Abstract
Background and Aims:
Minimal consumption of local anesthetic and opioid for epidural labor analgesia has been advocated for safe obstetric outcome and superior maternal satisfaction. The primary objective of this study was to evaluate and compare the analgesic efficacy of mode of administration of epidural 0.1% ropivacaine with 0.0002% fentanyl via continuous infusion or intermittent boluses during labor.
Material and Methods:
Sixty term primi or second gravida healthy parturients in labor requesting epidural analgesia were recruited in this study. Lumbar epidural catheter was inserted, and analgesia initiated with 0.2% ropivacaine. Patients were randomized to receive ropivacaine 0.1% with fentanyl 0.0002% via either continuous infusion (Group A) or intermittent boluses (Group B) on an hourly basis. If the parturient complained of pain and visual analog scale (VAS) score was >3, an additional bolus of the study drug was given. VAS score, motor blockade, maternal hemodynamics and fetal heart sounds were frequently monitored. Side effects, mode of delivery and neonatal outcome were noted.
Results:
To achieve similar VAS, the mean total dose of ropivacaine was 18.78 ± 3.88 mg in Group A and 16.86 ± 4.3 mg in Group B, the difference being statistically significant (P = 0.04). Seventeen out of 30 patients in Group A that is, 56.6% and nine patients in Group B that is, 30% required additional top-ups, and this was significantly higher (P = 0.037). Side effects, mode of delivery and neonatal outcome were comparable in both groups.
Conclusion:
Intermittent bolus administration provides a more efficacious route of drug delivery when compared to continuous infusion by significantly decreasing the total amount of local anesthetic plus opioid without adversely affecting patient safety or maternal satisfaction.
Keywords: Analgesia, epidural, local anesthetics, ropivacaine
Introduction
Most of the Indian parturients still suffer from agony of labor pains due to lack of awareness.[1] Enhanced patient safety and satisfaction have contributed to growing use of epidural labor analgesia.[2] Reduction in total dose of local anesthetic and thus motor blockade is crucial to improve the obstetric outcome.[3,4,5] Studies that compare the modes of epidural drug delivery during labor from the Indian clinical scenario are lacking. We hypothesized that regular bolus of low concentration local anesthetic (0.1% ropivacaine) plus opioid (0.0002%) via the intermittent bolus technique would offer safe and superior quality labor analgesia by reducing total amount of the drug combination. We designed a study to compare the intermittent bolus administration of 0.1% ropivacaine with 0.0002% fentanyl to continuous infusion during labor. The primary outcome was to evaluate the analgesic efficacy of both routes of epidural drug delivery in terms of visual analogue scale (VAS) score, total drug dose and incidence of pain that required top-up administration (breakthrough pain). The secondary outcomes were to measure the degree of motor blockade, neonatal and obstetric outcomes.
Material and Methods
This prospective randomized clinical trial was carried out from July 2009 to December 2011 after obtaining Institutional Ethics Committee approval. Sixty-two healthy term primi or second gravid parturients aged 18-30 years with a singleton, live fetus in vertex presentation when in active stage of labor with cervical dilation of 3-5 cm were recruited in this study after they requested epidural for pain relief. Two patients were eliminated from the study, first due to complete motor blockade after test dose and second due to inadvertent intrathecal puncture. We excluded patients having preeclampsia, preterm labor, previous lower section cesarean section, multiple pregnancy, abnormal lie or placenta praevia and those with associated medical history like morbid obesity, bleeding disorders/anticoagulation therapy, severe anemia or any psychiatric or neurologic disorder.
Patients were explained about the procedure and written informed consent was obtained. They were made familiar with 10 point VAS shown on a scale where zero represents no pain, and 10 represents “worst imaginable pain”. An intravenous access was secured, and 500 mL of ringer lactate solution was started to preload. Under strict aseptic precautions, lumbar epidural space was located by the loss of resistance technique at L3–L4 or L2–L3 interspinous space with 18 G Tuohy's needle in left lateral position. With the bevel directed cephalad, a 20 G multiorifice epidural catheter (Perifix, B’Braun) was inserted through the epidural needle, advanced further till 5 cm within the epidural space and secured in place. The patient was positioned supine with a pillow under her right buttock to provide left uterine displacement.
A test dose of 3 mL of 2% lignocaine with 1:200,000 adrenaline was administered through the epidural catheter. After 5-10 min of administration of the test dose, each patient received 5 mL of 0.2% ropivacaine in incremental doses till bilateral T10 sensory level or adequate pain relief was achieved, whichever being earlier. This time was defined as T0 or Timezero. The parturients were then randomly assigned by sealed envelope method to one of the two groups to receive the drug combination of 0.1% ropivacaine with 2 μg/mL of fentanyl. Study drug solution was formulated by an anesthesiologist not directly involved in the patient's care or data collection. 50 mL solution was prepared by aspirating 24 mL of 0.2% ropivacaine, diluting with 24 mL of normal saline; and then adding 2 mL that is, 100 μg of fentanyl. Patient's baseline heart rate, blood pressure, respiratory rate and VAS scores were noted.
Patients in Group A received a continuous infusion of the study drug at 10 mL/h via infusion pump (InjectomatAgilia, Fresenius Kabi, USA) started immediately after attainment of T0. Parturients in Group B received 10 mL of the drug manually on an hourly basis by intermittent bolus technique; first dose being given 1 h after time zero. The attending anesthesiologist was informed whenever pain recurred (breakthrough painie, VAS ≥3) and additional top-ups of the study drug were given in 3-5 mL titrated doses. Parturient's vitals, VAS score, sensory level by absence of sensation to pin prick and motor blockade by Bromage scale were recorded every 15 min till the next 1 h and then on ½ h basis till delivery. All baseline and outcome data were gathered by the attending anesthesiologist who was blinded to the participant study group allocation.
When crowning of the fetal head was seen, parturients were made to lie in lithotomy position with the head up and a bolus of 5 mL of study drug was given epidurally. The study ended at the time of delivery or when it was decided to perform a cesarean section. Motor blockade was assessed by the modified Bromage scale as follows:[6]
No impairment,
Unable to raise extended leg but able to move knees and feet,
Unable to raise extended leg and to flex knees, able to move feet,
Unable to flex ankles, knees or feet (complete block).
Labor was managed according to the Obstetrics Department standard protocol. The mode of delivery was noted at the end.
Fetal heart sounds were monitored with a continuous Doppler machine, and fetal outcome was assessed by Apgar scores at 1 min and 5 min after delivery. The total dose of ropivacaine with fentanyl and the number of additional top-ups required was documented. The incidence of side effects such as nausea, vomiting, pruritus, urinary retention, etc. was recorded. On the next day of delivery, maternal satisfaction was assessed by asking the female to rate her analgesia on a scale of one to three as:
Excellent,
Satisfactory,
Poor and whether they will prefer to have similar analgesia in subsequent deliveries.
At the end of delivery, the epidural catheter was removed. If a cesarean section was performed, the catheter was removed 24 h after delivery.
Statistical analysis was performed using Statistical package of Social Sciences, version 12 (IBM, Business analytics software) and Microsoft Excel 2007 software. We considered the number of bolus doses required to maintain adequate analgesia as the primary outcome based on a previous study.[7] With 60% incidence in Group A and 20% incidence in Group B to allow an alpha error of 0.05 and beta error of 0.1 and power of study as 0.9, we calculated a sample size of 29/group to avoid getting a significant result by random probability. Data are expressed as mean ± standard deviation for continuous variables and no (%) for categorical variables. Continuous variables were compared using an independent t-test with two tail significance. Chi-square analysis was used for comparing nominal data. P < 0.05 was considered to be statistically significant.
Results
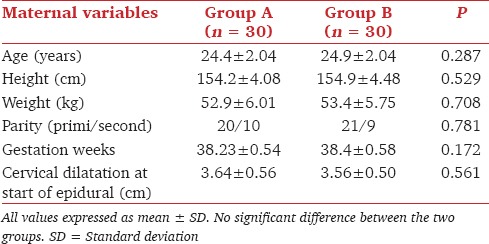
Both groups were comparable in terms of demographic data and obstetric parameters at the onset of labor as presented below Table 1.
Table 1.
Demographic data and obstetric parameters
Analgesia was scored on the VAS and analyzed starting from T0 as presented in Figure 1. At the time of insertion of the epidural catheter, all parturients had severe labor pain with median VAS of nine, interquartile range of 1.25 and range three for both groups. After about 30 min of the initial loading bolus, the median VAS was one, interquartile range was two for both groups while the range was three for Group A and two for Group B.
Figure 1.
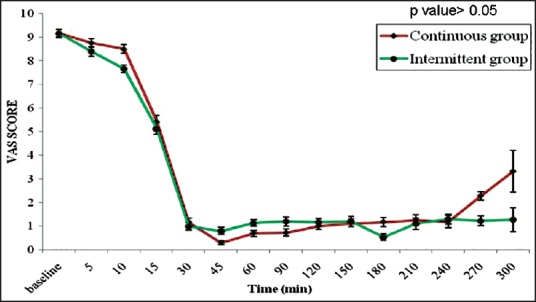
Median visual analog scale score. The figure shows median visual analog scale (VAS) scores against time for the two groups. No significant difference in VAS scores between the two groups at any time during labor (P > 0.05)
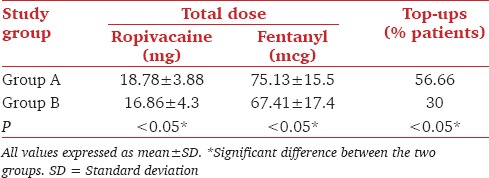
The total dose requirement of ropivacaine in Group A was 18.78 mg and 16.86 mg in Group B while that of fentanyl was 75.13 μg in Group A and 67.41 μg in Group B [Table 2]. To achieve similar VAS, this dose requirement was significantly higher in Group A (P = 0.04). 56.6% patients in Group A and 30% patients in Group B required additional top-ups, and this was significantly higher (P = 0.037).
Table 2.
Total dose and top-ups requirement
Majority of parturients did not develop any motor blockade represented as Bromage scale 0. Only 10% patients in Group A and 3.33% parturients in Group B developed a motor blockade of 1 on Bromage scale, and this difference was not statistically significant. There was no significant difference in the mode of delivery among the two groups. 66.67% of parturients in Group A and 73.3% patients in Group B underwent spontaneous vaginal delivery [Figure 2]. Two patients in Group A and one in Group B were taken up for cesarean section, one for borderline cephalopelvic disproportion (CPD) and other two for nonprogression of labor.
Figure 2.
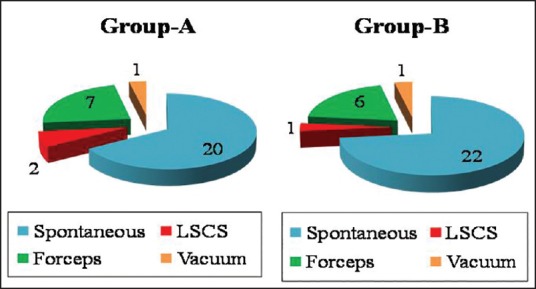
Distribution of mode of delivery. The pie chart illustrates the distribution of mode of delivery in both groups. No significant difference exists between the two groups (P > 0.05)
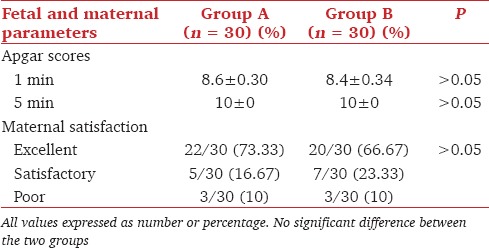
The intrapartum hemodynamics were comparable in both the groups and stable throughout the course of labor [Figure 3]. Only one patient in the continuous infusion group developed transient hypotension after the initial epidural bolus. The incidence of side-effects namely nausea, vomiting or pruritus, was minimal in both groups with no significant difference. Neonatal outcome in terms of Apgar scores at 1 min and 5 min was favorable in both groups without any significant difference. Majority of parturients rated their analgesia as excellent [Table 3].
Figure 3.
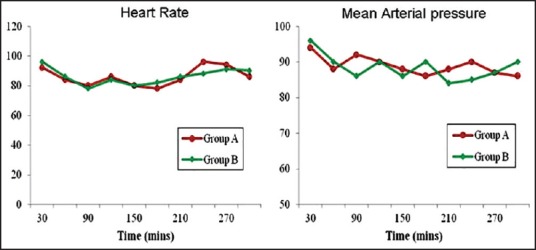
Intrapartum hemodynamics. Heart rate and mean arterial pressure plotted against time during labor. There is no significant difference between the two groups (P > 0.05)
Table 3.
Fetal outcome and maternal satisfaction
Discussion
Excessive patient load and a disproportionate doctor/patient ratio along with high equipment cost have made labor analgesia an unmet right of laboring women in developing countries.[8] Intermittent bolus administration of epidural local anesthetic has been shown to be more efficacious than continuous infusion for postoperative analgesia in surgical patients.[7]
Ropivacaine has a higher threshold than bupivacaine for causing cardiovascular toxicity.[9,10] Being less lipophilic, it causes lesser penetration of large myelinated nerve fibers, thus having a lesser propensity to cause motor blockade when used in lower concentration or dose.[6] Also, adding an opioid to the solution exhibits a local anesthetic sparing action by reducing the EC50 of ropivacaine in a dose-dependent manner.[10] Epidural ropivacaine and bupivacaine, with or without opioids have been found to be similar when compared at equal concentrations ranging from 0.125% to 0.25% for maintenance of labor analgesia.[11] Chhetty et al. found 0.2% ropivacaine with 2 μg/mL fentanyl more effective than 0.125% ropivacaine but recommended a comparison between intermittent bolus and continuous infusion technique to give a better estimation of local anesthetic plus opioid consumption.[12] We used 0.1% ropivacaine in a bid to further reduce the cumulative dose of local anesthetic and added 2 μg/mL fentanyl so as to provide adequate analgesia.[9,12]
Epidural infusions during labor are popular but at the cost of more numbness, motor blockade, and breakthrough top-ups.[13] Intermittent boluses given every 30-60 min have been shown to be more effective than continuous epidural infusion.[6,7,14]
Our most significant finding was a higher cumulative drug dose requirement in Group A than in Group B. We attribute it to a more uniform spread of drug in the intermittent group as compared to continuous group. The analgesic success of intermittent boluses may be related to the difference in dispersion of solutions in the epidural space.[15] When a large volume of drug is injected with a high injectate pressure; solutions tend to spread more evenly. This longitudinal and uniform spread of drug by the intermittent route leads to a more extensive blockade as compared to the limited, localized degree of blockade by the continuous infusion technique.
Lim et al. remarked that apart from the volume of injectate, the speed at which bolus is delivered and the pressure generated in the epidural space affects dispersion.[16] During continuous infusion of the drug under low pressure, the infusate discharges predominantly from the proximal hole of catheter with minimal flow from the distal hole. When injected as a bolus through a multiorifice epidural catheter, the solution exits the distal end of the epidural catheter.[17] This suggests that an epidural bolus through a multiorifice epidural catheter could result in wider sensory blockade compared with continuous infusion of the same volume, thereby improving the quality of analgesia.
Majority of the parturients did not develop any motor blockade as observed by us. The degree of motor blockade during epidural analgesia depends not only on the drug used but also on the cumulative dose of local anesthetic.[10] The mode of delivery is speculated to be affected by degree of motor blockade that in turn is affected by the choice, concentration and method of administration of local anesthetic agent. Motor blockade in lumbosacral region co-relates with lax pelvic floor muscles, which might delay the rotation of the fetal head and increase the need for assisted vaginal delivery. Also, loss of sensation in pelvis obtunds the Ferguson's reflex, thereby reducing oxytocin secretion, strength of maternal contractions and the maternal urge to bear down during the second stage of labor.
We found that the rate of instrumental delivery is high in our study without any associated significant motor blockade. The reasons cited for the application of forceps or vacuum were CPD, nonprogression of labor or signs suggestive of fetal distress and not related to motor blockade. Cochrane studies have concluded that the association of epidural with increased cesarean section and long-term backache remains only a myth.[13]
Assessment of the effects of local anesthetic and opioids on the fetus is always difficult and relies largely on evaluation of the newborn at delivery and over the ensuing hours by Apgar scores and umbilical cord acid-base status. Previous studies have shown that neonatal acid-base balance is improved by epidural analgesia compared to systemic or no analgesia.[18]
All parturients were hemodynamically stable throughout the course of labor and delivery under epidural analgesia. The initial hypotension was probably due to relative dehydration and increased venous capacitance caused by peripheral vasodilatation due to sympathetic blockade.
The incidence of side-effects like nausea, vomiting, pruritus was minimal in both the groups, mostly opioid related and treated symptomatically. Pregnant women seem to be more susceptible to dose-related pruritus after neuraxial opioid administration than other population with an incidence of 60-100%.[19] The quality of analgesia as rated by the parturients was excellent in both the groups.
The potential limitation of this study could be the need of a larger sample size to provide a broader perspective. Also inclusion of both primi and multigravidas into the sample population masks varying pain intensities.[20]
Conclusion
Both modes of epidural drug administration offer comparable analgesia during labor with favorable obstetric and neonatal outcome. However, we favor the intermittent group because it results in lesser total drug consumption and incidence of breakthrough pain thereby representing a more efficacious mode of epidural drug delivery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Shidhaye RV, Galande MV, Bangal VB, Joshi SS, Shidhaye UR. Awareness and attitude towards labour analgesia of Indian pregnant women. Anaesth Pain Intensive Care. 2012;16:131–6. [Google Scholar]
- 2.Salim R, Nachum Z, Moscovici R, Lavee M, Shalev E. Continuous compared with intermittent epidural infusion on progress of labor and patient satisfaction. Obstet Gynecol. 2005;106:301–6. doi: 10.1097/01.AOG.0000171109.53832.8d. [DOI] [PubMed] [Google Scholar]
- 3.Usha Kiran TS, Thakur MB, Bethel JA, Bhal PS, Collis RE. Comparison of continuous infusion versus midwife administered top-ups of epidural bupivacaine for labour analgesia: Effect on second stage of labour and mode of delivery. Int J Obstet Anesth. 2003;12:9–11. doi: 10.1016/s0959-289x(02)00158-9. [DOI] [PubMed] [Google Scholar]
- 4.Syal K, Dogra R, Ohri A, Chauhan G, Goel A. Epidural labour analgesia using Bupivacaine and Clonidine. J Anaesthesiol Clin Pharmacol. 2011;27:87–90. [PMC free article] [PubMed] [Google Scholar]
- 5.Sultan P, Murphy C, Halpern S, Carvalho B. The effect of low concentrations versus high concentrations of local anesthetics for labour analgesia on obstetric and anesthetic outcomes: A meta-analysis. Can J Anaesth. 2013;60:840–54. doi: 10.1007/s12630-013-9981-z. [DOI] [PubMed] [Google Scholar]
- 6.Chua SM, Sia AT. Automated intermittent epidural boluses improve analgesia induced by intrathecal fentanyl during labour. Can J Anaesth. 2004;51:581–5. doi: 10.1007/BF03018402. [DOI] [PubMed] [Google Scholar]
- 7.Fettes PD, Moore CS, Whiteside JB, McLeod GA, Wildsmith JA. Intermittent vs continuous administration of epidural ropivacaine with fentanyl for analgesia during labour. Br J Anaesth. 2006;97:359–64. doi: 10.1093/bja/ael157. [DOI] [PubMed] [Google Scholar]
- 8.Sharma S, Menia V, Bedi J, Dogra S. Labor analgesia: An unmet right of laboring women in India. J South Asian Fed Obstet Gynaecol. 2013;5:26–32. [Google Scholar]
- 9.Lee BB, Ngan Kee WD, Lau WM, Wong AS. Epidural infusions for labor analgesia: A comparison of 0.2% ropivacaine, 0.1% ropivacaine, and 0.1% ropivacaine with fentanyl. Reg Anesth Pain Med. 2002;27:31–6. doi: 10.1053/rapm.2002.27836. [DOI] [PubMed] [Google Scholar]
- 10.Fernández-Guisasola J, Serrano ML, Cobo B, Muñoz L, Plaza A, Trigo C, et al. A comparison of 0.0625% bupivacaine with fentanyl and 0.1% ropivacaine with fentanyl for continuous epidural labor analgesia. Anesth Analg. 2001;92:1261–5. doi: 10.1097/00000539-200105000-00034. [DOI] [PubMed] [Google Scholar]
- 11.Paddalwar S, Nagrale M, Chandak A, Shrivastava D, Papalkar J. A randomized, double-blind, controlled study comparing bupivacaine 0.125% and ropivacaine 0.125%, both with fentanyl 2 μg/ml, for labor epidural analgesia. Indian J Pain. 2013;27:147–53. [Google Scholar]
- 12.Chhetty YK, Naithani U, Gupta S, Bedi V, Agrawal I, Swain L. Epidural labor analgesia: A comparison of ropivacaine 0.125% versus 0.2% with fentanyl. J Obstet Anaesth Crit Care. 2013;3:16–22. [Google Scholar]
- 13.Pandya ST. Labour analgesia: Recent advances. Indian J Anaesth. 2010;54:400–8. doi: 10.4103/0019-5049.71033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lim Y, Sia AT, Ocampo C. Automated regular boluses for epidural analgesia: A comparison with continuous infusion. Int J Obstet Anesth. 2005;14:305–9. doi: 10.1016/j.ijoa.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Capogna G, Camorcia M, Stirparo S, Farcomeni A. Programmed intermittent epidural bolus versus continuous epidural infusion for labor analgesia: The effects on maternal motor function and labor outcome. A randomized double-blind study in nulliparous women. Anesth Analg. 2011;113:826–31. doi: 10.1213/ANE.0b013e31822827b8. [DOI] [PubMed] [Google Scholar]
- 16.Lim Y, Chakravarty S, Ocampo CE, Sia AT. Comparison of automated intermittent low volume bolus with continuous infusion for labour epidural analgesia. Anaesth Intensive Care. 2010;38:894–9. doi: 10.1177/0310057X1003800514. [DOI] [PubMed] [Google Scholar]
- 17.Wong CA, Ratliff JT, Sullivan JT, Scavone BM, Toledo P, McCarthy RJ. A randomized comparison of programmed intermittent epidural bolus with continuous epidural infusion for labor analgesia. Anesth Analg. 2006;102:904–9. doi: 10.1213/01.ane.0000197778.57615.1a. [DOI] [PubMed] [Google Scholar]
- 18.Reynolds F. The effects of maternal labour analgesia on the fetus. Best Pract Res Clin Obstet Gynaecol. 2010;24:289–302. doi: 10.1016/j.bpobgyn.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 19.Kumar K, Singh SI. Neuraxial opioid-induced pruritus: An update. J Anaesthesiol Clin Pharmacol. 2013;29:303–7. doi: 10.4103/0970-9185.117045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alehagen S, Wijma K, Wijma B. Fear during labor. Acta Obstet Gynecol Scand. 2001;80:315–20. doi: 10.1034/j.1600-0412.2001.080004315.x. [DOI] [PubMed] [Google Scholar]


