Abstract
Objective
Little is known about whether large-scale environmental changes, such as those seen with urbanization, are differentially associated with systolic versus diastolic blood pressure, and whether those changes vary by birth cohort.
Methods
We used data from the China Health and Nutrition Survey, a population-based cohort study of Chinese adults (n=18,976; ages 18–70y) seen a maximum of 7 times over 1991–2009. We used hierarchical multivariable linear models to simultaneously estimate systolic and diastolic blood pressure as correlated outcomes over time, accounting for their physiologic, time-varying correlation. Main exposure variables were urbanicity, age, and birth cohort. Over 18 years of modernization, median systolic and diastolic blood pressure increased by 10 and 7 mm Hg, respectively.
Results
Our hierarchical model results suggest greater temporal increases in systolic and particularly diastolic blood pressure at lower versus higher urbanicity. At the same chronological age, for a 10-year difference in birth cohort (i.e., born in 1980s versus 1970s) the adjusted mean diastolic blood pressure was ~3mm Hg higher for the later birth cohort (p<0.001). Pulse pressure (calculated as model-predicted systolic minus diastolic blood pressure) was also higher at low versus high urbanicity.
Conclusions
These results suggest increased susceptibility of diastolic blood pressure (and thus peripheral vascular resistance) to environmental change, particularly in younger Chinese adults. Because diastolic blood pressure more strongly predicts cardiovascular disease risk in younger adulthood, hypertension-related health burden in China may increase over time.
Keywords: population, epidemiology, hypertension
Introduction
Hypertension, the greatest attributable risk factor for death worldwide, is defined by two distinct, yet correlated, measures of arterial function: systolic blood pressure (SBP) and diastolic blood pressure (DBP). Though correlated, SBP and DBP have different functions and clinical meaning: SBP reflects arterial stiffness and DBP reflects peripheral vascular resistance. SBP and DBP respond differentially to aging[1–6] and environmental exposures,[6, 7] and differentially predict cardiovascular disease (CVD) events across adulthood.[1–3, 8] Examining factors associated with hypertension, a single measure that combines SBP and DBP, may mask clinically meaningful findings.
Though CVD risk increases linearly with SBP and DBP, without evidence for threshold effects,[9] most studies examine SBP and DBP in combination via hypertension (SBP/DBP≥140/90 mm Hg), [10–13] rather than as quantitative traits. The few studies examining SBP and DBP as quantitative traits have generally used separate regression models,[4, 5] failing to account for physiologic correlation between SBP and DBP. Thus, current approaches do not address simultaneous and differential associations between exposure variables with SBP versus DBP, limiting clinical targets for intervention.
We capitalize upon unique longitudinal blood pressure data from the China Health and Nutrition Survey (CHNS) spanning 20 years of rapid urbanization to examine the associations between environment and cohort factors with SBP and DBP. We estimated SBP and DBP as simultaneous outcomes, accounting for their within-individual and time-varying correlation.
Our simultaneous modeling method has important implications for hypertension prevention and intervention because it allows us to estimate systolic and diastolic blood pressure as time-varying, correlated outcomes, accounting for their true physiologic relationship. This is important because SBP and DBP are distinct measures of CVD risk (representing arterial stiffness and peripheral vascular resistance, respectively), and each varies in how it predicts CVD risk at different ages. Since heretofore researchers have been unable to examine differential predictors of SBP versus DBP, little is known about the differential associations of environmental and/or lifestyle exposures with these two measures. Rather, the vast majority of research has examined measures that combine SBP and DBP (i.e., hypertension), leaving fundamental gaps in understanding about how environmental and lifestyle factors may differentially contribute to changes in SBP and DBP over time. Thus, our aim in the current paper is to examine estimated differential associations of environmental and/or lifestyle exposures with SBP or DBP while accounting for their time-varying correlation. Our findings inform tailored efforts to address arterial stiffness (SBP) and/or peripheral vascular resistance (DBP) as differential components of hypertension.
We hypothesized that age-related increases in SBP are greater in older versus younger cohorts, since SBP rapidly increases during late adulthood relative to other lifecycle periods;[7] we further hypothesized that secular increases in SBP and DBP occur in conjunction with environmental changes particularly in younger adults, who may be more likely than older adults to adopt modern lifestyle behaviors associated with hypertension.
Methods
CHNS
The CHNS is a longitudinal study of 228 communities within 9 Chinese provinces (Liaoning, Jiangsu, Shandong, Henan, Hubei, Hunan, Guangxi, Guizhou, and Heilongjiang). Nine surveys have occurred every 2–4 years between 1989–2011. The CHNS was designed to provide representation of rural, urban, and suburban areas varying substantially in geography, economic development, public resources, and health indicators and to focus on health during urbanization and economic change.[14] It is the only large-scale, longitudinal study of its kind in China. A multistage, random cluster design was used to select a stratified probability sample by province. Using this sampling strategy, two cities (one large and one small city usually the provincial capital and a lower income city) and four counties (stratified by income: one high, one low, and two middle income counties) were selected. Within cities, two urban and two suburban communities were selected; within counties, one community in the capital city and three rural villages were chosen, and then 20 households per community were randomly selected.
Ethics Statement
The study met the standards for the ethical treatment of participants and was approved by the Institutional Review Boards of the University of North Carolina at Chapel Hill and the Institute of Nutrition and Food Safety, Chinese Center for Disease Control and Prevention.
Sample
The eligible sample for analysis included 19,014 adults aged 18–70y for whom blood pressure was collected during at least one of the 1991, 1993, 1997, 2000, 2004, 2006, or 2009 exams (57,789 observations). Observations were excluded due to pregnancy at time of exam (total observations=344; 54 in 1991, 46 in 1993, 43 in 1997, 41 in 2000, 60 in 2004, 25 in 2006, and 75 in 2009) or missing covariates (total observations=1,508; 224 in 1991, 204 in 1993, 181 in 1997, 280 in 2000, 189 in 2004, 263 in 2006, and 167 in 2009) at multiple exams, resulting in an analytic sample of 18,754 individuals (55,937 observations) with complete covariate data for one to seven measurement occasions (mean number of exams: 4.2). Compared to the ~1% of participants (n=260 individuals) excluded due to missing data or pregnancy, the 18,754 individuals in the analytic sample were more likely to be women, have higher incomes, to have been previously pregnant (women), or to smoke (men).
Measurement of Dependent Variables
SBP and DBP were measured in triplicate at each survey using an appropriately-sized cuff from a standard mercury sphygmomanometer on the right arm after five-minute initial seated rest and 30-second interval between cuff inflations by experienced physicians. The mean value was used in analyses. Hypertension was defined at each survey year as a self-reported doctor diagnosis of hypertension, a measured mean SBP ≥140 mm Hg or mean DBP≥90 mm Hg.[7] Pulse pressure was defined as SBP minus DBP.
Measurement of Independent Variables
Age and birth year, sex, smoking status, and pregnancy status/history were self-reported at each survey. Alcohol consumption and dietary intake were collected via 3-day household food records which were calibrated to simultaneous, individual, 3 consecutive 24-hour recalls. A detailed weekly physical activity recall spanning one-year was used to measure multiple domains of physical activity. Metabolic equivalents of task (MET) hours per week were calculated for occupational and domestic activity using the Compendium of Physical Activity[15, 16]. Household income, derived from individual and household questionnaires, was inflated to 2009 Yuan currency in analysis for comparability over time. Height and weight were measured at each survey without shoes and in light clothing using a portable Seca stadiometer and on a calibrated floor scale (Seca Zhong Guo, Hangzhou, China). In descriptive analysis, we include the prevalence of overweight according to the World Health Organization,[17] Asian,[18] and Chinese[19] cut points.
Urbanicity reflects the degree of modernization of each of the communities at each survey period. Urbanicity was assessed using individual and community-level survey items from which a multicomponent scale was created representing infrastructure, economic, and social service domains.[20] The scale was developed specifically for the CHNS and has high reliability, validity, and temporal stability,[20] with a possible range of 0–120 (higher score reflects more “urban” characteristics across multiple domains). There is low residential mobility in our sample, and thus our time-varying measure reflects urbanization-related changes occuring in each community, or length of stay in an urban environment for individuals with high urbanicity and no change over time. We entered urbanicity as a time-varying, continuous, cubic polynomial in models.
Statistical Analysis
All descriptive analyses were conducted in Stata 13 (Stata Corp, College Station, TX, USA). Statistical models and tests were administered in SAS 9.2 (SAS, Cary, NC, USA). In descriptive analyses, we examined individual- and household-level characteristics in 1991 and 2009 (the first and last waves of the survey) according to tertiles of urbanicity (low, medium, and high) and gender.
We modeled SBP and DBP simultaneously because of their inherent interdependence and because of an interest in determining whether covariates differentially influenced SBP and DBP. Hierarchical multivariable linear models simultaneously estimated SBP and DBP as two correlated outcomes over time (proc mixed) with random effects at the province, community, and individual levels to account for both the data structure and the dependence of the outcome within individuals over time. We jointly estimated a within-subject residual covariance characterized by the Kronecker product of an unstructured matrix for blood pressure type (SBP or DBP) and an unstructured matrix over time (1991, 1993, 1997, 2000, 2004, 2006, or 2009), allowing variances of SBP and DBP to change with time as well as a time-varying correlation between SBP and DBP. Our sex-stratified model contained separate parameters for the SBP and DBP mean functions (i.e., each covariate had distinct parameters capturing separate associations with SBP and DBP). The mean functions for SBP and DBP included household income, current smoking status (yes versus no; men only, given low [~4%] prevalence in women), ever pregnant (yes versus no; women only), time, birth cohort (categorized into decade of birth [1930s, 1940s, 1950s, 1960s, 1970s, or 1980s]; 1930s includes 832 individuals born between 1921–1930, and 1980s includes 43 individuals born in 1990–1991 due to small sample in those decades), urbanicity, and interactions between time, birth cohort, and urbanicity (detailed description in Supplemental Methods). We conducted Wald tests for the inclusion of specific combinations of polynomial and interaction terms, and contrasts of model coefficients, with significance set at p=0.05. Birth cohort by urbanicity interaction terms were statistically significant for both sexes (p<0.01), thus all were retained.
Sensitivity Analysis
We conducted several sensitivity analyses to examine 1) inclusion of body mass index (BMI) in statistical models, 2) whether findings were affected by the use of hypertension medication, 3) differences according to classification of urbanicity, and 4) model results for the subset of individuals with complete data across all seven exam visits (details and results in Supplemental Methods).
Presentation of results
To facilitate interpretations from our simultaneous model, we used model coefficients to predict mean SBP and DBP at specified, well-represented levels of key covariates: low (25th percentile) and high (75th percentile) urbanicity, and for the 1940s (25th percentile) and 1970s (75th percentile) birth cohorts. Because mean urbanicity increased over time, we compared the 75th (high) and 25th (low) percentile of the urbanicity scale at each survey wave to examine relative urbanicity. All control variables were predicted at sample median or referent levels. We used model-predicted SBP and DBP to derive adjusted pulse pressure (SBP minus DBP), which we present at low and high urbanicity for the 1940s and 1970s birth cohorts. We calculated Wald test statistics and p values to compare the adjusted mean SBP and DBP levels for these specific contrasts.
Results
In Chinese adults aged 18–70y, median SBP and DBP increased over time for men and women between 1991 and 2009 (Tables 1 and 2). Differences in SBP and DBP according to urbanicity were particularly apparent for men in 1991, though these differences narrowed considerably over the survey period. The crude prevalence of hypertension (SBP/DBP≥140/90 mmHg or doctor diagnosis) doubled from 13% in 1991 to ~26% in 2009 concurrent with increasing urbanicity (Table 1). SBP and DBP were higher in older adults at all survey years (Supplemental Table 1).
Table 1.
Median (IQR) or Percent (SE) for sample characteristics according to urbanicity level in men (China Health and Nutrition Survey)
| 1991 | 2009 | |||||
|---|---|---|---|---|---|---|
| Low | Medium Urbanicity* | High | Low | Medium Urbanicity* | High | |
| N | 1287 | 1208 | 1238 | 1335 | 1304 | 1290 |
| Descriptive Statistics | ||||||
| Age (years) (median,SE) | 37.7 (26.5, 48.2) | 36.8 (27.9, 47.0) | 38.9 (28.7, 54.7) | 46.7 (37.7, 57.6) | 47.1 (37.9, 57.2) | 48.3 (38.8, 57.5) |
| BMI (kg/m2) (median,SE) | 20.6 (19.4, 22.1) | 21.1 (19.8, 22.8) | 21.8 (19.9, 23.9) | 22.5 (20.7, 24.9) | 23.2 (20.9, 25.7) | 23.8 (21.6, 25.9) |
| Income (1000 Yuan) † (median,SE) | 10.5 (6.8, 15.3) | 12.0 (7.6, 19.5) | 13.4 (9.8, 19.1) | 28.4 (16.4, 49.1) | 32.9 (17.9, 54.9) | 36.5 (21.9, 60.0) |
| Urbanicity* (median,SE) | 28.8 (25.4, 32.1) | 44.5 (41.3, 50.9) | 63.9 (61.0, 68.4) | 47.2 (40.3, 50.9) | 64.2 (58.7, 71.5) | 89.6 (84.7, 93.0) |
| SBP (mm Hg) (median,SE) | 110.0 (103.3, 120.0) | 113.3 (105.3, 121.3) | 118.0 (109.3, 127.3) | 120.7 (112.0, 131.0) | 121.0 (112.7, 131.3) | 121.3 (114.7, 131.3) |
| DBP (mm Hg) (median,SE) | 74.0 (68.0, 80.0) | 75.0 (70.0, 80.0) | 78.0 (70.0, 83.3) | 80.0 (75.3, 89.0) | 80.0 (74.7, 89.3) | 80.7 (77.3, 88.0) |
| Hypertension, % (SE)‡ | 8.9 (0.8) | 13.7 (1.0) | 21.7 (1.2) | 27.6 (1.2) | 30.4 (1.3) | 30.5 (1.3) |
| Current smokers, % (SE) | 72.1 (1.3) | 67.8 (1.3) | 64.0 (1.4) | 60.4 (1.3) | 56.2 (1.4) | 54.3 (1.4) |
| Infrequent Alcohol Consumption, % (SE)§ | 25.4 (1.2) | 18.6 (1.1) | 20.7 (1.2) | 20.3 (1.1) | 17.0 (1.0) | 21.4 (1.1) |
| Frequent Alcohol Consumption, % (SE)|| | 40.0 (1.4) | 50.0 (1.4) | 40.0 (1.4) | 40.0 (1.4) | 40.0 (1.4) | 40.0 (1.4) |
| Sodium Intake (g/day)¶ (median,SE) | 6.3 (4.4, 9.0) | 6.8 (4.8, 9.2) | 5.7 (3.8, 8.3) | 4.4 (3.2, 6.1) | 4.3 (3.2, 5.9) | 4.3 (3.1, 5.9) |
| Seafood Intake (g/day)¶ (median,SE) | 0.0 (0.0, 0.0) | 0.0 (0.0, 33.3) | 8.3 (0.0, 66.7) | 0.0 (0.0, 0.0) | 0.0 (0.0, 66.7) | 33.3 (0.0, 83.3) |
| Fruit & Vegetable Intake (g/day)¶ (median,SE) | 350.0 (233.3, 483.3) | 316.7 (216.7, 450.0) | 283.3 (200.0, 383.3) | 373.3 (260.0, 503.3) | 343.3 (238.3, 463.3) | 380.0 (266.7, 498.3) |
| Physical Activity (MET-hours/week)** (median,SE) | 524.7 (400.0, 641.4) | 408.0 (244.9, 563.1) | 180.0 (100.0, 255.4) | 355.5 (266.2, 462.1) | 214.5 (103.5, 361.3) | 120.0 (29.4, 210.0) |
| Overweight/Obesity using three different classifications | ||||||
| WHO17 [≥25 kg/m2], % (SE) | 4.0 (0.5) | 8.6 (0.8) | 17.8 (1.1) | 24.1 (1.2) | 32.0 (1.3) | 34.1 (1.3) |
| China18 [≥24 kg/m2], % (SE) | 14.5 (1.0) | 22.9 (1.2) | 34.7 (1.4) | 43.2 (1.4) | 53.1 (1.4) | 59.2 (1.4) |
| Asian19 [≥23 kg/m2], % (SE) | 14.5 (1.0) | 22.9 (1.2) | 34.7 (1.4) | 43.2 (1.4) | 53.1 (1.4) | 59.2 (1.4) |
Urbanicity is defined by tertiles of a 12-component index (range: 0–120) based upon community-level features, which define and distinguish urbanicity in China.
Annual household income inflated to 2009 Yuan currency values.
Hypertension is defined as SBP/DBP ≥140/90 mm Hg or doctor diagnosed hypertension.
Infrequent alcohol consumption is defined as <1 alcoholic beverage per week.
Frequent alcohol consumption defined as 1 or more alcoholic beverages per week.
Sodium, fruit & vegetable, and fish intake data were collected by 3-day household food records, calibrated with 3 days of simultaneous, individual 24-hour recalls.
Physical activity defined by self-reported time and intensity of domestic and occupational physical activity at each survey.
Abbreviations: BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; IQR, interquartile range; SE, standard error; WHO, World Health Organization
Table 2.
Median (IQR) or Percent (SE) for sample characteristics according to urbanicity level in women (China Health and Nutrition Survey)
| 1991 | 2009 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Low Urbanicity* | Medium Urbanicity* | High Urbanicity* | Low Urbanicity* | Medium Urbanicity* | High Urbanicity* | |
| N | 1395 | 1406 | 1395 | 1417 | 1406 | 1433 |
| Descriptive Statistics | ||||||
| Age (years) (median,SE) | 37.9 (27.5, 47.9) | 36.4 (27.9, 46.5) | 38.4 (28.4, 53.7) | 46.9 (38.4, 57.5) | 47.3 (38.2, 56.1) | 48.2 (38.8, 57.6) |
| BMI (kg/m2) (median,SE) | 21.0 (19.5, 22.9) | 21.5 (19.9, 23.5) | 22.0 (19.9, 24.5) | 22.9 (20.8, 25.5) | 23.0 (21.1, 25.7) | 23.1 (20.8, 25.4) |
| Income (1000 Yuan) † (median,SE) | 10.6 (6.8, 15.6) | 11.8 (7.5, 18.6) | 13.4 (9.8, 18.9) | 27.3 (15.4, 45.4) | 32.0 (16.8, 54.3) | 35.7 (20.7, 59.1) |
| Urbanicity* (median,SE) | 28.8 (24.9, 32.1) | 44.5 (41.3, 50.9) | 64.5 (61.0, 68.4) | 47.2 (40.3, 50.9) | 64.1 (58.5, 71.1) | 89.6 (84.7, 93.0) |
| SBP (mm Hg) (median,SE) | 108.0 (100.0, 120.0) | 110.0 (100.0, 120.0) | 110.0 (100.0, 120.7) | 120.0 (110.0, 130.0) | 120.0 (110.0, 130.0) | 119.3 (109.3, 130.0) |
| DBP (mm Hg) (median,SE) | 70.0 (62.0, 78.3) | 70.7 (66.0, 80.0) | 72.3 (67.3, 80.0) | 79.3 (70.0, 83.3) | 79.3 (70.0, 84.7) | 79.3 (70.7, 84.0) |
| Hypertension, % (SE)‡ | 7.3 (0.7) | 11.6 (0.9) | 15.7 (1.0) | 22.6 (1.1) | 24.3 (1.1) | 24.1 (1.1) |
| Current smokers, % (SE) | 2.1 (0.4) | 4.6 (0.6) | 4.6 (0.6) | 5.2 (0.6) | 2.3 (0.4) | 1.7 (0.3) |
| Infrequent Alcohol Consumption, % (SE)§ | 7.2 (0.7) | 6.9 (0.7) | 9.4 (0.8) | 4.0 (0.5) | 4.8 (0.6) | 8.0 (0.7) |
| Frequent Alcohol Consumption, % (SE)|| | 0.0 (0.5) | 0.0 (0.5) | 0.0 (0.5) | 0.0 (0.5) | 0.0 (0.5) | 0.0 (0.5) |
| Sodium Intake (g/day)¶ (median,SE) | 6.3 (4.4, 8.5) | 6.3 (4.6, 8.7) | 5.3 (3.6, 7.6) | 4.1 (3.0, 5.5) | 3.9 (2.9, 5.4) | 3.9 (2.9, 5.5) |
| Seafood Intake (g/day)¶ (median,SE) | 0.0 (0.0, 0.0) | 0.0 (0.0, 30.0) | 0.0 (0.0, 50.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 50.0) | 33.3 (0.0, 66.7) |
| Fruit & Vegetable Intake (g/day)¶ (median,SE) | 333.3 (228.3, 466.7) | 300.0 (200.0, 433.3) | 266.7 (193.1, 366.7) | 360.0 (236.7, 483.3) | 326.7 (220.0, 450.0) | 370.0 (268.3, 496.7) |
| Physical Activity (MET-hours/week)**(median,SE) | 636.0 (501.5, 762.0) | 488.1 (277.8, 670.4) | 163.9 (93.6, 300.0) | 360.2 (133.6, 474.5) | 198.2 (48.3, 374.2) | 100.0 (19.3, 154.9) |
| Overweight/Obesity using three different classifications | ||||||
| WHO17 [≥25 kg/m2], % (SE) | 8.4 (0.7) | 15.3 (1.0) | 20.9 (1.1) | 28.9 (1.2) | 30.2 (1.2) | 28.7 (1.2) |
| China18 [≥24 kg/m2], % (SE) | 24.0 (1.1) | 30.9 (1.2) | 39.6 (1.3) | 49.3 (1.3) | 50.3 (1.3) | 51.1 (1.3) |
| Asian19 [≥23 kg/m2], % (SE) | 24.0 (1.1) | 30.9 (1.2) | 39.6 (1.3) | 49.3 (1.3) | 50.3 (1.3) | 51.1 (1.3) |
Urbanicity is defined by tertiles of a 12-component index (range: 0–120) based upon community-level features which define and distinguish urbanicity in China.
Annual household income inflated to 2009 Yuan currency values.
Hypertension is defined as SBP/DBP ≥ 140/90 mm Hg or doctor diagnosed hypertension.
Infrequent alcohol consumption is defined as <1 alcoholic beverage per week.
Frequent alcohol consumption defined as 1 or more alcoholic beverages per week.
Sodium, fruit & vegetable, and fish intake data were collected by 3-day household food records, calibrated with 3 days of simultaneous, individual 24-hour recalls.
Physical activity defined by self-reported time and intensity of domestic and occupational physical activity at each survey.
Abbreviations: BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; IQR, interquartile range; SE, standard error; WHO, World Health Organization
From the simultaneous, multilevel models, Wald tests of combined coefficients (Supplemental Table 2) suggest that DBP increased with age (p<0.001 for all birth cohort by time interaction terms) and differed more by urbanicity level for earlier versus later cohorts (older versus younger in 2009; p<0.01 for interaction between all urbanicity and birth cohort terms). Men and women who lived in communities of lower urbanicity had greater predicted increase in DBP over time (p<0.05 for urbanicity and time interaction terms). We observed greater temporal increase in SBP in earlier versus later birth cohorts (younger versus older in 2009; p<0.001 for all birth cohort by time interaction terms). Except for younger adult men, SBP increased more with age at lower versus higher urbanicity (p<0.05 for all urbanicity and birth cohort interaction terms). Model-based correlation between SBP and DBP at each survey (~0.68 women, 0.70 men) was higher than correlation between two different surveys for DBP (men: ranging from 0.21 to 0.39; women: ranging from 0.24 to 0.41) or SBP (men: ranging from 0.1 to 0.36; women: ranging from 0.20 to 0.39) [not shown].
Model-adjusted changes in SBP and DBP with age for two different cohorts
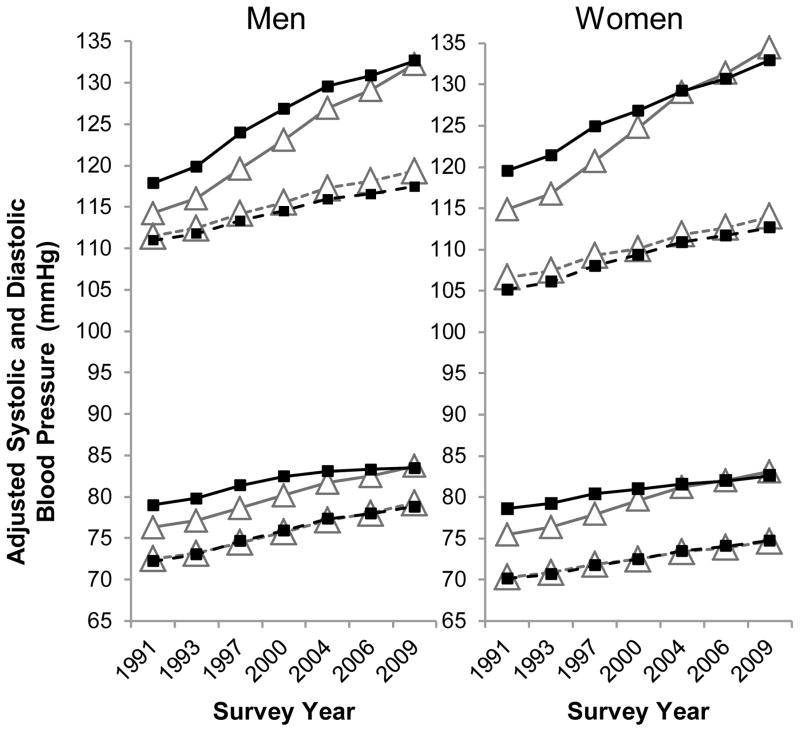
Using the coefficients from Supplemental Table 2, Figure 1 shows that the difference in DBP (men and women), and SBP (women) at high (75th percentile) versus low (25th percentile) urbanicity narrowed over time for the 1940s cohort (p<0.05; Supplemental Table 4). Differences in DBP by urbanicity were smaller for the 1970s cohort (p>0.05; Supplemental Table 4).
Figure 1. Model-predicted SBP and DBP in adults (18–70y): the China Health and Nutrition Survey.
Sex-stratified models show 1940s (solid lines) and 1970s (dashed lines) birth cohorts by urbanicity at each survey year: low (grey lines with triangle markers; 25th percentile) or high (black lines with square markers; 75th percentile). Adjusted for time, smoking (men), parity (women), alcohol consumption, and income.
Abbreviations: SBP: systolic blood pressure; DBP: diastolic blood pressure
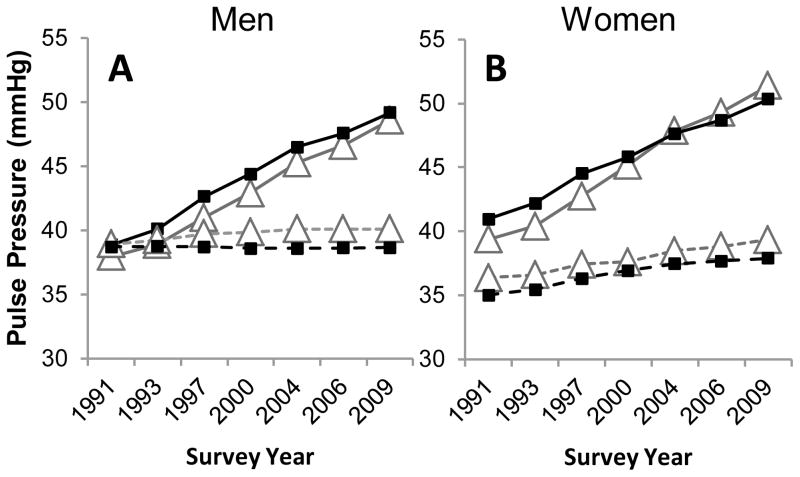
Model-adjusted changes in pulse pressure with time for two different cohorts
Pulse pressure (model-predicted systolic minus diastolic blood pressure) increased more in the 1940s than 1970s cohort (Figure 2). Temporal increase in pulse pressure was greater, albeit not statistically significantly, at low (versus high) urbanicity, particularly for earlier birth cohorts (Supplemental Table 4).
Figure 2. Adjusted pulse pressure derived from the simultaneous SBP-DBP model: the China Health and Nutrition Survey.
Pulse pressure calculated from sex-stratified regression models as systolic minus diastolic blood pressure. 1940s (solid) and 1970s (dashed) birth cohorts by urbanicity at each survey year: low (grey with triangle markers; 25th percentile) or high (black with square markers; 75th percentile). Adjusted for time, smoking (men), parity (women), alcohol consumption, and income.
Abbreviations: SBP: systolic blood pressure; DBP: diastolic blood pressure
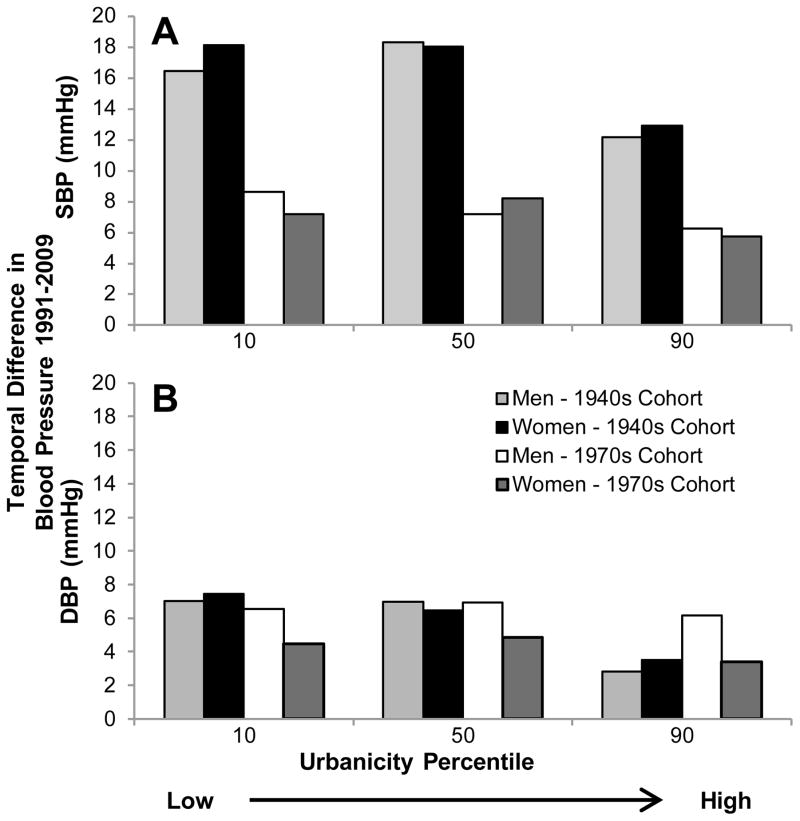
Difference in mean SBP and DBP between 1991 and 2009 according to level of urbanicity, gender, and cohort
Higher urbanicity was associated with smaller temporal increases in DBP for women across birth cohorts (negative coefficient for urbanicity, birth cohort, and time interaction terms; Supplemental Table 2); this association was similar, albeit smaller, for DBP in men. Using model coefficients from Supplemental Tables 2 and 3, the predicted difference in SBP (2009 minus 1991 values) was larger at lower urbanicity than higher urbanicity for the 1940s versus 1970s birth cohort (Figure 3). For men, cohort differences in DBP were negligible at lower urbanicity, but not at higher urbanicity (Supplemental Table 5). The opposite was true for women: cohort differences in DBP were negligible at higher urbanicity, but not at lower urbanicity (Supplemental Table 5).
Figure 3. Temporal difference in SBP and DBP from 1991–2009: the China Health and Nutrition Survey.
Adjusted for time, smoking (men), parity (women), alcohol consumption, and income. Predictions based on the urbanicity scale distribution in 1991 and 2009 (e.g., DBP at the 90th percentile of urbanicity in 2009 minus DBP at the 90th percentile of urbanicity in 1991).
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
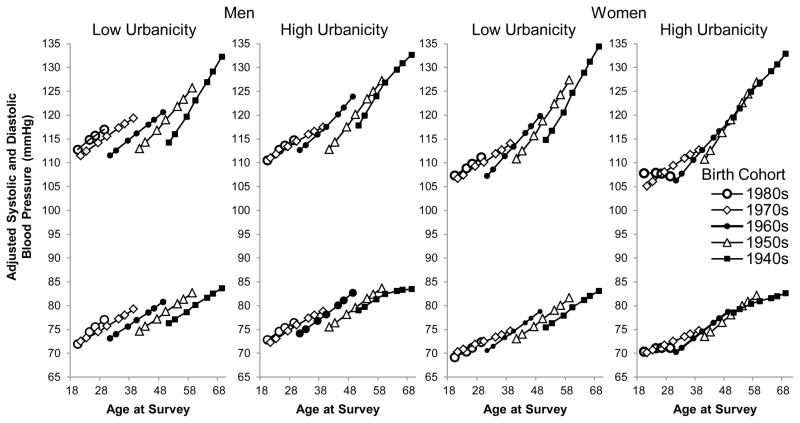
Model-adjusted changes in DBP and SBP with age according to birth cohort and urbanicity
In Figure 4, slopes for DBP and SBP by age and birth cohort illustrate secular and cohort effects. For men at low (25th percentile) urbanicity, even at the same age, later birth cohorts (younger in 2009) had consistently higher SBP and DBP than earlier birth cohorts (e.g., SBP was 3.6 mm Hg higher for men aged 40 if they were born in the 1970s versus 1960s). Men from later birth cohorts had larger temporal increases in DBP and smaller temporal increases in SBP over time compared to earlier birth cohorts, even at the same age (Supplemental Table 5). Findings were similar for women, albeit with statistical significance only at low urbanicity (Supplemental Table 5).
Figure 4. Model-predicted SBP and DBP in adults aged 18–70y: the China Health and Nutrition Survey.
Adjusted for time, smoking (men), parity (women), alcohol consumption, and income. Cohorts defined by decade of birth. The differences between lines at any given age at survey represent differences by birth cohort. The urbanicity scale distribution at each wave defined low (25th percentile) and high (75th percentile) urbanicity.
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure
Model-adjusted changes in DBP and SBP according to lifestyle factors
From statistical models, smoking status was negatively associated with DBP and SBP in men (p<0.05). Infrequent alcohol consumption was negatively associated with SBP and DBP in men and women (p<0.05), while more frequent alcohol consumption was positively associated with SBP and DBP in men (p<0.05). Though income increased over the survey period it was not significantly associated with SBP or DBP in men or women.
Sensitivity Analysis
In sensitivity analyses, urbanicity was associated with SBP and DBP even after control for BMI (Supplemental Figures 1–4). Results did not differ when baseline and change in urbanization were modeled (Supplemental Figure 5), rather than average urbanization (Figure 3). Model results and predictions were similar in magnitude in models excluding individuals on hypertension medication (results not shown). We found smaller cohort differences in the subsample of respondents seen all 7 exam years versus the full analytic sample (results not shown).
Discussion
In the context of a rapidly urbanizing environment, we sought to understand how environmental and cohort factors were differentially associated with SBP and DBP across adulthood illuminating important population targets for CVD prevention. We found that even at the same chronological age, later cohorts (i.e., born in 1980 versus 1970) had higher DBP and larger temporal increase in DBP than earlier cohorts, highlighting the malleability of DBP over the course of urbanization. In addition, greater temporal and secular increases in SBP and DBP at lower versus higher urbanicity across adulthood suggest comparatively higher CVD risk in less urban areas. Together, our findings suggest that environmental change has the potential to differentially influence DBP and SBP, and may have greater impact on DBP, a marker of peripheral vascular resistance.
While high blood pressure is the number one attributable risk factor for death worldwide, it is also potentially highly modifiable throughout the life course.[7, 8, 21, 22] In developed countries that experienced slow rates of modernization, studies have suggested declines or leveling off in mean blood pressure over the last century, potentially due to increased hypertension treatment.[4, 5, 23, 24] However, in China during a period of rapid modernization, we observed a substantial increase in mean SBP and DBP over time, particularly in low urbanicity areas. From 1991 to 2009, increases in SBP and DBP for the 1940s (versus 1970s) birth cohort were approximately 3–4mm Hg higher at low versus high urbanicity. Similar differences in SBP and DBP are observed when individuals adopt a low-salt diet[7] or lose 5–10% of their body weight.[25, 26]
In our analysis, we examined SBP and DBP as quantitative traits, addressing major limitations of using hypertension as an outcome measure. We avoid potential threshold effects related to hypertension cut points[7] and estimate independent associations between urbanicity, age, and cohort with SBP and DBP over time, while accounting for their physiologic correlation. SBP and DBP inter-correlation differs within individuals and over time[1–3, 6] (e.g., SBP increases throughout adulthood, while DBP stabilizes or decreases around age 50y), however, studies that examine SBP and DBP independently in separate regression models[4, 5] or within strata of one or the other,[6] do not account for this correlation. From our models, men in the 1970s cohort had a slightly larger mean increase in DBP versus SBP over 1991–2009 (4.5 mmHg). For the same level of increase, DBP more strongly predicts CVD than SBP in men <60y,[1, 7] thus, we posit that young adult men in this sample are at increased risk of CVD due to higher peripheral vascular resistance.
Our findings relative to differential estimated effects of SBP and DBP provide insights into physiologic responses to environmental change and age-related associations, as well as future CVD risk. From our simultaneous model, we compared cohort differences in SBP and DBP at the same biological age, finding that later birth cohorts had comparatively smaller increases in SBP and similar, if not larger, increases in DBP than earlier birth cohorts. We observed greater secular increase in DBP than SBP in response to urbanization, particularly in young adulthood, which is consistent with findings from a longitudinal study of US adults that examined SBP and DBP in separate hierarchical models.[6] Model-adjusted pulse pressure (SBP minus DBP), a measure of left ventricular ejection fraction, large-artery stiffness, and early pulse wave reduction[1] was higher at low versus high urbanicity across all cohorts. Together, these findings suggest that DBP (and thus peripheral resistance) is more responsive than SBP (and thus arterial stiffness) to environmental change, and that higher pulse pressure levels at lower urbanicity may be due to effects on peripheral vasculature, rather than central vasculature or cardiac output.
With the unique experience of a cohort of Chinese adults undergoing rapid urbanization and environmental change,[10, 20] we gain insight into the association between age, birth cohort, and environment with SBP and DBP over time. Lifestyle behaviors also changed considerably during the survey period. Over the past 30 years of modernization, CVD risk factors have become more prevalent in China,[10, 16, 27–29] particularly in high urbanicity areas.[20, 30–32] However, recent research suggest increasing risk of CVD in less urban areas.[31, 33] Our study contributes to this body of evidence and suggests the need for expansion of CVD prevention, screening, and treatment to rural areas and to young adults, who are not typically seen as ‘at high risk’ of hypertension or CVD.
We controlled for a host of economic and lifestyle factors in addition to urbanization, age, and cohort. We found that consistent with previous studies,[34, 35] being a current smoker versus non-smoker was negatively associated with DBP and SBP in men, potentially because chronic smoking has a depressant effect on the autonomic nervous system.[34] Also similar to the previous literature, infrequent/moderate alcohol consumption was negatively associated with SBP and DBP[36], while more frequent alcohol consumption was positively associated with SBP and DBP.[37] These associations, while statistically significant, were relatively small when compared to the observed associations between age, cohort, and urbanicity with SBP and DBP. Lastly, in our sensitivity analysis, we found that BMI was positively associated with absolute SBP and DBP in men and women. It is well established that higher BMI is associated with higher SBP and DBP due to greater cardiac output and vascular resistance with increased weight,[38] however, even with BMI in the models, associations of urbanicity and cohort with SBP and DBP were still present, suggesting the possibility of environmental effects on blood pressure that go above and beyond the effects of lifestyle factors alone.
Our study has some limitations. We do not address early life factors that might be relevant to the observed differences across birth cohorts.[24] However, we report differential increases in SBP and DBP across a wide age range (18–70y) and across six decades of birth cohorts. Age restrictions for the analytic sample, original survey sampling design, and loss to follow up meant that we do not have the full 7 observations for each individual. In sensitivity analysis, we restricted the sample to the 2,738 participants seen at all 7 occasions, and did not find differences in the magnitude of association between urbanization and age with SBP and DBP for the full versus reduced sample. Previous work from our group has found limited bias due to sample participation at each survey wave of the CHNS.[39] While the CHNS is not nationally representative of China, the sampling design encompassed communities with variation in geography, level of urbanization, and economic structure; this diversity is unique to the CHNS and is what makes this analysis possible. As we were not conducting etiologic modeling, we did not address lifestyle behaviors or effects of urbanization. Rather, we focused on marginal associations by urbanicity, age, and birth cohort with SBP and DBP over time. Lastly, though we make use of the most widely-measured and predictive markers of CVD (SBP, DBP, and pulse pressure), we were unable to examine other markers, such as pulse rate, that are related to CVD outcomes independent of blood pressure,[40] and could provide further insight into associations between environment and physiology. Despite these limitations, our study uses a sophisticated modeling strategy that accounts for within-individual SBP-DBP correlation, providing a new paradigm for examining heterogeneous biological, environmental, and behavioral determinants of SBP and DBP. We measure urbanization using a scale that captures diverse changes across community-level services, infrastructure, economic factors, and food and health markets over time, improving upon standard demographic urban-rural dichotomous measures.
In sum, temporal increases in SBP, DBP, and pulse pressure were greater in low relative to high urban areas. Even at the same chronological age, later cohorts (i.e., born in 1980 versus 1970) had higher DBP and larger temporal increase in DBP than earlier cohorts. These findings suggest that DBP is particularly responsive to environmental change. Our work highlights the need to increase prevention of, and screening for, hypertension in rural areas of China and across low and middle income countries facing equally rapid modernization and urbanization.
Supplementary Material
Acknowledgments
We are grateful to Nora Franceschini, MD for her helpful advice regarding etiological differences in SBP and DBP.
Funding Sources: This work was supported by NIH: NIDDK (R21DK089306) and NHLBI (R01-HL108427). NIH had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. This research uses data from the China Health and Nutrition Survey, funded by NIH: NICHD (R01-HD30880), although no direct support was received from grant for this analysis. We also are grateful to the Carolina Population Center (R24 HD050924) for general support.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
Author Contributions: SMA and PG-L were responsible for conception and design of the study. BZ, SD, and BMP contributed to data collection. SMA and AHH contributed to data analysis, and SMA, BMP, and PG-L contributed to data interpretation. SMA and PG-L wrote the first draft of the manuscript, and all authors contributed to revision and approval of the final manuscript.
Disclosures: None.
References
- 1.Sesso HD, Stampfer MJ, Rosner B, Hennekens CH, Gaziano JM, Manson JE, Glynn RJ. Systolic and diastolic blood pressure, pulse pressure, and mean arterial pressure as predictors of cardiovascular disease risk in men. Hypertension. 2000;36:801–7. doi: 10.1161/01.hyp.36.5.801. [DOI] [PubMed] [Google Scholar]
- 2.Franklin SS, Lopez VA, Wong ND, Mitchell GF, Larson MG, Vasan RS, Levy D. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119:243–50. doi: 10.1161/CIRCULATIONAHA.108.797936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benetos A, Thomas F, Safar ME, Bean KE, Guize L. Should diastolic and systolic blood pressure be considered for cardiovascular risk evaluation: A study in middle-aged men and women. J Am Coll Cardiol. 2001;37:163–8. doi: 10.1016/s0735-1097(00)01092-5. [DOI] [PubMed] [Google Scholar]
- 4.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–50. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 5.Luepker RV, Steffen LM, Jacobs DR, Jr, Zhou X, Blackburn H. Trends in blood pressure and hypertension detection, treatment, and control 1980 to 2009: the Minnesota Heart Survey. Circulation. 2012;126:1852–7. doi: 10.1161/CIRCULATIONAHA.112.098517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choh AC, Nahhas RW, Lee M, Choi YS, Chumlea WC, Duren DL, et al. Secular trends in blood pressure during early-to-middle adulthood: the Fels Longitudinal Study. J Hypertens. 2011;29:838–45. doi: 10.1097/HJH.0b013e328344da30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 8.Stokes J, 3rd, Kannel W, Wolf P, D’Agostino R, Cupples L. Blood pressure as a risk factor for cardiovascular disease. The Framingham Study -- 30 years of follow-up. Hypertension. 1989;13:I13–8. doi: 10.1161/01.hyp.13.5_suppl.i13. [DOI] [PubMed] [Google Scholar]
- 9.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 10.Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, Remais JV. Urbanisation and health in China. Lancet. 2012;379:843–52. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, et al. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension. 2002;40:920–7. doi: 10.1161/01.hyp.0000040263.94619.d5. [DOI] [PubMed] [Google Scholar]
- 12.Ueshima H, Zhang X-H, Choudhury S. Epidemiology of hypertension in China and Japan. J Hum Hypertens. 2000;14:765–9. doi: 10.1038/sj.jhh.1001054. [DOI] [PubMed] [Google Scholar]
- 13.Zhao Y, Lu F, Sun H, Liu Z, Zhao Y, Sun S, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in Shandong Province of China. J Clin Hypertens (Greenwich) 2012;14:637–43. doi: 10.1111/j.1751-7176.2012.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39:1435–40. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 16.Ng SW, Norton EC, Popkin BM. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc Sci Med. 2010;68:1305–14. doi: 10.1016/j.socscimed.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Expert Committee on Physical Status. Physical Status: the use and interpretation of anthropometry: Technical Report Series 854. Geneva: 1995. [PubMed] [Google Scholar]
- 18.WHO Expert Consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 19.Chen C, Lu FC Department of Disease Control Ministry of Health PRC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36. [PubMed] [Google Scholar]
- 20.Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med. 2010;71:1436–46. doi: 10.1016/j.socscimed.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–9. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Global Status Report on noncommunicable diseases 2010. 2011 [Google Scholar]
- 23.Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26:60–9. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- 24.McCarron P, Okasha M, McEwen J, Smith GD. Changes in blood pressure among students attending Glasgow University between 1948 and 1968: analyses of cross sectional surveys. Br Med J. 2001;322:885–8. doi: 10.1136/bmj.322.7291.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Look AHEAD Research Group. Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566–75. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Horvath K, Jeitler K, Siering U, Stich AK, Skipka G, Gratzer TW, Siebenhofer A. Long-term effects of weight-reducing interventions in hypertensive patients: systematic review and meta-analysis. Arch Intern Med. 2008;168:571–80. doi: 10.1001/archinte.168.6.571. [DOI] [PubMed] [Google Scholar]
- 27.Popkin BM. Urbanization, Lifestyle Changes and the Nutrition Transition. World Development. 1999;27:1905–16. [Google Scholar]
- 28.Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49:509–38. [PubMed] [Google Scholar]
- 29.Raymond SU, Leeder S, Greenberg HM. Obesity and cardiovascular disease in developing countries: a growing problem and an economic threat. Curr Opin Clin Nutr Metab Care. 2006;9:111–6. doi: 10.1097/01.mco.0000214568.52192.91. [DOI] [PubMed] [Google Scholar]
- 30.Wang H, Du S, Zhai F, Popkin BM. Trends in the distribution of body mass index among Chinese adults, aged 20–45 years (1989–2000) Int J Obes. 2007;31:272–8. doi: 10.1038/sj.ijo.0803416. [DOI] [PubMed] [Google Scholar]
- 31.Attard SM, Herring AH, Mayer-Davis EJ, Popkin BM, Meigs JB, Gordon-Larsen P. Multilevel examination of diabetes in modernising China: what elements of urbanisation are most associated with diabetes? Diabetologia. 2012;55:3182–92. doi: 10.1007/s00125-012-2697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van de Poel E, O’Donnell O, Van Doorslaer E. Urbanization and the spread of diseases of affluence in China. Econ Hum Biol. 2009;7:200–16. doi: 10.1016/j.ehb.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Yan S, Li J, Li S, Zhang B, Du S, Gordon-Larsen P, et al. The expanding burden of cardiometabolic risk in China: the China Health and Nutrition Survey. Obesity Reviews. 2012;13:810–21. doi: 10.1111/j.1467-789X.2012.01016.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leone A. Does smoking act as a friend or enemy of blood pressure? Let release Pandora’s Box. Cardiol Res Pract. 2011;2011:1–7. doi: 10.4061/2011/264894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Green MS, Jucha E, Luz Y. Blood pressure in smokers and nonsmokers: epidemiologic findings. Am Heart J. 1986;111:932–40. doi: 10.1016/0002-8703(86)90645-9. [DOI] [PubMed] [Google Scholar]
- 36.Sesso HD, Cook NR, Buring JE, Manson JE, Gaziano JM. Alcohol consumption and the risk of hypertension in women and men. Hypertension. 2008;51:1080–7. doi: 10.1161/HYPERTENSIONAHA.107.104968. [DOI] [PubMed] [Google Scholar]
- 37.Zatu MC, van Rooyen JM, Loots DT, Wentzel-Viljoen E, Greeff M, Schutte AE. Self-reported alcohol intake is a better estimate of 5-year change in blood pressure than biochemical markers in low resource settings: the PURE study. J Hypertens. 2014;32:749–55. doi: 10.1097/HJH.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 38.Felber JP, Golay A. Pathways from obesity to diabetes. Int J Obes Relat Metab Disord. 2002;26:S39–45. doi: 10.1038/sj.ijo.0802126. [DOI] [PubMed] [Google Scholar]
- 39.Jaacks LM, Gordon-Larsen P, Mayer-Davis EJ, Adair LS, Popkin BM. Age, period and cohort effects on adult body mass index and overweight from 1991 to 2009 in China: the China Health and Nutrition Survey. International journal of epidemiology. 2013;42:828–37. doi: 10.1093/ije/dyt052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Julius S, Palatini P, Kjeldsen SE, Zanchetti A, Weber MA, McInnes GT, et al. Usefulness of heart rate to predict cardiac events in treated patients with high-risk systemic hypertension. Am J Cardiol. 2012;109:685–92. doi: 10.1016/j.amjcard.2011.10.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.