Abstract
A one-day satellite workshop was organized to coincide with the 17th International Symposium on Radiopharmaceutical Sciences held in Aachen, Germany, April 30-May 4, 2007. The workshop, “Production and application of ‘non-standard’ PET nuclides”, was held on Sunday April 29, 2007 at the Eurogress Aachen and was organized by J. Lewis, PhD, L. Tang, and M. Welch, PhD. The workshop was designed for the radiopharmaceutical community discussing the production, use and dissemination of the “non-standard” PET nuclides. The definition of “nonstandard” positron emission tomography (PET) nuclides included 45Ti, 60Cu, 61Cu, 64Cu, 66Ga, 72As, 74As, 76Br, 86Y, 89Zr, 94mTc and 124I. The workshop was supported by the grant Research Resource for Cancer Applications (R24 CA86307) funded by the National Cancer Institute at the National Institutes of Health. The workshop was attended by over 110 scientists and engineers from over 20 countries from all over the world and was designed with an open forum style to allow for discussions and interactions by all participants. All of the invited speakers were asked to make a contribution to this edition of the Quarterly Journal of Nuclear Medicine. The individual articles following this introduction are reviews of their area of expertise and the current state-of-the-art. This introduction briefly describes the role of the workshop, the aims and the general outcome. Also, the translation of these nuclides to the clinic, perhaps the most important goal of this work is discussed in this introductory article.
Keywords: Radiopharmaceuticals, Tomography, emission computed, Radioisotopes
Aims of the Workshop
The 17th International Symposium on Radiopharmaceutical Sciences was held in Aachen, Germany, April 30-May 4, 2007. Given the rapidly expanding interest and use of longer-lived positron emission tomography (PET) nuclides, the group from Washington University School of Medicine in St Louis organized a workshop highlighting the production and use of these longer-lived nuclides: The workshop, “Production and application of ‘non-standard’ PET nuclides”, was held on Sunday April 29, 2007 at the Eurogress Aachen and was organized by J. Lewis, PhD, L. Tang, and M. Welch, PhD. The planning of the workshop was undertaken with the staff at the Eurogress and with the very valuable help and assistance of Dr. H. H. Coenen. The workshop was supported by the grant Research Resource for Cancer Applications (R24 CA86307) funded by the National Cancer Institute at the National Institutes of Health with the help and approval of the Program Director at the NCI, Dr. B. Y. Croft. This financial support enabled the workshop to be held without charging a registration fee making it open to academic and industry-based scientists at all levels of their careers. The workshop was attended by over 110 scientists and engineers from over 20 countries from all over the world and was designed with an open forum style to allow for discussions and interactions by all attendees.
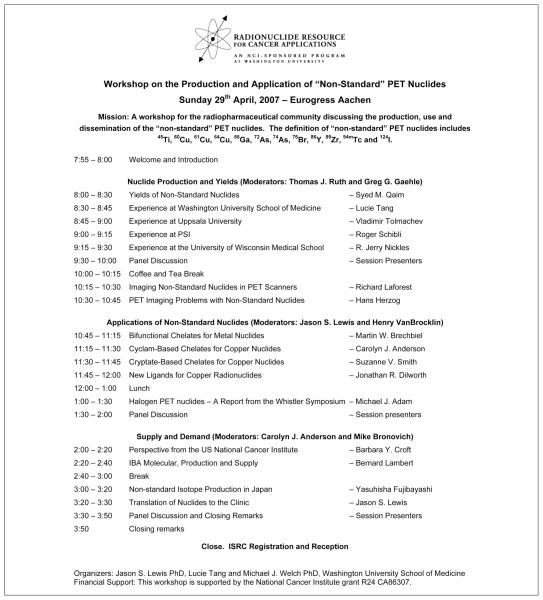
During the planning of this workshop it was decided to define the “non-standard” PET nuclides as 45Ti,60Cu, 61Cu, 64Cu, 66Ga, 72As, 74As, 76Br, 86Y, 89Zr, 94mTc and 124I, although it became evident during the workshop that there was varying levels of interest in each of these nuclides as well as in some that were not listed. The organizers did not include generator-produced positron-emitting radionuclides, such as 68Ga (from a 68Ge generator) and 62Cu (from a 62Zn generator), although the latter of these is discussed in the contribution by Fujibayashi et al. Shown in Figure 1 is the final schedule of the conference. The workshop was split into three distinct sections: “Nuclide production and yields”, “Applications of nuclides” and finally, “Supply and demand”. Two moderators were assigned for each section to help involve the audience and to stimulate discussion of the topics being presented. The primary objective of the meeting was to generate discussion on all the topics and to educate the participants in all aspects of non-standard PET nuclide technology. All of the invited speakers were asked to make a contribution to this edition of the Quarterly Journal of Nuclear Medicine. The individual articles following this introduction are reviews of the current state-of-the-art in the area of expertise of the speakers.
Figure 1.
Final schedule of the conference.
Nuclide production and yields
The main academic institutions responsible for the development of production methods were represented in the first session of the Workshop. The first speaker was Dr. S. Qaim who gave an outline of the latest physical characteristics of the non-standard nuclides including up-to-date decay data and production yields. This was felt to be of great importance given the vast difference in values often quoted in the literature by researchers, and it was felt that everyone should be quoting consistent values. This was then followed by a series of presentations given by scientists representing some of the academic institutions that lead in the production and supply of these nuclides. The emphasis was on production methods and yields from smaller in-house cyclotrons. This session was then closed with discussion on the image quality associated with the non-standard nuclides on commercial PET scanners. Since the decay schemes of the non-standard radionuclides can ultimately affect image resolution, Drs. Herzog and Laforest discussed state-of-the-art methods to generate the highest resolution images possible from these nuclides.
Applications of non-standard nuclides
The effective use of a non-standard nuclide often relies on its attachment to the targeting probe via a bifunctional chelator. The second session was, therefore, opened with a talk by Dr. M. Brechbiel, who reviewed many of the chemical and physical properties required for an efficient bifunctional chelator. A series of requirements were presented with reference to known chelators, with an open question to the audience of when is a chelator ‘good enough’ for a given application. Given the simple fact that 64Cu is currently the most widely used metallic non-standard nuclide, it was felt to be important to focus on which chelates are currently available for use with this nuclide. Talks by Drs. Anderson, Smith and Dilworth presented and compared the current state-of-the-art in copper chelate chemistry. Dr. Adam who has been the organizer of a series of meetings on radiohalogens presented the current status of labeling chemistry using positron-emitting halogen radionuclides.
Supply and demand
It was evident from the workshop that the majority of non-standard nuclide development has been undertaken by academic institutions. Within the United States, Washington University School of Medicine, University of Wisconsin Medical Physics Department, Memorial Sloan Kettering Cancer Center and the National Institutes of Health intramural program have been the leaders in production of the non-standard radionuclides. In Japan, Fukui Medical School has taken the lead; in Europe, Uppsala University (Sweden), Research Center Jülich (Germany) and PSI (Switzerland) are the main contributors to the production of the non-standard nuclides. However, multiple academic institutions, in Europe, the United States, Asia and Australia are actively participating in the use of these nuclides, either in characterizing the physical properties and the image quality of the nuclide in commercial PET scanners, the development of chelates or producing new radiopharmaceuticals based on these longer-lived nuclides.
Although the use of these nuclides has grown exponentially over the last decade, academic institutions have largely been responsible for their production and supply. Moreover, the vast majority of radio-pharmaceutical development based on these nuclides has also been in academic institutions. It has now reached the point where the interest in these nuclides and agents requires wider and consistent availability in their supply to meet the increasing demands. In response to this, the majority of the cyclotron-producing companies are now interested in providing solid targetry systems with their cyclotrons. Dr. B. Lambert represented a company’s point of view in the supply of these isotopes. He presented the goals and technology of IBA Molecular and discussed their compact solid target irradiation system (Nirta® Solid), which is easy to install on existing cyclotrons and ideal for the production of non conventional PET radionuclides based on solid target technology. The expansion of commercially available systems that can be placed on existing equipment or supplied with new cyclotrons was met with enthusiasm by the audience. The general feeling was that the community could not rely on a limited number of academic institutions to supply the increasing demand of these nuclides and that the ability to either make them for themselves, or purchase them commercially was very important. There is now a number of other industrial companies, such as MDS Nordion (Canada), ACOM (Italy) and Trace Life Sciences (USA), IBA Molecular (USA and Europe), and IsoTrace (USA), which are selling some of the non-standard nuclides and are, therefore, helping to meet the demands of the market.
Translation of the non-standard nuclides to the clinic for human studies
Perhaps, the ultimate goal of this area of research is the translation of these nuclides into the clinical arena. The workshop was ended by a discussion by Dr. J. Lewis on the translation of these nuclides, the obstacles to translation and examples of some successes. A number of these examples were supplied by researchers prior to publication and we wish to acknowledge their helpful contributions. It is apparent there have been very successful translations of 124I and 64Cu agents (incorporated into both small molecules and larger biomolecules) to the clinic and human imaging studies. There are now agents approved for use in the USA and Europe, but there are major issues, such as nuclide supply, and financial and regulatory hurdles, still slowing down the clinical translation of new agents. There are a number of companies that are supplying nuclides helping to overcome supply limitations, and as discussed by Dr. Croft, funding assistance can be sought from sources such as the DCIDE program. Regulatory approval remains somewhat of a hurdle, and differs greater between countries. To help in getting approval for new agents within the USA, the United States Food and Drug Administration (US FDA) have initiated the exploratory investigational new drug (EIND)1 mechanism that could help simplify the approval process for pilot human studies.
Historically, 64Cu (as 64CuCl2) has been administered to humans with Wilson’s disease and in patients with primary biliary cirrhosis.2 A summary of the reports in this area are reviewed in detail by Linder.2 This, however, was done to simply monitor changes in liver function and did not involve imaging and were often done prior to the development of PET technology. More recently, with support from the DCIDE program at the National Cancer Institute at the United States National Institutes of Health to generate the pharmacology and toxicity data for Cu-ATSM, the FDA approved an investigational pilot study in 2006 (IND 62,675) examining the uptake and kinetics of [64Cu]ATSM in women with cancer of the uterine cervix. This was done to compare the image quality of [64Cu]ATSM against [60Cu]ATSM, following previous studies where [60Cu]ATSM uptake in tumors was correlated with the response of the tumor to conventional therapies.3, 4 It is anticipated that this pilot IND study will lead to a multicenter trial within the United States starting in November 2007. With the current production of 64Cu in other countries, it is likely that additional clinical trials with [64Cu]ATSM will be initiated soon in England, Italy and Japan.
Other examples presented of clinically-tested agents with 64Cu included work by ACOM SpA (Advanced Center Oncology Macerata, Italy) and their collaborating medical institutions who supplied data on their clinical imaging studies with [64Cu]asparagine for imaging patients with glioblastoma and [64Cu]TETA-octreotide for imaging neuroendocrine tumors. The work with [64Cu]TETA-octreotide follows on from the original work of Anderson et al., published in 2001, the first report of a 64Cu-labeled peptide in humans.5 In this original study, 8 patients with a history of neuroendocrine tumors (5 patients with carcinoid tumors and 3 patients with islet cell tumors) were imaged by conventional scintigraphy with both [111In]DTPA-OC and by PET imaging with [64Cu]TETA-octreotide. The high lesion-detection, sensitivity, as well as favorable dosimetry and pharmacokinetics of [64Cu]TETA-octreotide indicated that it is a promising radiopharmaceutical for PET imaging of patients with neuroendocrine tumors. There has been one published trial utilizing 64Cu-labeled to an antibody.6 Copper-64-TETA-1A3 was evaluated in 36 patients with suspected advanced primary or metastatic colorectal cancer. In 29 patients, one or more tumor sites (n=56) were proven, in 5 patients the absence of active tumor was confirmed and in the remaining 2, tumor status had not yet been confirmed at the time of publication. The use of the F(ab’)2 of this antibody has been published in abstract form.7 On the whole this Phase I/II results confirmed that PET with 64Cu-radiolabeled MAbs may have important applications in clinical oncology, particularly for detecting smaller tumor foci and for determining accurate dosimetry for therapy, using either 64Cu or 67Cu agents. Several reports of 67Cu-labeled antibodies in humans have been published.8–13
Of the radiohalogens, both 76Br and 124I have been administered to humans. Dupont et al. studied [76Br]4-bromodexetimide (BDEX) in patients with medial temporal lobe epilepsy focusing on the regional distribution and binding kinetics of the 76Br-agent.14 This preliminary study suggested that [76Br]BDEX is a suitable radiotracer for studies in humans and that further studies are required to investigate the potential value of [76Br]BDEX PET in other neurological disorders with muscarinic disturbances. This study has laid the foundation for other brominated compounds to be translated to the clinic; these could also include analogs to previously studied 77Br compounds, such as the estrogen-receptor-binding radiopharmaceutical, 16-a-[77Br]bromoestradiol, which was used to imaging patients with mammary carcinoma.15
Iodine-124 has been used for labeling both small and large molecules for use in humans. Iodine-124, in the simple chemical form of Na124I, has been used for the diagnosis of thyroid disease and for evaluating the spread of metastatic thyroid carcinoma.16, 17 One study reported the distribution of 124I in 64 patients with a variety of thyroid conditions.18 A number of small molecules have been labeled with 124I as analogs of 131I compounds; for example, patients designated to receive [131I]meta-iodobenzylguanadine (mIBG) for the treatment of neural crest tumors have been scanned with [124I]mIBG.19 Another small molecule labeled with 124I, 124I-labelled 2′-fluoro-2′-deoxy-1b-D-arabino-furanosyl-5-iodo-uracil ([124I]FIAU) is perhaps the most widely studied. The use of 124I, a specific marker substrate for gene expression of HSV-1-tk, was used to identify the location, magnitude, and extent of vector-mediated HSV-1-tk gene expression in a phase I/II clinical trial of gene therapy for recurrent glioblastoma in 5 patients.20 The expression of this exogenous gene introduced by gene therapy into patients with gliomas was monitored non-invasively by PET. Dr. M. Pomper of John Hopkins Medical Institutions kindly supplied images and data on their translation of [124I]FIAU to the clinic for the imaging of musculoskeletal bacterial infections. Although this clinical data has not been published the exciting potential of this technology was evident and holds exceptional promise for future applications. Another iodinated small molecule, [124I]iododeoxyuridine ([124I]IUdR) has been used to measure the proliferative activity of tumors in 20 patients with brain tumors, including meningiomas and gliomas.21
Iodine-124 has perhaps it greatest clinical applicability in the labeling of large biomolecules such as antibodies and there are a quite a few examples of this within the literature.22–24 For example, in 2002, Jayson et al., developed HuMV833, a humanized version of a mouse monoclonal anti-VEGF antibody (MV833) and investigated the distribution and biologic effects of [124I]HuMV833 in 20 patients in a phase I trial.23 More recently, in 2007, Divgi et al., undertook a Phase 1 study with 124I-labelled antibody chimeric G250 [124I]cG250 in 26 patients with renal masses.22 It was shown that [124I]cG250 could identify clear-cell renal carcinoma where 15 of 16 clear-cell carcinomas were identified accurately by antibody PET, and all 9 non-clear-cell renal masses were negative for the tracer.
Finally, there have been reports of the use of 86Y in humans. Yttrium-90 is used as a radiotherapeutic nuclide, but, because it is a pure β-emitter, data on the pharmacokinetics and radiation doses to primary tumors, metastases and unaffected organs are lacking. In 1996, Rösch et al., compared the properties of two different 86Y complexes-[86Y]citrate and [86Y]ethylene diamine tetramethylene phosphonate (EDTMP), in 10 patients with prostatic cancer who had developed multiple bone metastasis.25 The 86Y PET images from these compounds provided quantitative information applicable to the clinical use of 90Y. This method has also been useful in the design of other 90Y radiopharmaceuticals and for planning radiotherapy dosages. For example, pre-therapeutic dosimetry and biodistribution of [90Y]DOTA-Phe1-Tyr3-octreotide has been measured with [86Y]DOTA-Phe1-Tyr3-octreotide (SMT487) in patients with metastatic carcinoid tumors (n=3) and advanced neuroendocrine tumors (n=24).26, 27
Clearly, there is huge potential for translating nonstandard nuclide-based radiopharmaceuticals to the clinic, but hurdles do exist that must be overcome. Also, despite the interest in the translation of new agents to the clinic the literature is still lacking in examples of agents that have been approved. To help achieve translation of more agents, researchers must publish their data and images in the literature to motivate other scientists to discover the huge potential of these PET radiopharmaceuticals.
Acknowledgments
Funding.—This meeting was supported by a grant from the National Institutes of Health/National Cancer Institute grant R24 CA86307.
We wish to acknowledge the help of the staff at the Eurogress, Aachen and Dr. H. H. Coenen.
References
- 1.Guidance for industry, investigators, and reviewers exploratory IND studies [homepage on the Internet] Rockville, MD, USA: U.S. Food and Drug Administration; Available from: http://www.fda.gov/CDER/guidance/7086fnl.htm. [Google Scholar]
- 2.Linder MC. Biochemistry of copper. New York: Plenum Press; 1991. [Google Scholar]
- 3.Dehdashti F, Grigsby PW, Mintun MA, Lewis JS, Siegel BA, Welch MJ. Assessing tumor hypoxia in cervical cancer by positron emission tomography with 60Cu-ATSM: relationship to therapeutic response-a preliminary report. Int J Radiat Oncol Biol Phys. 2003;55:1233–8. doi: 10.1016/s0360-3016(02)04477-2. [DOI] [PubMed] [Google Scholar]
- 4.Dehdashti F, Mintun MA, Lewis JS, Bradley J, Govindan R, Laforest R, et al. In vivo assesment of tumor hypoxia in lung cancer with 60Cu-ATSM. Eur J Nucl Med Mol Imaging. 2003;30:844–50. doi: 10.1007/s00259-003-1130-4. [DOI] [PubMed] [Google Scholar]
- 5.Anderson CJ, Dehdashti F, Cutler PD, Schwarz SW, Laforest R, Bass LA, et al. 64Cu-TETA-octreotide as PET imaging agent for patients with neuroendocrine tumors. J Nucl Med. 2001;42:213–21. [PubMed] [Google Scholar]
- 6.Philpott GW, Schwarz SW, Anderson CJ, Dehdashti F, Connett JM, Zinn KR, et al. RadioimmunoPET: detection of colorectal carcinoma with positron-emitting copper-64-labeled monoclonal antibody. J Nucl Med. 1995;36:1818–24. [PubMed] [Google Scholar]
- 7.Philpott GW, Dehdashti F, Schwarz SW, Connett JM, Anderson CJ, Zinn KR, et al. RadioimmunoPET (MAb-PET) with Cu-64-labeled monoclonal antibody (MAb 1A3) fragments [F(ab’)2] in patients with colorectal cancers. J Nucl Med. 1995;36:9P. [PubMed] [Google Scholar]
- 8.DeNardo GL, DeNardo SJ, Kukis DL, O’Donnell RT, Shen S, Goldstein DS, et al. Maximum tolerated dose of 67Cu-2IT-BAT-LYM-1 for fractionated radioimmunotherapy of non-Hodgkin’s lymphoma: a pilot study. Anticancer Res. 1998;18:2779–88. [PubMed] [Google Scholar]
- 9.DeNardo GL, DeNardo SJ, Meares CF, Kukis D, Diril H, McCall MJ, et al. Pharmacokinetics of copper-67 conjugated Lym-1, a potential therapeutic radioimmunoconjugate, in mice and in patients with lymphoma. Antibodies Immunconj Radiopharm. 1991;4:777–85. [Google Scholar]
- 10.DeNardo GL, Kukis DL, Shen S, DeNardo DA, Meares CF, DeNardo SJ. 67Cu- versus 131I-labeled Lym-1 antibody: comparative pharmacokinetics and dosimetry in patients with non-Hodgkin’s lymphoma. Clin Cancer Res. 1999;5:533–41. [PubMed] [Google Scholar]
- 11.DeNardo S, DeNardo G, Kukis D, Mausner L, Moody D, Meares C. Pharmacology of Cu-67-TETA-Lym-1 antibody in patients with B cell lymphoma. Antibody Immunoconj Radiopharms. 1991;4:36. [Google Scholar]
- 12.O’Donnell RT, DeNardo GL, Kukis DL, Lamborn KR, Shen S, Yuan A, et al. A clinical trial of radioimmunotherapy with 67Cu-2IT-Lym-1 for non-Hodgkin’s lymphoma. J Nucl Med. 1999;40:2014–20. [PubMed] [Google Scholar]
- 13.Novak-Hofer I, Schubiger PA. Copper-67 as a therapeutic nuclide for radioimmunotherapy. Eur J Nucl Med. 2002;29:821–30. doi: 10.1007/s00259-001-0724-y. [DOI] [PubMed] [Google Scholar]
- 14.Dupont S, Semah F, Loc’h C, Strijckmans V, Baulac M, Samson Y, et al. In vivo imaging of muscarinic cholinergic receptors in temporal lobe epilepsy with a new PET tracer: [76Br]4-bromodexetimide. J Nucl Med. 1999;40:935–41. [PubMed] [Google Scholar]
- 15.McElvany KD, Katzenellenbogen JA, Shafer KE, Siegel BA, Senderoff SG, Welch MJ. 16 alpha-[77Br]bromoestradiol: dosimetry and preliminary clinical studies. J Nucl Med. 1982;23:425–30. [PubMed] [Google Scholar]
- 16.Eschmann SM, Reischl G, Bilger K, Kupferschläger J, Thelen MH, Dohmen BM, et al. Evaluation of dosimetry of radioiodine therapy in benign and malignant thyroid disorders by means of iodine-124 and PET. Eur J Nucl Med Mol Imaging. 2002;29:760–7. doi: 10.1007/s00259-002-0775-8. [DOI] [PubMed] [Google Scholar]
- 17.Freudenberg LS, Antoch G, Görges R, Knust J, Pink R, Jentzen W, et al. Combined PET/CT with iodine-124 in diagnosis of spread metastatic thyroid carcinoma: a case report. Eur Radiology. 2003;13:L19–L23. doi: 10.1007/s00330-003-1884-x. [DOI] [PubMed] [Google Scholar]
- 18.Frey P, Townsend D, Flattet A, De Gautard R, Widgren S, Jeavons A, et al. Tomographic imaging of the human thyroid using 124I. J Clin Endocrin Metab. 1986;63:918–27. doi: 10.1210/jcem-63-4-918. [DOI] [PubMed] [Google Scholar]
- 19.Ott RJ, Tait D, Flower MA, Babich JW, Lambrecht RM. Treatment planning for 131I-mIBG radiotherapy of neural crest tumours using 124I-mIBG positron emission tomography. Br J Radiol. 1992;65:787–91. doi: 10.1259/0007-1285-65-777-787. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs A, Voges J, Reszka R, Lercher M, Gossmann A, Kracht L, et al. Positron-emission tomography of vector-mediated gene expression in gene therapy for gliomas. Lancet Oncol. 2001;358:729–29. doi: 10.1016/s0140-6736(01)05904-9. [DOI] [PubMed] [Google Scholar]
- 21.Blasberg RG, Roelcke U, Weinreich R, Beattie B, von Ammon K, Yonekawa Y, et al. Imaging brain tumor proliferative activity with [124I]iododeoxyuridine. Cancer Res. 2000;60:624–35. [PubMed] [Google Scholar]
- 22.Divgi CR, Pandit-Taskar N, Jungbluth AA, Reuter VE, Gonen M, Ruan S, et al. Preoperative characterisation of clear-cell renal carcinoma using iodine-124-labelled antibody chimeric G250 (124I-cG250) and PET in patients with renal masses: a phase I trial. Lancet Oncol. 2007;8:304–10. doi: 10.1016/S1470-2045(07)70044-X. [DOI] [PubMed] [Google Scholar]
- 23.Jayson GC, Zweit J, Jackson A, Mulatero C, Julyan P, Ranson M, et al. Molecular imaging and biological evaluation of HuMV833 anti-VEGF antibody: implications for trial design of antiangiogenic antibodies. J Natl Cancer Inst. 2002;94:1484–93. doi: 10.1093/jnci/94.19.1484. [DOI] [PubMed] [Google Scholar]
- 24.Larson SM, Pentlow KS, Volkow ND, Wolf AP, Finn RD, Lambrecht RM, et al. PET scanning of iodine-124-3F9 as an approach to tumor dosimetry during treatment planning for radioimmunotherapy in a child with neuroblastoma. J Nucl Med. 1992;33:2020–3. [PubMed] [Google Scholar]
- 25.Rösch F, Herzog H, Plag C, Neumaier B, Braun U, Müller-Gärtnere HW, et al. Radiation doses of yttrium-90 citrate and yttrium-90 EDTMP as determined via analogous yttrium-86 complexes and positron emission tomography. Eur J Nucl Med. 1996;23:958–66. doi: 10.1007/BF01084371. [DOI] [PubMed] [Google Scholar]
- 26.Helisch A, Förster GJ, Reber H, Buchholz HG, Arnold R, Göke B, et al. Pre-therapeutic dosimetry and biodistribution of 86Y-DOTA-Phe1-Tyr3-octreotide versus 111In-pentetreotide in patients with advanced neuroendocrine tumours. Eur J Nucl Med Mol Imaging. 2004;31:1561–6. doi: 10.1007/s00259-004-1561-6. [DOI] [PubMed] [Google Scholar]
- 27.Jamar F, Barone R, Mathieu I, Walrand S, Labar D, Carlier P, et al. 86Y-DOTA0-d-Phe1-Tyr3-octreotide (SMT487)—a phase 1 clinical study: pharmacokinetics, biodistribution and renal protective effect of different regimens of amino acid co-infusion. Eur J Nucl Med Mol Imaging. 2003;30:510–8. doi: 10.1007/s00259-003-1117-1. [DOI] [PubMed] [Google Scholar]