Abstract
Background
Delays in follow-up after breast cancer screening contribute to disparities in breast cancer outcomes. The objective of this research was to determine the impact of race/ethnicity and health insurance on diagnostic time, defined as number of days from suspicious finding to diagnostic resolution.
Methods
This retrospective cohort study of 1538 women examined for breast abnormalities between 1998-2010 at 6 hospitals/clinics in the District of Columbia measured mean diagnostic times between non-Hispanic whites (NHWs), non-Hispanic blacks (NHBs), and Hispanics with private, government, or no health insurance using a full-factorial ANOVA model.
Results
Respective average—geometric mean (95% CI)— diagnostic times (in days) for NHWs, NHBs, and Hispanics were: 16 (12, 21), 27 (23, 33), and 51 (35, 76) among privately insured; 12 (7, 19), 39 (32, 48), and 71 (48, 105) among government insured; 45 (17, 120), 60 (39, 92), and 67 (56, 79) among uninsured. Government insured NHWs had significantly shorter diagnostic times than government insured NHBs (p=0.0003) and Hispanics (p<0.0001). Privately insured NHWs had significantly shorter diagnostic times than privately insured NHBs (p=0.03) and Hispanics (p<0.0001). Privately insured NHBs had significantly shorter diagnostic times than uninsured NHBs (p=0.03).
Conclusions
Insured minorities waited >2 times longer to reach their diagnostic resolution than insured NHWs. Having private health insurance increased the speed of diagnostic resolution in NHBs; however, their diagnostic time remained significantly longer than for privately insured NHWs. These results suggest diagnostic delays in minorities are more likely caused by other barriers associated with race/ethnicity than by insurance status.
Keywords: disparities, race, ethnicity, health insurance, breast cancer
INTRODUCTION
Delays in follow-up after breast cancer screening may contribute to disparities in breast cancer outcomes. This present study examines follow-up delays among a sample of women in the District of Columbia (DC), a metropolitan area known to have high mortality from breast cancer compared to national rates. Increased screenings and advances in treatment have had a significant impact in reducing mortality rates of black women living in DC from 49.8 (per 100,000) in 1995 to 31.5 (per 100,000) in 2005.1 Despite these improvements, disparities between population groups persist. In 2005, mortality rates from breast cancer among white women (20.7 per 100,000) remained markedly lower than those of their local black counterparts.1 In 2001, a publicly funded safety-net insurance program for low-income DC residents was implemented and has helped to lower the number of uninsured (9% compared to 15% nationally); however, among these uninsured individuals, the burden falls disproportionately on blacks (56%) and Hispanics (23%).2,3
These statistics led to an examination of the effects of race, ethnicity and health insurance status on a sample of women with suspicious breast findings from DC. These women represent the controls from a patient navigation intervention study designed to potentially reduce diagnostic delays. The primary objective of this study was to determine the impact of race, ethnicity and health insurance on diagnostic time, defined as the number of days from a suspicious finding to diagnostic resolution.
This study began with the primary hypothesis that patients with health insurance would have a shorter diagnostic time than patients without health insurance. Furthermore, it was posited that every insured patient would receive the same timely diagnosis as any other patient with equivalent insurance, regardless of her race or ethnicity. Exploring these hypotheses will give medical professionals a better understanding of the relationships between race, ethnicity, health insurance and diagnostic delay in breast cancer patients.
Under the hypothesis that health insurance is the primary barrier to a timely diagnosis, differences in time to diagnosis should be negligible between the various race and ethnicity groups with equivalent health insurance. Therefore, significant differences in diagnostic times would imply that additional barriers exist. Acknowledging the existence of additional barriers is the first step toward eliminating them.
METHODS
This is a retrospective cohort study of 1538 women examined for breast abnormalities between 1998 and 2010 at six hospitals/clinics in DC, including the George Washington University Hospital, Howard University Hospital, Providence Hospital, Washington Hospital Center’s Center for Breast Health, Unity Health Care, Inc., and the George Washington University Mammovan (an outreach program focusing on underserved women in DC). These facilities service the vast majority of the poor and underserved community in DC. Homogeneity was assumed across facilities in the sense that every patient had an equal opportunity to receive a timely diagnosis. The majority of the suspicious findings were detected between 2007 and 2009—26% in 2007, 38% in 2008, and 25% in 2009.
The women in this study represent the records-based control group for a larger study of the effectiveness of patient navigation, The DC Citywide Patient Navigation Research Program.4 All of these women had a suspicious breast abnormality, but they did not receive the main study’s intervention, patient navigation, due to timing and logistical constraints. The selection of the controls was developed in an attempt to match as closely as possible the demographics of the women being navigated. For example, sites visited by the GWU Mammovan were chosen to match the proportion of Hispanic and African-American women seen at the Capital Breast Care Center and the Washington Hospital Center Preventorium, which try to navigate all women and did not provide any controls. Navigated cancer patients who did not have controls selected at the site were matched by time of first detected abnormality, race and ethnicity in the George Washington University Cancer Registry. The control women in this study were identified over a 12-year period from 1998-2010 to ascertain the time between suspicious finding and diagnostic resolution in relation to the effects of race/ethnicity and type of health insurance.
Suspicious finding was defined as any breast abnormality identified by a clinician during the physical exam, mammography, or ultrasound. Diagnostic resolution represents the definitive diagnosis for that patient (i.e., the result obtained after diagnostic studies were completed in order to resolve a suspicious finding). The results were primarily either (i) no evidence of malignancy on diagnostic mammogram or (ii) definitive diagnosis by biopsy (benign or malignant).
Since control subjects were never directly contacted and only de-identified data was obtained, informed consent was waived for this group.
The goal of this study was to identify the effect of race, ethnicity, and health insurance on diagnostic time (defined as the number of days from suspicious finding to diagnostic resolution). The primary dependent variable of interest was diagnostic time, reported as a continuous variable in days. The independent variables of interest included race/ethnicity (non-Hispanic white [NHW], non-Hispanic black [NHB], Hispanic) and type of insurance coverage (private, government, none). Government insurance included federal (Medicaid and Medicare) and the DC government safety-net insurance “Alliance”. If a woman had both private and government insurance, then she was assigned to the private insurance group. For race/ethnicity, the analysis was restricted to NHW, NHB, and Hispanic because the numbers in the “other” race/ethnicity groups were too small to provide reliable estimates, e.g., Asian (47), Native Hawaiian/Pacific Islander (5), and American Indian/Alaska Native (5).
All patient data were abstracted from medical records and de-identified before being entered into a central database. Data were abstracted to match the race/ethnicity of navigated patients as they were enrolled. All abstracted records were reviewed by a physician with many years of experience in oncology and pathology. If there were any potential inconsistencies or irregularities, the physician reviewed the original medical record. The exclusion criteria included: women under the age of 18, history of prior cancer within the previous 5 years, and current treatment for cancer except for non-melanoma skin cancer or CIN. Data on marital status, employment, education, income, and primary language were not usually provided in the medical records.
For 427 women seen by the GWU Mammovan, race and ethnicity were imputed based on the demographics of the screening sites, which were predominantly African-American, Hispanic, and Asian churches known to be homogeneous with regard to race and ethnicity. Imputation was applied only for those women seen by the GWU Mammovan. The imputed values were selected with a high degree of confidence based on the specific location of the GWU Mammovan on the date of initial abnormal screening, either an African-American, Hispanic, or Asian church.
Examination of log-log survival curves and goodness-of-fit tests revealed that the proportional hazards assumption was not satisfied. Therefore, Cox proportional hazards regression was not appropriate for the data in this study. Alternatively, one-way and factorial ANOVA models were used to examine the relationships between diagnostic time and the independent variables race/ethnicity and type of health insurance either individually or collectively. Age was considered as a potential confounder in the multivariable analysis. Log transformations were taken on non-normal data to satisfy model assumptions. Residual plots showed that the log-transformed data satisfied the assumptions of normality and homogeneous variance, supporting the use of the log-transformed data. The Tukey-Kramer method was used for p-value adjustment in performing multiple comparisons.
Importantly, the Centers for Disease Control and Prevention (CDC) established a set guideline stating “the date of final diagnosis must not exceed 60 days from the date of abnormal mammogram”.5 The odds of having a diagnostic delay greater than 60 days for the racial/ethnic and insurance groups were examined by categorizing diagnostic time into two groups (≤60 and >60 days) and fitting simple and multiple logistic regression models.
All statistical tests were two-sided, and the level of significance was set at 0.05. All statistical analyses were performed using SAS® software, Version 9.1 (SAS Institute, Cary, NC).
RESULTS
The sample in this study consisted of 1538 women ranging in age from 23 to 93 years (median=51). Descriptive statistics are provided in Table 1. Diagnostic time was missing for 1 NHW woman with private insurance and 1 NHB woman with unknown insurance. Diagnostic times of 0 were replaced with 0.01 in calculating geometric means. While only 5% of NHWs and 8% of NHBs were known to be uninsured, 67% of Hispanics were known to be uninsured.
Table 1.
Descriptive Statistics of Diagnostic Time (in Days) Stratified by Race/Ethnicity and Type of Insurance*
| Type of Insurance | Non-Hispanic White |
Non-Hispanic Black |
Hispanic | Other | Unknown | Total |
|---|---|---|---|---|---|---|
| Private | ||||||
| n | 119 | 227 | 52 | 29 | 237 | 664 |
| Mean (STD) | 43 (62) | 55 (75) | 75 (74) | 39 (38) | 61 (71) | 56 (71) |
| Median (Q1, Q3) | 21 (9, 53) | 32 (20, 59) | 51 (31, 91) | 30 (12, 40) | 41 (27, 64) | 35 (19, 64) |
| Government | ||||||
| n | 34 | 189 | 50 | 7 | 77 | 357 |
| Mean (STD) | 64 (106) | 80 (100) | 94 (78) | 25 (15) | 73 (82) | 78 (93) |
| Median (Q1, Q3) | 26 (11, 34) | 41 (22, 89) | 60 (41, 105) | 35 (6, 35) | 49 (28, 83) | 42 (23, 89) |
| None | ||||||
| n | 8 | 43 | 261 | 37 | 59 | 408 |
| Mean (STD) | 59 (36) | 94 (108) | 78 (60) | 70 (47) | 79 (59) | 79 (65) |
| Median (Q1, Q3) | 49 (40, 86) | 65 (37, 102) | 63 (50, 80) | 56 (42, 85) | 67 (54, 76) | 63 (49, 83) |
| Unknown | ||||||
| n | 3 | 49 | 26 | 2 | 29 | 109 |
| Mean (STD) | 31 (31) | 66 (61) | 74 (76) | 88 (39) | 117 (164) | 81 (103) |
| Median (Q1, Q3) | 31 (0, 61) | 47 (26, 95) | 52 (36, 68) | 88 (60, 115) | 66 (34, 113) | 52 (33, 90) |
| Total | ||||||
| n | 164 | 508 | 389 | 75 | 402 | 1538 |
| Mean (STD) | 48 (72) | 69 (88) | 80 (66) | 54 (44) | 70 (83) | 69 (78) |
| Median (Q1, Q3) | 24 (9, 53) | 39 (21, 77) | 62 (46, 83) | 40 (29, 81) | 46 (30, 71) | 47 (26, 76) |
The numbers in this table include the imputed race/ethnicity values for the 427 women seen by the GWU Mammovan.
Histograms and QQ plots revealed that diagnostic time was positively skewed. Log-transformations were taken to normalize the data, and the transformed variable was used in the following ANOVA models.
A one-way ANOVA model on race/ethnicity revealed significant differences in diagnostic times between the three race/ethnicity groups—excluding women of ‘other’ or unknown race/ethnicity (p<0.0001). Results are summarized in Table 1. Without controlling for any other factors, NHWs had significantly shorter diagnostic times than NHBs (p<0.0001) and Hispanics (p<0.0001), and NHBs had significantly shorter diagnostic times than Hispanics (p<0.0001). NHWs, NHBs, and Hispanics had average diagnostic times of approximately one-half of a month, one month, and two months, respectively.
Similarly, a one-way ANOVA model on type of insurance coverage revealed significant differences in diagnostic times between women with private, government, or no insurance—excluding women with unknown type of insurance (p<0.0001). Results are summarized in Table 1. Uninsured women had significantly longer diagnostic times than women with private (p<0.0001) or government insurance (p<0.0001), and women with government insurance had significantly longer diagnostic times than women with private insurance (p=0.009). While privately insured women had an average diagnostic time <1 month and women with government insurance had an average diagnostic time >1 month, uninsured women had an average diagnostic time of >2 months, revealing that uninsured women had to wait twice as long as insured women for a diagnostic resolution following suspicious finding.
Fig. 1 displays the results of the full-factorial ANOVA model (p<0.0001) using race/ethnicity, type of insurance, and the significant interaction between race/ethnicity and type of insurance (p=0.04) as independent variables. Age was not a significant covariate (p=0.89). Moreover, the inclusion of age in the model did not result in meaningfully different interpretations of the relationship between diagnostic time and race/ethnicity and type of insurance nor did it contribute any additional information to the final conclusions reached. Therefore, age was removed from the final model.
Figure 1.
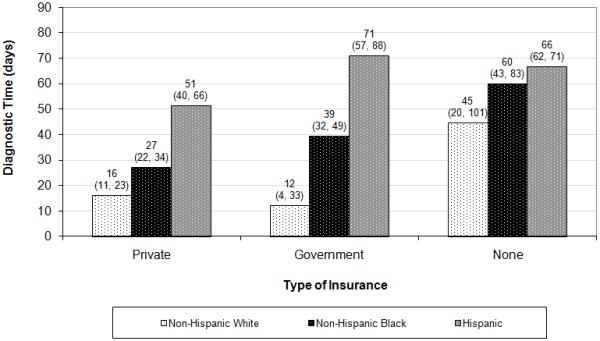
Average—geometric mean (95% CI)—diagnostic time (in days) stratified by race/ethnicity and type of insurance. Refer to Table 1 for the sample sizes corresponding to each bar.
From the full-factorial ANOVA model and the Tukey-Kramer method for p-value adjustment in performing multiple comparisons, NHWs with government insurance had significantly shorter diagnostic times than both NHBs (p=0.0003) and Hispanics (p<0.0001) with government insurance. While NHWs with government insurance had an average diagnostic time of only 12 days, NHBs with government insurance had an average diagnostic time of about 39 days and Hispanics with government insurance had an average diagnostic time of about 70 days.
Also, privately insured NHWs had significantly shorter diagnostic times than both privately insured NHBs (p=0.03) and Hispanics (p<0.0001). While privately insured NHWs had an average diagnostic time of only 16 days, privately insured NHBs had an average diagnostic time of about 27 days and privately insured Hispanics had an average diagnostic time of about 51 days.
Finally, privately insured NHBs had significantly shorter diagnostic times than uninsured NHBs (p=0.03). While privately insured NHBs had an average diagnostic time of only 27 days, uninsured NHBs had an average diagnostic time of about 60 days.
The Kaplan-Meier curves presented in Fig. 2 visually describe the various distributions of diagnostic time among the racial/ethnic and insurance groups. Fig. 2a shows that 79% of NHWs, 68% of NHBs, and only 47% of Hispanics were diagnosed within 60 days. Interestingly, while 61% of NHWs and 40% of NHBs were diagnosed within 30 days, only 8% of Hispanics were diagnosed so quickly. Fig. 2b reveals that 73% of privately insured, 66% of government insured, and 44% of uninsured women were diagnosed within 60 days. Differences are more pronounced at the 30-day cutoff, at which point only 6% of uninsured have been diagnosed, whereas 43% of privately insured and 35% of government insured women have been diagnosed. As shown in Fig. 2c, privately insured NHBs were diagnosed much faster than uninsured NHBs. Overall, 62% of the women were diagnosed within 60 days, whereas only 30% were diagnosed within 30 days.
Figure 2.
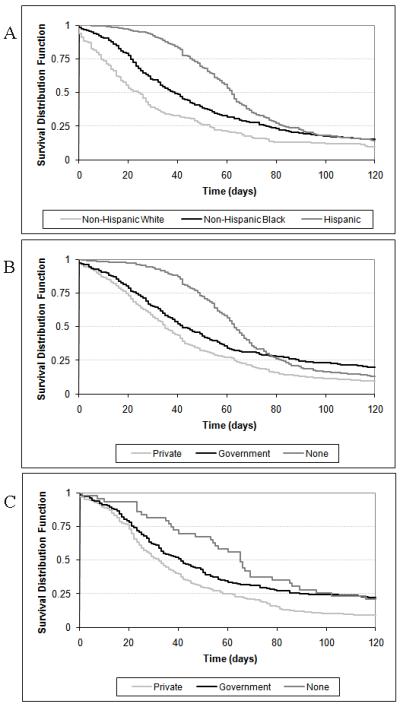
Stratified Kaplan-Meier (K-M) curves for diagnostic time (in days). (a) K-M curves for all women stratified by race/ethnicity. Refer to the column totals in Table 1 for the sample sizes corresponding to each K-M curve. (b) K-M curves for all women stratified by type of insurance. Refer to the row totals in Table 1 for the sample sizes corresponding to each K-M curve. (c) K-M curves for NHB women stratified by type of insurance. Refer to the Non-Hispanic Black column in Table 1 for the sample sizes corresponding to each K-M curve.
Considering the CDC’s 60-day guideline, odds of having a diagnostic delay greater than 60 days were examined in a multiple logistic regression model (p<0.0001) with the dichotomous form of diagnostic time as the response and race/ethnicity (p=0.0001) and type of insurance (p=0.0009) as independent variables. A 30-day cutoff was modeled for comparison. Age (60-day p=0.16; 30-day p=0.35) and the two-way interaction between race/ethnicity and type of insurance (60-day p=0.22; 30-day p=0.30) were not significant in either of the models. Results are summarized in Table 2.
Table 2.
Diagnostic Delay Odds Ratios from Multiple Logistic Regression Models with Time Cutoffs of 60 and 30 Days
| 60-day cutoff | 30-day cutoff | |||
|---|---|---|---|---|
| Variable | OR | 95% CI | OR | 95% CI |
| Race/Ethnicity | ||||
| Non-Hispanic White (ref) | --- | --- | --- | --- |
| Non-Hispanic Black | 1.6 | (1.03, 2.5) | 2.0 | (1.4, 2.9) |
| Hispanic | 2.8 | (1.7, 4.7) | 7.4 | (4.2, 12.8) |
| Type of Insurance | ||||
| Private (ref) | --- | --- | --- | --- |
| Government | 1.3 | (0.9, 1.8) | 1.4 | (1.003, 1.9) |
| None | 2.1 | (1.4, 3.2) | 6.5 | (3.6, 11.7) |
The odds of having diagnostic delays >60 days were almost 3 times more for Hispanics than for NHWs, after controlling for type of insurance. Similarly, the odds for NHBs were 1.6 times more than the odds for NHWs, after controlling for type of insurance. Moreover, uninsured women had twice the odds of privately insured women, after controlling for race/ethnicity.
Interestingly, while the odds of having diagnostic delays >30 days for NHBs were twice the odds for NHWs, the odds for Hispanics were >7 times the odds for NHWs, after controlling for type of insurance. Also, the odds of having diagnostic delays >30 days for government insured women were about 1.4 times more than the odds for privately insured women, while uninsured women had >6 times the odds of privately insured women, after controlling for race/ethnicity.
DISCUSSION
In this study, privately insured NHBs had significantly shorter diagnostic times than uninsured NHBs; however, privately insured NHBs and Hispanics had significantly longer times to diagnostic resolution than privately insured NHWs. Among government insured women, both NHBs and Hispanics had significantly longer diagnostic times than NHWs. Since there were only eight uninsured NHWs in this sample, it was difficult to assess the impact of no insurance on NHWs.
Another limitation of this study is that race and ethnicity had to be imputed for 427 women seen by the GWU Mammovan. As stated previously, the imputed values were selected with a high degree of confidence based on specific locations of the GWU Mammovan on the date of initial abnormal screening, which were primarily African-American, Hispanic, and Asian churches. While these sites were known to be almost exclusively African-American, Hispanic, or Asian, it is possible that a few subjects may have been misclassified with respect to race/ethnicity.
In addition, insurance status may have changed for a small number of patients during the interval being assessed. Also, medical records were relied on to assess variables and outcomes. Data on socioeconomic status or psychosocial variables were not available for inclusion in the study model that might have enhanced understanding of race. Finally, this study was based on a sample that was not probabilistic and that was selected from a single metropolitan area.
However, overall, these results suggest that lack of health insurance may not be the primary barrier to optimal diagnostic resolution in minority women indicating the importance of determining what other factors serve as the primary barriers to accessing diagnostic care, as well as if these delays affect the final breast cancer outcome for these patients.
Andrulis6 and Lillie-Blanton and Hoffman7 have stressed the importance of eliminating financially-based differences in access to care in order to create equity in outcomes across socioeconomic status (SES) groups6 and across racial/ethnic groups7. However, studies performed in other countries with universal coverage or populations with similar insurance have demonstrated persistent health care disparities by race and/or income indicating that insurance alone does not eliminate disparities.8 The majority of our nation’s 44 million uninsured are white, but minority groups are disproportionately affected by the lack of health insurance.9 The uninsured rate for blacks is > 50% higher than for whites and the income gap between blacks and whites means that blacks are >3 times as likely as whites to live in poverty. Nearly 4 in 10 Latinos are uninsured even though the great majority of them are legal residents.9
Several studies lend support to the present study’s findings that race/ethnicity has a stronger effect or is equally important in terms of its influence on diagnostic delay than insurance status.10-14 This review focuses on breast cancer since the analysis of the present study was restricted to breast abnormalities, but some of the cited studies examined other cancers as well. Press et al. 10 found the median number of days to follow-up after an abnormal mammogram was greater for blacks (20 days) and Hispanics (21 days) compared with whites (14 days) in their study of 6722 women at a NYC medical center. These differences remained significant in a multivariable model controlling for insurance status among other relevant covariates.10
A study of 28,237 incident cancers in Florida in 1994 found that uninsured breast cancer cases were more likely to be diagnosed at a late stage than patients with insurance, and blacks and Hispanics were more likely to be diagnosed with late stage breast cancer than whites leading the authors to conclude that race differences in diagnostic stage are not explained by insurance coverage.11 When health plan status was held constant in a retrospective study of 476 white and 99 black women with newly diagnosed breast cancer from 2000-2004, blacks had a higher mortality rate (8.1%) and were diagnosed at later stages (OR=1.71, p=0.02) than whites (mortality rate 3.6%, p=0.06).12 Holding insurance status constant in their study of 49,865 female Medicare recipients, Gorin et al.13 also found that blacks compared to whites had a 1.39-fold odds (95% CI: 1.18, 1.63) of diagnostic delay >2 months and a 1.64-fold odds (95% CI: 1.40, 1.91) of treatment delay >1 month.13 A study of 1659 women found to have breast cancer through their participation in the CDC’s NBCCEDP program for uninsured women identified differences in median days from abnormal screening to diagnosis by race: whites = 29 days, blacks = 36 days, Hispanics = 38 days (p<0.0001).14
However, one study found that race is no longer significantly associated with diagnostic delay after controlling for other factors including insurance status and SES.15 This study examined 5719 Michigan women diagnosed with breast cancer with initial results indicating blacks had an increased risk of an unfavorable outcome than whites prior to performing the adjusted analysis.15 In a study investigating whether race/ethnicity, education, age, health insurance, and family history of breast cancer influenced adherence to recommended follow-up on screening mammography, initial results indicated that non-white women in each of the other racial/ethnic groups were less likely to adhere to recommendation than were white women (p<0.05).16 However, when these results were broken down for each racial group by age, education, insurance status, and family history of breast cancer, black un-/under-insured women were more likely to adhere to recommendation for follow-up after screening mammogram than white women (whites: 18.5%, RR=1.00; blacks: 29.1%, RR: 1.58 (95% CI: 1.16, 2.15)).16
The results of the present study combined with the brief literature review above tend to support the finding that having insurance does not always improve diagnostic delays for minority women with breast cancer. Interventions are needed to reduce the disparities between blacks and whites. A qualitative study of low income, ethnically diverse women aged over 40 years identified salient themes differentiating women who receive timely follow-up from those who did not.17 For women who delayed follow-up, prominent themes were dissatisfaction with result communication, disrespect on the part of providers and clinic staff, logistical barriers to access services, anxiety and fear about a possible cancer diagnosis, and lack of information about breast cancer screening and symptoms. Women who received timely care had themes showing appreciation of efforts by providers and clinic staff to support prompt follow-up, availability of social support facilitating appointment keeping, confidence in their ability to advocate for their health, and a high priority placed on self care.17
Another study that interviewed cancer survivors to assess their opinions on diagnostic delays and reasons for these delays found that the economically challenged (p=0.001) and those with public/government assisted healthcare (p=0.05) were more likely to report diagnostic delays.18 Waiting to seek medical attention after self detecting an abnormality was reported by 36% of breast cancer survivors and 34% of these indicated they waited because of fear of finding cancer.18 Neither cancer type nor ethnicity was related to the number of days to diagnostic care but Latinas reported greater diagnostic delays compared with other groups. Mean number of days delayed was 113 for those who cited fear, compared with 39 days for those who did not cite fear.18 The authors concluded that culturally and socioeconomically informed health education, cancer screening promotion, and medical care navigational services are needed for the delivery of comprehensive cancer care.18
A pilot study done at a hospital in Atlanta examined whether or not the use of community lay health advocates (CLHA) in promoting follow-up for abnormal mammograms would reduce the delay experienced by black women.19 CLHA support included encouragement of timely follow-up, appointment reminders, identification and removal of barriers to follow-up, and accompaniment to appointments. Women in the intervention group were significantly more likely than those not receiving the intervention to keep their appointments for first abnormal mammogram follow-up. In addition, the intervention group was significantly more likely to keep all their scheduled follow-up appointments and was significantly more likely to follow through with their biopsy or fine needle aspiration procedure than women in the non-intervention group.19
Similarly, an evaluation of a patient navigator intervention among inner-city women with abnormalities referred to an urban hospital-based diagnostic breast health practice from January to June 2000 (n=314 preintervention) and November 2001 to February 2003 (n=1018 intervention) found that the intervention group had 78% more timely follow-up versus the preintervention group (64%; p<0.0001).20 Timely follow-up in the adjusted model was associated with older age, having private insurance, having an abnormal mammogram, and being referred from a hospital-based practice.20
This present study examined the effect that health insurance, one barrier to accessing health care, had on diagnostic time. As discussed above, privately insured NHBs had significantly shorter diagnostic times than uninsured NHBs. However, NHBs and Hispanics had significantly longer diagnostic times than NHWs with equivalent insurance. The clear implication of these data is that lack of health insurance is not the only barrier to accessing a timely diagnostic resolution among NHBs and Hispanics in DC.
This present study highlights the need for identifying other barriers to accessing health care for NHBs and Hispanics. Once these barriers are known, the medical community and others will be able to work toward reducing and eliminating them. Intervention studies will provide additional insight into these barriers.
The women in this present study form part of the control group for an intervention study, the DC Citywide Patient Navigation Research Program (DC PNRP). DC is one of nine PNRP sites across the nation funded by NCI/ACS to evaluate the effectiveness of patient navigation in reducing disparities in breast cancer outcomes between whites versus other ethnic groups.4 The national PNRP study will also evaluate the influence of SES and insurance status among other potential barriers (e.g., transportation, co-pay, child-care, fear, medical mistrust, coping styles, and literacy) that could influence the delay in diagnosis and/or treatment. The national PNRP includes in its design the five principles for addressing disparities in cancer care: 1) recognizing disparities as a significant quality problem; 2) collecting relevant and reliable data; 3) stratifying performance measures by SES and race/ethnicity; 4) adjusting population-wide performance measures for SES and race/ethnicity; and 5) evaluation of the relationships between both SES and race/ethnicity with morbidity.21 The DC PNRP is specifically designed to reach out to the poor and underserved populations in DC. The results of the DC PNRP will provide insight into the causes of diagnosis and treatment delays among minority groups compared to NHWs.
Acknowledgments
SUPPORT: Grant Number 1 U01 CA116937 to Steven R. Patierno; Patient Navigation Research Program (PNRP), Center for Research on Cancer Health Disparities (CRCHD), National Cancer Institute (NCI).
Footnotes
FINANCIAL DISCLOSURES: None
REFERENCES
- 1.National Cancer Institute (NCI) State Cancer Profiles. National Cancer Institute (NCI) National Institutes of Health (NIH) U.S. Department of Health and Human Services (USDHHS); [accessed Jan. 14, 2010]. 2009. in conjunction with the Centers for Disease Control and Prevention. Available at: http://statecancerprofiles.cancer.gov. [Google Scholar]
- 2.Kaiser Family Foundation. D.C. Health Care Access Survey, Race, Ethnicity, and Health Care, Issue Brief. Kaiser Family Foundation. [accessed Jan. 2010]. Oct, 2003. Publication #6108. Available at: http://www.kff.org/minorityhealth/upload/D-C-Health-Care-Access-Survey-2003.pdf.
- 3.Lurie N, Gresenz CR, Blanchard JC, Ruder T, Chandra A, Ghosh-Dastidar B, Price A. Assessing Health and Health Care in the District of Columbia: Working Paper, Rand Health, Prepared for the Executive Office of the Mayor, District of Columbia. [accessed Jan. 14, 2010]. Jan, 2008. Available at: http://www.rand.org/pubs/working_papers/2008/RAND_WR534.pdf.
- 4.Patierno SR, LaVerda NL, Alexander LM, Levine PH, Young HA, Hoffman HJ. Longitudinal Network Patient Navigation: Development of a city-wide integrative model to reduce breast cancer disparities in Washington, DC. Oncology Issues. 2010;25:28–35. [Google Scholar]
- 5.Centers for Disease Control and Prevention National Breast and Cervical Cancer Early Detection Program (NBCCEDP), NBCCEDP Program Manual. [accessed August 22, 2010]. Available at: http://www.cancerutah.org/Healthcare_Provider/UCCP_policies/P&P_PDFs/NBCCEDP_policies_procedures.pdf.
- 6.Andrulis DP. Access to care is the centerpiece in the elimination of socioeconomic disparities in health. Ann Intern Med. 1998;129:412–416. doi: 10.7326/0003-4819-129-5-199809010-00012. [DOI] [PubMed] [Google Scholar]
- 7.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Affairs. 2005;24:398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 8.Meyers K. Issue Brief: Racial and ethnic health disparities. Kaiser Permanente Institute for Health Policy; Oakland, CA: 2007. [Google Scholar]
- 9.Morales J, Singh R. News Release. New report provides critical information about health insurance coverage and access for racial and ethnic minority groups; Most minority Americans are working yet lack job-based coverage. The Henry J. Kaiser Foundation; Menlo Park, CA: 2000. [Google Scholar]
- 10.Press R, Carrasquillo O, Sciacca RR, Giardina EGV. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J Women Health. 2008;17:923–930. doi: 10.1089/jwh.2007.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roetzheim RG, Pal N, Tennant C, Voti L, Ayanian JZ, Schwabe A, Krischer JP. Effects of health insurance and race on early detection of cancer. JNCI. 1999;91:1409–1415. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- 12.Short LJ, Fisher MD, Wahl PM, Kelly MB, Lawless GD, White S, Rodriguez NA, Willey VJ, Brawley OW. Disparities in medical care among commercially insured patients with newly diagnosed breast cancer: opportunities for intervention. Cancer. 2010;116:193–202. doi: 10.1002/cncr.24691. [DOI] [PubMed] [Google Scholar]
- 13.Gorin SS, Heck JE, Cheng B, Smith SJ. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med. 2006;166:2244–2252. doi: 10.1001/archinte.166.20.2244. [DOI] [PubMed] [Google Scholar]
- 14.Caplan LS, May DS, Richardson LC. Time to diagnosis and treatment of breast cancer: results from the national Breast and Cervical Cancer Early Detection Program, 1991-1995. Am J Public Health. 2000;90:130–134. doi: 10.2105/ajph.90.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. JNCI. 2002;94:490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 16.Strzelczyk JJ, Dignan MB. Disparities in adherence to recommended follow-up on screening mammography: interaction of sociodemographic factors. Ethn Dis. 2002;12:77–86. [PubMed] [Google Scholar]
- 17.Allen JD, Shelton RC, Harden E, Goldman RE. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: findings from a qualitative study. Patient Educ Couns. 2008;72:283–292. doi: 10.1016/j.pec.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 18.Ashing-Giwa KT, Gonzalez P, Lim JW, Chung C, Paz B, Somio G, Wakabayashi MT. Diagnostic and therapeutic delays among a multiethnic sample of breast and cervical cancer survivors. Cancer. 2010;116(13):3195–204. doi: 10.1002/cncr.25060. [DOI] [PubMed] [Google Scholar]
- 19.Crump SR, Shipp MP, McCray GG, Morris SJ, Okoli JA, Caplan LS, Thorne SL, Blumenthal DS. Abnormal mammogram follow-up: do community lay health advocates make a difference? Health Promot Pract. 2008;9:140–148. doi: 10.1177/1524839907312806. [DOI] [PubMed] [Google Scholar]
- 20.Battaglia TA, Roloff K, Posner MA, Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. A patient navigation intervention. Cancer. 2007;109(2 suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 21.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]


