Abstract
A young female presented with blurred vision in the left eye after she rubbed her eye. On examination of both eyes, she had 360° thinning adjacent to the limbus, lipid deposition and superficial vascularization with a perforation in the left eye. The patient was diagnosed with bilateral Terrien's marginal degeneration (TMD) with perforation. Corneal topography of the right eye revealed high oblique astigmatism confirming the diagnosis. A peripheral patch graft was performed for the left eye. At 18 months postoperatively, the best-corrected visual acuity was 20/20 in both eyes. The graft was clear. Topography of right eye was stable, and the left eye had oblique astigmatism. Bilateral advanced TMD in a young patient presenting with corneal perforation following trivial trauma is extremely uncommon. Patch graft may be an option for restoring the globe integrity in such cases. Regular follow-up is necessary as the condition progresses slowly.
Keywords: Corneal Perforation, Patch Graft, Peripheral Corneal Degeneration, Terrien's Marginal Degeneration
INTRODUCTION
Terrien's marginal degeneration (TMD) is a rare peripheral corneal ectatic disorder typically occurring in males over 40 years old1 with a variant with episodic inflammation occurring in younger patients.2 Initial management involves prescription of glasses or contact lenses for astigmatism, however, surgical intervention is usually required for advanced cases with ectasia and high astigmatism. We describe a rare case of bilateral TMD with 360° corneal involvement in a young female presenting with corneal perforation in one eye following trivial trauma.
CASE REPORT
A 23-year-old female nurse presented to the emergency room with complaints of pain, redness, and decreased vision in the left eye, which started after rubbing the eye. She had a history of recurrent redness and pain in both eyes for the past 5 years, which subsided with some medication purchased over-the-counter at a local pharmacy. Her uncorrected visual acuity in the right eye was 20/100 improving to 20/20 with + 0.50DS/−5.50DC × 50°. The visual acuity in the left eye was 20/160. The anterior segment examination in the right eye revealed 360° peripheral corneal thinning associated with superficial vascularization and lipid deposition at the leading edge [Figure 1a]. The overlying epithelium was intact. There was no evidence of scleral inflammation. The left eye had a 5 mm × 2 mm corneal perforation with uveal prolapse from 10 to 2 O’clock adjacent to the superior limbus, with peripheral thinning, superficial vascularization and lipid deposition in the entire circumference [Figure 1b]. She had no history of joint pains, skin rash or respiratory problems. A systemic examination was not suggestive of any collagen vascular disorder. The patient was diagnosed with bilateral TMD with perforation in the left eye. Corneal topography of the right eye showed high oblique astigmatism with Sim K values of 48.75D at 140° and 43.25D at 50° [Figure 2a] thereby confirming this diagnosis. A tectonic corneal patch graft with iris abscission was performed for the left eye by hand fashioning the donor tissue to fit the perforation. The size of the perforation was measured using calipers, and a 0.5 mm larger trephine (5.5 mm) was selected to make a groove on the cornea. A rim of recipient corneal tissue was excised along the groove. The uveal tissue was abscissed. A 6.0 mm trephine was used to punch the donor tissue with an Iowa punch. The donor tissue was transferred to the recipient bed and anchored at the limbus and to the recipient cornea with 10-0 nylon sutures. The excess donor tissue was excised along the recipient limbus ensuring good alignment. This edge was also sutured with 10-0 nylon interrupted sutures. Postoperatively the patient was prescribed 0.3% gatifloxacin eye drops 6 times/day for 2 weeks and 1% Prednisolone acetate eye drops hourly with a gradual taper over a 1-year. Polycarbonate protective glasses were prescribed. On follow-up visits, the graft remained clear, and the anterior chamber was well formed [Figure 1c]. All sutures have been removed. The best-corrected visual acuity was 20/20 with + 0.50DS/−5.50DC × 50° and −1.50DS/−3.00DC × 100° in the right and left eyes respectively. Corneal topography performed for both eyes at 18 months showed no change in the right eye and in the left eye, the Sim K was 49.37D at 14° and 45.37D at 104° [Figure 2b]. She has been asked to follow-up at regular intervals and is on low maintenance dose of topical steroid in the left eye along with artificial tears.
Figure 1.
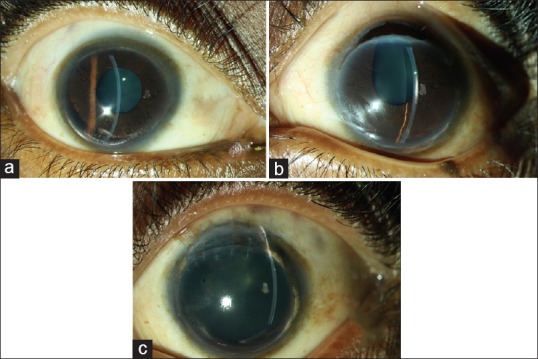
(a) Slit lamp photograph of the right eye showing 360° peripheral corneal thinning with areas of lipid deposition and superficial vascularization. (b) Slit lamp photograph of the left eye showing a corneal perforation with iris prolapse adjacent to the limbus. (c) Slit lamp photograph of the left eye showing the clear graft superiorly with areas of lipid deposition superonasally and inferiorly
Figure 2.
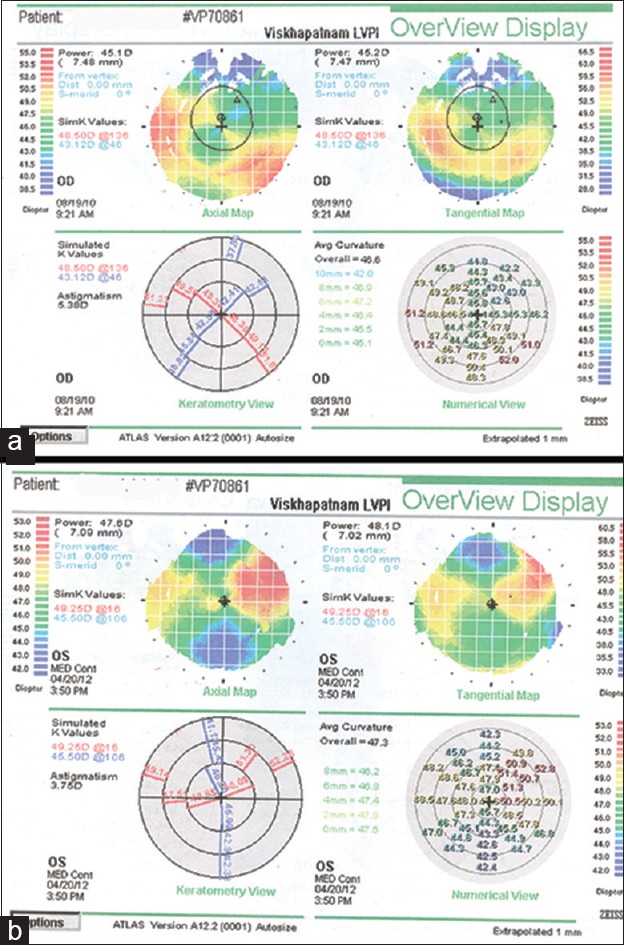
(a) Topography of the right eye showing high oblique astigmatism with a classical “lobster claw” pattern on the axial map and skewing of the principal meridians. (b) Topography of the left eye after the patch graft showing irregular astigmatism and flattening of the cornea in the vertical meridian with steepening in the horizontal meridian
DISCUSSION
Terrien's marginal degeneration is a rare slowly progressive peripheral ectatic degenerative corneal disease characterized by superficial vascularization, scarring and thinning with lipid deposition at the advancing edge, which commences superiorly and progresses circumferentially.3 The disease progresses very slowly and thus advanced bilateral 360° involvement in a young patient as seen in our case is extremely uncommon indicating a need for close monitoring of these patients for early diagnosis of progression.
Patients usually present with blurred vision due to irregular astigmatism4 and recurrent redness and pain are common manifestations in young patients with the inflammatory form of the disease.2,5 Our patient presented with blurred vision due to perforation following trivial trauma.
Complications in the form of perforation may occur in 15% of the cases.3 However a review of the literature revealed just a few reports of corneal perforation in TMD.6,7,8,9 Three of four cases with perforation described by Richards were managed with observation alone.6 Conjunctival flaps,6 penetrating keratoplasty and bandage soft contact lenses9 have been used with success in the management of perforations in TMD. Since our patient presented with a 5 mm × 2 mm perforation in the superior cornea and had good visual potential, the best option was a peripheral patch graft. A tectonic hand fashioned patch graft was performed with good visual outcome. Since the condition is slowly progressive, patients may develop thinning, ectasia and perforation at other affected sites and hence regular follow-up is advocated.
CONCLUSION
Terrien's marginal degeneration may present with advanced 360° involvement in young patients. Though rare, perforation following trivial trauma is a serious problem and warrants close observation. Patch graft is a good surgical option for peripheral perforations in TMD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Duke-Elder S, editor. St. Louis: Mosby; 1965. System of Ophthalmology. Diseases of the Outer Eye; pp. 909–13. [Google Scholar]
- 2.Austin P, Brown SI. Inflammatory Terrien's marginal corneal disease. Am J Ophthalmol. 1981;92:189–92. doi: 10.1016/0002-9394(81)90768-6. [DOI] [PubMed] [Google Scholar]
- 3.Chang RI, Ching S. Corneal and conjunctival degenerations. In: Krachmer J, Mannis M, Holland E, editors. Cornea. Fundamentals, Diagnosis and Management. St. Louis: Mosby; 2011. pp. 901–17. [Google Scholar]
- 4.Pesudovs K. Terriens marginal degeneration. Case reports and literature review. Clin Exp Optom. 1994;77:97–104. [Google Scholar]
- 5.Fernandes M. Scanning slit topography: Diagnostic boon in presumed unilateral Terrien's marginal degeneration. Cont Lens Anterior Eye. 2011;34:282–6. doi: 10.1016/j.clae.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Richards WW. Marginal degeneration of the cornea with perforation. Arch Ophthalmol. 1963;70:610–5. doi: 10.1001/archopht.1963.00960050612006. [DOI] [PubMed] [Google Scholar]
- 7.Pouliquen Y, Dhermy P, Renard G, Goichot-Bonnat L, Foster G, Savoldelli M. Terrien's disease: Clinical and ultrastructural studies, five case reports. Eye (Lond) 1989;3:791–802. doi: 10.1038/eye.1989.123. [DOI] [PubMed] [Google Scholar]
- 8.Lopez JS, Price FW, Jr, Whitcup SM, Li Q, de Smet M, Chan CC. Immunohistochemistry of Terrien's and Mooren's corneal degeneration. Arch Ophthalmol. 1991;109:988–92. doi: 10.1001/archopht.1991.01080070100045. [DOI] [PubMed] [Google Scholar]
- 9.Srinivasan S, Murphy CC, Fisher AC, Freeman LB, Kaye SB. Terrien marginal degeneration presenting with spontaneous corneal perforation. Cornea. 2006;25:977–80. doi: 10.1097/01.ico.0000226367.41925.ab. [DOI] [PubMed] [Google Scholar]


