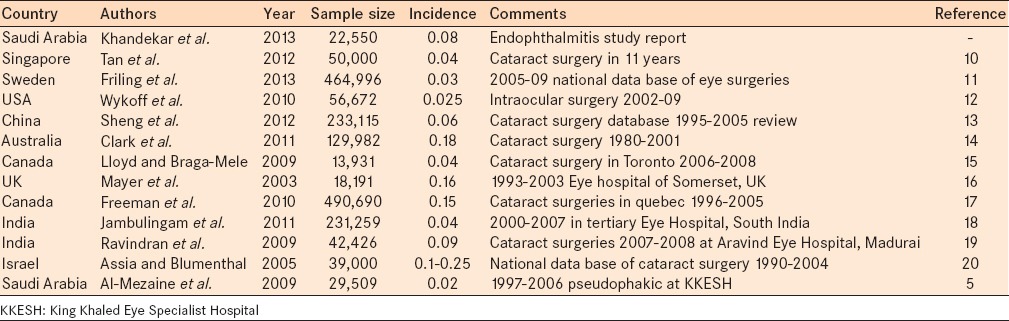
The incidence of endophthalmitis in the current study was compared to the incidence in the literature [Table 2].
Table 2.
Incidence of endophthalmitis in different studies
Samples from vitreous taps of 17 eyes were sent for microscopic examination, culture and sensitivity tests. Five specimens did not show any bacteria or fungus. Gram-positive organisms included Staphylococcus epidermis (3 cases), Propionibacterium granulosom, Enterococcus faecalis, Streptococcus viridans, Streptococcus pneumoniae (2 cases) and one case of a Gram-negative organism (Sphingomonas paucimobilis). The person with diabetes and endophthalmitis had hyphe in the vitreous sample on microscopic examination, but type of fungus could not be identified. Patient responded to intravenous vancomycin (5 mg/ml) mixed in 500 ml of normal saline.
Topical treatment included fortified vancomycin, fortified ceftazidime, pred forte and atropine in all cases. Oral or intravenous antibiotics were provided in cases where systemic focus of infection was found. In all eyes with endophthalmitis except one case, intravitreal antibiotics (within 2 h of diagnosis of endophthlamitis) (vancomycin + ceftazidime) and dexamethasone were administered.
Visual outcomes after endophthalmitis treatment were compared to the vision noted prior to the endophthalmitis treatment [Table 3 and Figure 1].
Table 3.
Visual outcomes of eyes with endophthalmitis 6 weeks after treatment and before starting endophthalmitis treatment
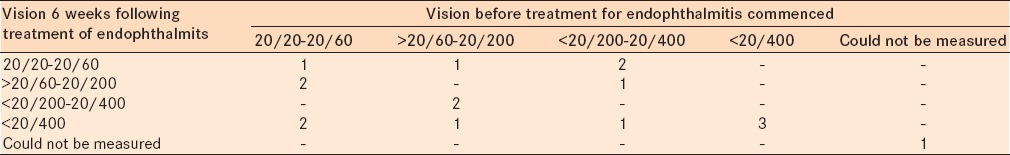
Figure 1.
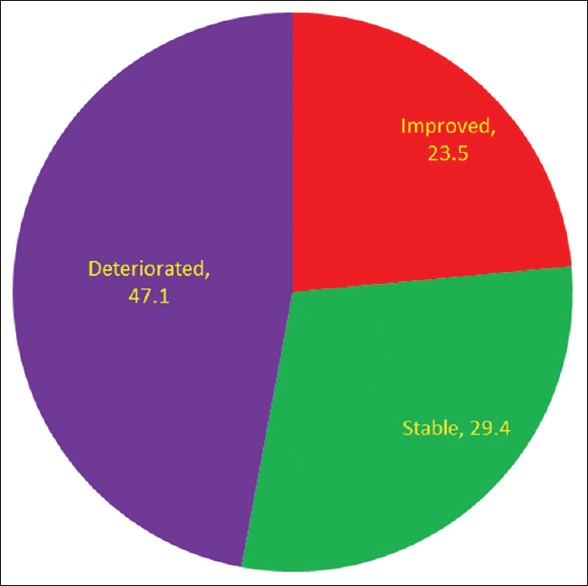
Status of vision before and 6 weeks after management of endophthalmitis
In four eyes, signs of infection were noted within the 1st week postoperatively. In six eyes, infection was noted within 3 weeks postoperatively. Infection was reported within 6 months in five eyes. Late presentation of infection (6 months postoperatively) was reported in two eyes. None of the patients with infection after 6 months had undergone additional surgical procedure after cataract surgery. In one eye, Bacterial culture showed P. granulosom.
In another eye, Gram and Giemsa stain showed rare Gram variable cocci.
DISCUSSION
The 0.08% incidence of endophthalmitis noted in our study was low compared with that noted in UK (0.16%) and Canada (0.15%). However it was higher than that reported in USA (0.025), Sweden (0.03%) and Singapore (0.04%) [Table 2]. A wide variation in endophthalmitis rates in the literature could be due to differences in intraocular surgeries, year of reporting, notification systems and aseptic techniques used at these institutions.10,11,12,13,14,15,16,17,18,19,20
The incidence of endophthalmitis following cataract surgeries in our study was 0.12%. Cataract surgery is a common intraocular procedure worldwide. Endophthalmitis negatively affects the visual outcomes in these patients. Therefore, there are numerous publications on endophthalmitis following cataract surgery.10,13,14,15,17,19,20
In our study, there was only one case of endophthalmitis following intravitreal injection. Cavalcante et al. reported a 0.009% incidence of endophthalmitis following intravitreal triamcinolone injections.21 In contrast, Jonisch et al. reported a 1.9% incidence of sterile endophthalmitis following intravitreal injection of the preserved triamcinolone.22 The incidence of endophthalmitis following intravitreal injections was 0.07% in a study from Turkey.23
There were different types of organisms responsible for endophthalmitis in our study. The leading causative organisms were S. epidermis and S. pneumoniae. Nearly one-third of cases had a dry tap yielding no organisms in the culture reports. Irigoyen et al. have reported similar organism profiles and rates of negative culture.3
Gram-positive organisms were the most common microbes associated with endophthalmitis in our study. Ding et al. also found Gram-positive bacteria as the most common cause in their series of 46 patients with endophthalmitis in China.24 S. epidermis was the causative organism in 18% of cases in our series. Cao et al. had reported this organism to be responsible for 50% of cases in their series.25 We found one case of fungal endophthalmitis that was reported after cataract surgery in a diabetic patient. In another study in Kingdom of Saudi Arabia, 3/17 (17.6%) eyes had fungal endophthalmitis.5 A failure of the sterilization system has been considered to be the cause of fungal endophthalmitis.26
Visual outcomes following endophthalmitis management in our study suggested that in nearly half of cases of endophthalmitis, vision deteriorated and in less than one-fourth of the cases, vision improved. Presence of diabetes, Gram-negative organisms and fungal infections were the primary reasons for poor visual outcomes. These observations have been reported previously in the Kingdom of Saudi Arabia.5 Due to poor visual prognosis following standard treatment of endophthalmitis, clinicians should be cautious about counseling patients about positive visual outcomes.
The role of surveillance and timely action both for eliminating the potential sources of infection and ensuring a standard mode of management for endophthalmitis is crucial. Periodic collection of samples from different sites within the operating theatre, review of intraocular irrigating solutions, assessing infections and commensals among staff in the operating theatre and maintenance of cold chain are few useful measures in controlling infections.27,28 Newer modalities to prevent and treat endophthalmitis have been proposed. The infection control unit of a hospital should review their impact periodically.29,30
There were some limitations to our study. The surveillance of endophthalmitis at KKESH is based on event notification. Mild endophthalmitis cases might have been underestimated as clinicians could decide to treat such cases with a topical and oral antibiotic regimen and refrain from reporting. Comorbidities before primary surgeries were not noted. Hence, compromised vision before and after endophthalmitis treatment can be due to causes other than endophthalmitis.
A vigilant infection control unit in a large eye hospital helps in monitoring endophthalmitis related catastrophes and suggests timely preventive measures to reduce the occurrence and appropriate measures to limit visual disabilities following eye surgery related endophthalmitis. All cases suspected to have endophthalmitis should undergo microscopic examination of material collected through aspiration of vitreous/aqueous and then tested for culture and sensitivity. Intravitreal injection of the mixture of ceftazidime, vancomycin and pred fort should be as soon as possible. Based on the report of the culture and sensitivity, the subsequent antibiotic treatment should be altered. Visual prognosis in such cases is not predictable hence surgeon should give guarded prognosis to the patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pathengay A, Flynn HW, Jr, Isom RF, Miller D. Endophthalmitis outbreaks following cataract surgery: Causative organisms, etiologies, and visual acuity outcomes. J Cataract Refract Surg. 2012;38:1278–82. doi: 10.1016/j.jcrs.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 2.Simunovic MP, Rush RB, Hunyor AP, Chang AA. Endophthalmitis following intravitreal injection versus endophthalmitis following cataract surgery: Clinical features, causative organisms and post-treatment outcomes. Br J Ophthalmol. 2012;96:862–6. doi: 10.1136/bjophthalmol-2011-301439. [DOI] [PubMed] [Google Scholar]
- 3.Irigoyen C, Ziahosseini K, Morphis G, Stappler T, Heimann H. Endophthalmitis following intravitreal injections. Graefes Arch Clin Exp Ophthalmol. 2012;250:499–505. doi: 10.1007/s00417-011-1851-1. [DOI] [PubMed] [Google Scholar]
- 4.Al-Turki TA, Al-Shahwan S, Al-Mezaine HS, Kangave D, Abu El-Asrar AM. Microbiology and visual outcome of bleb-associated endophthalmitis. Ocul Immunol Inflamm. 2010;18:121–6. doi: 10.3109/09273940903370730. [DOI] [PubMed] [Google Scholar]
- 5.Al-Mezaine HS, Al-Assiri A, Al-Rajhi AA. Incidence, clinical features, causative organisms, and visual outcomes of delayed-onset pseudophakic endophthalmitis. Eur J Ophthalmol. 2009;19:804–11. doi: 10.1177/112067210901900519. [DOI] [PubMed] [Google Scholar]
- 6.Al-Mezaine HS, Kangave D, Al-Assiri A, Al-Rajhi AA. Acute-onset nosocomial endophthalmitis after cataract surgery: Incidence, clinical features, causative organisms, and visual outcomes. J Cataract Refract Surg. 2009;35:643–9. doi: 10.1016/j.jcrs.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Barry P, Behrens-Baumann W, Pleyer U, Seal D. Dublin, Ireland: 2007. [Last accessed on 2015 Mar 10]. ESCRS Guidelines on Prevention, Investigation and Management of Post-Operative Endophthalmitis. Version 2. Available from: http://www.chulaophthalmology.org/userfiles/download/ESCRS_Guidelines_2007.pdf . [Google Scholar]
- 8.Peyman G, Lee P, Seal DV. London: Taylor and Francis; 2004. Endophthalmitis – Diagnosis and Management; pp. 1–270. [Google Scholar]
- 9.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version 2.3. [Last updated on 2009 May 20; Last accessed on 2013 Mar 27]. Available from: http://www.OpenEpi.com .
- 10.Tan CS, Wong HK, Yang FP. Epidemiology of postoperative endophthalmitis in an Asian population: 11-year incidence and effect of intracameral antibiotic agents. J Cataract Refract Surg. 2012;38:425–30. doi: 10.1016/j.jcrs.2011.09.040. [DOI] [PubMed] [Google Scholar]
- 11.Friling E, Lundström M, Stenevi U, Montan P. Six-year incidence of endophthalmitis after cataract surgery: Swedish national study. J Cataract Refract Surg. 2013;39:15–21. doi: 10.1016/j.jcrs.2012.10.037. [DOI] [PubMed] [Google Scholar]
- 12.Wykoff CC, Parrott MB, Flynn HW, Jr, Shi W, Miller D, Alfonso EC. Nosocomial acute-onset postoperative endophthalmitis at a university teaching hospital (2002-2009) Am J Ophthalmol. 2010;150:392–398.e2. doi: 10.1016/j.ajo.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Sheng Y, Sun W, Gu Y, Lou J, Liu W. Endophthalmitis after cataract surgery in China, 1995-2009. J Cataract Refract Surg. 2011;37:1715–22. doi: 10.1016/j.jcrs.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 14.Clark A, Morlet N, Ng JQ, Preen DB, Semmens JB. Whole population trends in complications of cataract surgery over 22 years in Western Australia. Ophthalmology. 2011;118:1055–61. doi: 10.1016/j.ophtha.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd JC, Braga-Mele R. Incidence of postoperative endophthalmitis in a high-volume cataract surgicentre in Canada. Can J Ophthalmol. 2009;44:288–92. doi: 10.3129/i09-052. [DOI] [PubMed] [Google Scholar]
- 16.Mayer E, Cadman D, Ewings P, Twomey JM, Gray RH, Claridge KG, et al. A 10 year retrospective survey of cataract surgery and endophthalmitis in a single eye unit: Injectable lenses lower the incidence of endophthalmitis. Br J Ophthalmol. 2003;87:867–9. doi: 10.1136/bjo.87.7.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freeman EE, Roy-Gagnon MH, Fortin E, Gauthier D, Popescu M, Boisjoly H. Rate of endophthalmitis after cataract surgery in quebec, Canada, 1996-2005. Arch Ophthalmol. 2010;128:230–4. doi: 10.1001/archophthalmol.2009.380. [DOI] [PubMed] [Google Scholar]
- 18.Jambulingam M, Parameswaran SK, Lysa S, Selvaraj M, Madhavan HN. A study on the incidence, microbiological analysis and investigations on the source of infection of postoperative infectious endophthalmitis in a tertiary care ophthalmic hospital: An 8-year study. Indian J Ophthalmol. 2010;58:297–302. doi: 10.4103/0301-4738.64132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ravindran RD, Venkatesh R, Chang DF, Sengupta S, Gyatsho J, Talwar B. Incidence of post-cataract endophthalmitis at Aravind Eye Hospital: Outcomes of more than 42,000 consecutive cases using standardized sterilization and prophylaxis protocols. J Cataract Refract Surg. 2009;35:629–36. doi: 10.1016/j.jcrs.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Assia E, Blumenthal M. Cataract surgery and incidence of postoperative endophthalmitis in Israel. Harefuah. 2005;144:768–71. 823. [PubMed] [Google Scholar]
- 21.Cavalcante LL, Cavalcante ML, Murray TG, Vigoda MM, Piña Y, Decatur CL, et al. Intravitreal injection analysis at the Bascom Palmer Eye Institute: Evaluation of clinical indications for the treatment and incidence rates of endophthalmitis. Clin Ophthalmol. 2010;4:519–24. doi: 10.2147/opth.s11094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jonisch J, Lai JC, Deramo VA, Flug AJ, Fastenberg DM. Increased incidence of sterile endophthalmitis following intravitreal preserved triamcinolone acetonide. Br J Ophthalmol. 2008;92:1051–4. doi: 10.1136/bjo.2007.136069. [DOI] [PubMed] [Google Scholar]
- 23.Artunay O, Yuzbasioglu E, Rasier R, Sengül A, Bahcecioglu H. Incidence and management of acute endophthalmitis after intravitreal bevacizumab (Avastin) injection. Eye (Lond) 2009;23:2187–93. doi: 10.1038/eye.2009.7. [DOI] [PubMed] [Google Scholar]
- 24.Ding Y, Lin M, Liu H, Zhang W, Wang L, Li Y. Outcomes of post-cataract surgery endophthalmitis referred to a tertiary center from local hospitals in the south of China. Infection. 2011;39:451–60. doi: 10.1007/s15010-011-0138-0. [DOI] [PubMed] [Google Scholar]
- 25.Cao X, Liu A, Zhang J, Li Y, Jie Y, Liu W, et al. Clinical analysis of endophthalmitis after phacoemulsification. Can J Ophthalmol. 2007;42:844–8. doi: 10.3129/i07-173. [DOI] [PubMed] [Google Scholar]
- 26.Chakrabarti A, Shivaprakash MR, Singh R, Tarai B, George VK, Fomda BA, et al. Fungal endophthalmitis: Fourteen years’ experience from a center in India. Retina. 2008;28:1400–7. doi: 10.1097/iae.0b013e318185e943. [DOI] [PubMed] [Google Scholar]
- 27.Oduyebo O, Odugbemi T, Idewu A, Adefule-Ositelu AA. Infection control audit and potential sources of infection of a Nigerian eye unit. West Afr J Med. 2007;26:196–200. doi: 10.4314/wajm.v26i3.28308. [DOI] [PubMed] [Google Scholar]
- 28.Dancer SJ, Stewart M, Coulombe C, Gregori A, Virdi M. Surgical site infections linked to contaminated surgical instruments. J Hosp Infect. 2012;81:231–8. doi: 10.1016/j.jhin.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 29.García-Sáenz MC, Arias-Puente A, Rodríguez-Caravaca G, Bañuelos JB. Effectiveness of intracameral cefuroxime in preventing endophthalmitis after cataract surgery Ten-year comparative study. J Cataract Refract Surg. 2010;36:203–7. doi: 10.1016/j.jcrs.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 30.Anderson EM, Noble ML, Garty S, Ma H, Bryers JD, Shen TT, et al. Sustained release of antibiotic from poly(2-hydroxyethyl methacrylate) to prevent blinding infections after cataract surgery. Biomaterials. 2009;30:5675–81. doi: 10.1016/j.biomaterials.2009.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]


