Abstract
Background and Aims:
Shortening the duration of efficacious preoxygenation would provide benefit in emergency situations like fetal distress etc. This study aims to compare the margin of safety following preoxygenation using 8 vital capacity breaths (VCB) in 1 min and tidal volume breathing (TVB) for 3 min, by assessing changes in PaO2 and apnea induced desaturation time.
Material and Methods:
Patients were randomly divided into Group A and B. In Group A, 3 min of TVB using O2 flow of 5 l/min and in Group B, 8 VCB in 60 s using O2 flow of 10 l/min were used. Anesthesia was induced in all patients with propofol followed by succinylcholine 2 mg/kg intravenously. Mask ventilation was not done and following intubation endotracheal tube was kept open to atmosphere. The time taken for the patients to desaturate to 90% was noted and immediately ventilation was resumed. Arterial blood gas samples were taken while patients were breathing room air, immediately after preoxygenation and at 90% desaturation.
Results:
Baseline PaO2 of both the groups were comparable. After preoxygenation Group B had a significantly high PaO2 value than Group A (439.05 ± 62.20 vs. 345.16 ± 20.80). At 90% desaturation there was no significant difference between groups. Group B showed a significantly high apnea induced desaturation time when compared to Group A (6.87 ± 1.78 vs. 3.47 ± 0.38 min).
Conclusions:
Preoxygenation by 8 VCB in 1 min provides a greater margin of safety, as it results in a significantly high PaO2 with an almost doubled apnea induced desaturation time, in comparison with TVB for 3 min.
Keywords: Arterial oxygen tension, preoxygenation, tidal volume breathing, vital capacity breathing
Introduction
Maximal preoxygenation prior to induction of general anesthesia is essential in situations of difficult intubation/mask ventilation.[1,2] However in certain clinical situations like fetal distress, lifesaving emergencies etc., shorter preoxygenation would be more appropriate, if it is as effective as the traditional way of tidal volume breathing (TVB) of 100% O2 for 3 min.
We aimed to compare the margin of safety following preoxygenation using 8 vital capacity breaths (VCB) in 1 min and TVB for 3 min, by assessing changes in arterial partial pressure of oxygen and apnea induced desaturation time.
Material and Methods
As the difference in the mean values of the two important parameters, PaO2 (215.13 ± 47.76 vs. 327.49 ± 56.3, P <0.00005) and desaturation time (3.70 ± 0.44 vs. 4.70 ± 0.27, P < 0.005) in the previous study by Singh et al.[3] was high, the minimum sample size when calculated initially, with 80% confidence and 90% power, was very small. Hence, the sample size was finally calculated with 99% confidence and 99% power and each group required 10 patients to get statistically significant results.
Hence, 20 American Society of Anesthesiologist Grade I and II patients of both sexes, aged 20-60 years, scheduled for surgical procedures under GA with endotracheal intubation requiring invasive blood pressure (BP) monitoring, were included in this randomized clinical trial, which was conducted from September 2012 to May 2013. Patients with ischemic heart disease, chronic obstructive pulmonary disease obesity (body mass index >30), anemia and anticipated difficult airway were excluded. Approval of the hospital ethical committee and written informed consent from all patients were obtained.
Patients were randomly allocated to one of the two groups using computer generated sequence of random numbers. In Group A, 3 min of TVB using oxygen flow of 5 l/min was used whereas in Group B, patients were asked to take 8 VCB in 60 s using O2 flow of 10 l/min.
After obtaining a venous access in the operation theatre a finger probe pulse oximeter, noninvasive BP and electrocardiogram were connected to the patient. A good tracing was ensured in the pulseoxymeter. The radial artery was cannulated (22G) under local anesthesia for arterial blood sampling and invasive BP monitoring. Circle anesthesia system with a 3 L capacity reservoir bag and proper sized tight fitting face masks were used for preoxygenation.
Following preoxygenation with either method, induction of anesthesia was achieved with propofol 2-2.5 mg/kg body weight followed by succinylcholine 2 mg/kg intravenously (IV). Positive pressure ventilation was not administered, and the time at which patients became apneic was noted, that is, time at which there was the cessation of bag movement and/or EtCO2 showing a flat line. A quick and gentle laryngoscopy was done at 1 min following administration of succinylcholine and trachea was intubated with 7-8 mm ID cuffed endotracheal tube, which was kept open to atmosphere without administering positive pressure ventilation.
Vecuronium 0.1 mg/kg and midazolam 0.05 mg/kg were given IV to prevent the patients from regaining spontaneous respiration and development of awareness respectively. Correct endotracheal tube placement was confirmed using a fiberoptic bronchoscope. SpO2, heart rate (HR), systolic BP (SBP), diastolic BP (DBP) and mean arterial pressures (MAP) were closely monitored. The time at which saturation reached the study end point of 90% was noted, and the patients were immediately bag ventilated with 100% O2. The point of maximum desaturation was also noted, and bag ventilation was continued till saturation became 98-100%. Then, anesthetic gases were added, and patients were put on a ventilator.
Arterial blood gas samples were taken before induction while patients were breathing room air (baseline), immediately after preoxygenation and also at 90% desaturation to note PaO2, PaCO2 and pH. At these three points of time SpO2, HR, SBP, DBP and MAP were also documented. During the study period if there was tachycardia (HR >100/min) or hypertension (SBP >160 mmHg), plane of anesthesia was deepened with propofol 30 mg bolus IV. In the case of sustained tachycardia, hypertension or development of arrhythmias, even with saturation >90%, patients were immediately ventilated and excluded from the statistical analysis.
Results
To test the statistical significance of the difference in mean values between the two groups Student's t-test was applied. As the difference of mean values at basal level was statistically significant for PaCO2, for this variable, the two groups were compared for statistical significance with difference in the percentage change.
Distribution of age, sex, weight and height were comparable in both groups [Table 1]. Comparison of SpO2 at baseline, after preoxygenation and at maximum desaturation did not show any significant difference between groups [Table 2]. Similar observations were made when SBP, DBP, MAP and HR were compared [Tables 3 and 4].
Table 1.
Comparison of demographics
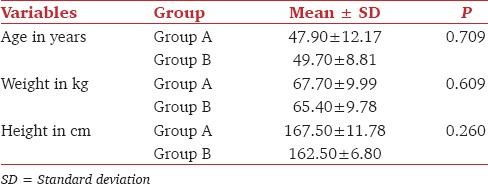
Table 2.
Comparison of SpO2
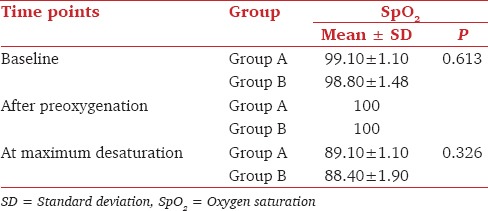
Table 3.
Comparison of SBP, DBP and MAP (mmHg)
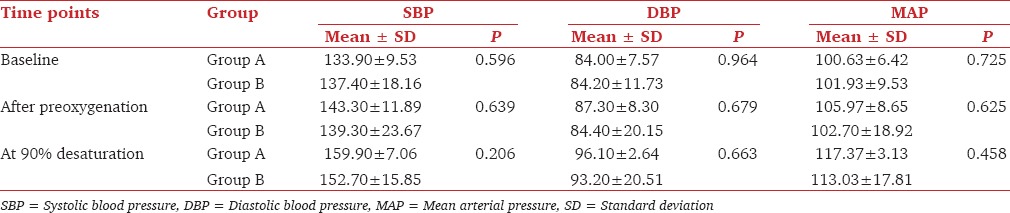
Table 4.
Comparison of HR, PaO2 and pH
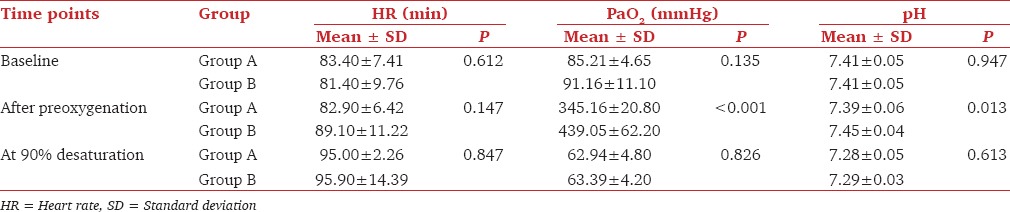
Comparison of baseline PaO2 among groups was comparable. However after preoxygenation Group B had a significantly high PaO2 value than Group A (439.05 ± 62.20 vs. 345.16 ± 20.80, P < 0.001), but at 90% desaturation there was no significant difference between groups [Table 4]. Baseline pH in both groups was comparable, but after preoxygenation Group B had a significantly high pH as compared to Group A (7.39 ± 0.06 vs. 7.45 ± 0.04, P = 0.013). The pH at 90% desaturation was comparable in both groups [Table 4].
Comparison of PaCO2 at baseline showed a significant difference between groups with Group A having a higher value (40.31 ± 3.40 vs. 36.82 ± 3.80, P = 0.044)). So percentage changes of PaCO2 from the baseline value were calculated for comparing PaCO2 after preoxygenation. There was no significant difference between groups after preoxygenation and also at 90% desaturation [Table 5 and Figure 1]. Statistical analysis had shown that there was a significant difference between groups when time to desaturate to 90% was compared. Group B showed a significantly high apnea induced desaturation time when compared to Group A (6.87 ± 1.78 vs. 3.47 ± 0.38 min) [Table 6 and Figure 2].
Table 5.
Comparison of changes in PaCO2
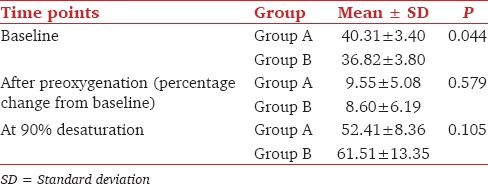
Figure 1.
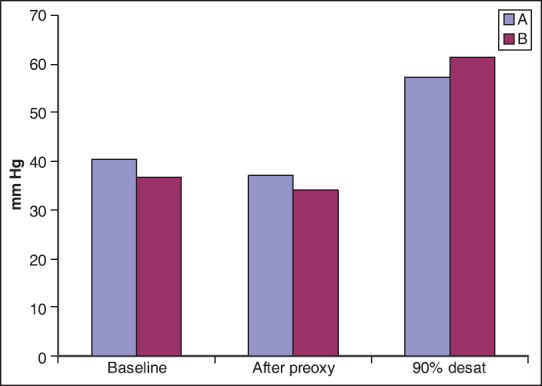
Changes in PaCO2
Table 6.
Time (in min) to desaturate to 90%
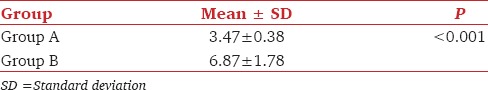
Figure 2.
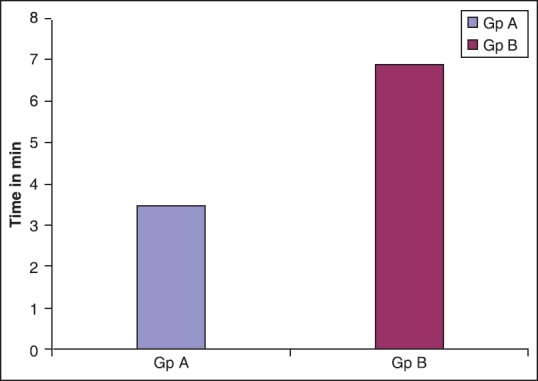
Time to desaturate to 90%
Discussion
The importance of preoxygenation in the safe conduct of GA is well established. Preoxygenation works by denitrogenation of the functional residual capacity, leading to an increase in oxygen stores which delays arterial desaturation during the apneic period.
During TVB there exists underventilated areas in the lungs which contain high concentrations of nitrogen. But with VCB these areas will also get ventilated with 100% O2 leading to an increased reserve.[4] This explains why oxygenation is better following deep breaths. Though patients are usually preoxygenated with the commonly used anesthesia systems, circle absorber system was also found to be equally effective.[5]
To achieve maximal preoxygenation alveolar, vascular (arterial and venous), and tissue compartments should be saturated with oxygen.[2,6] Failure to breathe a high inspired concentration of O2[5] or leak under the mask will affect the alveolar oxygenation. This is important as the effectiveness of preoxygenation depends greatly on tight face mask fit which may not be a very pleasant experience for a fully conscious patient. So reducing the tight face mask holding time with VCB technique for preoxygenation will improve patient comfort and acceptability.
Another concern is the duration of preoxygenation. The alveolar oxygenation will not be maximally effective if there is inadequate time for preoxygenation.[2,7] TVB for 3-5 min was found to be effective in attaining maximal preoxygenation compared to VCB for half a minute which resulted in suboptimal preoxygenation.[8] It was observed that 3 VCB produced significantly inferior, 4 and 5 VCB equally effective and 6 VCB superior preoxygenation as compared to TVB for 3 min. Therefore, 4 or more VCB was recommended as a reliable and rapid alternative to preoxygenation by 3 min of TVB.[4] Deep breathing yielded maximal preoxygenation when extended to 1.5 or 2 min, and only when high fresh gas flow (FGF) (10 l/min) was used.[8] Taking this into consideration, in our study, patients were asked to take 8 VCB in 1 min using O2 flow of 10 l/min. The different FGFs used in our study (10 vs. 5 l/min) can be further justified by the fact that, as tidal volume is one of the factors which decides FGF in different breathing circuits, if patient is taking VCB, to avoid rebreathing, higher flows will be required.
Previous studies have shown that 8 VCB preoxygenation in 1 min significantly delayed apnea-induced desaturation in comparison with TVB for 3 min.[3,9] Similar observation was made in our study also. This observation will be of importance whenever we anaesthetize a patient with a difficult airway where difficulty and/or delay in intubation or ventilation is anticipated. A prolonged apnea-induced desaturation time significantly improves patient safety in these cases. The duration of VCB for preoxygenation is also important. The safe upper time limit is said to be 2 min as, if extended for more than 2 min undesirable side-effects of hypocarbia will set in.[8]
Though few patients developed tachycardia and/or hypertension during the apneic period it could be controlled with propofol bolus.
Conclusion
Preoxygenation by 8 VCB in 1 min provides greater margin of safety, as it results in a significantly high arterial partial pressure of oxygen with an almost doubled apnea induced desaturation time, as compared to preoxygenation with TVB for 3 min.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Farmery AD, Roe PG. A model to describe the rate of oxyhaemoglobin desaturation during apnoea. Br J Anaesth. 1996;76:284–91. doi: 10.1093/bja/76.2.284. [DOI] [PubMed] [Google Scholar]
- 2.Benumof JL, Dagg R, Benumof R. Critical hemoglobin desaturation will occur before return to an unparalyzed state following 1 mg/kg intravenous succinylcholine. Anesthesiology. 1997;87:979–82. doi: 10.1097/00000542-199710000-00034. [DOI] [PubMed] [Google Scholar]
- 3.Singh B, Afzal L, Kaur B, Osahan NK. Comparison of pre oxygenation by maximal breathing and tidal volume breathing techniques. Indian J Anaesth. 2006;50:209–13. [Google Scholar]
- 4.Rooney MJ. Pre-oxygenation: A comparison of two techniques using a Bain system. Anaesthesia. 1994;49:629–32. [PubMed] [Google Scholar]
- 5.Nimmagadda U, Salem MR, Joseph NJ, Lopez G, Megally M, Lang DJ, et al. Efficacy of preoxygenation with tidal volume breathing. Comparison of breathing systems. Anesthesiology. 2000;93:693–8. doi: 10.1097/00000542-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Campbell IT, Beatty PC. Monitoring preoxygenation. Br J Anaesth. 1994;72:3–4. doi: 10.1093/bja/72.1.3. [DOI] [PubMed] [Google Scholar]
- 7.Berry CB, Myles PS. Preoxygenation in healthy volunteers: A graph of oxygen “washin” using end-tidal oxygraphy. Br J Anaesth. 1994;72:116–8. doi: 10.1093/bja/72.1.116. [DOI] [PubMed] [Google Scholar]
- 8.Nimmagadda U, Chiravuri SD, Salem MR, Joseph NJ, Wafai Y, Crystal GJ, et al. Preoxygenation with tidal volume and deep breathing techniques: The impact of duration of breathing and fresh gas flow. Anesth Analg. 2001;92:1337–41. doi: 10.1097/00000539-200105000-00049. [DOI] [PubMed] [Google Scholar]
- 9.Baraka AS, Taha SK, Aouad MT, El-Khatib MF, Kawkabani NI. Preoxygenation: Comparison of maximal breathing and tidal volume breathing techniques. Anesthesiology. 1999;91:612–6. doi: 10.1097/00000542-199909000-00009. [DOI] [PubMed] [Google Scholar]


