Abstract
Addiction to the illicit and prescribed use of opiate is an alarming public health issue. Studies on addictive disorders have demonstrated severe nutritional deficiencies in opiate abusers with behavioral, physiological and cognitive symptoms. Opiate addiction is also link with a significant number of diseases including Human Immunodeficiency Virus (HIV), Hepatitis C Virus (HCV) and other blood borne diseases generally stem from the use of needles to inject heroin. The use of medication assisted treatment for opioid addicts in combination with behavioural therapies has been considered as a highly effective treatment. Methadone is a long-lasting μ-opioid agonist and a pharmacological tool which attenuates withdrawal symptoms effectively replacement therapies. This review article aims to explain opiate addiction mechanisms, epidemiology and disease burden with emphasis on dietary and nutritional status of opiate dependent patients in methadone maintenance therapy.
Keywords: Opiate, Nutritional status, Methadone maintenance therapy
Introduction
Opiates such as heroin, morphine, and some other types are among the most extensively prescribed and efficient medications for the managing of chronic pain clinically. However, the consumption of these compounds due to the agile development and physical dependency has been so relentlessly troubled (1). Historically, addiction was perceived as disease of poor characteristics and was not systematically addressed by the medical and academic societies until 20th century. Drug abuse including opiates, methamphetamine, cannabis, and alcohol has already become a major public health problem (2, 3).
The extensive uptake of the morphine hypodermic syringes after 1805 by doctors to treat general symptoms caused converting many of their patients into drug abuse inadvertently (4–5). The intake of opiate and its dependence cause major health damage, including poor quality of life, increasing the risk of cancer, and many other damages (6–8). Major changes have been seen in past few decades about the culture and patterns of drug consumption, such as decreasing opioid injection or intravenous drug use and also prescription opioids have become more accessible, although, morbidity and mortality among opioid users are continuing by chronic infectious diseases such as HIV and premature death because of accidents and overdose (9–10).
Opiates have been well-known for their effects on human’s central nervous system, such as dizziness, relief, mental clouding, mood changes and loss of fine motor skills (11). Consequently, the frequent opiates consumption influence several neurotrans-mitter activity and neuropeptide systems in brain circuits which causes mood, behavior and other activities regulation. Some of activities including analgesia, species-regular behaviour, and reward are done by opioid receptors which are distributed across the brain and spinal cord. Researchers have shown three separated classes of opioid receptors, the kappa, delta, and mu, although it is likely that there are additional types. Opioids usually act independently of G proteins through calcium-dependent potassium channels contrary to the concept that opioids occasionally activate G proteins (12).
A dependence on opiates such as heroin or prescription painkillers is one of the most devastating addictions found in the treatment community. There are various types of opiate addiction treatment. The type of treatment that is most effective or which is safest for you will depend on various factors. One of the most effective treatments for opioid dependence is the use of Medication Assisted Treatment (MAT) with effective medications combined with behavioural therapies (13). One of the safest and efficient treatments of heroin abuse and dependence is Methadone for over forty years (14–15) as well as Buprenorphine which is authorised to use by licenced doctors (16). Similarly l-alpha-acetyl methanol (LAAM) and Naltrexone have also been used as a replacement therapies. Methadone meets most criteria for a pharmacological agent and long-term treatment of addiction which results in the normalization of many vital physiological processes that have been interrupted during opiates addiction (17). Metha-done treatment also effectively lowers blood-borne illnesses such as HIV infection and hepatitis C virus which in injecting drug users are common (18–19). However, extensive deviation and high level of mortality in this group which is caused by overdose, force government to set up the high regulated methadone maintenance treatment model (20). Advancement in scientific approaches has unveiled that there is a correlation between health and diet for various genders, ages and ecological conditions. The daily essential nutrients which are necessary for the human body to grow and maintain normal function of life are namely carbohydrates, fats, protein, vitamins, minerals, and water. Studies have reported poor diets with overweight and obesity among people in recovery from opiates addiction. In most of the opiate addicts, serious nutritional deficiencies of key proteins, fats, vitamins and minerals exist which disrupt their ability to digest carbohydrates efficiently. Physical and biochemical changes that occur from drug and alcohol use also cause nutritional deficiencies in opiate addicts (21–22).
Therefore, this review aimed to assess the effects and mechanisms of opiate addiction with an emphasis on the nutritional status of opiate dependence patients during methadone maintenance therapy.
Opiate
A group of pain killer drugs are opiates, which comes from the poppy plant. Opiates derived from opium are used as anodyne and hypnagogic. The natural opiates include opium, morphine, and codeine. There are also some man-made substances called opioids (23). Although the most commonly used term is opiate, however the term “opiate” is sometimes used for close relatives of opium such as codeine, morphine and heroin, while the term “opioid’ is used for the entire class of drugs including synthetic opiates such as oxycontin (24).
Disease burden of opiate addiction
The intake of opiates and their dependence cause significant damage to health, increase mortality and morbidity and make a poor quality of life (25–26). Psychoactive substances including illicit drugs constitute 8.9 % of total burden of diseases which is recorded by World Health Report in 2002 (27). Opiate overdose may cause experiencing confusion and physical distress and even slowing down the persons’ respiration so much that breathing stops in severe cases (28).
Despite its adverse effects on health, opiates consumption is continued by different means including swallowing, smoking, and drinking in all over the world such as Southeast Asian countries (29).
Epidemiology of opiate addiction
Opiate addiction is now becoming a worldwide problem as 13-22 million people are afflicted and Asia encompasses more than half of that. Addiction to the illegal and prescribed use of opiate is an alarming public health issue. Three out of ten percent to 0.5% of the world population (i.e. 21-35 million people) used opioids (30). The prevalence of opiate use, particularly in young adults after the 1980s has been similar in the United States and Europe. Indeed, in early 1990s the problematic opiate use in the US was two-fold of that in the Western Europe. However, in a limited number of European countries the prevalence is now close to that of the United States (31). Opiate abuse and accidental mortality is rising in the U.S. The Centre for Disease Control (CDC) has estimated that almost 74% of all version drug overdose mortalities in the U.S in 2008 occurred by consumption of opiate sedative drugs. Furthermore 22.6 million Americans aged 12 or older were illegitimate drug users reported from 2012 National Survey on Drug Use and Health. United Nations Office on Drugs and Crime (UNODC), in Canada, reported the use of prescription opioids over shadows the use of heroin (0.3% annual prevalence), while in Brazil and Chile the prevalence is 0.5% of the population. However, in South West and Central Asia, most of the countries i.e. Iran, Pakistan and Afghanistan, the prevalence of opiate use is higher than the world average. There is no data available on drug consumption of many regions of Africa, Middle East and some parts of Asia (32). In Malaysia, The National Anti-Drug Agency has recorded 3611 drug abusers in 2010 which has been increased 110% over one year for corresponding period (33). There have been extensive regional differences in the use and abuse patterns of opiates. Heroin is the most widely used illegal drug in the majority of Africa, Europe and Asia, while hydrocodone, codeine, hydro morphine, morphine, oxycodone and meperidine are the main opioids of abuse in the Americas and Oceania, Although in the last decade, it is reported an increase of prescription opioid abuse in some African and Asian countries. Americans consume almost 80% of the world opioid supply while America has only 5% of the world population (30).
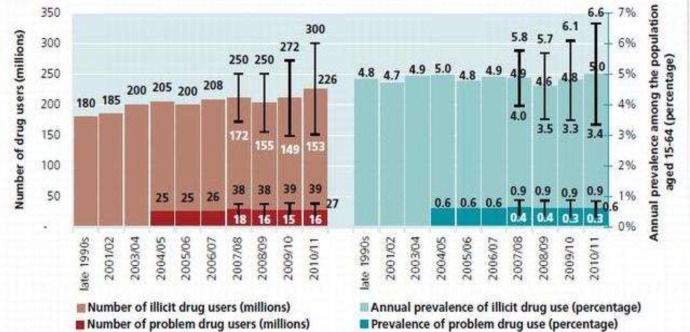
Fig. 1.
Illicit drug use at the global level, late 1990s-2010/11(Source: Estimates based on UNODC annual report questionnaire data)
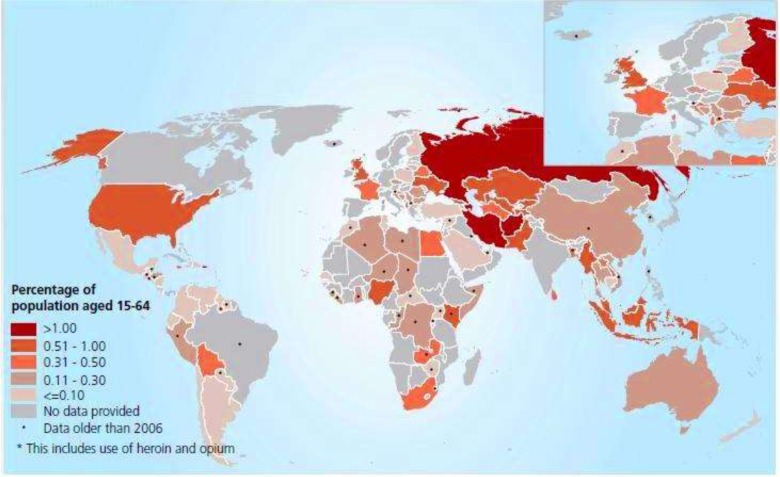
Map. 1.
Prevalence of the use of opiates in 2010 (or latest years with available data (Source: UNODC estimates based on annual report questionnaire data and other official sources)
Mechanism of opiate addiction
In 1992, a specific opiate receptor by two groups working independently simulated successfully that was a major breakthrough for the first time (34–35). This achievement was followed by the cloning of μ- and κ- opioid receptors of rodents and in humans opened new doors for both animal and basic clinical research studies, as well as molecular and human genetics studies (36–38). Opiates (39), show their effects by connecting to three opioid receptor types in the body (μ, δ, and κ) and imitating the actions of endogenous opioid peptides which are the endorphins, endomorphins, encephalin, and dynorphins. Opiates act mainly as μ-Opioid receptors (MOP-r), Increases dopamine level significantly in the synaptic clefts of body in case of the reward track. On these receptors, heroin and prescription opioids such as oxycodone and hydrocodone act partially with short period of operation, while cocaine- methamphetamine- act primarily to enhance synaptic dopamine by preventing of dopamine reuptake or an increased in emissions. A theory suggests that when the opiate attached to the opiate receptors on neurons, Gamma-amino butyric acid receptor (GABA) which is a neurotransmitter that inhibits dopamine will disperse less. This increment of dopamine causes feeling of extreme pleasure for the opiate addicts (40–41). Important advances have been made by humans on pathophysiology, as well as molecular and cellular neurobiology of opiate addiction over the last few decades. The ventral tegmental area (VTA) which is an important centre of DA activity is involved in opioid reward. A couple of studies on rats suggest that opioids in the VTA have a rewarding effect (42–43). Neurons were involved continuously in the valuable properties of opioids. Systematic administrations of opiates enhance dopamine turnover in the NA, which suggests that opioids increase dopamine activity (44). In 1992, DiChiara suggested that opioids, which reduce the inhibition on dopaminergic neurons projecting to the NA, hyper polarize GABA-interneurons in the VTA. Hence, increasing the amplification is associated with addiction. While this assumption is true, it has not been proven yet (39). Opiate usage damage on the psychomotor function in those who cannot quit the drug. Zacny and colleagues studied the intellectual, psychological and physiological effects of analgesics usually prescribed to weak patients who were previously healthy. Patients who cannot stop the drug and usually take prescribed amount of analgesics medications, experience subjective feelings a negative perception due to substance dependent incompatible withdrawing (45–47).
Effects on opiates on addicts
Opiates are initially central nervous system (CNS) depressant and analgesics. Opiate usage normally makes physical and psychological dependence. Opiates have been well-known for their effects on the central nervous system, such as dizziness, sedation, mental clouding, mood changes and loss of fine motor skills. In particular, performance may be impaired on cognitive tasks that require decision-making that involves balancing short-term rewards and long-term consequences (54–55). The opiate addict’s brain, takes months and even years to get hold of its normal functioning. During this time, these opiate addicts experience lack of motivation, extreme fatigue, depression and sensitivity to pain. General symptoms of opiates intoxication are slurred speech, drowsiness, pupillary constriction, decreased level of consci-ousness, hypotension, rhinorrhea, piloerection, nausea; vomiting, diarrhea, restlessness, respire-tory depression and hypothermia opiates induce tolerance. Following are few of the adverse effects if opiate use and misuse (56–57). Infectious side effects from opiate use are commonly caused by using a syringe to inject drugs, particularly heroin injection, that a significant number of HIV / AIDS and hepatitis cases have been reported. It is estimated that 60% to 90% of injection users are infected to hepatitis C virus (39–40), other infectious diseases, such as some of the common bacterial infections including Staphylococcus aurous and cellulitis, are transmitted by injections either (41). Metabolic problems and opiate abuse are unusual, but becomes more common as drug use rises. Metabolic problems often associated with heroin, cocaine, and ecstasy drug although there is a wide range of medical problems produced. The use of heroin has been implicated in blood sugar disorders in a number of mechanisms. Fasting insulin levels were found to be four times higher in heroin addicts than in control subjects and insulin resistance stemming from opioid use may be coupled with beta cell dysfunction. Acute insulin response in heroin addicts were found 42% lower than control subjects, accompanied by an 80% lower glucose disappearance rate, when they were given intravenous glucose (43–47). Opiate dependents do not usually have an ordinary life and they have many problems in their dietary and sleeping schedules. They usually ignore some of the basic requirements of life due to supply their daily usage of drugs. Hence, most of them become undernourished and impoverished. Moreover, they are more at risk of infectious diseases due to their drug abusing and lifestyle such as injection and risky sex behavior (48). The majority of substance dependent does not have an appropriate weight and their hormonal and immunological system usually remain imbalanced. In some cases a severe organ failure are observed among opiate dependents, like chronic liver failure (49).
Treatment options for opiate addicts
Opiate dependence has been treated by various approaches such as the use of Medication Assisted Treatment (MAT) in combination with behavioural therapies. Methadone, a schedule II opioid agonist and buprenorphine a schedule III partial opioid agonist are frequently employed as replacement therapies. Similarly l-alpha-acetyl methanol (LAAM) and Naltrexone have also been used as a replacement therapies. In the 1960’s, methadone gained appreciation as an effective treatment for heroin addicts. Methadone is a long-lasting μ-opi-oid agonist which assists patients in making the transition towards abstinence by mimicking some opiate actions (50). In 1999, almost 115,000 people who have been addicted to heroin participated in methadone maintenance therapy in the United
States (51). Methadone by itself is an opiate which causes depression of central nervous system. Methadone is a pharmacological that reduces the opiate craving as well as lessens withdrawal symptoms and if it coupled with counseling, enables to reach tolerance threshold although prevents from drowsiness and euphoria. Appropriate and safe daily dosage ranges from 20 to 30 mg in initial stages and average 60 to 100 mg at latter stages. Because of its long half-life of 24 to 36 hours, between 4 to 10 days is required to achieve a stable maintenance dosage (52–53). Several studies on methadone maintenance therapy have demonstrated conditions in which mortalities happened. Based on a cross sectional study most of the 238 patients who died in between 1990-1995 were drug users and suffered from medical illnesses. Almost 21% of the mortalities occurred in the first week of methadone treatment and 88% of these patients were polysubstance abusers. Only around 10% of deaths were related to the first week of MMT tested positive for methadone alone. In another study was reported 62 (71%) patients were involved illicit drug consumption from all 87 MMT patients ‘death. According to these studies, overdose during methadone maintenance therapy is related to polydrug use (54–56). Buprenorphine is a semi-synthetic opioid derivative and is a sectional μ-opioid agonist and κ-opioid antagonist which has less abuse potential than other opioids. Buprenorphine was initially proposed in 1978 for opioid addicts as an oral alternative opioid replacement therapy, because the intensity of the rewarding effect is milder at higher doses (57–59). Its use is promoted by the Substance Abuse and Mental Health Services Administration of the US Department of Health and Human Services (60). Buprenorphine acts on the same receptors as heroin and morphine, alleviating drug cravings without producing the same severe “high” or hazardous side effects. Due to wide metabolism in intestinal and liver tissues, buprenorphine has a very low oral bioavailability. Naltrexone and naloxone are the two most commonly used opioid (mu receptor) antagonists act centralized and subordinate, but have different pharmacokinetic indexes with different therapeutic uses.
The US Food and Drug Administration confirmed Naltrexone and naloxone for opioid dependence treatment because of their pharmacologic profile primarily. One of the pharmacologic profiles is antagonism at the μ-opioid receptors by Naltrexone and naloxone that block opioid effects (61). Naloxone often is not oral bioavailability, effects immediately for reversal of opioids. But Naltrexone is useful in detoxification and maintenance therapy by a long duration of action and it is used orally. (62–63). Naltrexone is also used in anesthesia-assisted detoxification, in which naloxone is administered under general anesthesia to speedup withdrawal. This technique is also known as ultra-rapid or rapid detoxification (63).
Dietary and nutritional status of opiate addicts in methadone maintenance treatment
The development of effective treatments for opiates addiction is a high priority in public health because addiction poses a significant burden on suffered individuals. Studies about addiction disorders have proven extreme nutritional deficiencies on drug abusers such as weight loss and dietary patterns changes. Changes in specific nutrient status can lead to develop barriers in withdrawal from opiates addiction (64–65). In opiate addicts there have been shown unhealthy eating behaviors due to lack of nutritional knowledge, food preparation skills, and environments (66–68). It is reported that a good nutrition education and physical activity are quite effective for substance abusers to their withdrawal from opiates (69). During withdrawal from heroin, nicotine, marijuana, and cocaine, weight gain or loss occurs which is caused by major changes in food intake selection. Nutrition is related with conditions and diseases, such as diabetes which decreases sensitivity to dependence on morphine and vitamin D deficiency that slows down morphine dependency as well as protein deprivation which generates preferential fat intake with low cocaine use (70). Nutritional status also plays important role in the process of recovery and survival of an individual, such as in HIV infection which endangers nutritional status till may produce malnutrition (71).
Several studies have concluded that there is a correlation between drug addiction, education, income levels, and body mass index; the higher the body mass index, the higher the income and educational levels and vice versa (72–73). In 2011, Alves et al. assessed nutritional and socio demographic characteristics of heroin addicts during detoxification program, and it was found that heroin addicts consume less than the minimum amount of vegetable, fruit and grains recommended by the food pyramid and are more eager to have sweets (74). Several other studies have also demonstrated that the consumption of vegetables and fruit in drug addicts are less than general population and they are more prone to consume food with low vitamin content. Unfortunately, the scope of nutrition services has not been defined well in detoxification programs and it has not been seen as a main problem. Larson et al.. asserts that because of the major deficiencies and absorption problems, proper eating behavior, is not the only solution to overcome the depletion of nutrients in the beginning of a detoxification program. Pantothenic acid administered orally is not absorbed by the alcoholic patients as it is found through urine test (75–77). Increasing the dietary intake of protein and reducing simple carbohydrates in the form of vegetables and whole grains can manage the carbohydrate-metabolism health problems (78). Therefore, to recover from opiates addiction, patients need to consume even more amino acids and protein during the treatment process (79–80). Methadone maintenance treatment, itself, is not a favorable approach until is coupled with proper diet due to negative role of vitamins and minerals deficiencies in withdrawal process. Williams found that high alcohol intake in rat resulted in vitamin B6, vitamin A, thiamine, riboflavin and pantothenic acid deficiencies (81). Despite proteins and key vitamins, as well as minerals such as zinc, iron, calcium, chromium, magnesium, potassium and other essential nutrients should be prescribed in detoxification programs to recovering addicts. Zinc can help to improve immune system and proper brain function (82). Many opiate and alcohol addicts have shown calcium and magnesium deficiencies due to poor diet and inadequate intake of calcium. Calcium and magnesium deficiencies are the major factors of pain and nervous/muscular disorders among addicts and alcohol consumers during detoxification programs (22).
Conclusion
Opiate addiction - as a major public health problem in all over the world- is rising globally. Opiate dependents have several deficiencies such as nutritional deficiencies and weight deficits. The most efficient recovering program is methadone maintenance therapy but it seems not to be the favorable approach unless be associated with consuming proper and diverse diet to overcome nutritional deficiencies further studies are required to assess the impact of other factors, such as different gender, food behavior, dietary intake, exercise, non-dietary determinants of nutritional status in the opioid-using population. An accurate and efficient nutritional intervention among drug addicts during detoxification could decrease their nutritional deficiencies and subsequently, boost up their productivity.
Ethical considerations
Ethical issues (Including plagiarism, Informed Consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgment
This work was funded by Postgraduate Research Grant project no: PG041-2012B from University of Malaya, Kuala Lumpur. The authors wish to thank Dr. Tahereh Seghatoleslam, Dr. Rusdi Bin Abd Rashid, and Dr. Abolfazl Ardakani for their kind cooperation. The first author is grateful of the University of Malaya for financial support by Postgraduate Research Grant fund during this study. The authors declare that there is no conflict of interests.
References
- Stockton SD, Devi LA (2012). Functional relevance of μ-δ opioid receptor heteromerization: a role in novel signaling and implications for the treatment of addiction disorders: from a symposium on new concepts in mu-opioid pharmacology. Drug Alcohol Depend, 121(3): 167–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habil MH, Said MA, Rashid RA, Sulaiman AH, Peters H, Zahari MMA, et al. (2010). Substance abuse violence behavior. Int J Addict Sci, 1–5. [Google Scholar]
- United Nations Office on Drugs and Crime (2010). World drug report. [Google Scholar]
- Courtwright DT (2001). A history of opiate addiction in America. Cambridge, MA: Harvard University Press; Available from: http://www.hawaii.edu/hivandaids/Dark Paradise. [Google Scholar]
- Hickman T (2004). The Double Meaning of Addiction. Habitual Narcotic Use and the Logic of Professionalizing Medical Authority in the United States, 1900–1920. In: Altering American Consciousness the History of Alcohol and Drug use in the United States, 1800–2000. Eds, Tracy SW, Acker CJ. Amherst and Boston University of Massachusetts Press; Pp. 182–202. [Google Scholar]
- Challier B, Chau N, Predine R, Choquet M, Legras B (2000). Associations of family environment and individual factors with tobacco, alcohol, and illicit drug use in adolescents. Eur J Epidemiol, 13: 33–42. [DOI] [PubMed] [Google Scholar]
- Torrens M, Domingo-Salvany A, Alonso J, Castillo C, Luís S (1999). Methadone and quality of life. Lancet, 13: 1101. [DOI] [PubMed] [Google Scholar]
- Virk S, Schwartz TL, Jindal S, Nihalani N, Jones N (2004). Psychiatric medication induced obesity: an aetiologic review. Obes Rev, 13: 167–170. [DOI] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Treacy S, Marsden J (2001). A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction, 97: 39–47. [DOI] [PubMed] [Google Scholar]
- McNeely J, Gourevitch MN, Shah S, Wright S, Heller D (2012). Estimating the prevalence of illicit opioid use in New York City using multiple data sources. BMC Public Health, 12(443): 1186–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vainio A, Ollila J, Matikainen E, Rosenberg P, Kalso E (1995). Driving ability in cancerpatients receiving long-term morphineanalgesia. Lancet, 346: 667–670. [DOI] [PubMed] [Google Scholar]
- Dhawan BN, Cesselin F, Raghubir R, Reisine T, Bradley PB, Portoghese PS, Hamon M (1996). International union of pharmacology classification of opioid receptors. Pharmac Rev, 48: 567–591. [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment (2005). Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. Treatment Improvement Protocol (TIP) Series 43. DHHS Publication No. (SMA) 12–4214. Rockville, MD: Substance Abuse and Mental Health Services Administration. [PubMed] [Google Scholar]
- Kreek MJ, Borg L, Ducat E, Ray B (2010). Pharmacotherapy in the treatment of addiction: Methadone. J Addict Dis, 29: 200–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banta-Green CJ, Maynard C, Koepsell TD, Wells EA, Donovan DM (2009). Retention in methadone maintenance drug treatment for prescription-type opioid primary users compared to heroin users. Addiction, 104: 775–783. [DOI] [PubMed] [Google Scholar]
- Cunningham C, Giovanniello A, Sacajiu G, Whitley S, Mund P, Beil R, Sohler N (2008). Buprenorphine Treatment in an Urban Community Health Center. NIHPA Author Manuscript, 40(7): 500–506. [PMC free article] [PubMed] [Google Scholar]
- Curran HV, Bolton J, Wanigaratne S, Smyth C (1999). Additional methadone increases craving for heroin: a double-blind, placebo-controlled study of chronic opiate users receiving metha-done substitution treatment. Addiction, 94(5): 665–674. [DOI] [PubMed] [Google Scholar]
- Caplehorn JRM, Ross MW (1995). Methadone maintenance and the likelihood of risky needle-sharing. Int J Addict, 30(6): 685–698. [DOI] [PubMed] [Google Scholar]
- Kwiatkowski CF, Booth RE (2001). Methadone maintenance as HIV risk reduction with street-recruited injecting drug users. J Acquir Immune Defic Syndr, 26(5): 483–489. [DOI] [PubMed] [Google Scholar]
- Rusdi AR, Masturah R, Robson N, Habil H (2011). Metha-done maintenance therapy (MMT): low versus high regulated model. Europ Psychiat, 26: 1–99. [Google Scholar]
- Lyle MH (2006). The Reclassification of Sugar as a Drug. Lethbridge Undergraduate Research Journal, 1(1): 1–5. [Google Scholar]
- Finnegan J, Gray D (1995). Recovery from Addiction. 1st ed. Berkeley, California. [Google Scholar]
- White WL (2007). Addiction recovery: Its definition and conceptual boundaries. J Subst Abuse Treat, 33(2007): 229–241. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse Research Report Series: Heroin Abuse and Addiction (1997). National Clearinghouse on Alcohol and Drug Information. [Google Scholar]
- Pawan M, Choudhary R, Mathur R, Choudhary MR, Kamla M (2011). Study on harmful effects of opium on liver and lungs in chronic opium addicts of western Rajasthan. J Bangladesh Soc Physiol, 13: 122–126. [Google Scholar]
- Galea S, Nandi A, Vlahov D (2004). The social epidemiology of substance use. Epidemiol Review, 13: 36–52. [DOI] [PubMed] [Google Scholar]
- Habil H, Huong AGW, Guan NC, Nordin ASA, Adlan ASA (2009). Quality of life assessment of opioid substance abusers on methadone maintenance therapy (MMT) in university Malaya medical centre. ASEAN J Psychiatr, 10 (1). [Google Scholar]
- Sadock BJ, Sadock VA (2008). Kaplan &Sadock's comprehensive textbook of psychiatry. 8th ed. Lippincott Williams & Wilkins. [Google Scholar]
- Suwanwela C, Poshyachinda V (1986). Drug abuse in Asia. Bull Narc, 13: 41–53. [PubMed] [Google Scholar]
- UNODC (2011), World Drug Report. United Nations Publication, New York: Available from:www.unodc.org/documents/data-and analysis/WDR-2011/World_Drug_Report_2011_ebook.pdf [Google Scholar]
- Hartnoll RL (1994). Opiates: prevalence and demographic factors. Addiction, 89(11): 1377–1383. [DOI] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime (2014). World Drug Report. [Google Scholar]
- Sulaiman AH, Said MA, Habil MH, Rusdi R, Siddiq A, Guan NC, et al. (2013). The risk and associated factors of methamphetamine psychosis in methamphetamine dependent patients in Malaysia. Comprehensive Psychiatr, 55(2014): 89–94. [DOI] [PubMed] [Google Scholar]
- Evans CJ, Keith DE, Morrison H, et al. (1992). cloning of a delta opioid receptor by functional expression. Science, 258: 1952–1955. [DOI] [PubMed] [Google Scholar]
- Kieffer BL, Befort K, Gaveriaux-Ruff C, et al. (1992). The delta-opioid receptor: isolation of a cDNA by expression cloning and pharmacological characterization. Proc Natl Acad Sci USA, 89: 12048–12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Mestek A, Liu J, et al. (1993). Molecular cloning and functional expression of a mu-opioid receptor from rat brain. Mol Pharmacol, 44: 8–12. [PubMed] [Google Scholar]
- Chen Y, Mestek A, Liu J, et al. (1993). Molecular cloning of a rat kappa opioid receptor reveals sequence similarities to the mu and delta opioid receptors. Biochem J, 295: 625–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JB, Imai Y, Eppler CM, et al. (1993). Mu opiate receptor: cDNA cloning and expression. Proc Natl Acad Sci USA, 90: 10230–10234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Chiara G, North RA (1992). Neurobiology of opiate abuse. Trends Pharmacol Sci, 13(5): 185–193. [DOI] [PubMed] [Google Scholar]
- Bruce RD, Altice FL (2007). Clinical care of the HIV-infected drug user. Infect Dis Clin North Am, 21(1): 174–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz RH (1998). Adolescent heroin use: a review. Pediatrics, 102: 1461–1466. [DOI] [PubMed] [Google Scholar]
- Welzl H, Kuhn G, Huston JP (1989). Self-administration of small amounts of morphine through glass micropipettes into the ventral tegmental area of the rat. Neuropharmac, 28: 1017–1023. [DOI] [PubMed] [Google Scholar]
- Phillips AC, LePiane EG (1980). Pharmacol. Biochem. Behav, 12: 965–968. [DOI] [PubMed] [Google Scholar]
- Westernik BH, Korf J (1976). Regional rat brain levels of dihydrophenylacetic acid and homovanillic acid: Concurrent fluoimetric measurement and influence of drugs. Eur J Pharmacol, 38: 281–291. [DOI] [PubMed] [Google Scholar]
- Zacny JP, Gutierrez S, Bolbolan SA (2005). Profiling the subjective, psychomotor, and physiological effects of a hydrocodone/acetaminophen product in recreational drug users. Drug Alcohol Depend, 78: 243–225. [DOI] [PubMed] [Google Scholar]
- Zacny JP, Gutierrez S (2003). Characterizing the subjective, psychomotor, and physiological effects of oral oxycodone in nondrug abusing volunteers. Psycho-pharmacol, 170: 242–254. [DOI] [PubMed] [Google Scholar]
- Zacny JP, Lichtor SA (2008). Within-subject comparison of the psychopharmacological profiles of oral oxycodone and oral morphine in non-drug abusing volunteers. Psychopharmacol, 196: 105–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NazrulIslama K, Hossaina J, Ahmeda A, Ahsana M (2002). prevalence of malnutrition and influence of illicit drugs and lifestyle. Br J Nutr, 88(5): 507–513. [DOI] [PubMed] [Google Scholar]
- De Luis D, Lopez AG (2006). Nutritional status of adult patients admitted to internal medicine departments in public hospitals in Castilla y Leon, Spain — a multi-center study. Europ J Int Med, 17(8): 556–560. [DOI] [PubMed] [Google Scholar]
- Dole V, Nyswander M, Kreek M (1966). Narcotic Blockade. Arch Intern Med, 118: 304–309. [PubMed] [Google Scholar]
- Aunno DT, Pollack HA, Frimpong JA (2014). Evidence-based treatment for opioid disorders: A 23-year national study of methadone dose levels. J Subst Abuse Treat, 10 pii: S0740–5472(14)00090–7. doi: 10.1016/j.jsat.20-14.06.001. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leavitt SB (2004). Methadone Maintenance Treatment (MMT). ATF, 1–8. [Google Scholar]
- Payte JT, Khuri ET (1993). Principles of methadone dose determination. In: Parrino MW. State methadone treatment guidelines; Ed, Rockville: Treatment improvement protocol (TIP) series. 47–58. [Google Scholar]
- Zador D, Sunjic S (2000). Deaths in metha-done maintenance treatment in New South Wales, Australia. Addiction, 2000;95(1): 77–84. [DOI] [PubMed] [Google Scholar]
- Zador DA, Sunjic SD (2002). Methadone-related deaths and mortality rate during induction into methadone maintenance, New South Wales, 1996. Drug Alcohol Rev, 21: 131–136. [DOI] [PubMed] [Google Scholar]
- Hummeniuk R, Ali R, McGregor C, Darke S (2003). Prevalence and correlates of intravenous methadone syrup administration in Adelaide, Australia. Addiction, 98: 413–418. [DOI] [PubMed] [Google Scholar]
- Bezchlibnyk-Butler KZ, Jeffries J, Virani A (2007). Clinical handbook of psychotropic drugs. 17th ed. Hogrefe& Huber, Cambridge. [Google Scholar]
- Mello NK, Mendelson JH (1985). Behavioral pharmacology of buprenorphine. Drug Alcohol Depend, 14(34): 283–303. [DOI] [PubMed] [Google Scholar]
- Walsh SL, Preston KL, Stitzer ML, Cone EJ, Bigelow GE (1994). Clinical pharmacology of buprenorphine: ceiling effects at high doses. Clin Pharmacol Ther, 55(5): 569–580. [DOI] [PubMed] [Google Scholar]
- Skurtveit S, Furu K, Kaasa S, Borchgrevink PC (2009). Introduction of low dose transdermal buprenorphine. Eur J Pain, 13: 949–953. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration (2010). FDA approves injectable drug to treat opioid-dependent patients. Available from: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm229109.htm [Google Scholar]
- Degenhardt L, Larance BK, Bell JR, Win-stock AR, Lintzeris N, Ali RL, Scheuer N, Mattick RP (2009). Injection of medicationsused in opioid substitution treatment in Australia after the introduction of a mixed partial agonist-antagonist formulation. MJA, 191: 161–165. [DOI] [PubMed] [Google Scholar]
- Kaye AD, Banister RE, Hoover JM, Baluch AR, Jacobs S, Shah RV (2005). Chronic pain andultrarapid opioid detoxification. Pain Pract, 5: 33–42. [DOI] [PubMed] [Google Scholar]
- Alves D, Costa AF, Custódio D, Natário L, Ferro-Lebres V, Andrade F (2011). Housing and employment situation, body mass index and dietary habits of heroin addicts in methadone maintenance treatment. Assoc Applic Neurosci Knowledge Soci Aims, 13(1): 1592–1638. [Google Scholar]
- Varela P, Marcos A, Ripoll S, Santacruz I, Requejo AM (1997). Effects of human immunodeficiency virus infection and detoxification time on anthropometric measurements and dietary intake of male drug addicts. Am J Clin Nutr, 66(2): 509–514. [DOI] [PubMed] [Google Scholar]
- Hauser MB, Iber FL (1989). Nutritional advice and diet instruction in alcoholism treatment. Alcohol Health Res, 13: 261–266. [Google Scholar]
- Hatcher AS (2004). Weight matters during recovery: unhealthy eating behaviors can impede client progress. Addiction Professional, 2: 23–24. [Google Scholar]
- Cowan J, Devine C (2008). Food, eating, and weight concerns of men in recovery from substance addiction. Appetite, 50: 33–42. [DOI] [PubMed] [Google Scholar]
- Hodgkins CC. Adolescent Weight Gain during Supervised Substance Abuse Treatment: An Examination of Two Interventions Selected as Possible Solutions to the Problem [PhD thesis]. University of Florida, Gainesville; 2003. [Google Scholar]
- Mohs ME, Watson RR, Leonard-Green T (1990). Nutritional effects of marijuana, heroin, cocaine, and nicotine. J Am Diet Assoc, 90(9): 1261–1267. [PubMed] [Google Scholar]
- Mangili A, et al. (2006). Nutrition and HIV infection: Review of weight loss and wasting in the era of highly active antiretroviral therapy from the nutrition for healthy living cohort. Clin Infect Dis, 42(6): 836–842. [DOI] [PubMed] [Google Scholar]
- Himmelgreen DA, Escamilla RP, Milla SS, Daza NR, Tanasescu M, Singer M (1998). A Comparison of the Nutritional Status and Food Security of Drug Using and Non-Drug-Using Hispanic Women in Hartford, Connecticut. Am J Phys Anthropol, 107: 351–361. [DOI] [PubMed] [Google Scholar]
- Islam SKN, Hossain KJ, Ahmed A, Ahsan M (2002). Nutritional status of drug addicts undergoing detoxification: prevalence of malnutrition and influence of illicit drugs and lifestyle. Br J Nutr, 88: 507–513. [DOI] [PubMed] [Google Scholar]
- Himmelgreen DA, Perez-Escamilla R, Segura-Millan S, Romero-Daza N, Tansescu M, Sin M (1998). A comparison of the nutritional status and food security of drug-using and non-drug-using Hispinic women in Hartford, connecticut. Am J Phys Anthropol, 107: 351–361. [DOI] [PubMed] [Google Scholar]
- Varela P, Marcos A, Ripoll S, Santacruz I, Requejo AM (1997). Effects of HIV infection and detoxi®cation time on anthropometric measurements and dietary intake of male drug addicts. Am J Clin Nutr, 66: 509–514. [DOI] [PubMed] [Google Scholar]
- Mathews LJ, Parker RA (1987). Alcoholism Treatment with Biochemical Restoration as a Major Component. Int J Biosocial Res, 9(1): 92–106. [Google Scholar]
- Tao H, H Fox (1976). Measurement of Urinary Pantothenic Acid Excretion of Alcoholic Patients. J Nutr Sci, 22: 333–337. [DOI] [PubMed] [Google Scholar]
- Fishbein D, Pease S (1988). The Effects of Diet on Behavior: Implications for Criminology and Corrections. Research in Corrections, 1(2). [Google Scholar]
- Feinman, L (1989). Absorption and Utilization of Nutrients in Alcoholism. Alcohol Health & Research World, 13(3): 207–210. [Google Scholar]
- Miller RP (2010). Nutrition in Addiction Recovery article. http://manyhandssust-ainabilitycenter.org/ [Google Scholar]
- Williams RJ (1994). Biochmical Individuality. New York: John Wiley & Sons. [Google Scholar]
- DesMaisons K (1998). Potatoes Not Prozac. Fireside, 79. [Google Scholar]