Abstract
Introduction:
Successful free tissue transfer depends on a multitude of factors, and adequate drainage of venous blood is one of the most critical part of successful free tissue transfers.
Material and Methods:
We report 6 cases of microvascular free flaps used for covering various defects, which developed venous congestion, that were salvaged with heparinised saline irrigation through the distal end of the congested vein by the help of an intravenous cannula. The irrigation was continued for 5 days.
Results:
All the flaps were successfully salvaged.
Conclusion:
This method has potential applications in situations for successful salvage of free tissue transfer particularly due to venous thrombosis.
KEY WORDS: Heparinised saline, salvage of congested flaps, venous obstruction in free flap
INTRODUCTION
Reliability of microvascular tissue transfer has improved in recent years owing to advances in instrumentation, improved surgical training and growing experience.[1,2] Failures, though less common, still occur and venous problems are the most common cause.[3] Essential factors for a reliable microvascular anastomosis are: Disease-free vessels with good flow, no tension on the pedicle and a technically perfect anastomosis.[4,5] Additionally, in post-trauma situations, especially in the lower extremities, the extent of injury and duration after the injury (inflammation/stasis) may influence the availability of vessels for free flap anastomosis.[5,6] Systemic factors (i.e., age of the patient and atherosclerotic disease) can also contribute to the prognosis, leaving only the technical part under surgeon's control. We present an innovative technique of free flap salvage due to venous thrombosis by continuous heparinised saline irrigation.
MATERIALS AND METHODS
A retrospective review was conducted in the department of plastic surgery, S.M.S Medical College between October 2013 and April 2014 during which 6 free flaps were selected which were re-explored due to venous congestion. Out of the 6 flaps, 3 osteocutaneous free fibula, 2 anterolateral thigh and one radial artery forearm flap were used for various defects of lower and upper extremities. Out of these, one osteocutaneous free fibula was used for bony defect of the right radius. Age of the patients ranged from 24 to 47 years. Out of the 6 patients, 5 were male, and one was female.
SURGICAL TECHNIQUE
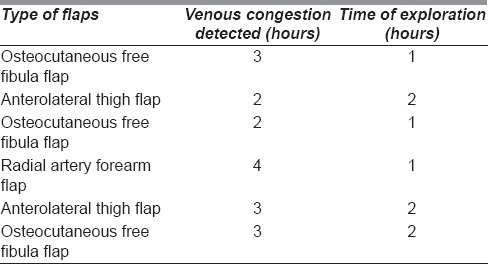
Six microvascular free flaps were performed using standard anastomotic techniques. Arterial anastomosis was performed with nylon 9-0 micropoint round body needle. Single vein anastomosis was performed in all the flaps between one of the vena commitantes and the recipient vein. Other vena commitantes was ligated at the end of the procedure. The patients were shifted to the postoperative ward. After the surgery, above flaps became congested. Venous congestion occurred within 2-4 h after surgery. Clinically, it was evident by brisk and congested bleeding on scratching the flap with needle. The flaps were explored within 1-2 h of venous congestion suspecting some compromise in the venous flow. The times of venous congestion and exploration after congestion have been indicated in Table 1.
Table 1.
Time-line of detection of venous congestion and exploration after detection
On exploration, after exposing the anastomotic sites, arterial anastomoses were patent but the veins were found to be congested. Both the anastomosed flap veins and the ligated venae commitantes were distended and tense. 2-3 sutures were opened in order to decongest the flap. Out of the six flaps, venous anastomosis was patent in 4 flaps where gentle manipulation and milking of flow from proximal to distal direction re-established the flow. But in the remaining 2 flaps, these manoeuvres were unsuccessful, and the anastomosis had to be redone after carefully excising 1 mm each from the opposing veins. One of the flaps (fibula flap) had to be explored 3 times due to repeated venous thrombosis. At the end of the third exploration, heparinised saline irrigation was used. There was availability of the second venae commitantes in both the cases which were re-explored and reanastomosed, but these were not used deliberately to know the efficacy of this newer technique. In all the six flaps, the proximal flap veins were ligated over a 22F cannula under appropriate pressure with 5/0 nylon. Also, the position of cannulas was secured over the skin by suturing their wings so as to prevent them from accidently getting dislodged. The cannulas were connected with extension tubing through which heparin (10,000 U in 500 ml of normal saline) infusion was started at a rate of 0.2 ml/min as the irrigation solution.
The irrigation of the flap vein through the external tubing was checked every 2 h along with flap monitoring. The irrigation was continued for 2 days at 0.2 ml/min, then tapered to 0.1 ml/min for 2 days. On 5th post-operative day, the concentration of the irrigating solution was changed to heparin (5000 U in 500 ml of normal saline) infusion and continued at a rate of 0.1 ml/min. By 6th day, the flap developed enough collateral venous drainage and there was no congestion on blocking the venous cannula [Figure 1].
Figure 1.

Well settled osteocutaneous fibula flap for radius defect on 4th postoperative day with irrigation cannula in situ
At this time, the irrigation was stopped, and the cannula was removed after ligation of vein. All the flaps survived, except a small area of necrosis in one free fibula flap. The distal necrotic portion was debrided, and the residual raw area was managed with regular dressings and was covered with the skin graft at a later date.
DISCUSSION
The success rate of a free flap following re-exploration depends upon the duration of occlusion of blood flow to the flap and the effects of hyper or hypo-perfusion of the flap due to venous or arterial problem respectively. Flap salvage rates after re-exploration have been reported to be between 44% and 80%.[7,8] Timely re-exploration and correction of the underlying problem is the most effective way to manage these problems.[5] After diagnosing vascular thrombosis, the treatment is thrombectomy and revision of the anastomosis. Even after early diagnosis and treatment, sometimes it may be difficult to re-vascularise the flap due to extension of the clot into the recipient or the donor vessels.[5] In the lower extremity, this is especially common if the vessels are affected by trauma, inflammation and stasis.[5] In multi-level injury also, vascular patency is greatly reduced because of possible intimal damage that cannot be ruled out pre-operatively, and there is high risk of vessel thrombosis. The ideal way to deal with this is to use vein grafts and perform the anastomosis out of the zone of trauma.
In all the patients being discussed, some of the deep recipient veins were thrombosed. In cases where larger flaps are harvested because of the need of additional soft tissue, there may be possibility of compromised drainage of flap and second vein anastomosis has been recommended in these cases (large bulky flaps) by few authors. The extension tube was irrigated continuously with heparin solution containing 10000 U heparin in 500 ml normal saline at the rate of 0.2 ml/min. Stringent monitoring was used for heparinised irrigation. Patient's coagulation parameters were monitored. There was a slight increase(1.2 times) in the Activated partial thromboplastin time (APTT) and prothrombin time after 24 h, and it remained stable for the rest of the (heparin) treatment period. The patients did not require any blood transfusion during this period. The renal function, liver functions were normal throughout the treatment period. The shunt used in this case was very cheap and could be changed periodically. The second flap vein was kept very close to the skin and with good available length there was no problem during the shunt change. The flap drainage through the anastomosed vein was periodically monitored by blocking the second vein. On the 6th day, all the flaps remained congestion free, and the external heparinised saline irrigation was stopped. This technique could have applications in some very selective situations in reconstructive microsurgery particularly due to venous thrombosis in selected fasciocutaneous flaps like free radial artery forearm flap, osteocutaneous fibula flap, anterolateral thigh flap, ulnar artery forearm flap where the distal end of the venae commitantes or superficial drainage systems are ligated during the flap harvest. This technique may not be useful in those cases where there is recipient arterial occlusion or in those microvascular free flaps in which there is no option of ligating the distal end of the second venae commitantes like latissimus dorsi flap. In such situations, it should be considered as a last resort (but potentially useful one) as a tool for salvaging the congested free flap.
CONCLUSION
In selected cases, this technique of heparinised saline irrigation for venous drainage of congested flap can be very useful.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Khouri RK, Cooley BC, Kunselman AR, Landis JR, Yeramian P, Ingram D, et al. A prospective study of microvascular free-flap surgery and outcome. Plast Reconstr Surg. 1998;102:711–21. doi: 10.1097/00006534-199809030-00015. [DOI] [PubMed] [Google Scholar]
- 2.Hidalgo DA, Jones CS. The role of emergent exploration in free-tissue transfer: A review of 150 consecutive cases. Plast Reconstr Surg. 1990;86:492–8. [PubMed] [Google Scholar]
- 3.Blondeel PN, Arnstein M, Verstraete K, Depuydt K, Van Landuyt KH, Monstrey SJ, et al. Venous congestion and blood flow in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2000;106:1295–9. doi: 10.1097/00006534-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Koul AR, Patil RK, Philip VK. Early use of microvascular free tissue transfer in the management of electrical injuries. Burns. 2008;34:681–7. doi: 10.1016/j.burns.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 5.Koul AR, Patil RK, Nahar S. Unfavourable results in free tissue transfer. Indian J Plast Surg. 2013;46:247–55. doi: 10.4103/0970-0358.118600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Acland RD. Refinements in lower extremity free flap surgery. Clin Plast Surg. 1990;17:733–44. [PubMed] [Google Scholar]
- 7.Chen KT, Mardini S, Chuang DC, Lin CH, Cheng MH, Lin YT, et al. Timing of presentation of the first signs of vascular compromise dictates the salvage outcome of free flap transfers. Plast Reconstr Surg. 2007;120:187–95. doi: 10.1097/01.prs.0000264077.07779.50. [DOI] [PubMed] [Google Scholar]
- 8.Kroll SS, Schusterman MA, Reece GP, Miller MJ, Evans GR, Robb GL, et al. Timing of pedicle thrombosis and flap loss after free-tissue transfer. Plast Reconstr Surg. 1996;98:1230–3. doi: 10.1097/00006534-199612000-00017. [DOI] [PubMed] [Google Scholar]


