Sir,
The study by Cherukuri et al., emphasizes the high mortality associated with Paraquat poisoning and the lack of effective treatment options.[1] In this context, we would like to bring to your attention a rare case of survival following ingestion of a significant amount of concentrated Paraquat solution. Early hemoperfusion (within 4 hours of ingestion) and immunosuppression is believed to have played a beneficial role.
A 19-year-old girl was brought to the emergency medical service with alleged history of consumption of 200 mL of 20% Paraquat solution with suicidal intent. She had stable vitals and a spO2 of 95% with an unremarkable systemic examination. Her hemogram, renal function tests, liver function tests and chest radiograph were normal. Charcoal hemoperfusion was done within four hours of Paraquat ingestion. Intravenous methyl prednisolone was administered in the dose of 1 gram/day and it was continued for three days. Following this, 40 mg oral prednisolone was given. She also received intravenous cyclophosphamide 750 mg along with methyl prednisolone on the first day. Supportive management was given in the form of injectable pantoprazole, and intravenous saline with 25% dextrose solution. Local anesthetic gel application was done for oral ulcers [Figure 1], which she had developed two days following consumption and she also received oral folic acid, riboflavin and Vitamin E supplements. The second session of hemoperfusion was carried out after a period of 48 hours. She developed non-oliguric renal failure during her hospital stay, which improved slowly over a period of one week. Her oral ulcers also improved with treatment. She was discharged after 10 days of hospital stay on prednisolone 40 mg/day. The chest X-ray at discharge showed no abnormality. Prednisolone was continued at a dose of 40 mg for 1 month following which it was tapered over a period of 6 weeks and stopped. Follow-up assessment after 7 months revealed stable vitals, spO2 of 96% with normal systemic examination. Chest X-ray was normal. High resolution computed tomography (HRCT) scan of the thorax showed only few fibrotic bands in lower lobes of both lungs with ground glass appearance in the surrounding areas. The middle lobe of right lung showed fibrotic bands with minimal traction bronchiectasis [Figure 2].
Figure 1.

Oral ulcers
Figure 2.
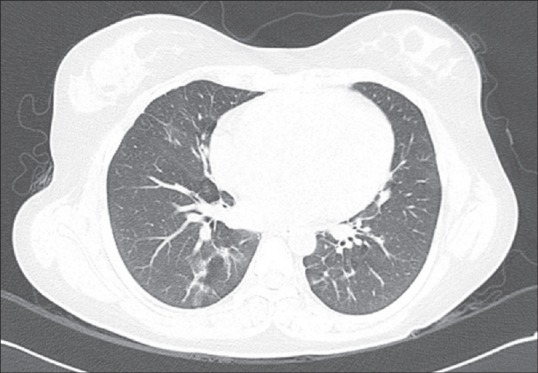
HRCT thorax showing few fibrotic bands, ground glass appearance and traction bronchiectasis
Paraquat, a herbicide is chemically a dipyridyl compound. It can produce local and systemic toxicity. The mortality in acute Paraquat poisoning is highly correlated with the plasma and urine Paraquat levels. Mortality in acute stage results from multi-organ dysfunction while in sub-acute stage, it results from lung fibrosis. The levels of Paraquat following ingestion peak in plasma around 1–2 hours, in the lung cells by 4–5 hours and 90% of Paraquat is cleared from plasma by 5–6 hours.[2,3] Hsu et al. studied the role of early hemoperfusion (<4 hrs) on survival in severe Paraquat poisoning.[4] They found that early hemoperfusion <4 hrs or <5 hrs was associated with a 62% and 41% reduction of relative risk of mortality of all severely poisoned patients, respectively. They also found that the reduction of relative risk of mortality was 81% (hemoperfusion <4 hrs) and 51% (hemoperfusion <5 hrs) in patients treated with repeated pulse therapy with methyl prednisolone and cyclophosphamide. Pulse therapy with these drugs causes immunosuppression, which may prevent ongoing inflammatory injury to the tissues. A study has found them to be effective in preventing pulmonary fibrosis.[5] Our case clearly demonstrates the importance of early initiation of hemoperfusion and immunosuppression in a case of Paraquat poisoning. Thus the initial 4 hours might be the ‘golden hour’ to initiate hemoperfusion in a case of Paraquat poisoning.
REFERENCES
- 1.Cherukuri H, Pramoda K, Rohini D, Thunga G, Vijaynarayana K, Sreedharan N, et al. Demographics, clinical characteristics and management of herbicide poisoning in tertiary care hospital. Toxicol Int. 2014;21:209–13. doi: 10.4103/0971-6580.139813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong SY, Yang JO, Lee EY, Kim SH. Effect of haemoperfusion on plasma paraquat concentration in vitro and in vivo. Toxicol Ind Health. 2003;19:17–23. doi: 10.1191/0748233703th171oa. [DOI] [PubMed] [Google Scholar]
- 3.Bismuth C, Scherrmann JM, Garnier R, Baud FJ, Pontal PG. Elimination of paraquat. Hum Toxicol. 1987;6:63–7. doi: 10.1177/096032718700600110. [DOI] [PubMed] [Google Scholar]
- 4.Hsu CW, Lin JL, Lin-Tan DT, Chen KH, Yen TH, Wu MS, et al. Early hemoperfusion may improve survival of severely paraquat-poisoned patients. PLoS One. 2012;7:e48397. doi: 10.1371/journal.pone.0048397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin JL, Leu ML, Liu YC, Chen GH. A prospective clinical trial of pulse therapy with glucocorticoids and cyclophosphamide in moderate to severe paraquat-poisoned patients. Am J Respir Crit Care Med. 1999;159:357–60. doi: 10.1164/ajrccm.159.2.9803089. [DOI] [PubMed] [Google Scholar]


