Abstract
BACKGROUND
Gabapentin is used for the treatment of hot flashes and neuropathic pain in breast cancer survivors, and is commonly used off-label for the treatment of anxiety. Yet, clinical trial evidence to support the use of gabapentin for anxiety symptoms is lacking.
METHODS
In a randomized, double-blinded controlled trial we compared 300mg gabapentin versus 900mg gabapentin versus placebo. Subjects were 420 breast cancer patients who had completed all chemotherapy cycles. Anxiety traits and current (state) anxiety were measured using the Speilberger Strait-Trait Anxiety Inventory at baseline, 4 weeks and 8 weeks. Pain was measured at baseline using a 10-point scale. Analyses included analysis of covariance (ANCOVA) and ordinary least squares regression.
RESULTS
At 4 weeks, state anxiety change scores were significantly better for gabapentin 300mg and 900mg (p=0.005) compared to placebo. The magnitude of improvement was proportional to baseline state anxiety. At 8 weeks, the anxiolytic effects of gabapentin compared to placebo persisted (p < 0.005). We found no significant interactions.
CONCLUSIONS
Given its similar pharmacology, efficacy in the treatment of hot flashes, and low cost, gabapentin may provide a low cost and parsimonious alternative treatment choice for breast cancer survivors presenting in primary care practices with anxiety symptoms. Gabapentin is effective for hot flashes, and therefore may provide therapeutic benefit for both anxiety and hot flashes at a generic drug price. For patients reluctant to take a controlled substance, such as a benzodiazepine, gabapentin may offer an alternative therapy. Similarly, patients with a history of substance use may benefit from gabapentin without risk of addiction or abuse.
For cancer survivors experiencing both hot flashes and anxiety, gabapentin may provide a single effective treatment for both and is an alternative therapy for anxiety for patients unwilling to take a benzodiazepine or those with a history of substance use.
Keywords: Gabapentin, Neurontin, anti-epileptics, breast, cancer, anxiety, randomized controlled trial, cancer survivorship
Introduction
Cancer survivors typically visit oncologists only annually for follow-up and otherwise seek care from primary care providers. More than 2.5 million breast cancer survivors present to primary care providers in the US [1]. Patient satisfaction has been shown to be higher among those followed by their primary care provider compared to those followed by an oncology specialist [2].
Among breast cancer survivors, a variety of symptoms such as fatigue, hot flashes and anxiety have been shown to persist 12 months after surgery [3,4] at which time as many as 38.4% of patients have been shown to have severe anxiety [5]. Fear of cancer recurrence is among the most frequently cited “unmet needs” in cancer survivors [6]. Of all patients visiting primary care providers, 19.5% have been shown to have at least one anxiety disorder, 40% of whom were not receiving any treatment [7].
A recent review of progress in pharmacologic treatment of anxiety disorders noted “the paucity of double-blind trials” of anticonvulsants (including gabapentin) for the treatment of anxiety disorders [8]. The only drug in this class for which significant randomized controlled trial evidence is available is pregabalin (Lyrica, Pfizer), which has been shown to be efficacious for the treatment of generalized anxiety disorder. The review recommends that clinicians use gabapentin or other anticonvulsants only for cases of treatment resistance to other drug classes or possibly as adjuvant therapy with “more established first line agents.”
Yet, the generic predecessor to pregabalin, is gabapentin (Neurontin, Pfizer) which has a similar pharmacology to pregabalin. Pfizer abandoned studies of gabapentin shortly before the drug lost is patent protection and instead conducted randomized controlled trials of its branded successor, pregabalin (Lyrica, Pfizer). Since then, pregabalin has been shown to be effective for both generalized anxiety disorder and social anxiety disorder, including for maintenance therapy [8-11]. Pregabalin and gabapentin are theorized to improve anxiety symptoms through the same mechanisms of action: (1) increasing GABAergic neurotransmission, and (2) Inhibiting voltage-gated sodium and calcium channels [12]. Yet, lack of clinical trial data supporting the use of gabapentin for the treatment of anxiety may have limited its use for this indication. If effective in the treatment of anxiety, gabapentin would present several advantages over pregablin: (1) It is generic, and therefore less expensive; (2) unlike pregablin, gabapentin is not a Schedule 4 drug; (3) gabapentin may treat more than one indication common in breast cancer survivors, as it has also been shown effective in the treatment of both neuropathic pain and hot flashes. Currently, both pregabalin and gabapentin are commonly used for the same indication in cancer (adjuvant anti-convulsant analgesics) [13]. Yet, to our knowledge, no randomized controlled trials yet exist that address the use of gabapentin (or its branded successor, pregabalin) for anxiety symptoms in cancer patients or in cancer survivorship.
If gabapentin is similarly effective for the treatment of anxiety, then it may represent an alternative to pregabalin. Pregabalin is both a branded drug and a controlled substance, whereas gabapentin is neither brand nor controlled. In addition, gabapentin has been shown in a randomized controlled trial to be effective for the treatment of hot flashes, a common symptom among breast cancer survivors. As such, if gabapentin were shown to be effective for the treatment of anxiety disorders, then it may be a valid monotherapy for both hot flashes and anxiety. Finally, if effective for the treatment of anxiety, then gabapentin would offer a therapeutic alternative to the benzodiazepines, controlled substances which carry the possibility of addiction, and anti-depressants, particularly for patients who do not exhibit explicit signs of depression.
Finally, cancer survivors may have already taken gabapentin during their cancer treatment and may therefore be more comfortable with taking it again than with trying a new medication. Gabapentin (generic; previously branded as Neurontin by Pfizer) is an anticonvulsant commonly used in the treatment of pain and hot flashes associated with cancer, its treatment and cancer survivorship. Since 1994, guidelines for the management of cancer pain have included the adjuvant use of gabapentin or other anticonvulsants [14]. It is an effective adjuvant therapy for the treatment of metastatic pain and neuropathic cancer pain [15-17]. Gabapentin may also be used preoperatively to improve acute pain after surgery, including breast cancer surgery [18, 19]. Most recently, adjuvant gabapentin analgesia has been cited as consistent with the World Health Organization's analgesic ladder for cancer pain relief [13]. Pain is experienced by approximately 90% of patients at some time during their cancer illness [20].
In breast cancer survivorship, chronic neuropathic pain (defined at 6 months post-treatment) is effectively treated with adjunctive gabapentin [18]. In a randomized, controlled trial in breast cancer subjects, gabapentin reduced the frequency and severity of hot flashes [21]. Migraine is another indication for which gabapentin is commonly prescribed [12].
The primary aim of this analysis of a large nationwide randomized clinical trial conducted by the University of Rochester Cancer Center Community Clinical Oncology Research Base is to compare the efficacy of gabapentin 300mg and gabapentin 900mg versus placebo for controlling anxiety symptoms among breast cancer survivors post chemotherapy and radiation therapy.
Methods
Data and Subjects
Based on the pharmacology of gabapentin, a relationship between exposure and anxiety was hypothesized and specified a priori in the design of a double-blinded, placebo-controlled trial of gabapentin for the treatment of hot flashes in breast cancer patients: Gabapentin for the Control of Hot Flashes in Women with Breast Cancer (ClinicalTrials.gov identifier: NCT00022074). Trial procedures and criteria are described in detail elsewhere [9]. Briefly, data were collected between June 2001 and July 2003 by the University of Rochester Community Clinical Oncology Program (CCOP) of the James P Wilmot Cancer Center at the University of Rochester Medical Center. Subjects were 420 women aged 18 or older with a diagnosis of breast cancer who had completed all chemotherapy cycles and reported experiencing two or more hot flashes per day for at least seven days prior to enrollment. Exclusion criteria included (1) current chemotherapy; (2) exposure to any other anti-epileptic drug or history of allergic reaction to gabapentin; (3) exposure to other medications for hot flashes, specifically clonidine or venlafaxine; (4) renal, liver, or hepatic dysfunction; (5) coronary insufficiency or significant recent history of coronary or cerebrovascular event; and (6) hypotension. To protect against any risk of birth defects due to exposure to gabapentin, subjects were excluded if they did not use a medically acceptable method of birth control, including abstinence. Outcomes were assessed at baseline, 4 and 8 weeks.
Baseline Assessments of Anxiety
Anxiety was assessed by the state scale of the Speilberger State-Trait Anxiety Inventory (STAI), a commonly used measure of anxiety symptoms in clinical research [21] and specifically in cancer screening, treatment and survivorship (for example, Beaver K, et al 2009; van den Bergh R, et al, 2009; Den Oudsten BL, et al, 2009; Fenlon DR et al, 2009) [22-25]. State anxiety response scales have 4 points measuring frequency of feelings (‘almost never’ to ‘almost always’). The STAI has adequate discriminate validity and distinguishes accurately between those with psychiatric diagnoses and adults in the general population [21]. The STAI has adequate predictive validity and demonstrates higher mean scores in stressful situations than in neutral or relaxed situations. The STAI yields a single summary score for current anxiety (“state” anxiety) ranging from 20 to 80, with higher scores representing greater anxiety.
Baseline Measurement of Pain
We measured pain at baseline using a 10-point scale first developed for the Symptom Inventory (SI) at MD Anderson and Memorial Sloan Kettering Cancer Centers. The scale range is 0 to 10 as follows: “0” = “pain not present” to “10” = “pain as bad as you can imagine it could be”.
Efficacy Outcomes
The aim of this study was to compare the effect of 3 treatment arms (placebo, gabapentin 300mg daily, gabapentin 900mg daily) on anxiety at 4 weeks and 8 weeks, respectively. Therefore, the primary efficacy variable was defined as the mean anxiety score at 4 weeks and 8 weeks, respectively.
Statistical Methods
Randomization did not include stratification by baseline anxiety or pain. To determine whether assignment to the 3 treatment arms varied by the efficacy measure (anxiety), confounder (pain), or clinical and demographic characteristics, we used one-way analysis of variance (ANOVA) to test for differences among means.
Analysis of the primary efficacy outcome, anxiety symptom scale score, was assessed using an analysis of covariance (ANCOVA) approach as suggested by Frison and Pocock. Each patient's post-treatment state anxiety values were average and then used as a dependent variable in an ANCOVA model with baseline state anxiety symptom scale score as covariate, as well as treatment arm and the interaction terms treatment arm by change score from baseline. For parsimony, insignificant baseline interaction terms were dropped. Data were not imputed; rather only those for whom data were complete were included in the analyses.
In addition, an ordinary least squares (OLS) regression model was estimated for the primary outcome measure at 8 weeks. Covariates included treatment group (3 arms), baseline anxiety symptom score, past chemotherapy exposure, past radiation treatment, baseline use of tamoxifen, pain at baseline, and interaction terms betweens these variables. To test model assumptions, we used residual plots and checked for outliers.
We used SAS Version 9.2 and R Version 2.9 for all analyses.
Results
Baseline Clinical Characteristics and Demographics
Subjects were 420 women. Withdrawal numbers and causes were previously described [20]. Table 1 illustrates that there were no significant differences between treatment arms in terms of age, race, education or marital status. Baseline pain and anxiety were similar across treatment arms as well (Table 1). No significant differences were found between withdrawal rates, history of radiation and chemotherapy and current tamoxifen use.
Table 1.
Demographic and Baseline Characteristics
| Placebo (n = 137) | 300mg gabapentin (n=139) | 900mg gabapentin (n=144) | F or X2 | |
|---|---|---|---|---|
| Age (SD), years | 54 (7.4) | 56 (8.7) | 55 (8.7) | 1.36 |
| White, n (%) | 127 (95.5) | 126 (94.7) | 136 (95.8) | 0.53 |
| Married, n (%) | 94 (73.4) | 97 (75.2) | 107 (78.1) | 0.87 |
| College/graduate degree, n (%) | 57 (44.5) | 35 (27.13) | 52 (38.0) | 0.20 |
| Current use of tamoxifen, n (%) | 94 (75.2) | 88 (69.3) | 94 (69.1) | 0.48 |
| Previous chemotherapy, n (%) | 11 (8.9) | 13 (10.2) | 15 (11.1) | 0.85 |
| Previous radiotherapy, n (%) | 10 (8.1) | 13 (10.3) | 12 (8.9) | 0.83 |
| Pain, M (SE) | 2.0 (0.22) | 1.6 (0.22) | 1.7 (0.22) | 1.07 |
| State Anxiety Symptom Score Baseline | 35.9 (0.99) | 36.7 (0.99) | 35.1 (0.94) | 0.71 |
Efficacy of Gabapentin 300mg and 900mg for the Treatment of Anxiety Symptoms
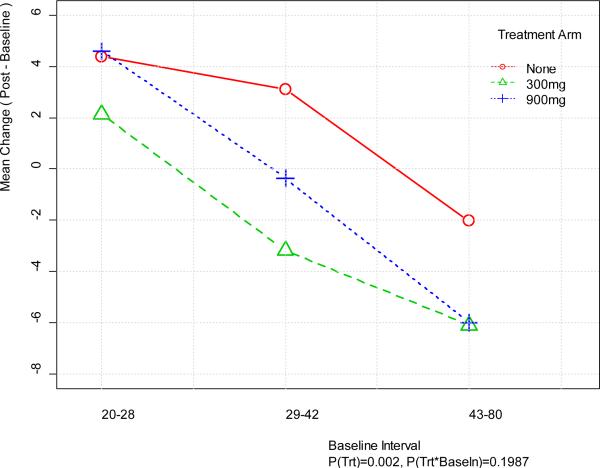
At 4 weeks, anxiety change scores for the placebo, 300mg and 900mg gabapentin treatment arms had diverged, demonstrating significantly better outcomes with gabapentin (p=0.005) (Table 2). The magnitude of improvement was proportional to baseline anxiety symptom score (Figure 1). That is, subjects with relatively high anxiety symptom scores at baseline showed the greatest improvement following treatment with gabapentin 300mg or 900mg. As Table 2 demonstrates, anxiety symptoms worsened in the placebo arm, improved significantly in the 300mg treatment arm, and showed little change in the 900mg arm at 4 weeks.
Table 2.
Analysis of anxiety mean change scores, baseline – 4 weeks
| Treatment arm | Anxiety |
|---|---|
| Gabapentin 900 mg | |
| Model adjusted mean change score | −0.07 |
| SE | 0.77 |
| Gabapentin 300 mg | |
| Model adjusted mean | −1.77 |
| SE | 0.79 |
| Placebo | |
| Model adjusted mean | 1.06 |
| SE | 0.82 |
| P | 0.005 |
Parameter estimates of the model (p values)
Coefficients: intercept = 36.57 (p < 0.001), 300 mg = −2.83 (p < 0.05), 900 mg = −1.12 (p > 0.10), cBase = 0.88 (p < 0.001), 300 mg × cBase = −0.28 (p < 0.001), 900 mg × cBase = −0.24 (p < 0.01); adjusted R2 = 0.46
Figure 1.
Mean Change in Anxiety at Week 4 versus Baseline Anxiety
At 8 weeks, the anxiolytic effects of gabapentin persisted (p < 0.005; Table 3). We found no significant interactions, but some features are similar to those seen at 4 weeks (Figure 2).
Table 3.
Analysis of Anxiety Mean Change Scores, Baseline – 8 weeks
| Treatment Arm | Anxiety |
|---|---|
| Gabapentin 900mg | |
| Model Adjusted Mean | −0.249 |
| SE | 0.851 |
| Gabapentin 300 mg | |
| Model Adjusted Mean | −2.440 |
| SE | 0.891 |
| Placebo | |
| Model Adjusted Mean | 2.140 |
| SE | 0.909 |
| P | 0.002 |
Figure 2.
Mean Change in Anxiety at Week 8 versus Baseline Anxiety
Patients with the lowest levels of anxiety experienced little change at 8 weeks. The 300 mg dose appears to be optimal, except for those with the highest levels of anxiety for whom both doses had similar effects.
Discussion
Gabapentin was efficacious in reducing anxiety in breast cancer survivors in this randomized, controlled double-blind trial. At both the 300mg and 900mg doses, significant reductions in anxiety were seen at 4 and 8 weeks. Effect sizes at 4 weeks (but not 8 weeks) were related to baseline anxiety; higher baseline anxiety was associated with larger reductions in anxiety during treatment with gabapentin at either dose. We found little, if any, difference in anxiolytic effect between the doses in this population with relatively low baseline anxiety and pain. Baseline scores for anxiety were similar across arms and relatively low, with arm means similar to those seen in other breast cancer survivor populations [23].
Bioavailability and the Dose-Response Relationship
Gabapentin bioavailability is not dose proportional and is therefore not expected to produce a linear dose-response relationship. As dose rises, bioavailability declines (Table 4). Specifically, when given in 3 evenly divided doses per day, bioavailability declines from 60% to 27% of dose as the dose increases from 300mg to 4800mg total per day [26].
Table 4.
Bioavailability of Gabapentin by Daily Total Dose
| Dose | Bioavailability | Effective Dose |
|---|---|---|
| 300mg | 60% | 180 mg |
| 1200mg | 47% | 564 mg |
| 4800mg | 27% | 1296 mg |
Food has only a slight effect on the rate and extent of absorption of gabapentin. It is plausible that the lower dose is more specific for the desired clinical outcome (anxiolytic) while the higher dose ends up being less specific as it has effects at multiple receptors. Many drugs have inverted U shaped curves as non-specific effects arise. Additionally, it is not uncommon for the characteristics of a drug to change as the dose changes. Meaning, for example, at a one dose the drug is an agonist, while at another dose the drug may act as an inverse- or partial- agonist, which would change the clinical outcomes. As a result, a relatively small 300mg daily dose is hypothesized to induce a similar improvement in anxiety symptoms to the 900mg dose, and with fewer side effects.
Did improvement in pain control lead to an improvement in anxiety symptoms?
Gabapentin has been demonstrated in numerous trials to be an efficacious treatment for pain. Pain pathways are linked directly to and moderated by both midbrain and cortical pathways. The cortical pathway expresses anxiety, depression, sleeplessness and fear. These interlinked pathways imply that anxiety will intensify the pain experience and vice versa [13]. These facts raise the question: was our reduction in anxiety an indirect result of pain control due to gabapentin?
This trial featured relatively low doses of gabapentin of 300mg/day and 900mg/day, respectively. Gabapentin dosing for adjuvant analgesia in cancer pain is 1800mg/day given in 3 equal doses at 8-hour intervals up to a maximum of 2400 mg/day (Gabapentin neuropathic pain dosing form) [27]. Our finding that 300mg/day improved anxiety symptoms as well or better than the 900mg/day dose suggests that the effect of gabapentin is direct because we would not expect significant pain control with such a low dose.
Support for this conclusion is also provided by the relatively low pain scores at baseline in our study subjects. On a scale of 0 to 10, baseline pain scores averaged below 2.
Every week, the FDA issues a labeling or dosing form change for a drug. Dosing form changes are usually made to reduce doses from their initial marketed dose. Our finding that clinically important and statistically significant improvements in anxiety symptoms could be obtained at the 300 mg dose may be a reflection of this trend. Dosing at the lowest possible dose may also prevent the occurrence or severity of the most common gabapentin side effects ranging from drowsiness, cold symptoms, weakness and blurred vision to dementia and delusions [28].
Exposure to Unobserved Agents
Our data were collected for a randomized controlled trial of gabapentin for the treatment of hot flashes in breast cancer patients [21]. This trial excluded patients who were taking clonidine or venlafaxine (a common comparison drug in anxiety trials) or any other medication in the same drug class as gabapentin (anti-convulsants or AEDs). Yet, other medications were permitted, including anti-depressants. It is possible that unobserved agents may have been in use by some study participants, yet randomization is expected to have eliminated the risk of any systematic bias across study groups. Use of other agents is expected to only reduce the power of this re-analysis to detect significant effects of gabapentin on anxiety.
The power of our sample to detect significant results in the face of confounding by other medication exposures was likely also limited by stable regimens over the short course of the trial which lasted only 8 weeks. Similarly, subjects had been diagnosed with cancer and completed chemotherapy prior to enrollment in the trial, suggesting that any anti-depressant regimens associated with the diagnosis of cancer were likely stable by the time of enrollment in the RCT. Finally, patients are generally reluctant to take multiple drug regimens simultaneously and may have postponed new drug regimens until completion of the 8-week RCT.
Clinical implications
Given its similar pharmacology, efficacy in the treatment of hot flashes, and low cost, gabapentin may provide a low cost and parsimonious alternative treatment choice for clinicians seeking drug treatments for breast cancer survivors presenting in primary care practices with anxiety symptoms. Gabapentin is effective for hot flashes, and therefore may provide therapeutic benefit for both anxiety and hot flashes at a generic drug price. For patients reluctant to take a controlled substance such as pregabalin or a benzodiazepine, gabapentin may offer an alternative therapy. Similarly, patients with a history of substance use may benefit from gabapentin without risk of addiction or abuse. Benzodiazepine use is higher among breast cancer patients than it is among the general population (7.9% vs. 3%) [29]. Benzodiazepines can cause sedation and ataxia, and their use has been associated with an increased risk of traffic accidents [30]. They also can cause a rare paradoxical increase in anxiety in certain patients [31]. Tolerance, addiction, and withdrawal can also become problematic, especially if benzodiazepines are taken for extended period of time. The use of benzodiazepines is not recommended for longer than 4 weeks [32]. Anxiety can continue in breast cancer patients for up to 12 months after treatment, and so a long-term treatment is preferred for these patients [4].
Gabapentin is currently used off-label in psychiatry to treat anxiety symptoms. It is also commonly used to treat hot flashes and neuropathic pain in breast cancer survivors. In this study we provide clinical trial evidence of the efficaciousness of gabapentin for anxiety in breast cancer survivors. Anxiety symptoms are prevalent and potentially devastating in cancer survivors, particularly breast cancer survivors whose may otherwise be expected to be highly functioning for many years to come.
In addition, gabapentin is a generic drug with relatively few side effects, making it an attractive therapeutic choice. After gabapentin went off-patent and became a generic drug, its next generation successor, pregabalin, was found to be effective in the treatment of anxiety disorders, specifically generalized anxiety disorder and social anxiety [10]. Pregabalin was shown to be well tolerated compared to other medications with indication for generalized anxiety disorder [33] Pregabalin and gabapentin are theorized to improve anxiety symptoms through the same mechanisms of action: (1) increasing GABAergic neurotransmission, and (2) Inhibiting voltage-gated sodium and calcium channels [12]. Yet, lack of clinical trial data supporting the use of gabapentin for the treatment of anxiety may have limited its use for this indication. Gabapentin has a similar mechanism of action and low effective dose, and so it may have similar tolerability to pregabalin for the treatment of anxiety. Pregabalin is currently on patent and is therefore more expensive than gabapentin, It is also a schedule 4 drug, unlike gabapentin. Currently, both pregabalin and gabapentin are commonly used for the same indication in cancer (adjuvant anti-convulsant analgesics) [13].
Conclusion
Given its similar pharmacology, efficacy in the treatment of hot flashes, and low cost, gabapentin may provide a low cost and parsimonious alternative treatment choice for clinicians seeking drug treatments for breast cancer survivors presenting in primary care practices with anxiety symptoms. Gabapentin is effective for hot flashes, and therefore may provide therapeutic benefit for both anxiety and hot flashes at a generic drug price. For patients reluctant to take a controlled substance such as pregabalin or a benzodiazepine, gabapentin may offer an alternative therapy. Similarly, patients with a history of substance use may benefit from gabapentin without risk of addiction or abuse.
Gabapentin 300mg and 900mg were each associated with significant improvement in anxiety symptoms compared to placebo. We demonstrated increased improvement due to gabapentin with higher levels of baseline anxiety. We found no effects for patients with low baseline anxiety.
Notably, the lower, 300 mg dose was associated with the best treatment outcomes for all patients except those with the highest baseline anxiety. This may be due to increased side effects at the higher gabapentin dose (900mg). For patients with high anxiety, both the 300 and 900 mg doses produced similar reductions in anxiety.
Our finding that gabapentin is effective for anxiety symptoms in this relatively healthy group of breast cancer survivors provides support for recent clinical papers supporting the use of gabapentin to treat anxiety disorders in primary care settings.
Acknowledgments
Sources of Support requiring Acknowledgement: This research was funded by the National Cancer Institute.
References
- 1.Chalasani P, Downey L, Stopeck AT. Caring for the breast cancer survivor: a guide for primary care physicians. Am J Med. 2010;123(6):489–95. doi: 10.1016/j.amjmed.2009.09.042. [DOI] [PubMed] [Google Scholar]
- 2.Khatcheressian J, Wolff A, Smith T, et al. American Society of Clinical Oncology 2006 Update of Breast Cancer Follow-Up and Management Guidelines in the Adjuvant Setting. Journal of Clinical Oncology. 2006;24(31):5091–5097. doi: 10.1200/JCO.2006.08.8575. [DOI] [PubMed] [Google Scholar]
- 3.Lavigne JE, Griggs JJ, Tu XM, Lerner DJ. Hot flashes, fatigue, treatment exposures and work productivity in breast cancer survivors. J Cancer Surviv. 2008 Dec;2(4):296–302. doi: 10.1007/s11764-008-0072-z. Epub 2008 Nov 12. [DOI] [PubMed] [Google Scholar]
- 4.Hartl K, Schennach R, Muller M, Engel J, Reinecker H, Sommer H, Friese K. Quality of life, anxiety, and oncological factors: A follow-up study of breast cancer patients. Psychosomatics. 2010;51:112–123. doi: 10.1176/appi.psy.51.2.112. [DOI] [PubMed] [Google Scholar]
- 5.Vahdaninia M, Omidvari S, Montazeri A. What do predict anxiety and depression in breast cancer patients? A follow-up study. Social Psychiatry and Psychiatric Epidemiology. 2010;45(3):355–61. doi: 10.1007/s00127-009-0068-7. [DOI] [PubMed] [Google Scholar]
- 6.Armes J, Crowe M, Colbourne L, et al. Patients’ Supportive Care Needs Beyond the End of Cancer treatment: A Prospective, Longitudinal Survey. Journal of Clinical Oncology. 2009;27(36):6172–6179. doi: 10.1200/JCO.2009.22.5151. [DOI] [PubMed] [Google Scholar]
- 7.Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity and detection. Annals of Internal Medicine. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 8.Ravindran LN, Stein MB. The pharmacologic treatment of anxiety disorders: A review of progress. J Clin Psychiatry. 2010;71:7. doi: 10.4088/JCP.10r06218blu. [DOI] [PubMed] [Google Scholar]
- 9.Pande AC, Feltner DE, Jefferson JW, et al. Efficacy of the novel anxiolytic pregabalin in social anxiety disorder: A placebo-controlled multi-center study. J Clin Psychopharmacology. 2004;24:141–149. doi: 10.1097/01.jcp.0000117423.05703.e7. [DOI] [PubMed] [Google Scholar]
- 10.Montgomery SA, Tobias K, Zornberg GL, et al. Efficacy and safety of pregabalin in the treatment of generalized anxiety disorder: a 6-week, multicenter, randomized, double-blind, placebo-controlled comparison of pregabalin and venlafaxine. J Clin Psychiatry. 2006;67:771–82. doi: 10.4088/jcp.v67n0511. [DOI] [PubMed] [Google Scholar]
- 11.Scheiner FR. Clinical Practice: Social Anxiety Disorder. N Engl J Med. 2006;355:1029–36. doi: 10.1056/NEJMcp060145. [DOI] [PubMed] [Google Scholar]
- 12.Landmark CJ. Antiepileptic drugs in non-epilepsy disorders: Relations between mechanisms of action and clinical efficacy. CNS Drugs. 2008;22(1):27–47. doi: 10.2165/00023210-200822010-00003. [DOI] [PubMed] [Google Scholar]
- 13.Jacox A, Carr DB, Payne R, et al. Management of Cancer Pain. Clinical Practice Guideline No. 9. AHCPR Publication No. 94-0592. Agency for Health Care Policy and Research, U.S. Department of Health and Human Services, Public Health Service; Rockville, Maryland: 1994. [Google Scholar]
- 14.Keskinbora K, Pekel EF, Aydinli I. Gabapentin and an opioid combination versus opioid alone for the management of neuropathic cancer pain: a randomized open trial. J Pain Symptom Manage. 2007;34:183–189. doi: 10.1016/j.jpainsymman.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 15.Caraceni A, Zecca E, Bonezzi C, et al. Gabapentin for neuropathic cancer pain: A randomized, controlled Trial from the gabapentin cancer pain study group. J Clin Oncol. 2004;22:2909–2917. doi: 10.1200/JCO.2004.08.141. [DOI] [PubMed] [Google Scholar]
- 16.Caraceni A, Brunelli C, Martini C, et al. Cancer pain assessment in clinical trials. A review of the literature. J Pain Symptom Manage. 2005;29:507–19. doi: 10.1016/j.jpainsymman.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 17.Fassoulaki A, Triga A, Melemeni A, et al. Multimodal Analgesia with Gabapentin and Local Anesthetics Prevents Acute and Chronic Pain After Breast Surgery for Cancer. Anesth Analg. 2005;101:1427–32. doi: 10.1213/01.ANE.0000180200.11626.8E. [DOI] [PubMed] [Google Scholar]
- 18.Menigaux C, Adam F, Guignard B, Sessler DI, Chauvin M. Preoperative gabapentin decreases anxiety and improves early functional recovery from knee surgery. Anesth Analg. 2005;100:1394–1399. doi: 10.1213/01.ANE.0000152010.74739.B8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Caraceni A, Portenoy RKA working group of the IASP task force on cancer pain. An international survey of cancer pain characteristics and syndromes. Pain. 1999;82:263–74. doi: 10.1016/S0304-3959(99)00073-1. [DOI] [PubMed] [Google Scholar]
- 20.Pandya KJ, Morrow GR, Roscoe JA, et al. Gabapentin for hot flashes in 420 women with breast cancer: a randomized double-blind placebo-controlled trial. Lancet. 2005;366:818–24. doi: 10.1016/S0140-6736(05)67215-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Speilberger CD, Gorsuch RL, Luschene R. STAI Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA: [Google Scholar]
- 22.Beaver K, Tysver-Robinson D, Campbell M, Twomey M, Williamson S, Hindley A, et al. Comparing hospital and telephone follow-up after treatment for breast cancer: randomized equivalence trial. BMJ. 2009;338:s3147. doi: 10.1136/bmj.a3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van den Bergh R, Essink-Bot ML, Roobol MJ, et al. Anxiety and distress during active surveillance for early prostate cancer. Cancer. 2009;115(17):386–3878. doi: 10.1002/cncr.24446. [DOI] [PubMed] [Google Scholar]
- 24.Den Oudsten BL, Van Heck GL, Van der Steeg AFW, Roukema JA, DeVries J. The WHOQOL-100 has good psychometric properties in breast cancer patients. J Clin Epi. 2009;62(2):195–205. doi: 10.1016/j.jclinepi.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 25.Fenlon DR, Corner JL, Haviland J. Menopausal hot flushes after breast cancer. European Jrnl Cancer Care. 2009;18(2):14–148. doi: 10.1111/j.1365-2354.2007.00902.x. 2009. [DOI] [PubMed] [Google Scholar]
- 26.Cundy K, Annamalai T, Bu L, De Vera J, Estrela J, Luo W, Shirsat P, Torneros A, Yao F, Zou J, Barrett RW, Gallop MA. XP13512: A Novel gabapentin prodrug: II. Improved Oral Availability, dose proportionality, and colonic absorption compared with gabapentin in rats and monkeys. J Pharmacology & Experiential Therapeutics. 2004;311:324–333. doi: 10.1124/jpet.104.067959. [DOI] [PubMed] [Google Scholar]
- 27.Laird B, Colvin L, Fallon M. Management of cancer pain: Basic principles and neuropathic cancer pain. European J Cancer. 2008;48:1078–1082. doi: 10.1016/j.ejca.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 28.Gabapentin . DRUGDEX® System. Thomson Healthcare; [August 7, 2012]. http://www.thomsonhc.com. [Google Scholar]
- 29.Vaidya R, Sood R, Karlin N, Jatoi A. Benzodiazepine Use in Breast Cancer Survivors: Findings from a Consecutive Series of 1000 Patients. Oncology. 2011;81:9–11. doi: 10.1159/000330814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orriols L, Phillip P, Moore N, et al. Benzodiazepine-like hypnotics and the associated risk of road traffic accidents. Clinical Pharmacology & Therapeutics. 2011;89(4):595–601. doi: 10.1038/clpt.2011.3. [DOI] [PubMed] [Google Scholar]
- 31.Cole J, Kando J. Adverse behavioral events reported in patients taking alprazolam and other benzodiazepines. The Journal of clinical psychiatry. 1993;54:49–63. [PubMed] [Google Scholar]
- 32.Lader M. Limitations on the use of benzodiazepines in anxiety and insomnia: are they justified? European Neuropsychopharmacology. 1999;9:s399–s40. doi: 10.1016/s0924-977x(99)00051-6. [DOI] [PubMed] [Google Scholar]
- 33.Baldwin D, Woods R, Lawson R. Efficacy of drug treatments for generalized anxiety disorder: systemic review and meta-analysis. BMJ. 2011;342:d1199. doi: 10.1136/bmj.d1199. [DOI] [PubMed] [Google Scholar]