Abstract
Acinetobacter lwoffii is a rare cause of endophthalmitis. We report a case of acute postoperative endophthalmitis in a female, who was treated successfully with pars plana vitrectomy and intravitreal antibiotics.
Keywords: Acinetobacter, Acinetobacter lwoffii, Endophthalmitis, Phacoemulsification, Vitrectomy
INTRODUCTION
Infective endophthalmitis is a devastating condition that can result in permanent loss of vision. The clinical outcomes of the infective endophthalmitis often depend on the nature of the infective strain. Acinetobacter lwoffii is a rare cause of endophthalmitis with only two previously published reports, which were posttraumatic in etiology.1,2 We report the first case of postoperative endophthalmitis caused by this bacteria and describe the trends of drug sensitivity.
CASE REPORT
A 57-year-old diabetic, nonhypertensive female presented to with complaints of severe pain and decreased vision in left eye, 5 days after uneventful phacoemulsification and intraocular lens implantation. On examination, the best-corrected visual acuity was 20/40 in right eye and light perception in the left eye. Slit-lamp biomicroscopy of the left eye showed lid edema, congested conjunctiva, microcystic corneal edema with severe anterior chamber reaction and a 2 mm brown hypopyon [Figure 1]. There was no view of the fundus in her left eye. Ultrasonography of the left eye revealed an attached retina with dense vitreous echoes.
Figure 1.
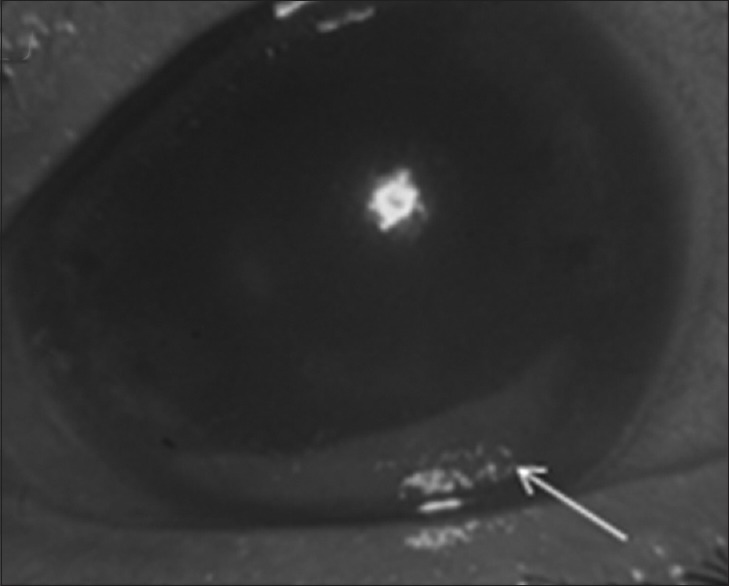
Anterior segment photograph of the left eye at presentation reveals diffuse corneal edema and a thick brown hypopyon (arrow)
She underwent a standard undiluted vitreous biopsy, pars plana vitrectomy with removal of the intraocular lens, followed by administration of intravitreal antibiotics twice (vancomycin 1 mg, ceftazidime 2.25 mg and dexamethasone 0.1 mg).
Acinetobacter lwoffii was isolated from more than one media. Identification was performed to the species level by application of standard biochemical reactions. Antibiotic-disc diffusion test was performed according to CSLI guidelines. The organism was sensitive to cefotaxime and ceftazidime, and was resistant to ciprofloxacin, amikacin, gentamicin and vancomycin. The patient was prescribed intensive topical therapy. In addition, intravitreal injections of ceftazidime and dexamethasone were administered thrice during follow-up. At last visit, 8 weeks postoperatively, the best-corrected visual acuity improved to 20/120. The anterior segment was quiet with a clear vitreous cavity and an attached retina [Figure 2a and b].
Figure 2.
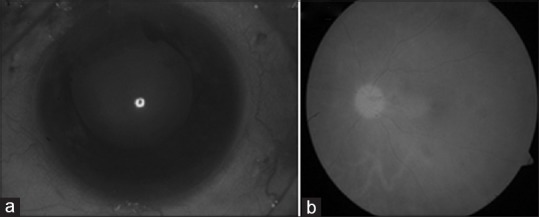
(a) Postoperative anterior segment photograph reveals a clear cornea and a good red glow. (b) Postoperative fundus photograph of the left eye reveals clear media with a healthy disc and an attached retina
DISCUSSION
Acinetobacter is a nonmotile Gram-negative coccobacilli classified under the family Moraxcellaceae. These organisms have variable virulence but can be multidrug resistant. Being ubiquitous in nature, this bacterium is part of the normal flora of the oropharynx, human skin, and the perineum in approximately 20–25% of healthy individuals.3 In patients with an impaired or compromised immune system, the bacteria turn into an opportunistic pathogen that can cause nosocomial infection. Cohen et al.4 reported growth of A. lwoffii in intraocular fluid culture after routine pars plana vitrectomy. In our patient, A. lwoffii was isolated from more than one media [Figure 3] and to the best of our knowledge, this is the first report of postoperative acute endophthalmitis induced by A. lwoffIi in the English peer review literature. Although A. lwoffii are an important cause of nosocomial infections, our case was exogenous in origin. The present case had an early presentation indicating the virulence of the organism. One striking feature was the presence of a brown colored hypopyon. Hypopyon that are brown in color has been reported in the setting of necrotic intraocular melanoma as well as endophthalmitis due to Listeria monocytogenes, Serratia marcescens and Streptococcus bovis.5 It may be an important distinguishing sign for A. lwoffii induced endophthalmitis as well. However, further studies are required prior to establishing A. lwoffii as the cause for brown hypopyon. Antimicrobial resistance of Acinetobacter species is a serious concern. The resistance pattern of the A. lwoffii isolate could be similar to other Acinetobacter species, which produce an AmpC beta-lactamase that inactivates aminopenicillins and narrow-spectrum cephalosporins, but remain susceptible to ceftazidime, cefepime, imipenem, aminoglycosides, cotrimoxazole and systemic fluoroquinolones such as levofloxacin and ciprofloxacin. Though Gopal et al.6 had reported a high level of sensitivity to ciprofloxacin by the Acinetobacter species; our isolate was resistant to ciprofloxacin. Our patient had a favorable outcome at final visit similar to previous reports on A. lwoffii endophthalmitis.
Figure 3.
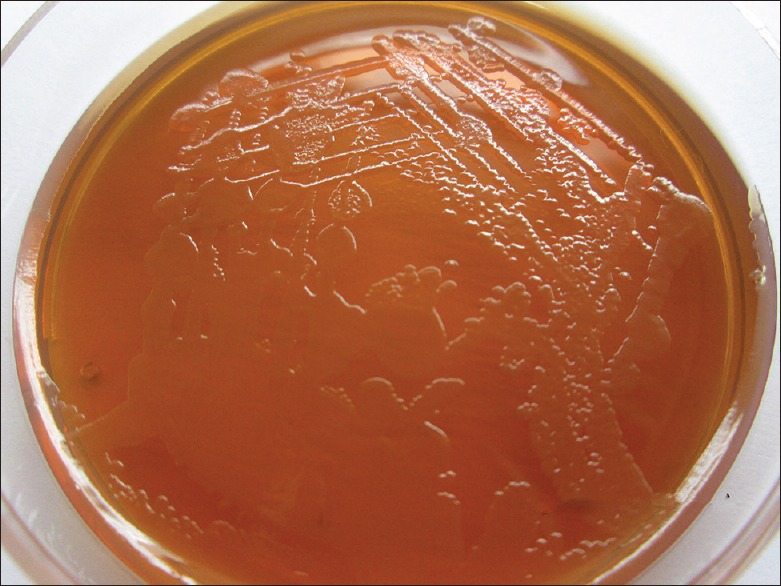
MacConkey agar shows growth of round colonies (1–2 mm in diameter) with irregular margins which are pale (nonlactose fermenting) consistent with Acinetobacter
To conclude this study adds to the body of literature on endophthalmitis caused A. lwoffii and provides the drug sensitivity patterns.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Melki TS, Sramek SJ. Trauma-induced Acinetobacter lwoffi endophthalmitis. Am J Ophthalmol. 1992;113:598–9. doi: 10.1016/s0002-9394(14)74744-0. [DOI] [PubMed] [Google Scholar]
- 2.Peyman GA, Raichand M, Bennett TO. Management of endophthalmitis with pars plana vitrectomy. Br J Ophthalmol. 1980;64:472–5. doi: 10.1136/bjo.64.7.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ku SC, Hsueh PR, Yang PC, Luh KT. Clinical and microbiological characteristics of bacteremia caused by Acinetobacter lwoffii. Eur J Clin Microbiol Infect Dis. 2000;19:501–5. doi: 10.1007/s100960000315. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SM, Benner JD, Landers MB, 3rd, Morse LS. Intraocular fluid cultures after primary pars plana vitrectomy. Am J Ophthalmol. 1992;114:697–9. doi: 10.1016/s0002-9394(14)74047-4. [DOI] [PubMed] [Google Scholar]
- 5.Hauch A, Eliott D, Rao NA, Vasconcelos-Santos DV, O’Hearn T, Fawzi AA. Dark hypopyon in Streptococcus bovis endogenous endophthalmitis: Clinicopathologic correlations. J Ophthalmic Inflamm Infect. 2010;1:39–41. doi: 10.1007/s12348-010-0008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gopal L, Ramaswamy AA, Madhavan HN, Battu RR, Sharma T, Shanmugam MP, et al. Endophthalmitis caused by Acinetobacter calcoaceticus. A profile. Indian J Ophthalmol. 2003;51:335–40. [PubMed] [Google Scholar]


