Abstract
AIM
To compare retinal artery-vein diameters (RAVDs) of patients with pseudoexfoliation (PSX) syndrome with healthy controls and investigate the correlations between retinal nerve fiber layer (RNFL) thickness parameters and RAVDs.
METHODS
Seventeen eyes with PSX and 17 eyes of age-matched controls were included in the study. All participants underwent routine ophthalmological examination, Humphrey visual field and RNFL examination by using Stratus OCT. Retinal images were obtained by using a retinal camera (Topcon 501X). RAVDs were measured from inferior nasal, inferior temporal, superior nasal and superior temporal arcuates by using IMAGEnet software. Superior, inferior, nasal, temporal and average RNFL thicknesses were recorded. RAVDs and RNFL parameters in groups and correlations were analyzed by Mann-Whitney U and Spearmann correlation tests.
RESULTS
Only inferior quadrant and average RNFL thickness were detected thinner in the PSX group compared with control group (P=0.009, P=0.038, respectively). No statistically significant difference regarding RAVDs was found between two groups.
CONCLUSION
RAVDs seems to be comparable in the PSX and control group. RNFL is thinner in the inferior quadrant in the PSX group. RNFL thickness and RAVDs show significant correlations in both groups. This correlation doesn't seem to be specific to PSX.
Keywords: pseudoexfoliation, retinal nerve fiber layer thickness, retinal artery-vein diameters
INTRODUCTION
Pseudoexfoliation (PSX) syndrome is a systemic disease characterized by the presence of dust-like PSX material in ocular tissues[1]. It was first defined by Linberg at 1917 and it is well known today that it may affect up to 30% of people older than 60 years old in a worldwide distribution. PSX is diagnosed biomicroscopically by the presence of an abnormal fibrillar deposits on ocular structures of the anterior segment. This syndrome may predispose to many intraocular complications including phacodonesis, lens subluxation, open angle glaucoma, corneal endothelial decompensation, posterior synechiae formation[2]. Development of open angle glaucoma secondary to PSX has been reported between 20%-25%[3]. The pathogenesis of chronic intraocular pressure (IOP) increase is explained by the local production of pseudoexfoliative material on the trabecular meshwork and degeneration of the Schlemm channel and juxtacanalicular tissues predisposed by this material. On the other hand, early structural changes in retinal nerve fiber layer (RNFL) secondary to PSX have been reported and these changes can be detected by optical coherence tomography (OCT)[4],[5].
Retinal arterial system supplies two third of inner layers of retina and it has a great importance for the retinal function and vision[6]. It's been reported that peripapillary retinal artery-vein diameters (RAVDs) were significantly smaller in the glaucomatous eyes than that of controls and this has been explained by the retinal nerve fiber loss because of glaucomatous damage[6]. According to these data, vessels corresponding to the hemifield with the greater visual defect seems to be narrower than those of the other hemifield. This reflects either an ischemic basis for glaucomatous damage or vascular constriction when there are fewer axons to nourish[7].
PSX is a situation that is known to be a risk factor for peripheral vascular disease[8]. It has also known to be associated with ischemic retinal vascular conditions[9]. In the current study, our hypothesis was RAVDs might have been an indicator for the structural changes in PSX. Thus, we aimed to compare RAVDs in patients with PSX with those of healthy controls and to investigate the correlation between RNFL thickness parameters and RAVDs.
SUBJECTS AND METHODS
Seventeen eyes of 17 patients with PSX and 17 eyes of 17 healthy controls were included in the study. Only one eye of each consecutively numbered case in groups were evaluated (right eye for odd numbers, left eye for even numbers). The study protocol adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects and institutional review board approval was taken for the study. Inclusion criterias for PSX group were the presence of PSX on biomicroscopy, non glaucomatous optic disc appearance (C/D ratio ≤0.3, asymmetry of the two eyes C/D ratio ≤0.2), normal visual fields and normal diurnal IOP measurements (≤21 mm Hg for each and the difference between two eyes ≤3 mm Hg). Healthy controls were otherwise healthy individuals with normal diurnal IOP measurements (≤21 mm Hg for each and the difference between two eyes ≤3 mm Hg). Refractive errors and veritcal optic nerve diameters were recorded. Exclusion criteria for both groups were any kind of retinal disease or optic disc pathology, the history of using topical antiglaucomatous agents, systemic vascular diseases like diabetes mellitus and hypertension. Patients with media opacity interfering with visualization and OCT images capturing such as corneal opacity or dense cataract or with history of previous ocular surgery and trauma were also exluded. After informed consent was signed, all participants underwent ophthalmic examinations including visual acuity, slit lamp biomicroscopy, Goldmann applanation tonometry, Humphrey (Central 24-2 threshold) visual field examination. Following dilation of pupils by tropicamide, fundoscopy and RNFL thicknesses analyze was performed by using Stratus OCT (Zeiss) and measurements with signal power ≥7 were included.
Measurements of Retinal Vessel Diameter
Thirty-five degree fundus photographs were acquired with a Topcon fundus camera (TRC50 IX, Topcon Corporation, Tokyo, Japan). Peripapillary artery and vein diameters were measured by a single masked grader (Yildiz BK) using one of the quantitative analysis tools available (measurement function) on IMAGEnet program of the Topcon digital angiography system[10]. IMAGE net is an image management software of Topcon's mydriatic retinal cameras and is available on the Topcon digital angiography system. The grader (Yildiz BK), chose the location of RAVD measurement using photodynamic therapy (PDT) marking tool on the vessel and measured the trunk of the vessel by a semi-automated process. The grader who was also masked to the patients made all measurements from inferior nasal, inferior temporal, superior nasal and superior temporal arcuates. Retinal vessel diameters were measured from five adjacent areas 0.75 mm away from the optic disc border. The average of five measurements was recorded for statistical analysis (Figure 1). To test intraobserver reliability of RAVD measurements, 3 readings were done at three different days.
Figure 1. Retinal vessel diameters are measured by using PDT measurement tool, available on IMAGEnet software system.
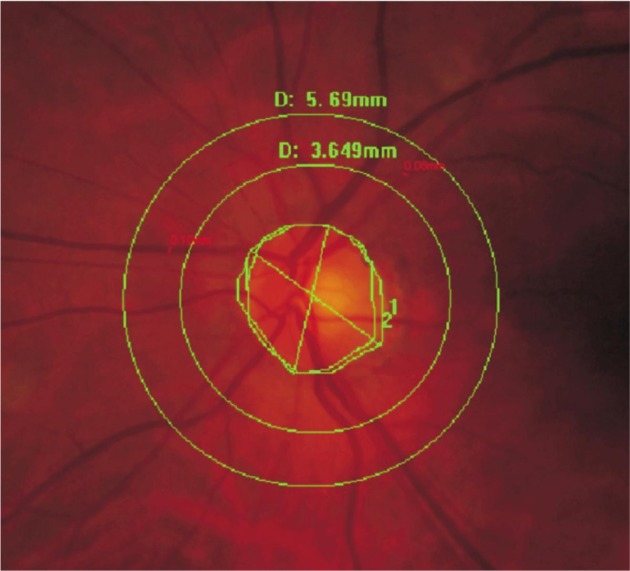
First green circle is 0.75 mm away from optic disc margin.
Statistical Analyses
RAVDs and RNFL thickness parameters were statistically analyzed and the differences regarding these parameters between two groups were analysed by Mann-Whitney U test. Spearman correlation test was used for the analyses of correlations between RAVDs and RNFL thickness parameters. Cronbach's alpha model was used to assess intra observer reliability of the RAVD measurements. SPSS version 11.0 system for personal computer was used and P value less than 0.05 was considered to be statistically significant.
RESULTS
There were 10 men and 7 women in the PSX group and 8 men and 9 women in control group. The mean ages of patients in PSX and control groups were 67.5±4.8y (59-82) and 65.7±5.1y (50-77), respectively (P=0.277). PSX and control groups had similar refractive errors (Spherical equivalents were -0.78±0.88 D and -0.64±0.87 D respectively, P=0.15) and similar optic disc areas (2.84±0.49-mm2 and 2.55±0.41-mm2 respectively, P=0.64).
RNFL thickness results (average, superior, inferior, nasal, temporal) are presented in Table 1. Only inferior quadrant and average RNFL thickness were thinner in PSX group than those of controls and this difference was statistically significant (P=0.009, P=0.038, respectively). There was no significant difference regarding other quadrants between groups (P>0.05).
Table 1. RNFL thicknesses in PSX and control groups (µm).
| Variables | Superior | Inferior | Nasal | Temporal | Average thickness |
| PSX group | 115.7 (73-145) SD: 22.7 | 99.3 (60-145) SD: 22.7 | 66.0 (38-100) SD: 20.1 | 66.1 (51-87) SD: 10.8 | 85.2 (61-102.2) SD: 12.2 |
| Control group | 118.3 (86-176) SD: 20.5 | 120.8 (85-152) SD: 20.5 | 77.3 (38-108) SD: 15.8 | 65.2 (50-87) SD: 9.7 | 95.4 (73- 115.6) SD: 10.7 |
| P (Mann Whitney U) | 0.823 | 0.009 | 0.085 | 0.945 | 0.038 |
Superior temporal, inferior temporal, inferior nasal, superior nasal RAVDs in the PSX and control groups are presented in Table 2. Cronbach's alpha for three different measurements of superior temporal inferior temporal, inferior nasal and superior nasal RAVDs were greater than 0.9. There was no statistically significant difference regarding RAVDs between two groups.
Table 2. Retinal artery vein diameters in PSX and control groups (mm).
| Variables | Superior temporal artery | Superior temporal vein | Inferior temporal artery | Inferior temporal vein | Superior nasal artery | Superior nasal vein | Inferior nasal artery | Inferior nasal vein |
| PSX group | 0.094 (0.08-0.12) SD: 0.117 | 0.140 (0.11-0.20) SD: 0.289 | 0.099 (0.08-0.15) SD: 0.164 | 0.141 (0.11-0.23) SD: 0.260 | 0.074 (0.06-0.09) SD: 0.009 | 0.096 (0.07-0.13) SD: 0.169 | 0.074 (0.06-0.09) SD: 0.106 | 0.101 (0.07-0.14) SD: 0.101 |
| Control group | 0.088 (0.07-0.12) SD: 0.148 | 0.132 (0.11-0.16) SD: 0.189 | 0.091 (0.07-0.12) SD: 0.138 | 0.148 (0.11-0.19) SD: 0.197 | 0.077 (0.05-0.11) SD: 0.165 | 0.101 (0.07-0.13) SD: 0.139 | 0.075 (0.06-0.09) SD: 0.123 | 0.105 (0.08-0.13) SD: 0.150 |
| P (Mann Whitney U) | 0.151 | 0.660 | 0.200 | 0.070 | 0.403 | 0.417 | 0.760 | 0.490 |
Significant correlation was found in the PSX group between superior temporal vein diameter and maximum-minimum, superior maximum (smax), superior average parameters (r=0.53, P=0.027; r=0.54, P=0.024; r=0.52, P=0.031, respectively). Furthermore, similar significant correlations were found between inferior temporal vein diameter and maximum-minimum, inferior maximum (imax), inferior average, average thickness, inferior quadrant thickness parameters (r=0.66, P=0.004; r=0.69, P=0.002; r=0.62, P=0.007; r=0.51, P=0.033; r=0.69, P=0.002, respectively).
In control group, significant correlation was also found between superior temporal vein diameter and average thickness (r=0.59, P=0.012); inferior temporal vein diameter and imax/smax, smax/imax parameters (r=0.51, P=0.036; r=-0.51, P=0.036, respectively); inferior nasal vein diameter and maximum-minimum, imax parameters (r=0.53, P=0.027; r=0.51, P=0.035, respectively); superior nasal artery diameter and imax/smax, smax/imax, maximum-minimum, imax parameters (r=0.51, P=0.033; r=-0.51, P=0.033; r=0.50, P=0.041; r=0.508, P=0.037, respectively); inferior temporal artery and imax/smax, smax/imax, maximum-minimum, imax, inferior quadrants parameters (r=0.679, P=0.003; r=-0.679, P=0.003; r=0.506, P=0.038; r=0.67, P=0.003; r=0.608, P=0.010, respectively).
DISCUSSION
PSX is currently the most important single identifiable risk factor for open angle glaucoma and it accounts for 25% of all glaucoma subtypes. It is not known which mechanism is responsible for the progression of PSX to pseudoexfoliative glaucoma (PSG), but PSG represents more severe and progressive disease than primary open angle glaucoma with a generally poor prognosis due to higher IOP levels, greater pressure differences between two eyes and fluctuations in the diurnal pressure curve.
The critical point is to detect ganglion cell damage early during the course of both PSX and PSG like all types of glaucoma. A defect in the standart visual field analysis represents 30%-40% loss of ganglion cells[11]. Measurement of peripapillery RNFL thickness is of importance for the early diagnosis of glaucoma[12].
PSX may cause significant RNFL loss in some patients compared with normal individuals. Mohamed[4] assessed RNFL thickness in 20 patients with PSX and compared them with 20 age matched normal control subjects and they documented that the RNFL in patients with PSX were significantly thinner than controls in all quadrants except the nasal quadrant (P<0.05). Yüksel et al[5] also evaluated the RNFL thickness in patients with unilateral PSX and their normal fellow eyes using Stratus OCT-3. The RNFL in eyes with PSX were significantly thinner than controls in all quadrants except the nasal quadrant with regard to quadratic and segmental analysis (P<0.05). Similarly, we also found decreased RNFL thickness measurements in PSX group but the differences were statistically significant regarding only inferior quadrant and average thickness values (P=0.009, P=0.038, respectively). These results may have resulted from relatively smaller number of the study group or the early stages of the disease.
IOP spikes detected in patients with PSX are the main factor leading RNFL loss. There is also reported other risk factors for optic nerve damage independent from IOP. Pseudoexfoliation material has also been suggested as a risk factor for the optic nerve damage in PSX[13]. On the other hand, it is well known that PSX is a systemic disease that is associated with vascular disorders such as abdominal aneurysims[14]. Retrobulbar blood flow velocities were found to be reduced in PSX in comparison to normal subjects[1]. Ocular blood flow disturbances reported in PSX may have a role in the development of RNFL loss. For that reason, we aimed to investigate RAVDs in patients with PSX and their relationship with RNFL thickness.
According to Hagen Pousille law, the diameter of a vessel is directly proportional to the blood volume it carries. Thus retinal vessel diameter is proportional to the retinal blood flow and this may clinically provide important clues.
There are various studies investigating the connection between vessel caliber and glaucoma in the current literature. These studies demonstrated that peripapillary retinal artery diameters were significantly thinner in patients with glaucoma than that of controls but no difference was reported regarding retinal vein diameters[6]. The decrease in retinal artery diameter in glaucoma may be explained by the glaucoma related loss of retinal tissue but the studies are unable to assess whether it was primarily a vascular insufficiency leading to the glaucomatous damage or whether the decrease in the retinal artery diameter occurred secondary to the tissue loss with a decreased demand for vascular supply[6]. Decreased vessel diameter was found to be correlated with increased peripapillary chorioretinal atrophy, decreased neuroretinal rim area, increased cup/disk ratios and decreased RNFL thickness in glaucoma[15].
Retinal artery diameter decreases also with age so we composed age matched groups in our study[16]. Systemic diseases like diabetes, hypertension cause narrowing of retinal arteries and enlargement of retinal veins[17]. Similarly retinal vessel diameters are thinner at nonglaucomatous optic neuropathies like anterior ischemic optic neuropathy and optic atrophy[18]. Patients with systemic diseases like hypertension and diabetes and optic neuropathy were excluded from the study for these reasons.
Since electron microscopic investigations in autopsy specimens have shown that exfoliation fibrils can be identified outside the eye such as heart, lung, liver, gall bladder and cerebral meninges; PSX has been classified as a systemic disease. Furthermore, it's now accepted as a some kind of systemic vascular disease[19]. Thus, we aimed to analyse RAVDs and its relationship with RNFL thickness in PSX. However, no difference was found between PSX and control groups. This result shows that during the early course of disease (showing loss only in the inferior quadrant) vessel diameters do not seem to be affected and different from that of controls. Thus, PSX does not seem to be a factor that facilitates the decrease in RAVDs.
Jonas et al[15] evaluated retinal vessel diameters between healthy and glaucomatous eyes by using the average of two measurements taken from the distance between the border of optic disc and 2 mm away from it. They found that inferior temporal artery, superior temporal artery, inferior temporal vein, superior temporal vein were thinner in glaucoma group than the control group. By the correlation analysis, arteries were detected to have higher correlation coefficient than veins. Hall et al[7] documented the association of retinal vessel caliber and visual field defects and they measured vessel calibers at the optic disc border on an enlarged image.
It has been detected that in healthy eyes the largest artery–vein diameter is inferior temporal and superior temporal, superior nasal, inferior nasal in a decreasing order. This pattern is concordant with the physiologic pattern of neuroretinal rim. Glaucomatous eyes have thinner superior temporal and inferior temporal arteries than healthy eyes and this difference is statistically significant. Superior nasal and inferior nasal arteries are also narrower in glaucomatous group but the difference is not statistically significant. The calibers of retinal veins at all quadrants were not different from healthy group[6].
In our study, it's remarkable that in both PSX and control group the vessel calibers are widest in inferior temporal region and the narrowest in superior nasal region. RAVDs were found to be significantly correlated most of the RNFL thickness parameters in both group. There were significant correlations between superior temporal vein diameter and maximum-minimum, superiormax, superior average; inferior temporal vein and maximum-minimum, superiormax, smax/naverage, superior average, average thickness, superior quadrant thickness in the PSX group. On the other hand, inferior nasal vein and maximum-minimum, inferiormax; inferior temporal artery and imax/smax, smax/imax, maximum-minimum, inferiormax, inferior; superior temporal vein and average thickness, inferior temporal vein and smax/imax, imax/smax; superior nasal artery and imax/smax, smax/imax, maximum-minimum, inferiormax have been found to be significantly correlated in the control group. There were various correlations in the PSX group but since similar correlations were found in the control group, this was not thought to be related with PSX. The relationship between PSX and retinal vessel diameters was further investigated with a study from north Chinese population aged 50y, but PEX was not associated (all P>0.05) neither with retinal vessel diameters nor with other parameters like sex, diabetes mellitus, blood pressure,psychological depression, smoking, dyslipidemia, body mass index, central corneal thickness, corneal diameter, optic nerve head measurements, choroidal thickness, early age-related macular degeneration or retinal vein occlusion[20].
To the best of our knowledge, our study is the first study investigating the RAVDs in PSX and its correlation with RNFL thickness. RNFL thickness is thinner in PSX group but the difference is significant only in the inferior quadrant. RAVDs seems to be comparable in patients with PXS and healthy controls. RNFL thickness and RAVDs shows significant correlation in both group. RAVDs doesn't seem to give a clinical clue about the pattern of the RNFL damage caused by PSX. On the other hand, the weakest part of the study is limited number of patients since isolated PSX patients without systemic vascular disease were included. Further prospective studies with increased number of patients are needed to identify the relationship between RNFL damage and other factors such as RAVDs in PSX.
Acknowledgments
Conflicts of Interest: Ozmen MC, None; Aktas Z, None; Yildiz BK, None; Hasanreisoglu M, None; Hasanreisoglu B, None.
REFERENCES
- 1.Yüksel N, Karabaş VL, Arslan A, Demirci A, Cağlar Y. Ocular hemodynamics in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Ophthalmology. 2001;108(6):1043–1049. doi: 10.1016/s0161-6420(01)00572-3. [DOI] [PubMed] [Google Scholar]
- 2.Elhawy E, Kamthan G, Dong CQ, Danias J. Pseudoexfoliation Syndrome, a systemic disorder with ocular manifestations. Hum Genomics. 2012;6:22. doi: 10.1186/1479-7364-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlötzer-Schrehardt U. Besharse & Dana, editor. Pseudoexfoliation syndrome and glaucoma. Encyclopedia of the Eye. 2010:539–548. [Google Scholar]
- 4.Mohamed MM. Detection of early glaucamatous damage in pseudo exfolation syndrome by assessment of retinal nerve fiber layer thickness. Middle East Afr J Ophthalmol. 2009;16(3):141–145. doi: 10.4103/0974-9233.56228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yüksel N, Altintas O, Celik M, Ozkan B, Cağlar Y. Analysis of retinal nerve fiber layer thickness in patients with pseudoexfoliation syndrome using optical coherence tomography. Ophthalmologica. 2007;221(5):299–304. doi: 10.1159/000104759. [DOI] [PubMed] [Google Scholar]
- 6.Wang S, Xu L, Wang Y, Jonas JB. Retinal vessel diameter in normal and glaucomatous eyes: the Beijing Eye Study. Clin Exp Ophthalmol. 2007;35(9):800–807. doi: 10.1111/j.1442-9071.2007.01627.x. [DOI] [PubMed] [Google Scholar]
- 7.Hall JK, Andrews AP, Walker R, Piltz-Seymour JR. Association of retinal vessel caliber and visual defects in glaucoma. Am J Ophtalmol. 2001;132(6):855–859. doi: 10.1016/s0002-9394(01)01200-4. [DOI] [PubMed] [Google Scholar]
- 8.Praveen MR, Shah SK, Vasavada AR, Diwan RP, Shah SM, Zumkhawala BR, Thomas R. Pseudoexfoliation as a risk factor for peripheral vascular disease: a case-control study. Eye (Lond) 2011;25(2):174–179. doi: 10.1038/eye.2010.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prata TS, Rozenbaum I, de Moraes CG, Lima VC, Liebmann J, Ritch R. Retinal vascular occlusions occur more frequently in the more affected eye in exfoliation syndrome. Eye (Lond) 2010;24(4):658–662. doi: 10.1038/eye.2009.152. [DOI] [PubMed] [Google Scholar]
- 10.Tatlıpınar S, Dinc UA, Yenerel NM, Görgün E. Short-term effects of a single intravitreal bevacizumab injection on retinal vessel calibre. Clin Exp Optom. 2012;95(1):94–98. doi: 10.1111/j.1444-0938.2011.00662.x. [DOI] [PubMed] [Google Scholar]
- 11.Budenz DL, Michael A, Chang RT, McSoley J, Katz J. Sensitivity and specifity of the stratus OCT for perimetric glaucoma. Ophthalmology. 2005;112(1):3–9. doi: 10.1016/j.ophtha.2004.06.039. [DOI] [PubMed] [Google Scholar]
- 12.Aydın A, Bilge AH. Application of optical coherence tomography in glaucoma. Glaucoma-Cataract. 2007;2:77–82. [Google Scholar]
- 13.Puska P, Vesti E, Tomita G, Ishida K, Raitta C. Optic disc changes in normotensive persons with unilateral exfoliation syndrome: a 3-year follow-up study. Graefes Arch Clin Exp Ophthalmol. 1999;237(6):457–462. doi: 10.1007/s004170050261. [DOI] [PubMed] [Google Scholar]
- 14.Schumacher S, Schlötzer-Schrehardt U, Martus P, Lang W, Naumann GO. Pseudoexfoliation syndrome and aneurysms of the abdominal aorta. Lancet. 2001;357(9253):359–360. doi: 10.1016/s0140-6736(00)03645-x. [DOI] [PubMed] [Google Scholar]
- 15.Jonas JB, Nguyen XN, Naumann GO. Parapapillary retinal vessel diameter in normal and glaucoma eyes. I. Morphometric data. Invest Ophthalmol Vis Sci. 1989;30(7):1599–1603. [PubMed] [Google Scholar]
- 16.Wong TY, Klein R, Klein BE, Meuer SM, Hubbard LD. Retinal vessel diameters and their associations with age and blood pressure. Invest Ophthalmol Vis Sci. 2003;44(11):4644–4650. doi: 10.1167/iovs.03-0079. [DOI] [PubMed] [Google Scholar]
- 17.Wang X, Cao H, Zhang J. Analysis of retinal images associated with hypertension and diabetes. Conf Proc IEEE Eng Med Biol Soc. 2005;6:6407–6410. doi: 10.1109/IEMBS.2005.1615964. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Fawzi AA, Varma R, Sadun AA, Zhang X, Tan O, Izatt JA, Huang D. Pilot study of optical coherence tomography measurement of retinal blood flow in retinal and optic nerve diseases. Invest Ophthalmol Vis Sci. 2011;52(2):840–845. doi: 10.1167/iovs.10-5985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tarkkanen A. Is exfoliation syndrome a sign of systemic vascular disease? Acta Ophthalmol. 2008;86(8):832–836. doi: 10.1111/j.1755-3768.2008.01464.x. [DOI] [PubMed] [Google Scholar]
- 20.You QS, Xu L, Wang YX, Yang H, Ma K, Li JJ, Zhang L, Jonas JB. Pseudoexfoliation: normative data and associations: the Beijing eye study 2011. Ophthalmology. 2013;120(8):1551–1558. doi: 10.1016/j.ophtha.2013.01.020. [DOI] [PubMed] [Google Scholar]


