Abstract
Background and aims:
Laryngeal mask airway (LMA) insertion requires anesthesia and suppression of airway reflexes. In search of an optimal drug, we compared dexmedetomidine and fentanyl, in combination with propofol for insertion of LMA.
Material and Methods:
This study was a prospective double blind randomized study. Eighty patients of ASA class 1&2 were randomly divided into two groups of 40 each. Group D received dexmedetomidine 1 mcg/kg and group F received fentanyl 1 mcg/kg intravenously (IV) over 2 minutes. For induction, propofol 2mg/kg was given IV and 90 seconds later LMA was inserted. We observed apnea time, heart rate, respiratory rate, non invasive blood pressure and oxygen saturation before induction, 30 seconds after induction, 1, 3, 5, 10 and 15 minutes after insertion of LMA. Patient's response to LMA insertion like coughing, gagging or any movement were noted and scored. Statistical analysis of data was done using student t test for parametric data, Chi-square test for non parametric data and SPSS 15.0 for windows software.
Results:
37 (92.5%) patients of group D and 35 (87.5%) patients of group F had LMA insertion score of <2 and 5 (12.5%) patients of group F had score >2. Adverse events to insertion of LMA and hemodynamic variables were comparable in both the groups. Number of patients developing apnoea was larger and apnoea times were longer in group F compared to group D. When compared to group F, group D showed an increased respiratory rate.
Conclusion:
Dexmedetomidine can be a comparable alternative to fentanyl as an adjuvant to propofol for providing optimum insertion conditions for LMA and preservation of respiration.
Keywords: Dexmedetomidine, propofol, fentanyl, laryngeal mask airway
Introduction
Airway management is one of the important skills and inability to secure the airway, can cause catastrophic results.[1] The laryngeal mask airway (LMA) is a device, which allows both spontaneous, as well as positive pressure ventilation. Intravenous agents (IV) especially propofol is preferred for insertion of LMA.[2] As propofol lacks analgesic property, opioids are added but, they failed to prevent laryngospasm in spite of normocapnia and dose-dependent depression of airway reflexes.[3]
Dexmedetomidine is a pharmacologically active dextro isomer of medetomidine, which displays specific and selective α2 adrenoceptor agonism. It has both anesthetic and analgesic effects in addition to its sedative effects at doses of 0.5-2 mcg/kg IV. Dexmedetomidine also causes a reduction in doses of propofol both during induction and maintenance.[2,4,5,6,7]
In this study, we compared dexmedetomidine and fentanyl, in combination with propofol for insertion of LMA.
Material and Methods
After obtaining institutional ethical committee approval and with informed consent of all patients, a prospective randomized double-blind study was conducted on 80 patients of American Society of Anesthesiologists (ASA) physical status 1 and 2. The study period lasted 10 months. We included patients of the age group 18-60 years, weighing between 30 and 80 kg, undergoing various elective minor surgical procedures under general anesthesia. Patients with risk of aspiration, smokers, undergoing oral surgeries, weighing more than 80 kg and ASA physical status 3 and 4 were excluded from the study. Informed consent was taken and patients were randomly assigned using computerized randomization table into two groups of 40 each. Group D or dexmedetomidine-propofol group received injection dexmedetomidine 1 mcg/kg IV over 2 min. In Group F or fentanyl-propofol group, the patients were given fentanyl 1 mcg/kg over 2 min. In both the groups, 30 s later, propofol 2 mg/kg was given over 30 s for induction without any neuromuscular blocking agents. Ninety seconds after the propofol injection, LMA was inserted by an anesthesiologist who was blinded to the choice of induction and adjuvant anesthetic agents. The correct LMA placement was confirmed with expansion of the chest wall with bag compression with slight outward movement of the tube with LMA cuff inflation. LMA insertion conditions were evaluated by the same anesthesiologist. From the induction to insertion of LMA, patients were given oxygen via mask and ventilated if apneic. If any movement occurred before LMA insertion or after, propofol 0.5 mg/kg was administered, and we waited for 30 s before next attempt at LMA placement. Heart rate (HR) <45 was considered as bradycardia and treated with atropine 0.01 mg/kg.
Parameters observed were, apnea time — the time from last spontaneous breath after propofol administration to first spontaneous breath, HR, respiratory rate (RR), noninvasive blood pressure and oxygen saturation. These were recorded before induction, that is, baseline, 30 s after induction, 1, 3, 5, 10 and 15 min after insertion of LMA. Patient's response to LMA insertion such as coughing, gagging or any movement were noted and scored according to the scoring system modified by Muzi et al.[8] Jaw mobility was graded as: 1-fully relaxed, 2-mild resistance, 3-tight but, opens, 4-close. Coughing/movement were graded as: 1-none, 2-one or two coughs, 3-three or more coughs, 4-bucking/movement. Other events such as spontaneous ventilation, breath holding, expiratory stridor and lacrimation were noted. In each category, scores ≤2 were considered optimum for LMA insertion.
The sample size was calculated using Statistical Package Software Statistical Analysis System software (Creative Research Systems) with an alpha error of 0.05, confidence of 95% for an infinite population. The calculated power of the study was 88%. Statistical analysis of data was performed using the Student t-test (z-test) for parametric data, and nonparametric data was analyzed using Chi-square test. Analysis was performed using Statistical Product for Social Sciences (SPSS) software. P< 0.05 was considered statistically significant.
Results
The two groups were similar in terms of distribution of age; sex and weight [Table 1]. Insertion conditions with respect to jaw mobility, were appropriate in all patients of Group D. In Group F, 39 patients had relaxed jaw and 1 patient had tight jaw, for which additional propofol 0.5 mg/kg was supplemented, and the second attempt after 30 s to insert LMA was successful. With respect to coughing/movement, in Group D, 3 (7.5%) patients had scored more than 2. In Group F 4 (10%) patients had scores more than 2. All these patients were supplemented with additional propofol 0.5 mg/kg and the second attempt of insertion of LMA was well tolerated [Table 2].
Table 1.
Demographic distribution of patients
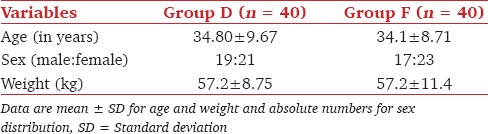
Table 2.
Observed parameters for LMA insertion conditions[8]
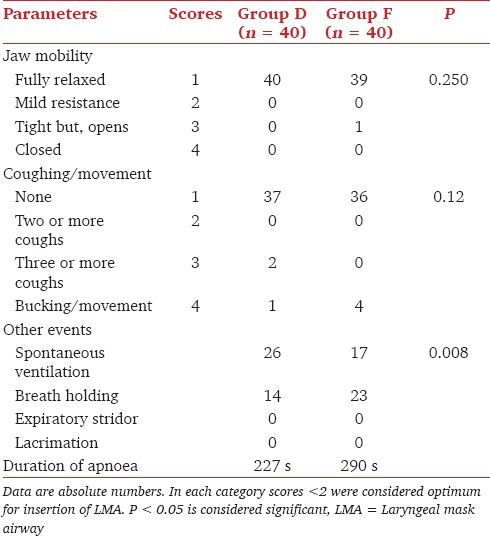
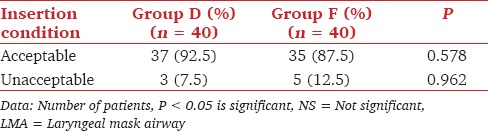
Summating the scores for insertion of LMA, 37 (92.5%) patients of Group D and 35 (87.5%) patients of Group F had score of <2 thus showing the acceptable conditions for insertion of LMA and 5 (12.5%) patients of Group F had score >2. The patient, who had closed jaw, was different from the four patients who had bucking/movement. All these five patients received additional propofol 0.5 mg/kg, and the second attempt of insertion of LMA was well-tolerated. The overall incidences of adverse events were comparable and statistically insignificant in both the groups [Table 3].
Table 3.
Distribution of patients according to insertion conditions of LMA
When compared with basal values there was a statistically significant and comparable fall in the mean pulse rate, throughout the study in both the groups. The maximum decrease of about 12% occurred at the 15th min.
The mean basal RR were comparable (P > 0.05) in both the groups [Figure 1]. There was statistically significant (P < 0.001) increase in the RR in Group D from 5 min onwards after insertion of LMA which got stabilized at 22/min by 15 min. In Group F there was no increase in the RR further, which got stabilized at 12/min by 15 min after the insertion of LMA. The duration of apnea was longer in Group F (290 s) than in Group D (227 s).
Figure 1.
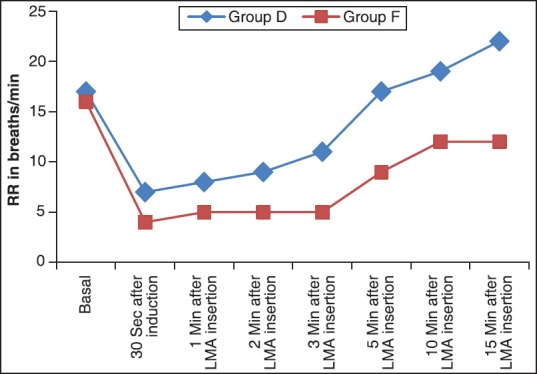
Changes in respiratory rate
Discussion
Smooth insertion of LMA needs sufficient depth of anesthesia to suppress the airway reflexes and relax the jaw muscles.[9]
Previous studies have found that, propofol is superior to thiopentone as an induction agent for insertion of LMA. However, when used alone, propofol provides less satisfactory conditions for LMA insertion and causes cardiorespiratory depression.[10,11] In order to decrease the adverse events of propofol, opioids or muscle relaxants were added. Muscle relaxants were found to increase the risk of aspiration whereas opioids increased the incidence and duration of apnea.[2]
Dexmedetomidine, a highly selective α2 adrenoceptor agonist, was shown to have sedative and analgesic properties. Insertion of LMA requires sufficient sedation and dry airway. We have used IV glycopyrrolate as an antisialogogue, which aids insertion by causing the drying of airway.[2]
In accordance with the studies by Belleville et al. and Uzümcügil et al.,[2,5,12,13] dose of dexmedetomidine used for intraoperative sedation, was 1 μg/kg given over 2 min. The intention was both to achieve rapid sedation and avoid alpha-1 side-effect such as hypertension and tachycardia. The obstructive respiration pattern and irregular breathing seen with such doses are probably related to deep sedation as well as anatomical features of the patient, and this could be overcome by insertion of an oral airway.[12] We did not encounter this problem to a major extent as our study was centered on insertion conditions of LMA.
Previous studies showed that anesthesia with propofol alone does not greatly suppress the airway reflexes, and incremental doses of fentanyl depress the airway reflexes in a dose-related manner.[4,14]
Heart rate does not change significantly after an induction dose of propofol. Propofol either may reset or inhibit the baroreflex, reducing the tachycardic response to hypotension. On the contrary, dexmedetomidine causes decrease in the HR by 27% after induction and returns to normal by 15th min.[15]
Our study has shown mild reduction (maximum of 12%) in HR in both the groups.[10] This might probably be because insertion of a bulky device like LMA could have caused some sympathetic response negating the effects of dexmedetomidine (bradycardia) on HR.
Supporting the study by Uzümcüügil et al.,[2] our study showed that the numbers of patients developing apnea were more in Group F (23) than in Group D (14). Breath holding/apnea was more in Group F and spontaneous ventilation was more in Group D indicating that respiration was better preserved in the dexmedetomidine group.
In support of the study conducted by Goh et al.,[16] the duration of apnea was longer in Group F (290 s) than in Group D (227 s). This might be because of potentiation of the depressant effect of propofol by fentanyl on respiration. The apnea developed in patients of Group D (14) was probably because of the depressant effect of propofol. However, as the respiratory depressant effect of propofol was not potentiated by dexmedetomidine the apnea times were significantly shorter.[16]
Our study, as expected shows increase in RR in dexmedetomidine group compared to fentanyl group. Previous studies have demonstrated increase in RR and decreased episodes of apnea with dexmedetomidine infusions.[14,17] Few studies have also shown that hypercapnic arousal phenomenon was not affected by dexmedetomidine, thus its sedation mimicking the natural sleep. As would be expected, the respiratory effects of dexmedetomidine is because, one of its sites of action is the locus caeruleus, which is known to play a role in both respiratory control and sleep modulation, and dexmedetomidine converges on the natural sleep pathway to exert its sedative effects, whereas natural sleep does result in ventilation modulation.[13,18]
Dexmedetomidine is unique among sedatives as it is clinically safe from a respiratory point of view, even during doses high enough to cause unresponsiveness to vigorous stimulation and exhibiting hypercarbic arousal phenomenon similar to the ones described during natural sleep.[18]
Our study has some limitations such as it has not included control group that is, propofol alone for insertion of LMA, as it would be unethical because the propofol was reported several times, to be inadequate for LMA insertion when used alone and the increase in dose to make it adequate were reported to be unsafe for hemodynamics and respiration.[4,11] We have not used any inhalational agents from induction till insertion of LMA, as it may affect the LMA tolerance and underestimate the drug effects as well as its requirements. Study was on single dose of dexmedetomidine for insertion of LMA, and we have not included the study concerned with its analgesic effects. Studies regarding different doses of the drug and its analgesia as IV injection and infusion may be needed further in the future. Pain, recovery and sedation scale were not included anywhere in the study as a present study was designed on insertion conditions for LMA.
Conclusion
We hereby conclude that dexmedetomidine is a comparable alternative to fentanyl as an adjuvant when co-administered with propofol for insertion of LMA. Both of the drugs provide stable hemodynamic profile but, dexmedetomidine is superior to fentanyl in preserving respiration.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sood J. Laryngeal mask airway and its variants. Indian J Anaesth. 2005;49:275–80. [Google Scholar]
- 2.Uzümcügil F, Canbay O, Celebi N, Karagoz AH, Ozgen S. Comparison of dexmedetomidine-propofol vs. fentanyl-propofol for laryngeal mask insertion. Eur J Anaesthesiol. 2008;25:675–80. doi: 10.1017/S0265021508004213. [DOI] [PubMed] [Google Scholar]
- 3.Kodaka M, Okamoto Y, Handa F, Kawasaki J, Miyao H. Relation between fentanyl dose and predicted EC50 of propofol for laryngeal mask insertion. Br J Anaesth. 2004;92:238–41. doi: 10.1093/bja/aeh033. [DOI] [PubMed] [Google Scholar]
- 4.Tagaito Y, Isono S, Nishino T. Upper airway reflexes during a combination of propofol and fentanyl anesthesia. Anesthesiology. 1998;88:1459–66. doi: 10.1097/00000542-199806000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Eren G, Cukurova Z, Demir G, Hergunsel O, Kozanhan B, Emir NS. Comparison of dexmedetomidine and three different doses of midazolam in preoperative sedation. J Anaesthesiol Clin Pharmacol. 2011;27:367–72. doi: 10.4103/0970-9185.83684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel CR, Engineer SR, Shah BJ, Madhu S. The effect of dexmedetomidine continuous infusion as an adjuvant to general anesthesia on sevoflurane requirements: A study based on entropy analysis. J Anaesthesiol Clin Pharmacol. 2013;29:318–22. doi: 10.4103/0970-9185.117066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khanduja S, Ohri A, Panwar M. Dexmedetomidine decreases requirement of thiopentone sodium and pentazocine followed with improved recovery in patients undergoing laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol. 2014;30:208–12. doi: 10.4103/0970-9185.130022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muzi M, Robinson BJ, Ebert TJ, O’Brien TJ. Induction of anesthesia and tracheal intubation with sevoflurane in adults. Anesthesiology. 1996;85:536–43. doi: 10.1097/00000542-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Dutt A, Joad AK, Sharma M. Induction for classic laryngeal mask airway insertion: Does low-dose fentanyl work? J Anaesthesiol Clin Pharmacol. 2012;28:210–3. doi: 10.4103/0970-9185.94877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown GW, Patel N, Ellis FR. Comparison of propofol and thiopentone for laryngeal mask insertion. Anaesthesia. 1991;46:771–2. doi: 10.1111/j.1365-2044.1991.tb09776.x. [DOI] [PubMed] [Google Scholar]
- 11.Scanlon P, Carey M, Power M, Kirby F. Patient response to laryngeal mask insertion after induction of anaesthesia with propofol or thiopentone. Can J Anaesth. 1993;40:816–8. doi: 10.1007/BF03009250. [DOI] [PubMed] [Google Scholar]
- 12.Belleville JP, Ward DS, Bloor BC, Maze M. Effects of intravenous dexmedetomidine in humans. I. Sedation, ventilation, and metabolic rate. Anesthesiology. 1992;77:1125–33. doi: 10.1097/00000542-199212000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Parikh DA, Kolli SN, Karnik HS, Lele SS, Tendolkar BA. A prospective randomized double-blind study comparing dexmedetomidine vs. combination of midazolam-fentanyl for tympanoplasty surgery under monitored anesthesia care. J Anaesthesiol Clin Pharmacol. 2013;29:173–8. doi: 10.4103/0970-9185.111671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong CM, Critchley LA, Lee A, Khaw KS, Ngan Kee WD. Fentanyl dose-response curves when inserting the LMA Classic laryngeal mask airway. Anaesthesia. 2007;62:654–60. doi: 10.1111/j.1365-2044.2007.05057.x. [DOI] [PubMed] [Google Scholar]
- 15.Miller RD. 7th ed. Philadelphia: Churchil Livingstone Elsevier Publications; 2010. Anaesthetic pharmacology; intravenous anaesthetics. Miller's Anesthesia; pp. 719–68. [Google Scholar]
- 16.Goh PK, Chiu CL, Wang CY, Chan YK, Loo PL. Randomized double-blind comparison of ketamine-propofol, fentanyl-propofol and propofol-saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intensive Care. 2005;33:223–8. doi: 10.1177/0310057X0503300211. [DOI] [PubMed] [Google Scholar]
- 17.Bindu B, Pasupuleti S, Gowd UP, Gorre V, Murthy RR, Laxmi MB. A double blind, randomized, controlled trial to study the effect of dexmedetomidine on hemodynamic and recovery responses during tracheal extubation. J Anaesthesiol Clin Pharmacol. 2013;29:162–7. doi: 10.4103/0970-9185.111665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu YW, Cortinez LI, Robertson KM, Keifer JC, Sum-Ping ST, Moretti EW, et al. Dexmedetomidine pharmacodynamics: Part I: Crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology. 2004;101:1066–76. doi: 10.1097/00000542-200411000-00005. [DOI] [PubMed] [Google Scholar]


