Abstract
Background
There are many plating systems available for treating distal radius fractures (DRFs), and the decision of which type to use can be difficult. This is a prospective cohort study that compares outcomes of two commonly used fixation systems: fragment specific fixation (FSF) and a fixed-angle volar locking plate system (VLPS).
Methods
Two cohorts of consecutive DRFs were prospectively evaluated. The first cohort was treated with FSF and the second with a VLPS. Radiographic, functional, and patient-rated outcomes (MHQ) were collected immediately post-operatively, and at six and twelve months post-operatively. Complications were recorded and graded by severity.
Results
Fourteen DRFs treated with FSF and eighty-five DRFs treated with the VLPS were enrolled. At final follow-up, radial inclination was similar in both cohorts (23° vs. 25°); however, volar tilt was worse in the FSF cohort (−10° vs. 10°, p<0.05). Additionally, the majority of the FSF cohort demonstrated a loss of relative radial length (63% of cohort with positive ulnar variance). Grip strength, pinch strength, MHQ scores, and most ROM measurements were superior in the VLPS cohort at 6 months, although not all differences were statistically significant. By 12 months the differences in functional and patient-rated outcomes were smaller, suggesting that the FSF cohort tended to reach the outcomes of the VLPS cohort over time. Complications requiring re-operation were higher in the FSF cohort (p<0.05).
Conclusions
The VLPS results in more stable fixation and better objective and subjective outcomes early in the post-operative period. It has fewer complications requiring re-operation than FSF.
Keywords: distal radius, fracture, open reduction internal fixation, ORIF, outcomes
Distal radius fractures (DRFs) are common injuries1 that will occur more frequently as the U.S. population ages.2 Successful treatment requires stable reduction followed by fracture healing and rehabilitation. Although in some cases DRFs can be treated non-operatively, open reduction and internal fixation (ORIF) is often required.3
Numerous fixation methods have been proposed for treating DRFs. In addition, new fixation systems continually become available, and existing ones are frequently modified. Kirschner wires, tension band wires, compression screws, intramedullary nails, volar plates, dorsal plates, ulnar and radial buttress plates, clamps, and various small T- or L-shaped plates may all be used.4 No single method is appropriate for all fractures, and the decision of which fixation system to use depends on factors such as fracture anatomy, bone quality, patient factors (such as other injuries and activity level), surgeon experience, and hardware availability.
The purpose of this comparative prospective cohort study is to evaluate outcomes of distal radius fracture ORIF using two common plating systems: 1) the volar locking plating system (VLPS), and 2) fragment specific fixation (FSF).
Materials and Methods
From 2001 through August 2003, the senior author (KCC) used various fixation systems including FSF, percutaneous pinning, and external fixation to treat unstable DRFs. Because FSF is most applicable to comminuted intra-articular fractures, the majority of fractures treated with FSF during this period were of this type. Other methods of fixation such as percutaneous pinning were used primarily to treat extra-articular and simple intra-articular fractures that required surgery. Outcomes data were prospectively collected from patients who were treated with FSF during this time period.
After the introduction of the VLPS, the senior author and his team switched exclusively to the VLPS because of the technical ease associated with this system. A prospective outcomes study was performed from September 2003 to July 2005 to evaluate the VLPS,5 and the VLPS cohort in this study was used for comparison.
Indications for ORIF remained consistent during the enrollment of both cohorts, and included radial height of less than 10 mm, radial inclination of less than 15 degrees, dorsal tilt of greater than 10 degrees (loss of volar tilt greater than 21 degrees), or an intra-articular step-off of 2 mm or greater. Patients with bilateral DRFs were excluded because of the confounding effect of bilateral injuries in the outcomes assessment. Patients with severe multi-system injuries were also excluded. All patients gave written informed consent for participation in the study, and all aspects of the study were approved by the Institutional Review Board of the University of Michigan Medical Center.
Radiographic Measurements
All patients underwent three-view x-rays of the injured wrist pre- and immediately postoperatively, and at six and twelve months post-operatively. Radial inclination and volar tilt were measured, and the absolute degree of deviation from accepted normal values (22 and 11 degrees respectively)6–8 was calculated. The absolute degree of deviation from normal values was used for statistical comparison, because simple mean values for radial inclination and volar tilt can be misleading. For example, two radial inclinations of 20 degrees and 24 degrees would have the same mean (22 degrees) as two radial inclinations of 10 degrees and 34 degrees. However, the mean absolute deviation from normal would be quite different in the two groups (2 degrees and 12 degrees respectively). Ulnar variance was used as a measure of relative radial length.
Objective Functional Measurements
Active range of motion (ROM) measurements including flexion-extension, radial-ulnar deviation, and forearm rotation were measured at six months and one year post-operatively. Grip strength, using a Jamar dynamometer (Bolingbrook, IL), and lateral pinch strength, using a B & L Engineering pinch gauge (Tustin, CA), were measured at the same intervals.
Subjective Outcomes Measurements
The Michigan Hand Outcomes Questionnaire (MHQ) was administered at six months and one year post-operatively. The MHQ is a self-administered test that was developed at the University of Michigan by the senior author (KCC). It is a validated instrument that measures health status domains important to patients with hand disorders, including 1) overall hand function, 2) activities of daily living, 3) pain, 4) work performance, 5) aesthetics, and 6) patient satisfaction. Its validity and responsiveness have been demonstrated for a number of common hand disorders,9–13 including distal radius fractures.14 More than 50 US and international publications have used the MHQ as the predominant outcomes tool for measuring hand impairment.15
Complications
Complications were recorded and categorized as major or minor. Major complications were those that required either hospitalization or re-operation. Minor complications were those that were treated non-operatively on an outpatient basis.
Statistical Analysis
Inter-cohort comparisons of continuous variable radiographic measurements (radial inclination and volar tilt) were made using the Wilcoxon two-sample test. Fisher’s exact test was used to compare the distribution of ordinal and categorical measurements such as ulnar variance (negative, neutral, or positive) and complications (minor or major). An inter-cohort comparison of the radiographic outcomes of all fractures regardless of AO-type was performed. In order to minimize the influence of fracture severity (AO-type) on the results, an inter-cohort comparison of only same AO-type fractures was also performed. Because of the low numbers of AO-type A and B fractures in the FSF cohort, the comparison of same-type fractures included only type C fractures.
Objective functional and patient-rated outcomes were evaluated using regression analysis. An effort was made to minimize the influence of patient age and fracture severity (AO-type) on the results. A matching code was created for every patient that included the patient’s 10-year age bracket and fracture AO-type. VLPS patients were then many-to-one matched with FSF patients with the same matching code. Treating the matched group codes as a clustering variable, a Generalized Estimating Equations (GEE) regression model was created that predicted the mean of each outcome (dependent variable) for each treatment group (FSF or VLPS, independent variable).
Fragment Specific Fixation
FSF (Trimed®) was performed primarily using two plates: a radial column pin plate and an ulnar column pin plate. The radial column pin plate (Figure 1) is contoured to fit the radial border of the distal radius, and the ulnar column pin plate (Figure 1) is contoured to fit the dorsal aspect of the central (intermediate) column. Both pin plates use screw fixation proximal to the fracture, and Kirschner-wire fixation of the distal fragments. Either one or both of the pin plates were used, depending on fracture anatomy (Figure 2). In addition, there are numerous wire forms (buttress pin clamps, buttress pins) that were used as needed to stabilize specific smaller fragments (Figure 3).16–18 It should be noted that the most recent generation of the FSF system now also includes a volar plate that is similar to the plate used in the VLPS cohort.
Figure 1.
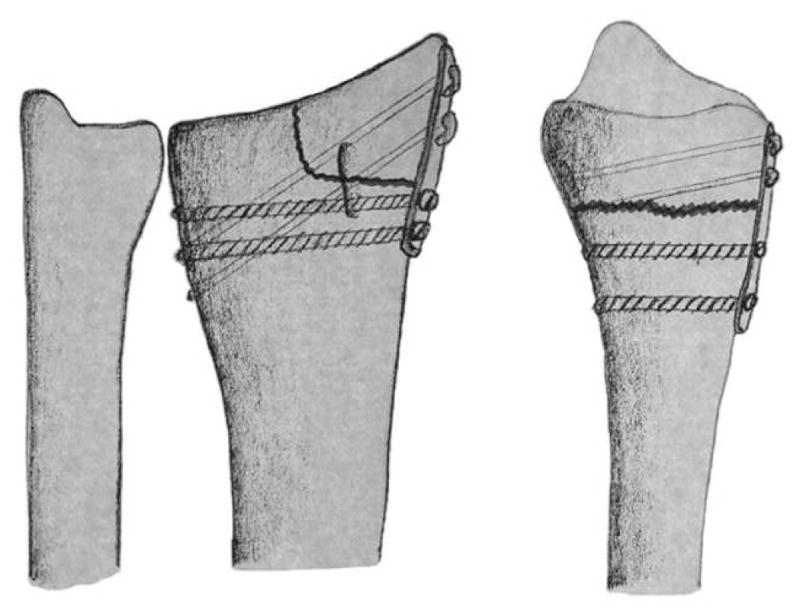
Radial and ulnar pin plates augmented with K-wires and proximal screws for fixation of radial and ulnar column fractures.
Figure 2.

Pre-operative views above show the fracture through the neck of the ulna and the ulnar translation of the distal radius fragment. Post-operative views below show contour plate fixation of the ulnar fracture, and 90-90 degree angle fixation of radial and ulnar columns of the distal radius.
Figure 3.

The sequential placement of the wire-form to support a depressed articular distal radius fracture.
The surgical approach for the radial pin plate consists of a 5-cm longitudinal incision over the radial styloid. Care is taken to protect the sensory branches of the radial nerve. The first extensor compartment is dissected off the radius, and the brachioradialis insertion is incised. After fracture reduction, the radial pin plate is applied. Two 2.7 mm bicortical screws are used to secure the pin plate proximal to the fracture. Fixation of the distal fragment is performed with two Kirschner wires.16–18
The surgical approach for the ulnar pin plate consists of a 5-cm longitudinal incision over the fourth extensor compartment. The fourth compartment extensor tendons are retracted ulnarly, and dissection is carried down to the dorsal aspect of the distal radius. The fracture is reduced and the ulnar pin plate is applied to the central (intermediate) column. The plate is secured with two 2.7 mm bicortical screws proximal to the fracture. Fixation of the distal fragment is performed with two Kirschner wires.16–18
Additional fixation of small fragments with the wire forms can be performed through these two exposures. Fluoroscopy is used to confirm fracture reduction and plate position prior to closing the incisions.
Volar Locking Plating System
The VLPS used in this study (Hand Innovations DVR™) is a T-shaped, anatomically contoured plate that uses non-locking screws in the stem proximal to the fracture, with two rows of intersecting fixed-angle locking pegs or screws for fixation of the distal fracture fragment (Figure 4). The surgical technique has been presented previously by the senior author (KCC).19 A 10-cm longitudinal incision is made over the flexor carpi radialis (FCR). The FCR sheath is opened and the tendon is retracted ulnarly. The floor of the tendon sheath is sharply opened exposing the flexor pollicis longus (FPL). The FPL is mobilized bluntly, exposing the pronator quadratus (PQ). The PQ is incised along its radial and distal edges and is elevated ulnarly, exposing the fracture. The brachioradialis insertion is released and the fracture is reduced. The plate is placed across the fracture and secured proximally with non-locking cortical screws and distally with smooth locking pegs. Fluoroscopy is used to confirm placement. The pronator quadratus is repaired and the incision is closed.
Figure 4.




Figure 4 A & B. Pre-operative above show a comminuted and dorsally angulated intra-articular distal radius fracture.
Figure 4C & D. Post-operative views demonstrate anatomic reduction and fixation with the VLPS. The lateral view may suggest entrance of the distal pegs into the radial carpal joint, but a 30-degree lateral view aligning with the x-ray beam will better demonstrate the subchondral placement of the pegs.
Rehabilitation Protocol
Both cohorts received the same postoperative rehabilitation. At one week postoperatively, a thermoplastic wrist splint is fabricated. Active and passive finger ROM, and active wrist ROM exercises are initiated. The patient wears the splint except for light activity and exercises. At two weeks, sutures are removed. At six weeks, passive wrist ROM and gentle strengthening are initiated. The patient begins to wean the splint off, and at twelve weeks discontinues the splint completely.
Results
Ninety-nine patients were included in the study, with 14 patients (14 fractures) in the FSF cohort and 85 patients (85 fractures) in the VLPS cohort. Demographic and clinical data are presented in Table I.
Table I.
Demographic Data
| FSF* Cohort | VLPS** Cohort | |
|---|---|---|
| No. of patients enrolled | 14 | 85 |
| No. of female patients | 5 (36%) | 55 (65%) |
| No. of right hand dominant patients | 12 (86%) | 80 (94%) |
| Mean age (range) | 46 (23 to 79) | 49 (18 to 83) |
| No. of fractures | 14 | 85 |
| No. of right-side fractures | 1 (7%) | 39 (46%) |
| No. AO type A | 1 (7%) | 36 (42%) |
| No. AO type B | 2 (14%) | 10 (12%) |
| No. AO type C | 11 (79%) | 39 (46%) |
Fragment specific fixation
Volar locking plate system
Radiographic Outcomes
Radiographic outcomes are shown in Tables II through VII. Table II demonstrates that although radial inclination differed between the two cohorts at the time of injury (p<0.05), it was corrected to near-normal values post-operatively, and remained corrected at final follow-up in both cohorts. Table III shows the same results when comparing only same AO-type fractures.
Table II.
Radial Inclination and Deviation from Normal* – All AO-types
| Pre-operative | Immediate post-operative | Final post-operative value at one year | ||||
|---|---|---|---|---|---|---|
| Mean | Deviation** | Mean | Deviation | Mean | Deviation | |
| FSF Cohort | 8° ± 10° | 13° ± 10° | 22° ± 5° | 3° ± 2° | 22° ± 4° | 4° ± 1° |
| VLPS Cohort | 19° ± 7° | 6° ± 5° | 25° ± 3° | 3° ± 3° | 25° ± 3° | 3° ± 2° |
Absolute deviation of mean radial inclination from normal value (22°)
Wilcoxon two-sample test
Table VII.
Ulnar Variance* -- Same AO-type only
| Pre-operative | Immediate post-operative | Final post-operative value at one year | ||
|---|---|---|---|---|
| FSF Cohort AO-type C** | Negative | 33% | 57% | 17% |
| Neutral | 0% | 29% | 17% | |
| Positive | 67% | 14% | 66% | |
| VLPS Cohort AO-type C** | Negative | 23% | 47% | 26% |
| Neutral | 37% | 38% | 59% | |
| Positive | 40% | 15% | 15% | |
| P-value† | 0.03 | 0.13 | 0.01 | |
Values are percentage of the cohort with negative, neutral, or positive ulnar variance
Because of the low N for AO-type A and B fractures, only AO-type C fractures are compared
Fisher’s exact test, comparing distribution of ulnar variance between cohorts at given time
Table III.
Radial Inclination and Deviation from Normal* – Same AO-type only
| Cohort | AO-type** | Pre-operative | Immediate post-operative | Final post-operative | |||
|---|---|---|---|---|---|---|---|
| Mean | Deviation† | Mean | Deviation | Mean | Deviation | ||
| FSF | C | 6° ± 10° | 16° ± 10° | 21° ± 6° | 4° ± 4° | 23° ± 5° | 5° ± 2° |
| VLPS | C | 19° ± 8° | 6° ± 6° | 25° ± 3° | 4° ± 2° | 25° ± 4° | 4° ± 3° |
Absolute deviation of mean radial inclination from normal value (22°)
Because of the low N for AO-type A and B fractures, only AO-type C fractures are compared
P-value < 0.05, Wilcoxon two-sample test
Measurements of volar tilt show a different pattern. Table IV demonstrates that in the FSF cohort, volar tilt was not normal in the immediate post-operative period (−5 degrees) and that it worsened over 12 months to −10 degrees. The same pattern can be seen in Table V, which compares volar tilt in only same AO-type fractures.
Table IV.
Volar Tilt and Deviation from Normal – All AO-types*
| Pre-operative | Immediate post-operative | Final post-operative | ||||
|---|---|---|---|---|---|---|
| Mean | Deviation | Mean | Deviation** | Mean | Deviation** | |
| FSF Cohort | −16° ± 12° | 27° ± 12° | −5° ± 8° | 15° ± 8° | −10° ± 10° | 21° ± 10° |
| VLPS Cohort | −13° ± 19° | 26° ± 16° | 10° ± 5° | 4° ± 3° | 10° ± 5° | 3° ± 3° |
Absolute deviation of mean volar tilt from normal value (11°)
P-value < 0.05, Wilcoxon two-sample test
Table V.
Volar Tilt and Deviation from Normal* – Same AO-type only
| Cohort | AO-type** | Pre-operative | Immediate post-operative | Final post-operative | |||
|---|---|---|---|---|---|---|---|
| Mean | Deviation | Mean | Deviation† | Mean | Deviation† | ||
| FSF | C | −14° ± 14° | 25° ± 14° | −8° ± 5° | 19° ± 5° | −12° ± 5° | 23° ± 5° |
| VLPS | C | −14° ± 19° | 26° ± 19° | 10° ± 5° | 4° ± 3° | 10° ± 5° | 4° ± 3° |
Absolute deviation of mean radial inclination from normal value (11°)
Because of the low N for AO-type A and B fractures, only AO-type C fractures are compared
P-value < 0.05, Wilcoxon two-sample test
Table VI demonstrates an improvement in relative radial length in both cohorts after surgery, with a majority of fractures having negative or neutral ulnar variance. However, by 12 months the FSF cohort had lost radial length, and a majority of fractures demonstrated positive ulnar variance. The VLPS cohort, however, maintained negative or neutral ulnar variance in a majority of fractures, suggesting better maintenance of radial length. When comparing only same AO-type fractures, the same pattern is seen (Table VII).
Table VI.
Ulnar Variance* – All AO-types
| Pre-operative | Immediate post-operative | Final post-operative value at one year | ||
|---|---|---|---|---|
| FSF Cohort | Negative | 25% | 66% | 25% |
| Neutral | 25% | 22% | 13% | |
| Positive | 50% | 12% | 62% | |
| VLPS Cohort | Negative | 17% | 42% | 25% |
| Neutral | 33% | 39% | 58% | |
| Positive | 50% | 19% | 17% | |
| P-value** | 0.78 | 0.53 | <0.01 | |
Values are percentage of the cohort with negative, neutral, or positive ulnar variance
Fisher’s exact test, comparing distribution of ulnar variance between cohorts
In summary, the VLPS cohort demonstrated near anatomic reduction after surgery that was maintained at 12 months post-operatively, whereas the FSF cohort demonstrated a loss of volar tilt and radial length over time.
Objective Functional Outcomes
Objective functional outcomes including grip and pinch strength, and ROM are shown in Tables VIII and IX. Both grip and lateral pinch strength were superior in the VLPS cohort at 6 and 12 months, even when controlling for AO types. However, by 12 months the differences in strength between the two cohorts had narrowed and were no longer statistically significant (Table VIII). Table IX shows that most ROM measurements were superior in the VLPS cohort at both 6 and 12 months, although not all differences were significant. As a group, the objective functional measurements demonstrate superior early results in the VLPS cohort, although this difference narrowed over time.
Table VIII.
Post-operative Hand Function on Injured Side*
| 6 months | 12 months | ||
|---|---|---|---|
| Grip strength | FSF Cohort (%) | 55.3 ± 25.2 | 73.7 ± 13.0 |
| VLPS Cohort (%) | 72.3 ± 24.3 | 81.3 ± 22.7 | |
| P-value** | < 0.01 | 0.06 | |
| Lateral pinch | FSF Cohort (%) | 74.5 ± 21.8 | 89.7 ± 14.7 |
| VLPS Cohort (%) | 91.8 ± 12.3 | 96.1 ± 11.4 | |
| P-value | < 0.01 | 0.31 | |
Values are given as a percentage of uninjured contralateral side
Age group and AO class matched regression analysis
Table IX.
Post-operative Range of Motion on Injured Side*
| 6 months | 12 months | ||
|---|---|---|---|
| Flexion-Extension | FSF Cohort (%) | 68.7 ± 13.1 | 78.3 ± 9.3 |
| VLPS Cohort (%) | 86.7 ± 14.2 | 91.4 ± 13.3 | |
| P-value** | <0.01 | 0.01 | |
| Ulnar Deviation | FSF Cohort (%) | 53.8 ± 20.8 | 72.4 ± 15.0 |
| VLPS Cohort (%) | 88.4 ± 19.4 | 86.5 ± 18.1 | |
| P-value | <0.01 | 0.27 | |
| Radial Deviation | FSF Cohort (%) | 88.5 ± 48.9 | 88.6 ± 27.1 |
| VLPS Cohort (%) | 89.7 ± 24.5 | 98.5 ± 27.7 | |
| P-value | 0.99 | 0.07 | |
| Pronation | FSF Cohort (%) | 91.2 ± 11.4 | 102.6 ± 5.3 |
| VLPS Cohort (%) | 95.4 ± 10.1 | 97.8 ± 7.1 | |
| P-value | 0.48 | 0.01 | |
| Supination | FSF Cohort (%) | 85.4 ± 21.0 | 83.5 ± 15.3 |
| VLPS Cohort (%) | 94.5 ± 12.9 | 96.8 ± 8.2 | |
| P-value | 0.14 | <0.01 | |
Values are given as a percentage of uninjured contralateral side
Age group and AO class matched regression analysis
Patient-Rated Outcomes
Table X shows patient-rated outcomes when controlling for AO types. The VLPS cohort scored better than the FSF cohort (p<0.05) in the domains of hand function, ADL, aesthetics, satisfaction, and overall scores at 6 months. Scores in the work and pain domains were also better in the VLPS cohort, although these were not statistically significant. However, by 12 months, although the VLPS cohort continued to have better scores than the FSF cohort in all domains, the only statistically significant differences were in the work and aesthetics domains. Overall, the VLPS cohort showed superior patient-rated outcomes, particularly in the early postoperative period.
Table X.
Patient Rated Outcomes (MHQ)*
| 6 months | 12 months | ||
|---|---|---|---|
| Overall | FSF Cohort | 62.3 ± 15.5 | 76.5 ± 19.8 |
| VLPS Cohort | 83.3 ± 14.9 | 86.9 ± 15.5 | |
| P-value** | < 0.01 | 0.25 | |
| Function | FSF Cohort | 58.3 ± 22.5 | 76.7 ± 19.1 |
| VLPS Cohort | 80.9 ± 16.2 | 86.1 ± 17.8 | |
| P-value | <0.01 | 0.45 | |
| ADL | FSF Cohort | 71.3 ± 22.7 | 87.9 ± 10.6 |
| VLPS Cohort | 89.9 ± 13.6 | 91.3 ± 14.1 | |
| P-value | <0.01 | 0.33 | |
| Work | FSF Cohort | 65.8 ± 30.3 | 46.7 ± 40.7 |
| VLPS Cohort | 85.7 ± 22.2 | 86.6 ± 23.2 | |
| P-value | 0.06 | <0.01 | |
| Pain | FSF Cohort | 39.6 ± 19.2 | 31.7 ± 23.2 |
| VLPS Cohort | 20.9 ± 17.6 | 15.5 ± 17.9 | |
| P-value | 0.06 | 0.22 | |
| Aesthetic | FSF Cohort | 59.9 ± 20.7 | 56.3 ± 20.2 |
| VLPS Cohort | 85.7 ± 19.8 | 90.1 ± 15.5 | |
| P-value | 0.01 | <0.01 | |
| Satisfaction | FSF Cohort | 57.0 ± 23.9 | 79.2 ± 27.8 |
| VLPS Cohort | 79.7 ± 20.4 | 83.0 ± 23.7 | |
| P-value | <0.01 | 0.84 | |
Score range is 0 to 100, with higher scores representing better outcomes (except for pain domain, in which a lower score indicates less pain)
Age group and AO class matched regression analysis
Complications
Table XI summarizes the post-operative complications. Three of the patients in the VLPS cohort (4%) experienced major complications, including infections that required operative intervention or hospital admission, and non-unions. One patient (1%) experienced a minor complication (cellulitis) that was treated without operation or admission. Eight patients in the FSF cohort (57%) experienced major complications, including tendon or nerve irritation or hardware palpability that required hardware removal. There were no minor complications in the FSF cohort.
Table XI.
Complications
Major complications were those requiring hospital admission or re-operation
Minor complications were those treated on an outpatient basis without surgery
Discussion
Historically, DRFs have been plated on the side of displacement: dorsally displaced fractures were plated dorsally, and volarly displaced fractures were plated volarly.4 This approach allowed the plate to buttress the fracture against re-displacement, and placed the plate on the side of greater comminution. Because most DRFs are dorsally displaced, early fixation systems focused on dorsal plates. However, dorsal plates caused frequent tendon-related complications necessitating re-operation in as many as 30% of patients.20 This led to an interest in volar plating. Recent advances in hardware design now allow reliable volar plating of DRFs, regardless of the direction of displacement.5
The VLPS used in this study is a T-shaped plate that is anatomically contoured. The proximal stem lies on the diaphysis proximal to the fracture and is secured with conventional screws. The transverse portion of the plate overlies the distal fracture fragment(s). The two intersecting rows of fixed-angle pegs lock into the plate. This creates two theoretical advantages: 1) the locking pegs increase the stability of the plate-screw construct4 and 2) the rows of pegs lie directly beneath subchondral bone, supporting axial loads.4 Because the pegs are locking, bicortical fixation is not absolutely necessary.
Another recent development in DRF fixation is that of FSF. The distal radius and ulna can be conceptualized as three longitudinal columns.21, 22 The radial half of the radius represents the radial column. The ulnar half of the radius represents the central or intermediate column. The ulna and TFCC form the ulnar column. Melone23 divided the central column into volar and dorsal components. The pin plates in combination with the wire forms in the FSF set permit fixation of the individual fragments of each column. This differs from the VLPS, which attempts to secure all fragments to a single plate.
A review of the literature reveals a number of studies that report good clinical outcomes using either the VLPS or FSF.5, 17, 18, 24 In addition, there are a number of biomechanical studies that directly compare the VLPS and FSF.25–27 However, this study is the first direct comparison of the clinical and radiographic outcomes of the VLPS versus FSF.
In this study, the VLPS cohort demonstrated better radiographic outcomes. Fractures treated with FSF tended to shorten and dorsally angulate post-operatively, a problem that did not occur with the VLPS. One possible explanation is that the VLPS provides better fixation than FSF. In a cadaveric biomechanical study by Taylor et al,26 both the fixed-angle VLPS and FSF systems performed similarly in terms of stiffness and failure load of the radial column. However, another recent cadaveric study by same group27 compared FSF with another locking volar plate, and showed differences in angulation at the osteotomy site between the two groups. At low loads, there was greater angulation in the volar plate group, but at higher loads the FSF group showed greater angulation. It should be noted that the cadaveric fracture models and the volar plates used in these two studies differed. These studies suggest that in general, volar plate fixation and FSF perform similarly, although at certain loads volar plates and FSF may provide different resistance to bending forces.
Another possible explanation for the difference in radiographic outcomes in this study is that volar tilt was not initially corrected as well in the FSF cohort as it was in the VLPS cohort, although the reduction in all patients were within acceptable limits. The limited surgical exposure required for FSF makes anatomic reduction more difficult when compared to the wide exposure and excellent fracture visualization achieved with the VLPS approach.
A third possibility is that the difference in AO-type between the two cohorts affected radiographic outcomes. The percentage of AO-type C fractures in the FSF cohort was substantially greater than in the VLPS cohort. This is because FSF was used preferentially to treat comminuted intra-articular fractures during the FSF cohort collection period. However, even when only same AO-type fractures are compared (type C only), the FSF group demonstrated a loss of relative radial length and volar tilt over time that did not occur in the VLPS cohort.
Both the objective functional and patient-rated outcomes showed a common pattern, with the VLPS cohort performing better at 6 months. By 12 months, the differences between the two cohorts had diminished. One possible explanation for better early objective and subjective outcomes in the VLPS cohort is the difference in fracture severity in the two cohorts. A higher AO-type is associated with greater soft tissue injury, which could affect the speed of recovery. However, the analysis of functional and patient-rated outcomes was matched for AO-type specifically to control for this factor. Another possible explanation is that superior maintenance of fracture reduction in the VLPS cohort contributed to better outcomes early on.28
The most striking difference between the two cohorts was the complication rate. Although other case series in the literature show a lower incidence of hardware removal (4% to 16%)17, 18, 24 approximately 50 percent of patients in the FSF cohort required hardware removal. Although the pin plates are low profile, there is little soft tissue coverage over the radial styloid and the dorsal distal radius. Additionally, the sensory branches of the radial nerve lie directly over the radial pin plate. In contrast, the VLPS is well covered by soft tissue, and the PQ can often be repaired over the volar plate, protecting the FPL tendon.
The small sample size of the FSF cohort and the difference in fracture AO-type between the two cohorts makes matching patient and fracture characteristics difficult. It is also quite possible that the outcomes with the VLPS are better because of increased experience with this technology. However, all radiographs in the FSF and VLPS groups have acceptable reduction based on fluoroscopy examination in the operating theater, which assured that there is no systematic difference in the quality of reduction for the two operations.
In conclusion, we believe that the VLPS provides more stable fixation, results in better early outcomes, and has a lower complication rate than FSF.
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
Footnotes
- Trimed Wrist Fixation System™, Trimed, Inc.
- DVR™ plate, Hand Innovations, LLC
Financial Disclosure Statement
One or more of the authors received funding from the American Association for Hand Surgery and the Department of Surgery at the University of Michigan. No commercial entity promised or provided payments or benefits to any of the authors, or to any of the research organizations or educational institutions with which they are associated.
References
- 1.Chung K, Spilson S. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg. 2001;26A:908. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Wright T. Malunion of the distal radius and ulna. In: Berger R, Weiss A, editors. Hand surgery. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 321–335. [Google Scholar]
- 3.Fernandez D, Palmer A. Fractures of the distal radius. In: Green D, Hotchkiss R, Pederson W, editors. Green’s operative hand surgery. 4. New York: Churchill Livingstone; 1999. pp. 929–985. [Google Scholar]
- 4.Freeland AE, Luber KT. Biomechanics and biology of plate fixation of distal radius fractures. Hand Clin. 2005;21:329. doi: 10.1016/j.hcl.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Chung K, Watt A, Kotsis S, et al. Treatment of unstable distal radial fractures with the Volar Locking Plating System. J Bone Joint Surg. 2006;88A:2687. doi: 10.2106/JBJS.E.01298. [DOI] [PubMed] [Google Scholar]
- 6.DiBenedetto MR, Lubbers LM, Ruff ME, et al. Quantification of error in measurement of radial inclination angle and radial-carpal distance. J Hand Surg [Am] 1991;16:399. doi: 10.1016/0363-5023(91)90004-u. [DOI] [PubMed] [Google Scholar]
- 7.Mann FA, Rasissdana SS, Wilson AJ, et al. The influence of age and gender on radial height. J Hand Surg [Am] 1992;18A:711. doi: 10.1016/0363-5023(93)90324-v. [DOI] [PubMed] [Google Scholar]
- 8.Gartland JJ, Werley C. Evaluation of healed Colles’ fractures. J Bone Joint Surg. 1951;33A:895. [PubMed] [Google Scholar]
- 9.Chung K, Pillsbury M, Walters M, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg [Am] 1998;23:575. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 10.Chung K, Hamill J, Walters M, et al. The Michigan Hand Outcomes Questionnaire (MHQ): Assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42:619. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Chung K, Wei F. An outcome study of thumb reconstruction using microvascular toe transfer. J Hand Surg [Am] 2000;25:651. doi: 10.1053/jhsu.2000.6913. [DOI] [PubMed] [Google Scholar]
- 12.Chung K, Kotsis S, Kim H. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg [Am] 2004;29:646. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kotsis S, Chung K. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder and Hand Questionnaire in Carpal Tunnel Surgery. J Hand Surg [Am] 2005;30:81. doi: 10.1016/j.jhsa.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 14.Kotsis S, Lau F, Chung K. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg [Am] 2007;32:84. doi: 10.1016/j.jhsa.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Chung K. [Accessed 2008 January 7];Michigan Hand Outcomes Questionnaire. [Web Page] 2008 [Google Scholar]
- 16.Schumer ED, Leslie BM. Fragment-specific fixation of distal radius fractures using the Trimed device. Tech Hand Up Extrem Surg. 2005;9:74. doi: 10.1097/01.bth.0000158974.15897.1b. [DOI] [PubMed] [Google Scholar]
- 17.Konrath G, Bahler S. Open reduction and internal fixation of unstable distal radius fractures: results using the Trimed fixation system. J Orthop Trauma. 2002;16:578. doi: 10.1097/00005131-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Gerostathopoulos N, Kalliakmanis A, Fandridis E, et al. Trimed fixation system for displaced fractures of the distal radius. J Trauma. 2007;62:913. doi: 10.1097/01.ta.0000219948.92935.cd. [DOI] [PubMed] [Google Scholar]
- 19.Chung K, Petruska E. Treatment of unstable distal radius fractures with the volar locking plating system. A surgical technique. J Bone Joint Surg. 2007;89A:256. doi: 10.2106/JBJS.G.00283. [DOI] [PubMed] [Google Scholar]
- 20.Lucas GL, Fejfar ST. Complications in internal fixation of the distal radius. J Hand Surg [Am] 1998;23A:111. doi: 10.1016/s0363-5023(98)80028-2. [DOI] [PubMed] [Google Scholar]
- 21.Rikli D, Regazzoni P. Fractures of the distal end of the radius treated by internal fixation and early function: a preliminary report of 20 cases. J Bone Joint Surg. 1996;78B:588. [PubMed] [Google Scholar]
- 22.Rikli D, Regazzoni P. The double plating technique for distal radius fractures. Tech Hand Up Extrem Surg. 2000;4:107. doi: 10.1097/00130911-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Melone CP., Jr Articular fractures of the distal radius. Orthop Clin North Am. 1984;15:217–236. [PubMed] [Google Scholar]
- 24.Benson LS, Minihane KP, Stern LD, et al. The outcomes of intra-articular distal radius fractures treated with fragment-specific fixation. J Hand Surg [Am] 2006;31A:1333–1339. doi: 10.1016/j.jhsa.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Grindel SI, Wang M, Gerlach M, et al. Biomechanical comparison of fixed-angle volar plate versus fixed-angle volar plate plue fragment-specific fixation in a cadaveric distal radius fracture model. J Hand Surg [Am] 2007;32A:194–199. doi: 10.1016/j.jhsa.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Taylor KF, Parks BG, Segalman KA. Biomechanical stability of a fixed-angle volar plate versus fragment-specific fixation system: cyclic testing in a C2-type distal radius cadaver fracture model. J Hand Surg [Am] 2006;31A:373–381. doi: 10.1016/j.jhsa.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 27.Cooper EO, Segalman KA, Parks BG, et al. Biomechanical stability of a volar locking-screw plate versus fragment-specific fixation in a distal radius fracture model. Am J Orthop. 2007;36:E46–49. [PubMed] [Google Scholar]
- 28.Chung K, Kotsis S, Kim H. Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg [Am] 2007;32A:76–83. doi: 10.1016/j.jhsa.2006.10.010. [DOI] [PubMed] [Google Scholar]


