Abstract
Purpose:
To study the use of four petals evisceration in atrophia bulbi to allow insertion of large orbital implant.
Materials and Methods:
An interventional case series. All cases were atrophia bulbi. The axial lengths (AL) of atrophic and contralateral normal eye were measured. It was planned to use implant 3 mm smaller than AL of the contralateral normal eye. Four petals evisceration was used in all cases.
Results
Twenty cases were included. The mean age was 27.08 ± 16.07 years. The mean axial length (AL) of atrophic eyes was 16.97 ± 1.42 mm. In 75% of cases, the planned implant was inserted. In all cases, the implant diameter was larger than AL of atrophic eye by a mean of 2.57 ± 0.64 mm. The AL of atrophic eye did not affect the implant size. The mean follow-up period was 22.4 ± 10.1 months. Implant exposure was not recorded in any case. Volume deficiency was recorded in 2 cases (10%).
Conclusions:
Four petals evisceration facilitated the use of suitable sized implant in atrophia bulbi with minimal complications.
Keywords: Atrophia Bulbi, Evisceration, Scleral Modification
INTRODUCTION
In atrophia bulbi the eye becomes soft because of ciliary body dysfunction and progressive diminution of intraocular pressure. The globe becomes smaller and assumes a squared-off configuration. Most of the internal structures of the eye will be atrophic, but recognizable histologically. Atrophy, shrinkage, and disorganization of the eye and intraocular contents is called phthisis bulbi.1
Evisceration or enucleation procedures are indicated in these cases for cosmetic indications or to alleviate pain. Evisceration has the advantages of better preservation of orbital anatomy including the muscular insertions, better preservation of socket volume and motility leading to superior cosmetic and functional results.2,3,4
Until now, various techniques and modifications have been developed that allow placement of a large implant and avoid the risk of implant exposure or extrusion as well as to provide a better cosmetic effect.5 The technique of four petals evisceration was described by Sales-Sanz and Sanz-Lopez3 to facilitate the placement of large implant whether the eye was atrophic or not. Here, this technique was used in case series of atrophia bulbi.
MATERIALS AND METHODS
Interventional case series, which included cases of atrophia bulbi in the period between 2011 and 2013. The study adhered to the principles of the declaration of Helsinki and has been approved by the institutional ethical committee. Evisceration was indicated for cosmetic reasons or for blind painful eye [Figure 1a and b]. Before the surgery, A-scan measurements of the axial length (AL) of atrophic eye, and AL of normal eye were done (PacScan 300, Sonomed Inc, New York, USA). The diameter of the planned porous polyethylene implant was determined using Kaltreider and Lucarelli6 formula (AL of contralateral normal eye - 3 mm subtracting 1 mm for hyperopia). Four petals evisceration described by Sales-Sanz, and Sanz-Lopez3 was used in all cases. After separating the eyelids by eyelid speculum, a 360° conjunctival periotomy was performed, and the dissection was carried-out peripherally in the sub-Tenon's space. The insertion of the recti muscles was identified and marked by four 3\0 silk sutures to maintain the proper position of the muscles. The cornea was removed followed by the ocular contents. Four sclerotomies were performed between the rectus muscle insertions from the limbus to the optic nerve fashioning four scleral flaps (or petals). Each petal, containing 1 rectus muscle insertion was separated from the optic nerve [Figure 1c]. A set of sizing implants was used intraoperative before inserting the implant to ensure that it can be inserted easily, and the scleral flaps can be closed without tension. Porous polyethylene implant (Medpor) was used in all cases (Porex surgical, Newnan, Georgia, USA), and was placed inside the four petals. The vertical and horizontal scleral petals were sutured as two separate layers with interrupted 5-0 polyester sutures. Tenon's capsule and conjunctiva were sutured separately with 6-0 Vicryl sutures, and ocular conformer was placed at the end of surgery. Systemic antibiotics, as well as topical combined antibiotic-corticosteroid drops, were prescribed for the 1st week. The combined drops were used for the following 4 weeks. The patients were referred to an ocularist for fitting of the prosthesis 4-6 weeks after surgery [Figure 1d]. The motility of the implant was evaluated by marking the conjunctiva with a marker pen at the center point of the implant. The patients were instructed to look in four extreme gaze positions (medial, lateral, superior, and inferior), and the excursion of the mark was measured with a millimeter ruler.
Figure 1.
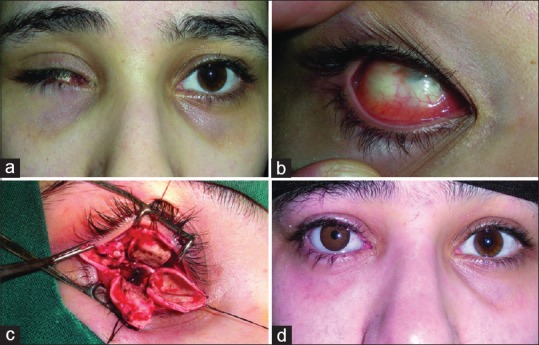
(a and b) Case of right atrophia bulbi, preoperative (c) intraoperative picture after fashioning the scleral flaps (d) postoperative, after fitting of the prosthesis
RESULTS
The study included 20 patients with unilateral atrophia bulbi in the period between 2011 and 2013. Twelve cases (60%) were females, and 8 cases (40%) were males. The age of patients ranged between 6, and 60 years with a mean of 27.08 ± 16.07 years. AL of atrophic eyes ranged between 15.23 mm, and 19.01 mm with a mean of 16.97 ± 1.42 mm. While AL of the normal contralateral eyes ranged between 21.08 mm, and 27.54 mm with a mean of 23.65 ± 2.11 mm. The implant used was larger than AL of atrophic eye by a mean of 2.57 ± 0.64 mm. AL of atrophic eye did not affect the implant size and did not affect the ability of inserting the planned suitable sized implant (P = 0.631, and 0.562, respectively). An implant of 18 mm diameter was used in 9 cases (45%), 20 mm was used in 7 cases (35%), and 22 mm was used in 4 cases (20%). The planned implant was inserted in 15 cases (75%). In 5 cases (25%), 2 mm smaller implant was used. Three of these 5 cases had a history of atrophia bulbi since early childhood. In these 3 cases, the intraoperative use of the implant sizing set showed that the planned implant would be too large, and scleral flaps would be under much tension. Other 2 cases had contralateral myopia, and the calculation formula gave implant size larger than 22 mm, which is not available. 22 mm implant was used in these 2 cases. The mean operative time was 56.6 ± 6.7 min. The follow-up period ranged between 10 months, and 42 months with a mean of 22.4 ± 10.1 months. Implant exposure was not recorded in any case. The implant motility had a mean of 8.9 ± 2.8 mm horizontal and 8.1 ± 1.6 mm vertical excursion. Volume deficiency with enophthalmos 3 mm or more, and or deep superior sulcus was recorded in 2 cases (10%).
DISCUSSION
The importance of complete volume replacement was emphasized as a primary object of orbital reconstruction procedures.7 Several materials have been used as orbital implants for volume replacement. Perry8 in 1990 first described the use of biointegrable implants in enucleated or eviscerated eyes. The choice of enucleation or evisceration procedure is controversial. In comparison with enucleation, the advantages of evisceration include relative preservation of tissue, better cosmetic result, superior motility of the prosthesis, and lower risk of intracranial infection or extrusion of orbital implant.9 Yousuf et al.10 found Evisceration a safe and quicker alternative to enucleation. They reported A change in surgical preference from enucleation to evisceration during the last 20-year. Shahd et al.11 in a national survey assessed the practice patterns regarding eye removal among oculoplastic surgeons. They found that surgeons who recently completed fellowship training are more likely to perform eviscerations than their senior counterparts.
Implant size has traditionally been determined on an empiric basis. Many surgeons use standard implants in all cases, which is often determined by the age of the patient.12,13 Others employ a set of sizing implants to ascertain, which is the most ideal for a particular individual.14,15 Insertion of an implant of inappropriate size results in a variety of complications. Excessively large implants are more prone to extrusion and may compromise the fitting and retention of comfort of the prosthesis. Placement of an abnormally small implant causes a volume deficit in the socket, contributing to a deep superior sulcus and the need for a large, poorly mobile prosthesis.16 For accurate determination of implant size, Custer and Trinkaus16 described the volumetric determination of implant size. This method is suitable for enucleation procedure only, as the volume of the enucleated tissue was measured by volume displacement with a sterile graduated cylinder filled with normal saline. Kaltreider and Lucarelli6 described a simple formula which allowed 100% volume replacement. They used implant diameter equals AL of the contralateral eye - 3 mm for the evisceration procedure.
The most common complication associated with porous orbital implants is exposure of the anterior implant surface. The actual incidences of implant exposure were variable in different reports using different surgical techniques. Viswanathan et al.17 in a national survey recorded 14% exposure rate after evisceration (18 of 128 cases). Detailed analysis of this complication was limited in this survey due to questionnaire design as specific clinical and surgical details were not requested. Wang et al.18 reported 11.4% exposure rate among evisceration cases in their series (8 of 70 cases). They used a corneal preservation technique with single posterior sclerotomy 5-10 mm from the optic nerve head, and 75% of exposure occurred in pegged implants. Other reports recorded lower exposure rates ranging from 3.3 to 6.5%.19,20 The main risk factors for exposure are inadequate surgical technique, covering the implant with high tension, and persistent conjunctival inflammation.3
Standard evisceration techniques typically only allow placement of a 13-16-mm spherical implant.21,22 To achieve optimum volume replacement with insertion of suitable large implant and reducing the tension on scleral flaps, the evisceration technique has undergone several modifications. Yang et al.23 described scleral quadrisection after evisceration, without releasing it from the optic nerve. Massry and Holds24 performed 2 full thickness sclerotomies from the anterior limbus incision to the optic nerve in inferonasal and superotemporal quadrants. Kim et al.25 used evisceration with four anterior full thickness scleral relaxing incisions between the recti muscles insertion to the equator, and circumferential posterior sclerotomy surrounding the optic nerve for 330°. Sales-Sanz and Sanz-Lopez3 described the four petals evisceration. They performed four sclerotomies from the limbus, between the recti muscles to the optic nerve with releasing the scleral flaps from the optic nerve. Huang et al.5 described a similar technique involving scleral quadrisection and suturing the implant with each rectus muscle through the scleral petal. In this series, which is the first to include only cases of atrophia bulbi, the four petals technique was used to facilitate the insertion of large implant and sclera closure without tension. The implant diameter was larger than AL of atrophic globe in all cases (mean 2.57 ± 0.64 mm). Implant of planned size could be inserted in 75% of cases (15 cases). In 25% of cases (5 cases), this was not possible. Three cases had a history of atrophia since early childhood, which could have an impact on the development of the bony orbit. While in 2 other cases the planned implant size was not available, and the largest possible implant (22 mm) was used. The AL of atrophic eye neither affected the implant size nor the ability of inserting the planned suitable sized implant. The follow-up period ranged between 10 months and 42 months with a mean of 22.4 ± 10.1 months. No implant exposure was recorded in any case. This was also reported by other authors.3,5,6,24,25 All these reports used different scleral division techniques to reduce the tension on the scleral flaps, which is the most important factor to avoid implant exposure.
Sclera quadrisection techniques may be complicated by posterior migration of the implant. Masry and holds24 argued that it is important to close the sclera at the equator to avoid posterior migration of nonintegrable implants. Sales-Sanz and Sanz-Lopez3 reported that the use of biointegrable implants prevented the possible posterior migration of the implant due to opening of the posterior sclera. This complication was not encountered here as biointegrable implants were used in all cases.
Volume deficiency was recorded in 2 cases (10%). Kim et al.25 reported that deep superior sulcus deformity was noted in 8.7%. Kaltreider and Lucarelli6 reported 15% incidence of volume deficiency, but this was recorded among patients with a history of infection, radiation, buphthalmos, or large orbital fractures. On the other hand, other authors recorded incidence of volume deficiency as low as 1.3%, or no volume deficiency.3,5
The mean operative time was 56.6 ± 6.7 min, which is longer than the previously reported time necessary for conventional evisceration technique. Yousuf et al.10 reviewed patients who underwent evisceration over 20 years and reported a mean operative time of 47.3 ± 10.3 min. The time necessary for fashioning the scleral flaps and suturing them may explain the longer operative time recorded in this series.
In conclusion, implant diameter 3 mm smaller than AL of the contralateral eye provides good volume replacement after evisceration in atrophia bulbi. The four petals technique facilitates the insertion of such large implant without tension on scleral flaps avoiding implant exposure, although it may take few minutes longer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grossniklaus HE, Brown HH, Glasgow BJ, Murray TG, Shetlar DJ, Wilson DJ, et al. Ophthalmic pathology and intraocular tumours. In: Liesegang TJ, Skuta GL, Cantar LB, editors. Basic and Clinical Science Course. San Francisco: American Academy of Ophthalmology; 2004. p. 28. [Google Scholar]
- 2.Collin JR, editor. In: A Manual of Systemic Eyelid Surgery. 3rd ed. Butterworth: Heinmann, Elsevier; 2006. Enucleation, evisceration, and socket surgery; p. 203. [Google Scholar]
- 3.Sales-Sanz M, Sanz-Lopez A. Four-petal evisceration: A new technique. Ophthal Plast Reconstr Surg. 2007;23:389–92. doi: 10.1097/IOP.0b013e318142cc4c. [DOI] [PubMed] [Google Scholar]
- 4.Dortzbach RK, Woog JJ. Choice of procedure. Enucleation, evisceration, or prosthetic fitting over globes. Ophthalmology. 1985;92:1249–55. doi: 10.1016/s0161-6420(85)33886-1. [DOI] [PubMed] [Google Scholar]
- 5.Huang D, Yu Y, Lu R, Yang H, Cai J. A modified evisceration technique with scleral quadrisection and porous polyethylene implantation. Am J Ophthalmol. 2009;147:924–8.e1. doi: 10.1016/j.ajo.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 6.Kaltreider SA, Lucarelli MJ. A simple algorithm for selection of implant size for enucleation and evisceration: A prospective study. Ophthal Plast Reconstr Surg. 2002;18:336–41. doi: 10.1097/00002341-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Culler AM. Enucleation and cosmetic rehabilitation; criteria for evaluation of current procedures. AMA Arch Ophthalmol. 1951;45:445–57. doi: 10.1001/archopht.1951.01700010455011. [DOI] [PubMed] [Google Scholar]
- 8.Perry AC. Integrated orbital implants. Adv Ophthalmic Plast Reconstr Surg. 1990;8:75–81. [PubMed] [Google Scholar]
- 9.Hansen AB, Petersen C, Heegaard S, Prause JU. Review of 1028 bulbar eviscerations and enucleations. Changes in aetiology and frequency over a 20-year period. Acta Ophthalmol Scand. 1999;77:331–5. doi: 10.1034/j.1600-0420.1999.770317.x. [DOI] [PubMed] [Google Scholar]
- 10.Yousuf SJ, Jones LS, Kidwell ED., Jr Enucleation and evisceration: 20 years of experience. Orbit. 2012;31:211–5. doi: 10.3109/01676830.2011.639477. [DOI] [PubMed] [Google Scholar]
- 11.Shah RD, Singa RM, Aakalu VK, Setabutr P. Evisceration and enucleation: A national survey of practice patterns in the United States. Ophthalmic Surg Lasers Imaging. 2012;43:425–30. doi: 10.3928/15428877-20120725-01. [DOI] [PubMed] [Google Scholar]
- 12.Nunery WR, Cepela MA, Heinz GW, Zale D, Martin RT. Extrusion rate of silicone spherical anophthalmic socket implants. Ophthal Plast Reconstr Surg. 1993;9:90–5. doi: 10.1097/00002341-199306000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Shields CL, Shields JA, De Potter P, Singh AD. Problems with the hydroxyapatite orbital implant: Experience with 250 consecutive cases. Br J Ophthalmol. 1994;78:702–6. doi: 10.1136/bjo.78.9.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashworth JL, Rhatigan M, Brammar R, Sunderland S, Leatherbarrow B. A clinical study of the hydroxyapatite orbital implant. Eur J Ophthalmol. 1997;7:1–8. doi: 10.1177/112067219700700101. [DOI] [PubMed] [Google Scholar]
- 15.Karesh JW, Dresner SC. High-density porous polyethylene (Medpor) as a successful anophthalmic socket implant. Ophthalmology. 1994;101:1688–95. [PubMed] [Google Scholar]
- 16.Custer PL, Trinkaus KM. Volumetric determination of enucleation implant size. Am J Ophthalmol. 1999;128:489–94. doi: 10.1016/s0002-9394(99)00252-4. [DOI] [PubMed] [Google Scholar]
- 17.Viswanathan P, Sagoo MS, Olver JM. UK national survey of enucleation, evisceration and orbital implant trends. Br J Ophthalmol. 2007;91:616–9. doi: 10.1136/bjo.2006.103937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang JK, Lai PC, Liao SL. Late exposure of the bioceramic orbital implant. Am J Ophthalmol. 2009;147:162–70.e1. doi: 10.1016/j.ajo.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Kostick DA, Linberg JV. Evisceration with hydroxyapatite implant. Surgical technique and review of 31 case reports. Ophthalmology. 1995;102:1542–8. doi: 10.1016/s0161-6420(95)30833-0. [DOI] [PubMed] [Google Scholar]
- 20.Blaydon SM, Shepler TR, Neuhaus RW, White WL, Shore JW. The porous polyethylene (Medpor) spherical orbital implant: A retrospective study of 136 cases. Ophthal Plast Reconstr Surg. 2003;19:364–71. doi: 10.1097/01.IOP.0000083643.36461.84. [DOI] [PubMed] [Google Scholar]
- 21.Soll DB. The anophthalmic socket. Ophthalmology. 1982;89:407–23. doi: 10.1016/s0161-6420(82)34774-0. [DOI] [PubMed] [Google Scholar]
- 22.Zolli CL. Implant extrusion in eviscerations. Ann Ophthalmol. 1988;20:127–32. 135. [PubMed] [Google Scholar]
- 23.Yang JG, Khwarg SI, Wee WR, Kim DM, Lee JH. Hydroxyapatite implantation with scleral quadrisection after evisceration. Ophthalmic Surg Lasers. 1997;28:915–9. [PubMed] [Google Scholar]
- 24.Massry GG, Holds JB. Evisceration with scleral modification. Ophthal Plast Reconstr Surg. 2001;17:42–7. doi: 10.1097/00002341-200101000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Kim KH, Lee H, Park M, Chi Mc, Lee J, Baek S. Evisceration with four anterior relaxing incisions and circumferential posterior sclerotomies with porous polyethylene orbital implants: An 8-year study. Acta Ophthalmol. 2011;89:686–90. doi: 10.1111/j.1755-3768.2009.01825.x. [DOI] [PubMed] [Google Scholar]


