Abstract
GlySH-surfactant herbicide (GlySH), one of the most commonly used herbicides worldwide, has been considered as minimally toxic to humans. However, clinical toxicologists occasionally encounter cases of severe systemic toxicity. The US Environmental Protection Agency (EPA) states that ‘GlySH’ is of relatively low oral and acute dermal toxicity. It does not have anticholinesterase effect and no organophosphate-like central nervous system (CNS) effects. The clinical features range from skin and throat irritation to hypotension and death. Severe GlySH-surfactant poisoning is manifested by gastroenteritis, respiratory disturbances, altered mental status, hypotension refractory to the treatment, renal failure, and shock.[1] GlySH intoxication has a case fatality rate 3.2–29.3%. Pulmonary toxicity and renal toxicity seem to be responsible for mortality. Metabolic acidosis, abnormal chest X-ray, arrhythmias, and elevated serum creatinine levels are useful prognostic factors for predicting GlySH mortality.[2] There is no antidote and the mainstay of treatment for systemic toxicity is decontamination and aggressive supportive therapy.
We report a case of acute pulmonary edema, which is a rare but severe manifestation of oral GlySH poisoning, where patient survived with aggressive supportive therapy.
Keywords: Acute pulmonary edema, aggressive treatment, GlySH poisoning
INTRODUCTION
Organophosphorous compound poisoning is one of the commonest forms of poisoning observed in patients admitted in the intensive care unit of Indira Gandhi Government Medical College, Nagpur, Maharashtra, India. GlySH-surfactant herbicide (GlySH), commercially known as ‘Glycel’ or ‘Roundup’ is a herbicide used by farmers in Vidarbha region of Central India [Figure 1]. However, poisoning with GlySH compound is uncommon in our area and acute pulmonary edema and respiratory failure is a rare presentation.
Figure 1.
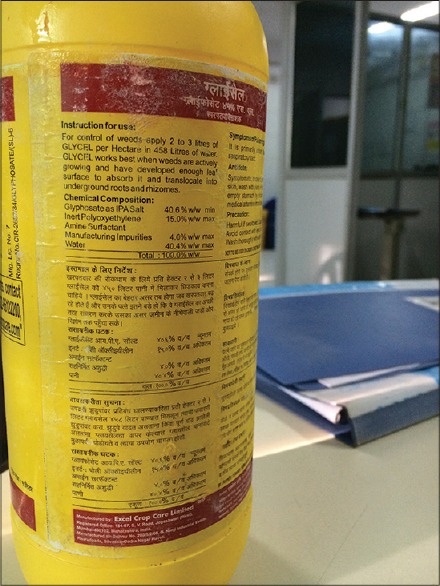
Glycel bottle
CASE REPORT
A 35-year-old male patient, farmer by occupation, and chronic alcoholic was brought to the emergency department of our hospital after ingestion of 75 ml (one cup) Glycel herbicide along with 120 ml of alcohol, half an hour before admission. This commercial preparation contains 40.6% GlySH, 15.0% inert polyoxyethylene amine surfactant, and water. He complained of abdominal pain and had two episodes of vomiting. There was no blood in vomitus. On admission, patient was conscious but irritable, agitated, and sweating profusely. Vitals were stable and pupils were normal size and reacting to light. On oral examination, buccal and posterior pharyngeal mucosa showed congestion and ulceration [Figure 2]. There were no fasciculations. Deep tendon reflexes were normal and plantars were flexors. On auscultation, chest was clear. Cardiovascular examination was normal. Patient had epigastric tenderness on palpation of abdomen.
Figure 2.

Oral ulcerations
On admission, body wash was given. Gastric lavage was done. Activated charcoal was not given as patient had oral ulcers.
Within half an hour of admission patient developed cyanosis and on chest examination he had bilateral end inspiratory fine crepitations. Within next half an hour patient's blood pressure (BP) dropped to 80 mmHg systolic and he developed respiratory distress with hypoxia and altered consciousness. He was intubated. Patient's vocal cords were congested and pink frothy secretions were coming out of the glottis. He was put on mechanical ventilation. Central line was inserted and central venous pressure was 16 cmH2O. Arterial blood gas (ABG) analysis revealed metabolic and respiratory acidosis (pH = 6.9930, HCO3− =15.5, and pCO2 = 64.3). Electrocardiogram (ECG) showed sinus tachycardia. X-ray chest revealed hilar congestion without cardiomegaly suggestive of acute pulmonary edema [Figure 3]. Patient was given forced diuresis cycles. Sodium bicarbonate was given through continuous infusion. He was also started on noradrenaline infusion. Approximately 12 h after admission, his BP improved to 100/60 mmHg. After 18 h, the patient developed watery diarrhea. Fluids were given according to CVP monitoring. Patient was in a state of altered consciousness for 3 days. He was supplemented with injectable thiamine and tube feeding was started on 4th day. Patient was on ventilator for 7 days. He was gradually weaned off ventilator and extubated. X-ray chest was repeated which showed clearing of hilar shadows. Serial liver function tests and kidney function tests normal except for rise in serum aspartate transferase (AST) with AST/serum alanine transferase (ALT) ratio of 1.34, consistent with alcoholic liver disease. Post extubation, patient was shifted to the ward. He improved and finally he was discharged on day 15.
Figure 3.
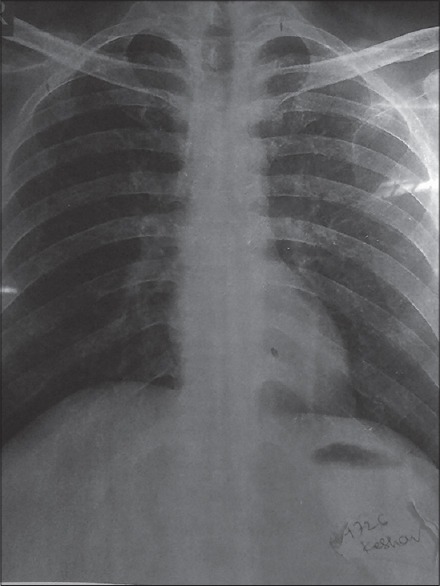
X-ray on admission showing hilar congestion
DISCUSSION
GlySH herbicide is promoted by the manufacturer as having no risks to human health, with acute toxicity being very low in normal use. Its use is likely to increase further as it is one of the first herbicides against which crops have been genetically modified to increase their tolerance. GlySH is an organophosphonate or salt of a phosphonic acid. It does not inhibit activity of the enzyme acetylcholinesterase like organophosphorus pesticides.[3] Accidental ingestion of glyphosate formulations is generally associated with only mild, transient, gastrointestinal features. The toxicity of the surfactant, polyoxyethyleneamine (POEA), is greater than the toxicity of glyphosate alone. Formulations containing GlySH and POEA caused more severe respiratory effects and damage to lung tissue than GlySH alone.[4] Acute pulmonary edema is a rare complication of GlySH poisoning.
After oral ingestion of GlySH, 30–36% is absorbed and peak concentrations occurs in tissues 6 h following dosing, undergoes little metabolism, and is excreted mostly unchanged in the feces and secondarily in the urine. The spectrum of GlySH poisoning includes minimal irritation of eyes to severe as shock and death.[1] Severe poisoning causes dehydration, hypotension, pneumonitis, oliguria, altered level of consciousness, hepatic dysfunction, acidosis, hyperkalemia, and dysrhythmias.[3] The clinical manifestations are determined by volume of surfactant ingested. In a study by Seok et al., for surfactant ingestion volumes of 8 mL, the incidence of clinical complications was as follows: Hypotension, 47.1%; mental deterioration, 38.6%; respiratory failure, 30.0%; acute kidney injury, 17.1%; and arrhythmia, 10.0%. Metabolic acidosis, abnormal chest X-ray, tachycardia, and elevated creatinine levels were useful prognostic factors for mortality.[5] In a single case report, patient developed neurotoxic sequels of GlySH-surfactant exposure with white matter lesions and development of Parkinsonism.[6] Our patient had oral ulcers, gastrointestinal involvement, and deteriorated due to development of acute pulmonary edema and respiratory failure.
Shock may be related to primary cardiovascular effects or to secondary effects from acidosis or electrolyte imbalance. The cardiovascular effects of glyphosate surfactant were examined in the aorta and heart of rat. Vasorelaxation and inhibition of heart twitch tension were observed in the study by Chang and Chang. Bradycardia and fatal ventricular arrhythmia often develop. It may also have primary toxicity in the conduction system and secondary toxicity in the circulation system.[7]
There is no antidote for GlySHand treatment is supportive. Gastric lavage or activated charcoal can be administered in patients who present <1 h after ingestion and who have no evidence of buccal irritation or burns. Early hemodialysis may improve prognosis. Han et al., demonstrated the effectiveness of intralipid fat emulsion (IFE) in severe poisoning patient who was refractory to inotropic support. The mechanism of action of IFE may be due to the lowering of serum concentration of the free surfactant POEA component of GlySH.[8] Gastrointestinal endoscopy should also be performed in those who have ulcerative lesions.
This case report is to increase awareness about poisoning by a widely available herbicide GlySH which may cause potentially fatal pulmonary edema. Mortality can be reduced by early aggressive treatment, in absence of specific antidote.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Beswick E, Millo J. Fatal poisoning with GlySH surfactant herbicide. J Iran Chem Soc. 2011;12:37–9. [Google Scholar]
- 2.Lee CH, Shih CP, Hsu KH, Hung DZ, Lin CC. The early prognostic factors of glyphosate-surfactant intoxication. Am J Emerg Med. 2008;26:275–81. doi: 10.1016/j.ajem.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Adams RD, Good AM, Bateman DN. Google Scholar. Edinburgh, UK: National Poisons Information Service; Report: Pesticide Exposure. Monitoring Using NPIS Resources April 2004-March 2005. [Google Scholar]
- 4.Mahendrakar K, Venkategowda PM, Rao SM, Mutkule DP. Glyphosate surfactant herbicide poisoning and management. Indian J Crit Care Med. 2014;18:328–30. doi: 10.4103/0972-5229.132508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seok SJ, Park JS, Hong JR, Gil HW, Yang JO, Lee EY, et al. Surfactant volume is an essential element in human toxicity in acute glyphosate herbicide intoxication. Clin Toxicol (Phila) 2011;49:892–9. doi: 10.3109/15563650.2011.626422. [DOI] [PubMed] [Google Scholar]
- 6.Potrebiæ O, Joviæ-Stosiæ J, Vuciniæ S, Tadiæ J, Radulac M. Acute glyphosate-surfactant poisoning with neurological sequels and fatal outcome. Vojnosanit Pregl. 2009;66:758–62. doi: 10.2298/vsp0909758p. [DOI] [PubMed] [Google Scholar]
- 7.Chang CB, Chang CC. Refractory cardiopulmonary failure after glyphosate surfactant intoxication: A case report. J Occup Med Toxicol. 2009;4:2. doi: 10.1186/1745-6673-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han SK, Jeong J, Yeom S, Ryu J, Park S. Use of a lipid emulsion in a patient with refractory hypotension caused by glyphosate-surfactant herbicide. Clin Toxicol (Phila) 2010;48:566–8. doi: 10.3109/15563650.2010.496730. [DOI] [PubMed] [Google Scholar]


