Abstract
Aim:
The aim of the study was to evaluate the efficacy of platelet-rich plasma (PRP) in the treatment of chronic alopecia areata (AA).
Material and Methods:
This is a prospective study that was conducted at Kamal Hospital, Kaushambi in which 20 patients who attended the outpatient department were enrolled for the study. All the patients had h/o patches and taken various line of treatments for a duration of 2 years. All the patients were biopsy-proven positive for AA disease. There was no randomisation done since all of them were healthy young adults. The patients’age ranged from 25 to 35 years, and none of them had any co-morbidities.
Results:
Of 20 patients, only one patient had a relapse. None of the patients had any side effects, and all of them tolerated the procedure well.
Conclusion:
We wish to conclude that PRP has a definite role in treating AA infections. However, still more long-term follow-up, studies are required for further validation of results and labelling it as a 100% cure for people suffering from AA with recurrences which are so common.
KEY WORDS: Alopecia areata, platelet rich plasma, cicatricial alopecia
INTRODUCTION
Alopecia areata (AA) is a common, non-scarring, autoimmune disease that can affect any hair-bearing area. Though various lines of management have been described for this condition,[1,2,3,4,5] all have significant relapse rate with, with side effects of the medications too. In this paper, we discuss 20 patients of chronic, biopsy proved AA disease, who had taken (unsuccessfully) 2 years of various forms of therapy.
Platelet-rich plasma (PRP) is a preparation of autologous platelets in concentrated plasma. It has been investigated in several disciplines of medicine for its role in wound healing. In our centre, we have treated 20 patients of alopecia areata with PRP alone, without any side effects, and with good preliminary results as seen in Figure 1a and b.
Figure 1.

(a) Pre-intervention state of the patient with alopecia areata (b) post-platelet rich plasma status-note the improved sustained hair growth at the end of 1 year
We decided to use PRP for improvement of the patient's outcome as we had success in the use of PRP for hair rejuvenation and cicatricial alopecia.[6,7] There has been only one double-blinded, placebo and active-controlled, half-head, parallel group study on 45 patients to evaluate the efficacy and safety of PRP in AA patients.[8] This study concluded that PRP is a safe and alternative treatment for AA, but further controlled trials are needed to validate the findings.
MATERIAL AND METHODS
This is a prospective study that was conducted at Kamal Hospital, Kaushambi in which 20 patients who attended the outpatient department were enrolled for the study. All the patients had h/o patches and taken various lines of treatments for a duration of 2 years. All the patients were biopsy-proven positive for AA disease. There was no particular randomisation done since all of them were healthy young adults. The patients’ ages ranged from 25 to 35 years, and none had any co-morbidities. All the patients were explained about the procedure in detail. A consent form was signed by each patient. All the patients were followed up at 4 weekly intervals for a duration of 6 months and then at the end of 1 year. All the patients received 6 sessions of PRP. Ethics committee approval was taken prior to the commencement of the study.
Treatment protocol
A volume of 25 ml blood was taken from each patient and the PRP solution obtained from the lab was used within 30 min of its preparation. It was injected in the scalp after local anaesthesia application, in the subfollicular plane. Patients were sent home once the PRP session was over, and they were in a stable condition which was confirmed after checking all the vitals. They were called for review after 4 weeks for the next session and told to report earlier if any need arose. All the patients received 6 sessions of PRP at 4 weekly intervals. Patients were reviewed every month for 6 months and then at the end of 1 year.
RESULTS
Of the 20 patients, one patient had a relapse, and his hair regrowth was also minimum [Figure 2a-c]. None of the patients had any side effects, and all of them tolerated the procedure well.
Figure 2.
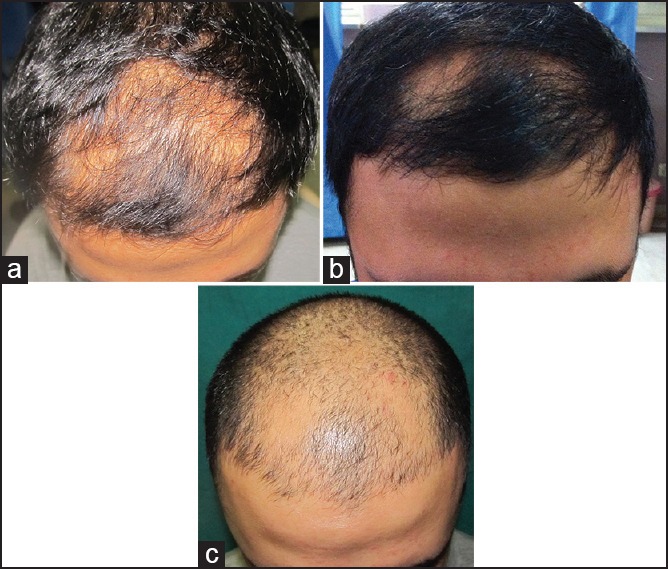
(a) Pre-intervention state of the patient with alopecia areata (b) post-platelet rich plasma (PRP) status-note the improved hair growth at the end of 6 months (c) post-PRP status-note the relapse at the end of 1 year
DISCUSSION
Proper counselling of the patient is very important before starting treatment for this disease since it is associated with recurrences very commonly. All the treatments available as of today are associated with both relapses and side effects, which affects the psychosocial life of the patients in the long run.
Various treatments are available for AA affliction. The effect of a single intralesional corticosteroid injection has been observed to persist for up to 9 months. In a few studies,[2] reported relapse rates were 29% in limited AA and 72% in alopecia totalis during a 3-month follow-up period.[1] The reported relapse rate of topical steroids is 37-63%.[4,5] In a placebo-controlled, double-blind study, hair regrowth was observed in 63.6% and 35.7% of the minoxidil-treated and placebo groups, respectively.[9] In another study, hair regrowth was achieved in 38% and 81% of patients treated with 1% and 5% topical minoxidil, respectively.[10] Side effects include contact dermatitis and facial hypertrichosis. Various forms of systemic corticosteroids have been used in different regimens. In one study, a once-monthly oral pulse of 300 mg prednisone induced a complete response in 41% of patients.[11] A similar effect has been reported in a placebo-controlled trial of oral prednisolone 200 mg once weekly in the treatment of extensive AA.[12] The relapse rate was 25%, and side effects of the therapy were noted in 55% of patients.[12] Other medications include methotrexate (with relapse rate of more than 50%); cyclosporine (with a high relapse rate of almost 100%);[13] azathioprine, and others.
There has been only one double-blinded, placebo and active-controlled, half-head, parallel group study on 45 patients to evaluate the efficacy and safety of PRP in AA patients,[8] which concluded that PRP is a safe and alternative treatment for AA, but further controlled trials are needed to validate the findings. Our study showed relapse in just one case and no side effects in any of the 20 treated patients. Though we have achieved initial success with PRP, further follow-up is required, and more studies needed to validate the final results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Abell E, Munro DD. Intralesional treatment of alopecia areata with triamcinolone acetonide by jet injector. Br J Dermatol. 1973;88:55–9. doi: 10.1111/j.1365-2133.1973.tb06672.x. [DOI] [PubMed] [Google Scholar]
- 2.Orentreich N, Sturm HM, Weidman AI, Pelzig A. Local injection of steroids and hair regrowth in alopecias. Arch Dermatol. 1960;82:894–902. doi: 10.1001/archderm.1960.01580060048005. [DOI] [PubMed] [Google Scholar]
- 3.Mancuso G, Balducci A, Casadio C, Farina P, Staffa M, Valenti L, et al. Efficacy of betamethasone valerate foam formulation in comparison with betamethasone dipropionate lotion in the treatment of mild-to-moderate alopecia areata: A multicenter, prospective, randomized, controlled, investigator-blinded trial. Int J Dermatol. 2003;42:572–5. doi: 10.1046/j.1365-4362.2003.01862.x. [DOI] [PubMed] [Google Scholar]
- 4.Tosti A, Piraccini BM, Pazzaglia M, Vincenzi C. Clobetasol propionate 0.05% under occlusion in the treatment of alopecia totalis/universalis. J Am Acad Dermatol. 2003;49:96–8. doi: 10.1067/mjd.2003.423. [DOI] [PubMed] [Google Scholar]
- 5.Pascher F, Kurtin S, Andrade R. Assay of 0.2 percent fluocinolone acetonide cream for alopecia areata and totalis. Efficacy and side effects including histologic study of the ensuing localized acneform response. Dermatologica. 1970;141:193–202. [PubMed] [Google Scholar]
- 6.Singh S. Platelet rich plasma — Protocol for its preparation and its role in hair rejuvenation. Aestheticians J. 2013;3:40–2. [Google Scholar]
- 7.Singh S. Role of platelet rich plasma in primary cicatricial alopecia. Aestheticians J. 2014;4:42–4. [Google Scholar]
- 8.Trink A, Sorbellini E, Bezzola P, Rodella L, Rezzani R, Ramot Y, et al. A randomized, double-blind, placebo-and active-controlled, half-head study to evaluate the effects of platelet-rich plasma on alopecia areata. Br J Dermatol. 2013;169:690–4. doi: 10.1111/bjd.12397. [DOI] [PubMed] [Google Scholar]
- 9.Price VH. Double-blind, placebo-controlled evaluation of topical minoxidil in extensive alopecia areata. J Am Acad Dermatol. 1987;16:730–6. doi: 10.1016/s0190-9622(87)70095-4. [DOI] [PubMed] [Google Scholar]
- 10.Fiedler-Weiss VC. Topical minoxidil solution (1% and 5%) in the treatment of alopecia areata. J Am Acad Dermatol. 1987;16:745–8. doi: 10.1016/s0190-9622(87)80003-8. [DOI] [PubMed] [Google Scholar]
- 11.Ait Ourhroui M, Hassam B, Khoudri I. Treatment of alopecia areata with prednisone in a once-monthly oral pulse. Ann Dermatol Venereol. 2010;137:514–8. doi: 10.1016/j.annder.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Kar BR, Handa S, Dogra S, Kumar B. Placebo-controlled oral pulse prednisolone therapy in alopecia areata. J Am Acad Dermatol. 2005;52:287–90. doi: 10.1016/j.jaad.2004.10.873. [DOI] [PubMed] [Google Scholar]
- 13.Gupta AK, Ellis CN, Cooper KD, Nickoloff BJ, Ho VC, Chan LS, et al. Oral cyclosporine for the treatment of alopecia areata. A clinical and immunohistochemical analysis. J Am Acad Dermatol. 1990;22:242–50. doi: 10.1016/0190-9622(90)70032-d. [DOI] [PubMed] [Google Scholar]


