Abstract
Objective(s)
To estimate the impact of various expansion scenarios of the National Bowel Cancer Screening program (NBSCP) on the number of bowel cancer deaths prevented. Impact of the expansion scenarios on colonoscopy demand was also investigated.
Design
MISCAN-Colon, a well-established, validated computer simulation model for bowel cancer screening, was adjusted to reflect the Australian situation. In July 2013, we simulated the effects of screening over a 50 year period, starting in 2006. The model parameters included participation rates for screening and follow up, cancerous and pre-cancerous lesion identification rates, bowel cancer incidence, mortality and the outcomes of the NBCSP. Five implementation scenarios, based on biennial screening using an immunochemical faecal occult blood test, were developed and modelled. A sensitivity analysis that increased screening participation to 60% was also conducted.
Setting/ Participants
Australian residents aged 50 to 74 years
Main outcome measures
Impact and comparison of five implementation scenarios on the number of bowel cancer deaths prevented and demand for colonoscopy.
Results
In its current state, MISCAN-Colon calculated that the NBCSP should prevent 35,169 bowel cancer deaths in the coming 40 years. Accelerating the expansion of the program to achieve biennial screening by 2020, more than 70,000 deaths would be prevented. If complete implementation of biennial screening resulted in a corresponding increase in participation to 60%, the number of deaths prevented increased across all scenarios.
Conclusion(s)
The findings strongly support the need for rapid implementation of the National Bowel Cancer Screening Program. Compared to the current situation, achieving biennial screening by 2020 could result in 100% more bowel cancer deaths being prevented (approximately 35,000) in the coming 40 years.
Introduction
With more than 14,000 newly diagnosed cases and approximately 4000 deaths each year, bowel cancer, or colorectal cancer, is an important health issue in Australia.1 Bowel cancer is the second most commonly reported cancer and the second most common cause of cancer related death in Australia.1 Estimates show that one in 12 Australians are likely to develop bowel cancer before the age of 85,2 making Australia highly ranked in bowel cancer incidence by international comparisons.3
Screening for bowel cancer is an attractive and viable option based on the World Health Organization's criteria for a cancer screening program.4 Screening using faecal occult blood tests (FOBT) is well established as an effective way to reduce incidence and mortality of bowel cancer in the general population.5-8 In 1999, the Australian National Health and Medical Research Council (NHMRC) recommended biennial screening with FOBT for those aged over 50.9 The National Bowel Cancer Screening Program (NBCSP), using immunochemical FOBTs (iFOBT), commenced in 2006 but was limited in scope, only offering screening to specific age cohorts (ages 55 and 65 years from 2006 and age 50 from 2008).10
In the 2012-13 Budget, the Australian Federal Government announced an on-going commitment to the NBCSP and additional funding to expand the eligibility criteria.11 The funding was used to add 60-year-olds in 2013 and will enable 70-year-olds to be included from 2015. The announcement also indicated the Government's intention to further expand the NBCSP to meet NHMRC guidelines, stating that biennial screening would be progressively phased in and achieved by 2034.11 In August 2013, the then Shadow Health Minister announced that under a Coalition government, biennial screening for 50 to 74-year olds would be achieved by 2020. The Coalition won the Federal election in September 2013 and is expected to act on this commitment, although to date, no further announcement has been made.
Using micro-simulation modelling this paper estimated the impact and outcome of various expansion scenarios to establish the best possible implementation of the NBCSP.
Methods
MISCAN-Colon Model
The MISCAN-Colon micro-simulation model and the data Appendix 1 (online at mja.com.au). In brief, the model simulates a large population of individuals from birth to death, first without and then with screening for bowel cancer. The simulation of life history modelled several factors including adenoma prevalence, size and multiplicity, progression of adenoma to cancer, stage at diagnosis and life expectancy after diagnosis.
The model simulated the Australian population age distribution as at June 2011,12 and life expectancy observed in 2009.13 The model was calibrated to match age-specific incidence of bowel cancer as observed in Australia before the introduction of the NBCSP (2006).10 Stage distribution, localisation of cancers in the bowel and five-year relative survival after clinical diagnosis of a cancer were based on Australian literature.14, 15
The validity of the MISCAN-Colon model has been successfully tested on the results of several large screening and surveillance studies.5-7, 16-18 The model has also been shown to explain observed incidence and mortality trends in the United States accounting for risk factor trends, screening practice, and chemotherapy.19
Modelling Parameters
Scenarios
Screening in the Australian population was simulated over 50 years starting in 2006 (the year the NBCSP commenced), using five scenarios (Table 1). The “current” scenario modelled the existing screening program including the addition of 70-year-olds in 2015. The base scenario (“slow”) was based on a proposed implementation plan, as set out in the 2012-13 Budget papers.11 In this scenario, one age cohort was added every two years, starting with 70-year-olds in 2015. Subsequent age cohorts were added every other year from oldest to youngest. Full implementation was achieved by 2035.
Table 1. Modelled implementation scenarios.
| Year | Current | Slow | Annual | Multiple | 5 year | |
|---|---|---|---|---|---|---|
| 2006 | 55/65 | 55/65 | 55/65 | 55/65 | 55/65 | |
| 2007 | ||||||
| 2008 | 50 | 50 | 50 | 50 | 50 | |
| 2009 | ||||||
| 2010 | ||||||
| 2011 | ||||||
| 2012 | ||||||
| 2013 | 60 | 60 | 60 | 60 | 60 | |
| 2014 | ||||||
| 2015 | 70 | 70 | 70 | 70 | 70/72/74 | |
| 2016 | 64/68# | |||||
| 2017 | 72/74 | 72/74 | 72/74 | 54/58* | ||
| 2018 | 68 | 64/68# | 62/66 | |||
| 2019 | 68 | 64# | 62/58/54* | 52/56˄ | ||
| 2020 | 62/58 | 52/66 | ||||
| 2021 | 68# | 66 | 56˄ | |||
| 2022 | 54* | |||||
| 2023 | 66 | 52 | ||||
| 2024 | 56˄ | |||||
| 2025 | 64 | |||||
| 2026 | ||||||
| 2027 | 62 | |||||
| 2028 | ||||||
| 2029 | 58* | |||||
| 2030 | ||||||
| 2031 | 56 | |||||
| 2032 | ||||||
| 2033 | 54 | |||||
| 2034 | ||||||
| 2035 | 52˄ | |||||
final year of screening for 55-year-olds
final year of screening for 65-year-olds
biennial screening achieved
Table shows the year in which age cohorts are added to the screening program for each modelled implementation scenario.
The other scenarios were accelerations of slow, addingone (“annual” scenario) or two (“multiple” scenario) age cohorts every year. The fifth scenario (“5 year”) completed implementation within five years, commencing in 2015 (Table 1). Full implementation of all scenarios was defined as being achieved when all those aged 50 to 74-years were invited to screen on a biennial basis. Additional details about the criteria used can be found in Appendix 2 (online at mja.com.au).
Follow-up and surveillance
After a positive iFOBT result, a diagnostic colonoscopy was offered. If no adenomas were found during the colonoscopy, the individual was invited to re-screen with iFOBT after five years.20 Adenomas identified at colonoscopy were removed and the individual entered surveillance according to the NHMRC-endorsed guidelines.21 It was assumed that surveillance stopped at 75 years of age.
Test Characteristics
The test characteristics were adjusted to simulate iFOBT positivity and cancer detection rates observed in the Queensland Health Bowel Cancer Screening Program between August 2006 and December 2010.22, 23 This data set was chosen due to the unique and comprehensive nature of data collected by the Queensland program. Sensitivity and specificity were chosen so that simulated iFOBT positivity rates and positive predictive values for cancer matched the observed rates to within 0.1%. The sensitivity of iFOBT for cancer was split to account for the variance in test sensitivity at different time points before clinical diagnosis (shortly before and longer before). Additional assumptions of the MISCAN-Colon model can be found in Table 2.
Table 2. MISCAN-Colon Model Assumptions.
| Percentage % | |
|---|---|
| Sensitivity and specificity of iFOBT | |
| Specificity (per person) | 95.0 |
| Sensitivity diminutive adenomas (1-5mm) | 0.0 |
| Sensitivity small adenomas (6-9mm) | 9.0 |
| Sensitivity large adenomas (≥10mm) | 32.0 |
| Sensitivity cancer long before clinical diagnosis | 36.5 |
| Sensitivity cancer shortly before clinical diagnosis | 72.8 |
| Simulated (Observed) Positivity Rates and Positive predictive values of iFOBT | |
| Overall iFOBT positivity rate | 7.7 (7.7) |
| Positives without histo-pathologically confirmed adenomas or cancer | 47.4 (47.7) |
| Positives with adenomas | 48.2 (48.0) |
| Positives with advanced adenomas | 25.6 (26.0) |
| Positives with confirmed cancer | 4.4 (4.3) |
| Sensitivity of colonoscopy | |
| Adenoma 1-5mm | 75.0 |
| Adenoma 6-9mm | 85.0 |
| Adenoma 10+ mm | 95.0 |
| Preclinical cancer | 95.0 |
| Uptake of rescreening | |
| Previously attended | 80.0 |
| Previously not attended | 15.0 |
| Participation rates for follow-up colonoscopy and surveillance | |
| Colonoscopy follow-up after positive iFOBT (%) | 74.0 |
| Surveillance (%) | 80.0 |
iFOBT – immunochemical faecal occult blood test
Sensitivity in the table constitutes the probability of an individual lesion to bleed and be detected. The overall probability of a positive iFOBT in a person depends on the number and type of lesions present in this person, as well as his/her probability of bleeding for other causes than adenomas/cancer. This latter probability is equal to the lack-of-specificity.
Simulated positivity rate is the percentage of iFOBTs that were positive – that is blood was detected in the sample.
Positive predictive value is the percentage of positive iFOBTs that have a clinically significant finding (e.g. adenoma, advanced adenoma or cancer).
Participation
In each of the modelled implementation scenarios, thoseeligible were invited to participate in screening. For all scenarios, age specific participation rates for uptake of first iFOBT screening and diagnostic colonoscopy following positive iFOBT were simulated based on participation rates for July 2008-June 2011 reported in the NBCSP Monitoring Report for Phase 210 (Appendix 3 online at mja.com.au). Participation rates for ages between those reported were linearly extrapolated. As rescreening within the NBSCP did not commence until mid-2013, there is no data available on adherence with rescreening in the Australian setting. Therefore, we used UK data on follow-up screening rounds, which assumed that 80% of those who participated in the previous screening round would do so again24 and 15% of non-participants would take up the next offer to screen. Similarly, attendance at surveillance colonoscopy was assumed to be 80%, based on data from US clinical practice.25
Outcomes
For each scenario, the model estimated the number ofbowel cancer deaths prevented and colonoscopies required from 2006 to 2055. These results were then compared to the current and slow scenarios. The number of colonoscopies required each year per scenario includes colonoscopies that were a result of both a positive iFOBT and surveillance colonoscopy. Overall estimates, as well as estimates by calendar year and birth cohort, were calculated. Due to space limitations, only the results of three scenarios – current, slow and 5 year will be presented. The results for the other scenarios are available in Appendix 4 (online at mja.com.au).
Sensitivity Analyses
As there is no target participation rate for the NBCSP, we used the sensitivity analysis to explore the impact of a potential increase in screening participation rates to 60% once full implementation was achieved. This participation rate was chosen because, on balance, it appears to be achievable; both BreastScreen and the National Cervical Screening Program have previously achieved similar rates of participation1 and, bowel cancer screening has the potential to achieve higher rates of participation as iFOBT is a convenient test that can be easily performed in private.
Results
Bowel cancer deaths prevented
Without expansion, the current NBCSP would prevent 35,169bowel cancer deaths between 2015 and 2055. Completing implementation by 2035, as per the slow scenario, prevented 25,702 extra deaths between 2015 (the first year the scenarios diverge) and 2055 (Table 3, see Appendix 4 for results of all scenarios online at mja.com.au). Accelerating the implementation, as per the 5 year scenario, with full implementation by 2020, prevented up to 9167 additional bowel cancer deaths (34,869 more deaths prevented compared to the current scenario), clearly demonstrating that speed of implementation significantly influences the number of deaths prevented.
Table 3. Summary of projected major outcomes by modelled implementation scenario, 2015-2055.
| Current | Slow | 5 year | |
|---|---|---|---|
| Total number of deaths prevented | 35,169 | 60,871 | 70,038 |
| Average number of deaths prevented per year | 879 | 1522 | 1750 |
| Total number of colonoscopies per scenario | 2,468,481 | 4,411,844 | 5,113,260 |
| Number of colonoscopies per death prevented | 65 | 69 | 70 |
| Additional deaths prevented compared to Current | - | 25,702 | 34,869 |
| Average additional deaths prevented per year compared to Current | - | 643 | 872 |
| Additional colonoscopies compared to Current (%increase) | - | 1,943,363 (85%) | 2,644,779 (116%) |
| Additional deaths prevented compared to Slow | - | - | 9167 |
| Average additional deaths prevented per year compared to Slow | - | - | 229 |
| Additional colonoscopies compared to Slow (%increase) | - | - | 701,416 (17%) |
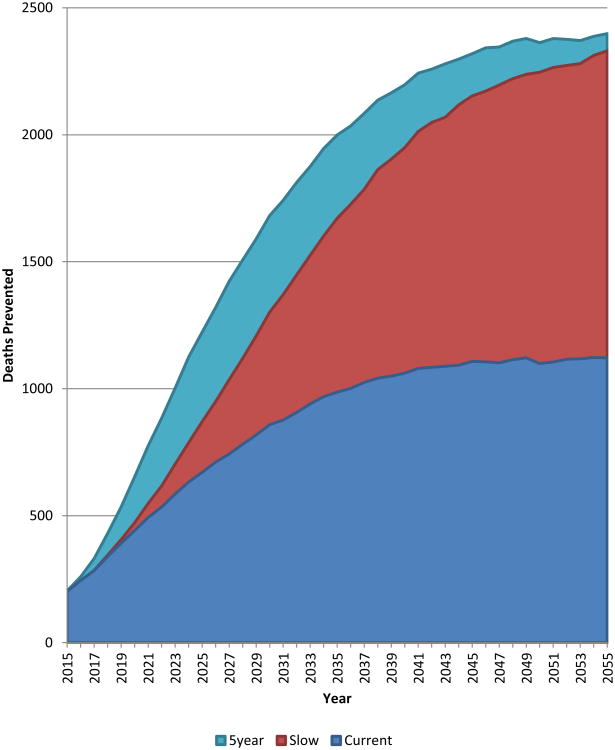
The annual distribution of deaths prevented when compared to the slow scenario showed that the difference in bowel cancer deaths between the scenarios reached its peak between 2026 and 2031, with almost 400 more deaths prevented in 2026 in the 5 year scenario (Figure 1). Although all scenarios simulate biennial screening (age 50-74) from 2035 onwards, the number of deaths prevented differs between scenarios until after 2055, with the 5 year scenario preventing the most deaths each year.
Figure 1. Deaths prevented over time by selected screening scenarios compared to slow, 2015-2055.
To ensure that no birth cohort was disadvantaged by the different scenarios, a comparison of deaths prevented by year of birth was conducted. In all cases, additional deaths were prevented in each birth cohort compared to current. This was most notable in the 5 year scenario.
Colonoscopy requirement
The scenarios with a faster implementation also requiredmore colonoscopies (Appendix 4 online at mja.com.au). To prevent the additional 25,702 deaths between the current and slow scenarios, 1,943,363 (85%) additional colonoscopies would be required. However, only a further 701,416 (17%) colonoscopies would be needed to prevent the additional 9167 deaths in the five year scenario. The overall number of colonoscopies required per death prevented is 65 in the current scenario, 69 in the slow scenario and 70 in the 5 year scenario, representing a good balance between burden and benefit.
Colonoscopy requirement over time (2015-2055) showed a distinct pattern related to the speed of implementation – the faster the implementation, the greater the increase in requirement. The greatest increase in colonoscopy requirement occurred during the implementation of each scenario. From 2014 to 2015, the absolute increase in colonoscopy requirement was largest, ranging from 6887 for the current scenario to 16,739 for the 5 year scenario. Over time, the absolute increase in colonoscopy requirement reduced for all scenarios, and at many time points, requirement was less than the previous year. There was a noticeable dip in the slow scenario in 2022 and 2030, when the 55- and 65-year-old cohorts were removed from the screening program.
Sensitivity Analyses
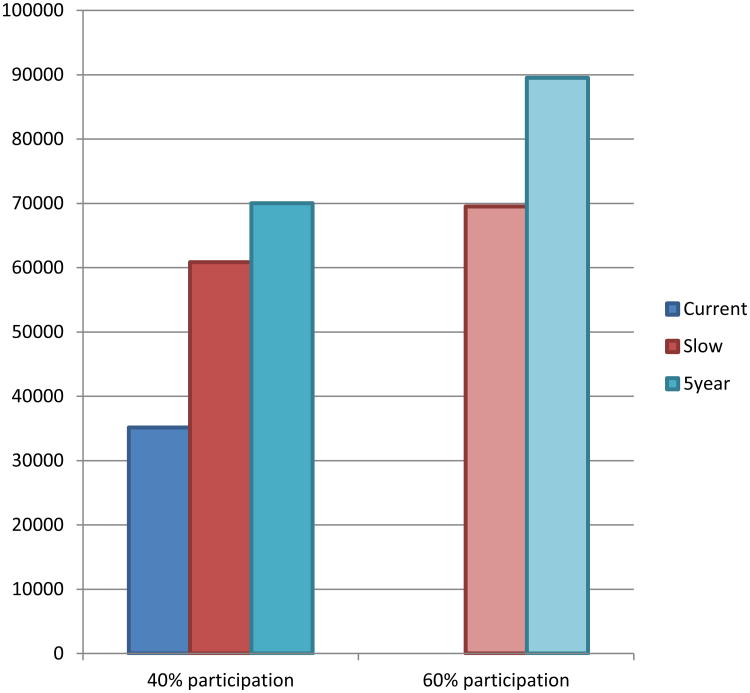
Once full biennial screening was achieved andparticipation increased to 60%, a substantial increase in deaths prevented was seen in all scenarios. This was most notable for the 5 year scenario where over 54,000 additional deaths were prevented between 2015 and 2055 compared to the current scenario (Figure 2). The number of required colonoscopies also increased for all scenarios, the most notable increase was in the 5 year scenario where approximately 4.35 million additional colonoscopies were required over the 40 year modelled period. Results for all scenarios can be found in Appendix 4 (online at mja.com.au).
Figure 2. Total deaths prevented by screening scenarios at 40% and 60% participation, 2015-2055.
Discussion
Our research clearly demonstrates that the choice of implementation scenario for the NBCSP significantly impacts the number of deaths prevented. Based on current participation rates in the NBCSP, the slow scenario prevents more than 25,000 additional bowel cancer deaths compared to the current scenario. Accelerating the implementation, as per the 5 year scenario, increases this number by approximately 40% to 34,869, or 100% more than the current situation. This equates to an annual average of 872 deaths prevented per year over 40 years (2015 to 2055), 229 per year more than the slow scenario.
The sensitivity analysis highlighted that, if, once fully implemented, participation reached 60%, there is potential to prevent an additional 20,000 deaths compared to the slow scenario, equating to approximately 500 additional deaths prevented per year over the 40 year period.
It is unsurprising that a faster implementation will result in greater numbers of deaths prevented. A strength of our research is that it quantified the impact of different implementation scenarios to establish their effect on deaths prevented. These results are conservative estimates as they are based on current rates of participation in the NBCSP which, while varying across age cohorts, remain collectively low. While acceptability of iFOBT has been reported to be as high as 83%26, low participation may, in part, be due to the lack of communication about the program and the difficulty in communicating a clear message about participation when eligibility is limited.27 The assumed 60% participation in the sensitivity analysis appears optimistic compared to the current rates of participation in bowel cancer screening, but it is an unrealistic target participation rate.28 The convenience of the iFOBT, coupled with the reported high levels of acceptability suggests iFOBT has the potential to reach more people, including those in regional and remote Australia. Given the current low participation rates, a well-planned, comprehensive and long-term social marketing campaign with support strategies including community and health professional education, will be required for the screening program to achieve an optimal level of participation – the importance of which cannot be underestimated.
Colonoscopy requirement also increased with all expansionscenarios (Appendix 4 online at mja.com.au). The calculations underpinning the modelled colonoscopy utilisation rely on national guidelines for screening and colonoscopy utilisation,9, 21 however as these assumptions do not necessarily reflect current practice, it was important to compare the increase in requirement resulting from a fully implemented screening program to current utilisation. Data from the Department of Human Services/Medicare Australia29 indicate that current colonoscopy utilisation (which is recognised as an underestimate of colonoscopy utilisation29, 30) is markedly higher than the modelled required utilisation, even for a program that is fully implemented within five years and achieves a participation rate of 60%. The NBCSP Quality Working Group reported that some colonoscopy utilisation in Australia is due to its overuse as a primary screening and surveillance tool.30 While this may have some impact on the mortality gains of the program, yield has been shown to be limited.31 A well-functioning program should encourage better compliance with NHMRC guidelines for screening and colonoscopic surveillance and, coupled with other appropriate strategies, should free up capacity for an increased number of NBCSP-related procedures, a notion supported by the NBCSP Quality Working Group.30 Recommendations for workforce, service capacity and program quality assurance were beyond the scope of this project but were investigated by the NBCSP Quality Working Group and a number of these recommendations have been, or are in the process of being, implemented.30
Our research considered the number of deaths prevented by bowel cancer screening and did not take into account disability or quality adjusted life years gained. It is not expected that this would greatly influence the results with respect to the speed of implementation.
While we did not investigate the cost-effectiveness of an expedited implementation, there is a strong body of evidence to show that bowel cancer screening is highly cost-effective, and in light of the increasing treatment costs, there is some suggestion that screening might even be cost-saving.14, 32, 33 This indicates that a faster rollout may actually be desirable from a cost-effectiveness perspective.
Implementing the NBCSP within a five year time frame from 2015 is not unrealistic, as both the national breast and cervical cancer screening programs became fully operational within five years.34 Moreover, while there is a substantial increase in colonoscopy requirement, within the context of current utilisation, the demand for colonoscopy due to overuse as a primary screening tool will likely decease.
Our analysis focused on the impact of accelerating the implementation of the NBCSP, comparing the current situation to the slow scenario with full implementation by 2035 and a 5 year scenario with full implementation by 2020. The findings strongly support an expedited implementation of the NBCSP, using the 5 year scenario as the benchmark, to prevent maximum loss of life from bowel cancer.
Supplementary Material
Acknowledgments
Bowel Cancer Education Coordinator position is funded by Western Australian Department of Health.
Footnotes
Competing interests: Competing interest: No relevant disclosures
Contributor Information
Dayna R Cenin, Email: dward@cancerwa.asn.au, Cancer Council WA, Perth, Western Australia, (08) 9388 4333.
James St John, Email: james.stjohn@bigpond.com, James.StJohn@cancervic.org.au, Cancer Council Victoria, Melbourne, Victoria, (03) 9635 5227.
Terry Slevin, Email: terry@cancerwa.asn.au, Cancer Council WA, Perth, Western Australia, (08) 9388 4333.
Melissa J Ledger, Email: mledger@cancerwa.asn.au, Cancer Council WA, Perth, Western Australia, (08) 9388 4333.
Iris Lansdorp-Vogelaar, Email: i.vogelaar@erasmusmc.nl, Department of Public Health, Erasmus MC, University Medical Centre, Rotterdam, The Netherlands, +31-10-7038454.
References
- 1.Australian Institute of Health and Welfare, Australasian Association of Cancer Registries. Canberra: AIHW; 2010. [accessed Mar 2012]. Cancer in Australia: an overview 2010. (AIHW Cancer series no. 60. Cat. no. CAN 56) http://www.aihw.gov.au/publication-detail/?id=6442472459. [Google Scholar]
- 2.Australian Institute of Health and Welfare. ACIM (Australian Cancer Incidence and Mortality) books. Bowel Cancer and All cancers. Canberra: AIHW; 2011. [accessed Oct 2012]. AIHW http://www.aihw.gov.au/acim-books/ [Google Scholar]
- 3.GLOBOCAN. Lyon: 2008. [accessed Mar 2013]. Cancer fact sheet. Colorectal Cancer Incidence, Mortality and Prevalence Worldwide in 2008. Summary. http://globocan.iarc.fr/ [Google Scholar]
- 4.Australian Population Health Development Principal Committee - Screening Subcommittee. Canberra: Australian Government; 2008. [accessed Mar 2012]. Population Based Screening Framework. http://www.cancerscreening.gov.au/internet/screening/publishing.nsf/Content/pop-based-screening-fwork/$File/screening-framework.pdf. [Google Scholar]
- 5.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472–1477. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 6.Kronborg O, Fenger C, Olsen J, et al. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348:1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 7.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood.Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328:1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 8.Towler B, Irwig L, Glasziou P, et al. A systematic review of the effects of screening for colorectal cancer using the faecal occult blood test, hemoccult. BMJ. 1998;317:559–565. doi: 10.1136/bmj.317.7158.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Australian Cancer Network Colorectal Cancer Guidelines Revision Committee. Sydney: The Cancer Council Australia and Australian Cancer Network; 2005. [accessed Mar 2012]. Clinical practice guidelines for the prevention, early detection and management of Colorectal Cancer. http://www.nhmrc.gov.au/guidelines/publications/cp106. [Google Scholar]
- 10.Australian Institute of Health and Welfare. Canberra: AIHW; 2012. [accessed Mar 2012]. National Bowel Cancer Screening Program monitoring report: phase 2, July 2008- June 2011. (AIHW Cancer Series No. 65 CAN 61) http://www.aihw.gov.au/publication-detail/?id=10737421408. [Google Scholar]
- 11.Australian Government. Canberra: Australian Government; 2012. [accessed Jun 2012]. Budget 2012-13 Part 2: Expense Measures. http://www.budget.gov.au/2012-13/content/bp2/html/bp2_expense-12.htm. [Google Scholar]
- 12.Australian Bureau of Statistics. Estimated Resident Population By Single Year Of Age, Australia. Canberra: ABS; 2012. [accessed Oct 2012]. 3101.0 - Australian Demographic Statistics - TABLE 59. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Jun%202012?OpenDocument. [Google Scholar]
- 13.Australian Bureau of Statistics. Canberra1: ABS; 2012. [accessed Oct 2012]. 3302.0 - Deaths, Australia, 2009. http://abs.gov.au/ausstats/abs@.nsf/Products/381E296AFC292B6CCA2577D60010A095?opendocument. [Google Scholar]
- 14.Tran B, Keating CL, Ananda SS, et al. Preliminary analysis of the cost-effectiveness of the National Bowel Cancer Screening Program: demonstrating the potential value of comprehensive real world data. Intern Med J. 2011;42:794–800. doi: 10.1111/j.1445-5994.2011.02585.x. [DOI] [PubMed] [Google Scholar]
- 15.Ananda SS, McLaughlin SJ, Chen F, et al. Initial impact of Australia's National Bowel Cancer Screening Program. Med J Aust. 2009;191:378–381. doi: 10.5694/j.1326-5377.2009.tb02843.x. [DOI] [PubMed] [Google Scholar]
- 16.Lansdorp-Vogelaar I, van Ballegooijen M, Boer R, et al. A novel hypothesis on the sensitivity of the fecal occult blood test. Cancer. 2009;115:2410–2419. doi: 10.1002/cncr.24256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loeve F, Boer R, van Ballegooijen M, et al. Final Report MISCAN-COLON microsimulation model for colorectal cancer: report to the National Cancer Institute Project No NO1-CN55186. Rotterdam: Department of Public Health Erasmus University; 1998. [Google Scholar]
- 18.Loeve F, Boer R, Zauber AG, et al. National Polyp Study data: evidence for regression of adenomas. Int J Cancer. 2004;111:633–639. doi: 10.1002/ijc.20277. [DOI] [PubMed] [Google Scholar]
- 19.Vogelaar I, van Ballegooijen M, Schrag D, et al. How much can current interventions reduce colorectal cancer mortality in the U.S.? Cancer. 2006;107:1624–1633. doi: 10.1002/cncr.22115. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health and Ageing. Canberra: Department of Health and Ageing; 2013. [accessed Jul 2013]. National Bowel Cancer Screening Program Participant Screening Program. http://www.cancerscreening.gov.au/internet/screening/publishing.nsf/Content/bw-part-scr-path. [Google Scholar]
- 21.Cancer Council Australia Colonoscopy Surveillance Working Party. Sydney: Cancer Council Australia; 2011. [accessed Oct 2012]. Clinical Practice Guidelines for Surveillance Colonoscopy – in adenoma follow-up; following curative resection of colorectal cancer; and for cancer surveillance in inflammatory bowel disease. http://www.nhmrc.gov.au/guidelines/publications/ext8. [Google Scholar]
- 22.Appleyard M, Grimpen F, Spucches C, et al. Participation in the national bowel cancer screening program and screening outcomes in Queensland. J Gastroenterol Hepatol. 2011;26(Suppl 4):29. [Google Scholar]
- 23.Queensland Health. Brisbane: Queensland Health; 2011. [accessed Oct 2012]. Queensland Bowel Cancer Screening Program: Statistical Report August 2006 – December 2010. http://www.health.qld.gov.au/bowelcancer/resources.asp. [Google Scholar]
- 24.Weller D, Coleman D, Robertson R, et al. The UK colorectal cancer screening pilot: results of the second round of screening in England. Br J Cancer. 2007;97:1601–1605. doi: 10.1038/sj.bjc.6604089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Colquhoun P, Chen HC, Kim JI, et al. High compliance rates observed for follow up colonoscopy post polypectomy are achievable outside of clinical trials: efficacy of polypectomy is not reduced by low compliance for follow up. Colorectal Dis. 2004;6:158–161. doi: 10.1111/j.1463-1318.2004.00585.x. [DOI] [PubMed] [Google Scholar]
- 26.Jalleh G, Donovan RJ, Lin C, et al. Beliefs about bowel cancer among the target group for the National Bowel Cancer Screening Program in Australia. Aust N Z J Public Health. 2010;34:187–192. doi: 10.1111/j.1753-6405.2010.00505.x. [DOI] [PubMed] [Google Scholar]
- 27.Olver IN, Young GP. The urgency of saving lives through bowel cancer screening. Med J Aust. 2012;196:490–491. doi: 10.5694/mja12.10476. [DOI] [PubMed] [Google Scholar]
- 28.Victorian Government Department of Human Services. Melbourne: Victorian Government Department of Human Services; 2008. [accessed May 2013]. Victoria's Cancer Action Plan 2008-2011. http://docs.health.vic.gov.au/docs/doc/Victorias-Cancer-Action-Plan-2008-2011-complete-document---Dec-2008. [Google Scholar]
- 29.Department of Human Services, Medicare Australia. Canberra: Department of Human Services; 2013. [accessed Aug 2013]. Requested Medicare items processed from January 1994 to June 2013. https://www.medicareaustralia.gov.au/cgi-bin/broker.exe?_PROGRAM=sas.mbs_item_standard_report.sas&_SERVICE=default&DRILL=ag&_DEBUG=0&group=32090%2C+32093&VAR=services&STAT=count&RPT_FMT=by+time+period+and+state&PTYPE=calyear&START_DT=199401&END_DT=201306. [Google Scholar]
- 30.The National Bowel Cancer Screening Program Quality Working Group. Canberra: Department of Health and Ageing; 2009. [accessed Apr 2012]. Improving Colonoscopy Services in Australia. http://www.cancerscreening.gov.au/internet/screening/publishing.nsf/Content/3FD09B61D2B4E286CA25770B007D1537/$File/Improving%20col%20serv0709.pdf. [Google Scholar]
- 31.Ee HC, Olynyk JK. Making sense of differing bowel cancer screening guidelines. Med J Aust. 2009;190:348–349. doi: 10.5694/j.1326-5377.2009.tb02444.x. [DOI] [PubMed] [Google Scholar]
- 32.Pignone MP, Flitcroft KL, Howard K, et al. Costs and cost-effectiveness of full implementation of a biennial faecal occult blood test screening program for bowel cancer in Australia. Med J Aust. 2011;194:180–185. doi: 10.5694/j.1326-5377.2011.tb03766.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bishop J, Glass P, Tracey E, et al. Cancer Institute NSW monograph. Eveleigh: Cancer Institute NSW; 2008. [accessed Mar 2012]. Health Economics Review of Bowel Cancer Screening in Australia. http://www.cancerinstitute.org.au/publications/i/health-economics-review-of-bowel-cancer-screening-in-australia-august-2008. [Google Scholar]
- 34.Australian Institute of Health and Welfare. Canberra: AIHW; 1998. [accessed Sep 2013]. Breast and Cervical Cancer Screening in Australia 1996–97. (AIHW Cancer Series. No 8. Cat. No. CAN 3) http://www.aihw.gov.au/publication-detail/?id=6442466999. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.