Abstract
Aims:
The aim was to describe the epidemiology of primary eyelid tumors over a 30-year period at the Ioannina University Eye Clinic, Greece.
Materials and Methods:
This retrospective case series examined the histopathology of eyelid tumor specimens of patients treated between 1983 and 2012. Data were collected on patient age, gender, location of the lesion, extent of tumor excision and recurrence. Descriptive and inferential statistics were used to describe the study subgroups.
Results:
A total of 851 eyelid tumors comprised the study sample. There were 351 (41.2%) malignant cases and 500 (58.8%) benign cases. For malignant tumors, there were 86% basal cell carcinomas, 7% squamous cell carcinomas, and 7% basosquamous cell carcinomas. The benign eyelid lesions were comprised of 20% cysts, 18% seborrheic keratosis, 13% nevi, and 13% papillomas. Benign eyelid lesions occurred with equal frequency in the upper and lower lids. Malignant lesions were more frequently located in the lower lid. The mean age at diagnosis was 49 ± 1.45 years for patients with benign lesions and 67 ± 1.6 years for patients with malignant lesions.
Conclusions:
In this Greek cohort, benign eyelid lesions affected mostly young individuals, and malignant lesions occurred predominantly in elderly patients. Males and females were equally affected by malignant lesions, and recurrence after surgical excision was rare.
Keywords: Basal Cell Carcinoma, Benign, Eyelids, Histology, Malignant, Squamous Cell Carcinoma, Tumors
INTRODUCTION
Eyelid tumors are the most common neoplasms encountered in ophthalmology.1,2 The clinical characteristics and epidemiology of patients with eyelid tumors have yet to be described for Greek populations. The objective of this study was to determine the epidemiological and clinical characteristics of eyelid tumors encountered in a Caucasian population from a rural region in northwest Greece (Epirus).
MATERIALS AND METHODS
A retrospective chart review was performed of patients who underwent excision of eyelid lesions from January 1983 to December 2012 at the Ophthalmology Clinic of the University Hospital of Ioannina, Greece. Tumor diagnosis and classification were based on histopathology using routine hematoxylin and eosin staining according to the World Health Organization classification criteria.3 All excisions were performed by specialist ophthalmologists, and histopathology reports were dictated by specialist histopathologists.
Data were also collected on patient age, sex, tumor location, extent of excision and recurrences. Data are presented as absolute numbers and percentages for binary and categorical variables and as mean with a standard deviation and 95% confidence intervals (CIs) (95% CI) for continuous variables. Chi-square tests and independent samples t-tests were used for group comparisons. Statistical significance was indicated by P < 0.05. Excel software (Microsoft Corp., Redmond, WA, USA) was used for all analyses.
RESULTS
A total of 851 specimens (351 malignant vs. 500 benign tumors) from 421 Caucasian males (49.5%) and 430 females (50.5%) were retrieved and analyzed. The mean age was 49.0 ± 1.5 years (95% CI: 48.8–49.2 years) for patients with benign lesions and 67.5 ± 1.6 years (95% CI: 67.3–67.7 years) for patients with malignant lesions (P < 0.01).
About 86% (303/351) of malignant tumors were basal cell carcinomas (BCC), 7% (25/351) were squamous cell carcinomas (SCC), 5% (17/351) were basosquamous cell carcinomas, and 2% (6/351) were malignant melanomas [Figure 1]. Twenty percent (100/500) of benign lesions were cysts, 18% (90/500) were seborrheic keratoses, 13% (64/500) were nevi, 13% (66/500) were papillomata, 10% (48/500) were chalazia, 6% (30/500) were hemangiomas, 4% (20/500) were actinic keratoses and the remainder (16%) were comprised of rare lesions such as hydrocystoma, xanthelasma, pilomatricoma, keratoacanthoma, etc.
Figure 1.
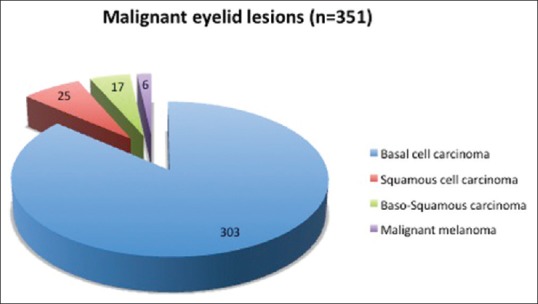
Malignant lesions in a rural Caucasian population from northwest Greece
Malignant tumors were located on the lower eyelid in 67% of cases, on the upper eyelid in 15% of the cases and the medial canthal region in 15% of the cases. Benign lesions occurred in 42% of the cases in the upper eyelids and in 45% of the cases in the lower eyelids (P = 0.745).
In our study, 52% (159) of the patients with BCC were male and 48% (144 cases) were female (P = 0.097). The mean age was 66.6 ± 1.32 years (95% CI: 66.4–66.8 years) for males and 67.0 ± 1.49 years (95% CI: 66.8–67.2 years) for females (P = 0.910). The mean age of the patients with SCC was 72.0 ± 1.8 years (95% CI: 71.0–72.9 years) for males and 78.75 ± 1.76 (95% CI: 77.7–79.8 years) for females.
The overall recurrence was 6.5% (23 cases) for malignant tumors. In these patients, the primary histological diagnosis was BCC (19 cases) and SCC (4 cases).
DISCUSSION
In the current study, approximately 40% of the excised lesions were malignant. This alarming proportion should increase awareness of health care workers, policy makers and the public regarding eyelid lesions in rural Caucasian populations exposed to high levels of solar radiation.
In this report, 59% of the eyelid lesions were benign. This contrasts to data from Switzerland1 (84% benign lesions) and China4 (86.2% benign lesions). Differences in the study populations, methodology, and the health systems may explain these discrepancies.
Patients with benign lesions were younger than those with malignant lesions, which concurs with previous studies.1,4,5 Benign lesions were found in the upper or lower eyelids with almost equal frequency, whereas malignant tumors occurred most often in the lower eyelid (67%). This difference may be related to the increased solar exposure of the lower eyelid.
Results of similar studies from other countries may vary considerably. In our patients, the most common malignancy was BCC (86%), followed by SCC (7%), basosquamous cell carcinoma (5%), and malignant melanoma (2%). A study from Switzerland reported that BCC was also the most common malignancy (84%), followed by SCC (7%) and sebaceous carcinoma (3%).1 Lin et al.6 reported that the most common eyelid tumors in Taiwan were BCC (65.1%), SCC (12.6%) and sebaceous gland carcinoma (7.9%).6 Interestingly, in some Asian populations, sebaceous gland carcinoma may be the second most common eyelid malignancy while SCC the third.7 Such differences across countries may be due to variations in skin type, genetic predisposition, geographical latitude, health-related behaviors, disease awareness and surveillance.6
Basal cell carcinomas are locally destructive but rarely life-threatening neoplasms.2 Although the average age for patients with BCC was 67 years, there were thirteen patients younger than 40 years, including one 7-year-old boy.2
In Western countries, SCC is the second most common eyelid malignancy.1 The relative frequency of SCC varies widely in different studies, likely due to a similar presentation of SCC to other tumors resulting in diagnostic ambiguity and misclassification.
Malignant eyelid tumors other than BCC and SCC are rare and usually occur in elderly Caucasians.1 Only six malignant melanomas were found in our study. Nevertheless, malignant melanoma carries a poor prognosis if local measures fail, with two-thirds of all deaths from skin cancer due to this tumor.2,8 Sebaceous carcinomas are among the rarest skin tumors (0.2–4.6%).6,9 In contrast to BCCs, these are rare in Caucasians but more common in Asians.6,9,10 We identified only one case of histologically confirmed sebaceous gland carcinoma. Of note, this particular malignancy may be underdiagnosed because distinguishing sebaceous gland carcinomas from benign conditions (e.g., blepharoconjunctivitis, blepharitis, and chalazion) or malignant lesions such as SCC can be challenging.9
In this study, all malignant lesions were surgically excised and sent for histopathological examination. It is significant that from 1983 to 1993, 53% of excisions for BCC and SCC were incomplete. However, this rate decreased to 33% from 1993 to 2002 and to 25.8% from 2003 to 2012. This trend was attributed to the introduction of an operating microscope and surgeon experience.
In summary, our results show that benign eyelid lesions are generally found in younger individuals, and occur with equal frequency in the upper and lower eyelids. In contrast, malignant lesions occur predominantly in elderly patients and are usually located in the lower eyelid. The use of an operating microscope is strongly recommended for the excision of eyelid tumors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. Am J Dermatopathol. 2009;31:256–62. doi: 10.1097/DAD.0b013e3181961861. [DOI] [PubMed] [Google Scholar]
- 2.Allali J, D’Hermies F, Renard G. Basal cell carcinomas of the eyelids. Ophthalmologica. 2005;219:57–71. doi: 10.1159/000083263. [DOI] [PubMed] [Google Scholar]
- 3.LeBoit PE, Burg G, Weedon D, Sarasin A, editors. Lyon: IARC Press; 2006. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of the Skin. [Google Scholar]
- 4.Xu XL, Li B, Sun XL, Li LQ, Ren RJ, Gao F, et al. Eyelid neoplasms in the Beijing Tongren Eye Centre between 1997 and 2006. Ophthalmic Surg Lasers Imaging. 2008;39:367–72. doi: 10.3928/15428877-20080901-18. [DOI] [PubMed] [Google Scholar]
- 5.Wang JK, Liao SL, Jou JR, Lai PC, Kao SC, Hou PK, et al. Malignant eyelid tumours in Taiwan. Eye (Lond) 2003;17:216–20. doi: 10.1038/sj.eye.6700231. [DOI] [PubMed] [Google Scholar]
- 6.Lin HY, Cheng CY, Hsu WM, Kao WH, Chou P. Incidence of eyelid cancers in Taiwan: A 21-year review. Ophthalmology. 2006;113:2101–7. doi: 10.1016/j.ophtha.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Chang CH, Chang SM, Lai YH, Huang J, Su MY, Wang HZ, et al. Eyelid tumors in southern Taiwan: A 5-year survey from a medical university. Kaohsiung J Med Sci. 2003;19:549–54. doi: 10.1016/S1607-551X(09)70505-4. [DOI] [PubMed] [Google Scholar]
- 8.Chan FM, O’Donnell BA, Whitehead K, Ryman W, Sullivan TJ. Treatment and outcomes of malignant melanoma of the eyelid: A review of 29 cases in Australia. Ophthalmology. 2007;114:187–92. doi: 10.1016/j.ophtha.2006.08.043. [DOI] [PubMed] [Google Scholar]
- 9.Warnecke KK, Sieg P. Sebaceous carcinoma of the eyelids – Case reports and review of the literature. Klin Monbl Augenheilkd. 2006;223:771–4. doi: 10.1055/s-2006-926809. [DOI] [PubMed] [Google Scholar]
- 10.Pornpanich K, Chindasub P. Eyelid tumors in Siriraj Hospital from 2000-2004. J Med Assoc Thai. 2005;88(Suppl 9):S11–4. [PubMed] [Google Scholar]


