SUMMARY
Trypanosoma brucei is the causative agent of African sleeping sickness in humans and one of several pathogens that cause the related veterinary disease Nagana. A complex co-evolution has occurred between these parasites and primates that led to the emergence of trypanosome-specific defences and counter-measures. The first line of defence in humans and several other catarrhine primates is the trypanolytic protein apolipoprotein-L1 (APOL1) found within two serum protein complexes, trypanosome lytic factor 1 and 2 (TLF-1 and TLF-2). Two sub-species of T. brucei have evolved specific mechanisms to overcome this innate resistance, Trypanosoma brucei gambiense and Trypanosoma brucei rhodesiense. In T. b. rhodesiense, the presence of the serum resistance associated (SRA) gene, a truncated variable surface glycoprotein (VSG), is sufficient to confer resistance to lysis. The resistance mechanism of T. b. gambiense is more complex, involving multiple components: reduction in binding affinity of a receptor for TLF, increased cysteine protease activity and the presence of the truncated VSG, T. b. gambiense-specific glycoprotein (TgsGP). In a striking example of co-evolution, evidence is emerging that primates are responding to challenge by T. b. gambiense and T. b. rhodesiense, with several populations of humans and primates displaying resistance to infection by these two sub-species.
Key words: Co-evolution, Genome, Trypanosome
INTRODUCTION
Trypanosoma brucei is the causative agent of African sleeping sickness in humans and one of several species that causes the related veterinary disease Nagana. Both diseases have a wide distribution across sub-Saharan Africa and affect some of the poorest areas of the world. Trypanosoma brucei is traditionally segregated into three morphologically identical sub-species based on host, geography and pathology, although the polyphyletic nature of the three sub-species and evidence for mating between them makes grouping them as such problematic. Trypanosoma brucei brucei is limited to domestic and wild animals throughout sub-Saharan Africa and is non-infective to humans (and some primates) due to sensitivity to trypanosome lytic factors (TLF) found in its serum (Seed and Sechelski, 1990; Lugli et al. 2004). Trypanosoma brucei gambiense and Trypanosoma brucei rhodesiense are human infective sub-species, named due to their relative geographic locations. Trypanosoma b. gambiense is found in Western and Central sub-Saharan African and causes a chronic infection that can persist for many years before symptoms appear (Gibson, 1986). It appears to be largely a disease limited to humans, although some animal reservoirs have been described (Gibson et al. 1978; Mehlitz, 1979; Felgner et al. 1981; Mehlitz et al. 1981, 1982; Zillmann et al. 1984). Trypanosoma b. rhodesiense is found in a limited but expanding area of Eastern sub-Saharan Africa, and there is a large potential animal reservoir in wild and domesticated animals (Welburn et al. 2001; Fèvre et al. 2001, 2005; Odiit et al. 2005). This sub-species causes a more acute form of the disease than T. b. gambiense (Gibson, 2002), although T. b. gambiense is by far the more prevalent human-infective sub-species and is responsible for more than 97% of human cases (World Health Organization, 2006; Simarro et al. 2011). The evolution of TLF in primates and the adaptations of T. brucei sub-species to resist lysis represent an excellent example of the co-evolutionary arms race between host and parasite.
HUMAN RESISTANCE TO TRYPANOSOME INFECTION
It has been known for more than a century that a component found in the serum of several primates, including humans, is toxic to trypanosomes (Fig. 1) (Laveran and Mesnil, 1912). After exposure to human serum, most trypanosomes are rapidly lysed with a defined morphology (Pays et al. 2006). Lysis is preceded by a characteristic swelling of the lysosome, suggesting that this organelle is intimately involved in the process. Fractionation of human serum identified a specific high-density lipoprotein (HDL) particle approximately 500 kDa in size that was able to lyse trypanosomes (Rifkin, 1978a, b ; Hajduk et al. 1989). This particle was originally termed the TLF but later renamed TLF-1 after the discovery of a second particle, a high molecular weight serum protein-binding complex related to TLF-1 that was consequently named TLF-2 (Raper et al. 1996). Both TLF-1 and TLF-2 contain the same protein complement: apolipoprotein A1 (APOA1), apolipoprotein L1 (APOL1) and haptoglobin-related protein (HPR), although TLF-1 is predominantly composed of lipid while TLF-2 is lipid poor (Raper et al. 2001). Despite this, TLF-2 is a much larger particle than TLF-1 due to being bound to several IgM molecules (Tomlinson et al. 1995; Raper et al. 1996). Considerable effort and much debate has focused on determining the trypanolytic component of TLF, largely focusing on TLF-1 as a result of the difficulty of purifying active TLF-2 ex vivo (Tomlinson et al. 1995; Raper et al. 1996). Investigation has centred on the two primate-specific proteins found in TLF, i.e. HPR and APOL1, both of which are the result of tandem gene duplication events during primate evolution. HPR is a haemoglobin binding protein with high sequence similarity to the haem scavenger protein haptoglobin (HP). Found within the same HDL complex as HPR, APOL1 is a lipid-binding protein that possesses both a secretory signal peptide and a Bcl-2 homology 3 (BH3) domain (Duchateau et al. 1997; Wan et al. 2008; Zhaorigetu et al. 2008). The BH3 domain is an important pro-apoptotic regulator of autophagy in many cell types (Lutz, 2000) and APOL1 itself appears to be able to induce autophagy if over-expressed in cell lines, indicating it may have a role in vertebrate controlled cell death (Zhaorigetu et al. 2008). APOL1 mutations are also associated with various pathologies, including schizophrenia and chronic kidney diseases (Mimmack et al. 2002; Genovese et al. 2010; Tzur et al. 2010).
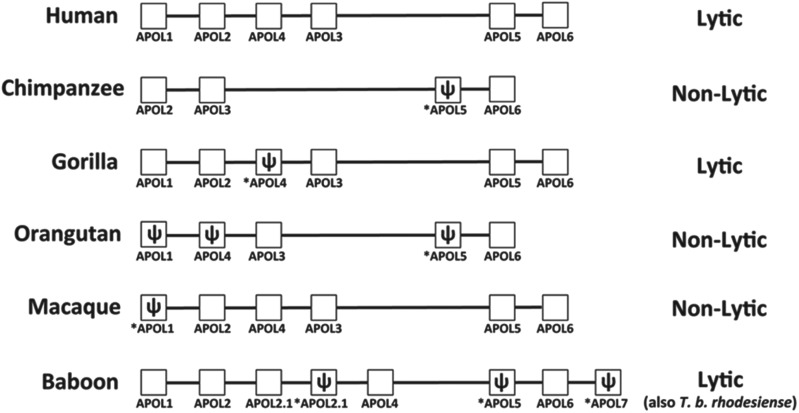
Fig. 1.
APOL gene cluster of various primate species. The complement of APOL genes and pseudogenes in several primate genera. The proposed genomic arrangement for each genus is shown, with pseudogenes indicated by ψ and *. The potential for the species’ serum to lyse T. brucei is also indicated (adapted from Smith and Malik, 2009).
While there has been some controversy concerning the roles of these two proteins with regards trypanosome lysis, the current consensus is that both proteins are necessary for optimal lysis and that HPR and APOL1 have complementary roles (Vanhollebeke et al. 2007; Widener et al. 2007). Although it has also been shown to have some trypanosome-specific toxicity itself (Harrington et al. 2010), possibly due to the un-cleaved signal peptide, which can affect membrane fluidity (Harrington et al. 2010), HPR acts primarily as a ligand. Similar to its haptoglobin ancestor, HPR binds haemoglobin and thus facilitates uptake of TLF-1 via a parasite haptoglobin-haemoglobin receptor (HpHbR) (Vanhollebeke et al. 2008; Vanhollebeke and Pays, 2010). This strategy likely evolved to take advantage of the fact that trypanosomes are haem auxotrophs (Korený et al. 2010). After being endocytosed (Hager et al. 1994), the TLF-1 particle is trafficked to the lysosome where APOL1 is released. The hairpin structure of APOL1 is normally configured closed at neutral pH, however, the low pH of the lysosome disperses the salt bridges which stabilize the hairpin ‘hinge’, resulting in a conformational change (Vanhollebeke and Pays, 2006). This reveals a membrane-addressing domain and the BH3 pore-forming domain (Vanhollebeke and Pays, 2006). With both of these domains exposed, APOL1 embeds in the lysosomal membrane, forming anionic pores and thus perturbing the osmotic balance of the organelle. This leads to lysis of the parasite, either by simple mechanical disruption due to swelling of the organelle or the leakage of digestive enzymes into the main cell body (Vanhamme et al. 2003; Pays et al. 2006; Vanhollebeke and Pays, 2010). As both HPR and APOL1 are found in TLF-2, it is likely that the lysis method for this particle involves both of these proteins, although the method of entry for TLF-2 only partially involves the HpHbR receptor (Bullard et al. 2012). The mechanism by which the majority of TLF-2 is bound and internalized by the parasite is currently unknown, but may involve weak interactions between IgM and the VSG coat of the parasite or a second receptor for TLF that has been described (Drain et al. 2001; Green et al. 2002; Vanhollebeke and Pays, 2010). The second trypanosome receptor for TLF is unidentified but was first described from low temperature binding assays showing TLF-1 is internalized by both a high-affinity low copy number receptor (now known to be HpHbR) and a second low-affinity, high copy number receptor (Drain et al. 2001). The putative second receptor was further investigated using HDL competition, binding and uptake assays (Green et al. 2002) and shown to act as a general lipoprotein scavenger which binds multiple classes of lipoprotein, including HDL, LDL, oxidized LDL and TLF.
Primates have likely evolved this highly effective innate immunity based on APOL1 because trypanosomes have escaped the effects of the adaptive immune response due to antigenic variation (Barry and McCulloch, 2001; Pays et al. 2001). Trypanosomes are covered in a highly immunogenic, dense, variable surface glycoprotein coat, which is rapidly turned over with the parasite membrane and frequently switched to a different VSG, rendering antibody-based immunity ineffective. The high turnover of the parasite's surface membrane requires a large amount of lipid, however, trypanosomes are lipid auxotrophs and so obtain their lipids in the form of HDL from their host (Green et al. 2002). The packaging of APOL1 into HDL exploits the parasite's requirement for this essential nutrient to deliver the highly toxic APOL1 molecule.
Dating the emergence of trypanolytic APOL1 in primates is challenging as the APOL gene cluster has undergone numerous expansion, duplication and loss events during primate evolution (Fig. 1) (Smith and Malik, 2009), although it must precede the time when the hominidae and cercopithecidae primate lineages diverged as both possess lytic APOL1 (approximately 20 mya) (Seed and Sechelski, 1990; Lugli et al. 2004). The addition of a secretory signal peptide to APOL1 appears to be a unique key factor allowing its use as a protective element against trypanosomes, as all other APOL proteins are intracellular (Vanhollebeke and Pays, 2006). The signal peptide appears to have originated due to a gain of function mutation after the divergence of APOL1 and APOL2 (Smith and Malik, 2009). Although the APOL1 defensive strategy works successfully against most species of African trypanosome, two human infective trypanosome sub-species have evolved to counter the innate defence provided by primate APOL1. Interestingly, both sub-species utilize a truncated VSG as an essential component of their resistance mechanisms. As several other genes also derive from VSGs, including the transferrin receptor ESAG6/ESAG7, it would appear that the huge VSG repertoire of these parasites provides a powerful resource that can be utilized by trypanosomes to quickly evolve to infect new hosts and overcome novel challenges (Jackson et al. 2013).
TRYPANOSOMA B. RHODESIENSE RESISTANCE TO TLF AND APOL1
Work to elucidate how the human infective sub-species of T. brucei overcame APOL1-mediated lysis initially focused on T. b. rhodesiense. A defining characteristic of human serum resistance within this sub-species is its variable phenotype. The serum resistance phenotype can vary during animal passage, with individual passages exhibiting the phenotype to differing degrees (Targett and Wilson, 1973; Willett and Fairbairn, 1955). It was noted that the expression of the resistance phenotype closely correlates with changes to the expressed VSG (van Meirvenne et al. 1976). This implicated an expression site associated gene (ESAG) being responsible for resistance (Fig. 2) (Rifkin et al. 1994). Comparison of isogenic serum-susceptible and serum-resistant T. b. rhodesiense lines provided an invaluable research tool and by comparing mRNA, a VSG-like gene transcript associated with resistance was identified (De Greef et al. 1989; De Greef et al. 1992). Both resistant and sensitive T. b. rhodesiense possess the serum resistance associated (SRA) gene, but only resistant lines actively transcribe it. Conclusive proof that human serum resistance in T. b. rhodesiense was due to this single gene was shown when transgenic T. b. brucei expressing SRA gained resistance to lysis by human serum (Xong et al. 1998). Anecdotally, this result was solidified by accidental infection of a human with this T. b. brucei–SRA strain (Gibson, 2005), demonstrating that the SRA gene alone is sufficient to confer human serum resistance.
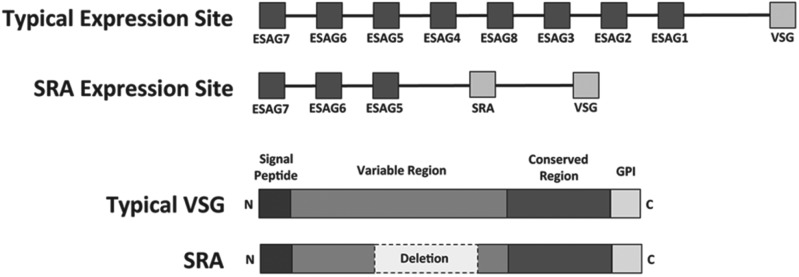
Fig. 2.
Human serum resistance of T. b. rhodesiense. (Upper) Schematic diagram of a typical trypanosome expression site and the SRA expression of T. b. rhodesiense (adapted from Gibson, 2005). (Lower) Diagram of the typical domains of a VSG and the approximate location of the 378 bp deletion in the SRA gene (adapted from Campillo and Carrington, 2003).
SRA has been shown to be present in nearly all T. b. rhodesiense lines (Gibson et al. 2002) although this is a circular argument, i.e. the presence of SRA is diagnostic of T. b. rhodesiense, so T. b. rhodesiense must always possess SRA. Structurally, the SRA gene appears to be a truncated VSG with a large deletion of a region in the centre of the sequence encoding the N-terminal domain (De Greef et al. 1992; De Greef and Hamers, 1994; Xong et al. 1998). SRA is present on the cell surface (Milner and Hajduk, 1999), where it is internalized in the flagellar pocket during cell surface protein turnover, leading to SRA presence in the endosomes and lysosome (Vanhamme et al. 2003; Oli et al. 2006; Shiflett et al. 2007). This is similar to the location of APOL1 in the endosomal pathway before lysis. The deletion of 126 amino acids in SRA removes two surface loops normally present in a VSG protein, exposing the internal α-helices (Fig. 2) (Campillo and Carrington, 2003). Based on modelled tertiary structure, it was proposed that the deletion resulted in human serum resistance by allowing an inter-chelating interaction between the exposed N-terminal helices of SRA and the C-terminal helical section of APOL1 after the protein undergoes conformational change in the acidic environment of the lysosome (Vanhamme et al. 2003; Vanhamme and Pays, 2004).
SRA is conserved at the nucleotide level in the T. b. rhodesiense population, with less than 3% sequence variation between strains (Gibson et al. 2002). The polymorphisms present in the SRA gene, which can be differentiated by allele-specific PCR (Gibson et al. 2002), divide T. b. rhodesiense into two groups, ‘Northern’ and ‘Southern’, broadly along geographical lines (Gibson et al. 2002; MacLean et al. 2004, Balmer et al. 2001). This geographical segregation of SRA variants associates closely with the molecular and clinical disease profiles that have also detected delineation between Northern and Southern T. b. rhodesiense strains (Gibson et al. 1980; Hide et al. 1991; MacLeod et al. 2000; MacLean et al. 2004).
The conservation of the SRA gene sequence combined with population analyses, which have highlighted the close genetic relationship between sympatric T. b. rhodesiense and T. b. brucei strains (Hide et al. 1994; MacLeod et al. 2000), indicate that although the formation of SRA is likely to have been the result of a single gene recombination event (Campillo and Carrington, 2003), human infectivity has spread in East Africa by genetic exchange of the SRA gene into genetically diverse T. b. brucei backgrounds, thereby creating new strains of T. b. rhodesiense (Gibson et al. 2002; Duffy et al. 2013). This potential for genetic exchange between T. b. brucei and T. b. rhodesiense, alongside the demonstration that expression of the SRA gene is all that is necessary for human serum resistance (Xong et al. 1998) has implications for the evolution of the disease, as the SRA gene may be transferred onto new genetic backgrounds resulting in genotypes with altered pathogenicity.
The discovery of SRA has led to advancements in diagnosis and suggested preventative action to combat sleeping sickness caused by T. b. rhodesiense. With the advent of specific PCR markers for SRA, trypanosomes with the potential to infect humans can be identified unambiguously without the need for laborious human serum resistance assays such as the BIIT (Welburn et al. 2001; Gibson et al. 2002; Radwanska et al. 2002). By providing a robust and specific single gene assay, requiring as little as a single parasite in starting material, SRA-PCR has proved revolutionary in understanding the role of wildlife and livestock in the epidemiology of the disease. For example, traditional microscopy techniques and HSR assays estimated the number of domestic cattle carrying human infective T. b. rhodesiense to be approximately 1%. PCR analysis has indicated that instead this value is closer to 18% (Welburn et al. 2001). Although the discovery of SRA has been a major boon to the understanding of T. b. rhodesiense genetics and biology, this gene is not present in the dominant human infective trypanosome sub-species, T. b. gambiense. Additionally, several strains have been described from T. b. rhodesiense foci that are human serum resistant but for which the SRA gene cannot be amplified by PCR (De Greef et al. 1992; Enyaru et al. 2006). Whether this is due to divergent SRA sequence in these strains or a novel resistance mechanism is unknown.
TRYPANOSOMA B. GAMBIENSE RESISTANCE TO TLF AND APOL1
Investigating the human serum resistance phenotype of T. b. gambiense has been hampered by the difficulty in working with the sub-species in a laboratory setting. Trypanosoma b. gambiense typically grows to very low parasitaemia and there have been immense difficulties in adapting it to in vitro or in vivo models. However, recent advances have allowed the generation of laboratory adapted lines and successful transfections have now been achieved (Baltz et al. 2009; Capewell et al. 2013; Uzureau et al. 2013). It is now possible to unravel the intricacies of the resistance phenotype of T. b. gambiense. An important first step was the observation that T. b. gambiense does not appear to internalize fluorescently tagged TLF-1 (Kieft et al. 2010; Capewell et al. 2011). This suggested that avoidance of TLF-1 is a feature of human serum resistance in T. b. gambiense. Several polymorphisms were identified in the HpHbR gene unique to T. b. gambiense relative to other T. brucei that affected TLF-1 uptake (Kieft et al. 2010). Subsequent research has confirmed that a single polymorphism reduced the binding affinity of HpHbR for its ligand 20-fold (DeJesus et al. 2013; Higgins et al. 2013). This polymorphism appears to be conserved across several T. b. gambiense foci (Symula et al. 2012). Avoidance of TLF-1 therefore appears to be a conserved trait in T. b. gambiense. Over-expression of a functional T. b. brucei HpHbR in T. b. gambiense results in normal TLF-1 uptake and restricted growth (Capewell et al. 2013). Incubating wild-type T. b. gambiense with serum containing high levels of TLF-1 also appears to result in the serum resistance mechanism of T. b. gambiense becoming overwhelmed (Uzureau et al. 2013). While the reduced expression and activity of HpHbR provide a plausible explanation for how T. b. gambiense avoids lysis by TLF-1, it does not explain how T. b. gambiense is able to avoid uptake and consequent lysis by TLF-2. This lytic particle is only partially internalized via HpHbR (Bullard et al. 2012). Additionally, T. b. gambiense exposed to recombinant APOL1 internalized by non-specific fluid phase endocytosis are still resistant despite observable uptake and trafficking of the lytic protein to the lysosome (Capewell et al. 2011).
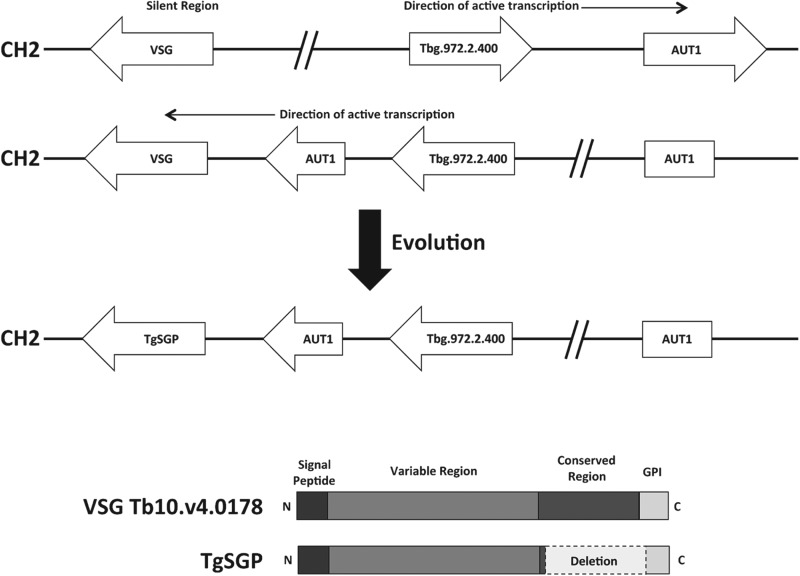
In an effort to discover the factor that confers resistance to TLF-2 and APOL1, the genomes of both T. b. brucei and T. b. gambiense were interrogated (Berriman, 2005; Jackson et al. 2010). To date, only one gene has been found to be unique to T. b. gambiense, the gene encoding the T. gambiense-specific glycoprotein (TgsGP) (Berberof et al. 2001). This gene was found while attempting to discover truncated VSGs similar to SRA in T. b. gambiense. Unlike SRA, TgsGP is not found in an expression site but is rather transcribed from a core chromosomal locus. This region was formed by an inversion event that disrupted part of chromosome 2 that allowed an ordinarily silent region containing VSGs to be transcribed (Fig. 3) (Berberof et al. 2001; Felu et al. 2007). This inversion event is ancestral and specific to T. b. gambiense (Felu et al. 2007). A VSG or VSG pseudogene close to an AUT1 fragment cleaved by the inversion has since evolved into the TgsGP gene. TgsGP appears to be highly conserved across several T. b. gambiense disease foci so is likely to have evolved only once (Gibson et al. 2010). It differs from other VSGs in that it does not possess the conserved VSG C-terminal domain and possesses a GPI anchor related to that of ESAG6s (Fig. 3) (Felu et al. 2007). It is closely related to the VSG Tb10.v4·0178, sharing more than 80% genetic similarity, indicating a possible ancestral VSG (Gibson et al. 2010). Initially TgsGP was thought unlikely to be involved in human serum resistance as ectopic expression of the gene in T. b. brucei did not confer resistance (Berberof et al. 2001). However, this does not take into account other factors that may be present in T. b. gambiense and absent in T. b. brucei that are necessary for TgsGP to function. When the TgsGP gene was deleted from the genome of T. b. gambiense, parasites became sensitive to both human serum and APOL1 (Capewell et al. 2013; Uzureau et al. 2013), although the parasites were still resistant to TLF-1. Removal of the TgsGP gene from T. b. gambiense parasites ectopically expressing a functional T. b. brucei HpHbR resulted in the parasites becoming sensitive to TLF-1 (Capewell et al. 2013; Uzureau et al. 2013). How TgsGP confers resistance is still unknown as there is no direct interaction between APOL1 and TgsGP despite both being found in similar endosomal compartments (Uzureau et al. 2013). Serial modification and ectopic expression of TgsGP indicated the presence of a specific Β-sheet structure within the protein that is essential for TgsGP to function. It was hypothesized that this Β-sheet structure interacts with and strengthens the parasite's internal membranes to allow them to resist the pore-forming activity of APOL1. Support for this hypothesis is based on the observation that recombinant TgsGP and derived peptides integrate with artificial lipid bilayers and can affect lateral flow of the parasite surface membrane (Uzureau et al. 2013). This suggests that membrane fluidity is different in T. b. gambiense (that contains TgsGP) compared with T. b. brucei and suggests a causal relationship with the human serum resistance phenotype. This is indeed a tempting hypothesis, although a direct relationship between the observation and human infectivity has not been shown. Recombinant TgsGP and related peptides have a negligible effect on human serum resistance when incubated with T. b. brucei. This fact, coupled to the observations that ectopic expression of TgsGP in T. b. brucei does not confer resistance and that TgsGP knockout T. b. gambiense still displays a markedly higher resistance to human serum than other T. b. brucei, suggests other factors may be present in T. b. gambiense that function in concert with TgsGP (Berberof et al. 2001; Capewell et al. 2011; Uzureau et al. 2013).
Fig. 3.
Human serum resistance of T. b. gambiense. (Upper) Model of the chromosomal inversion on chromosome 2 that allowed the silent region containing the progenitor of TgsGP to be constitutively transcribed and undergo selection. The inversion is present on one homologue of chromosome 2 and is conserved across all T. b. gambiense (adapted from Berberof et al. 2001; Felu et al. 2007). (Lower) Diagram of the typical domains of a VSG and the approximate location of the C-terminal deletion in TgsGP (adapted from (Gibson et al. 2010)).
One possible candidate for involvement is the cysteine protease protein family. These enzymes are heavily involved in degradation of host proteins, with several found in the endosomal pathway and lysosome. It has been demonstrated that cysteine protease inhibitors affect the ability of T. b. brucei to resist lysis by human serum, perhaps by affecting degradation of the TLF particles or APOL1 itself (Bishop et al. 2001). General inhibition of cysteine peptidase in T. b. gambiense strains without TgsGP reduced their capacity to resist human serum and APOL1 to a level approximately equivalent to T. b. brucei (Uzureau et al. 2013). RNAi and knockouts of ICP (inhibitor of cysteine peptidase) cause a general increase in cysteine protease expression in T. b. brucei and also raise human serum resistance, suggesting that these proteases could be a factor (Uzureau et al. 2013). However, an experiment that over-expresses cysteine proteases in a T. b. brucei with ectopic TgsGP expression has not been undertaken. This would confirm if high cysteine protease activity is indeed the missing factor necessary for TgsGP to function in T. b. brucei. While higher expression of cysteine proteases in T. b. gambiense may be the effector that leads to greater human serum resistance, it was also noted that the pH of the endocytic compartment of T. b. gambiense is slightly lower than that of T. b. brucei (Uzureau et al. 2013). This may increase the degradation of APOL1 and elicit a protective effect. Several T. brucei cysteine proteases, particularly cathepsins, are more active at low pH (O'Brien et al. 2008). Again, this hypothesis has not been tested and is at present conjecture.
Taken together, it would appear that the resistance mechanism of T. b. gambiense involves several factors: (1) reduction of lytic particle uptake by reducing expression and binding affinity of the HpHb receptor, (2) expression of TgsGP possibly affecting membrane fluidity and resistance to APOL1 disruption and (3) increased amounts of cysteine proteases that aid degradation of APOL1.
EVOLVING PRIMATE RESISTANCE TO T. B. RHODESIENSE AND T. B. GAMBIENSE
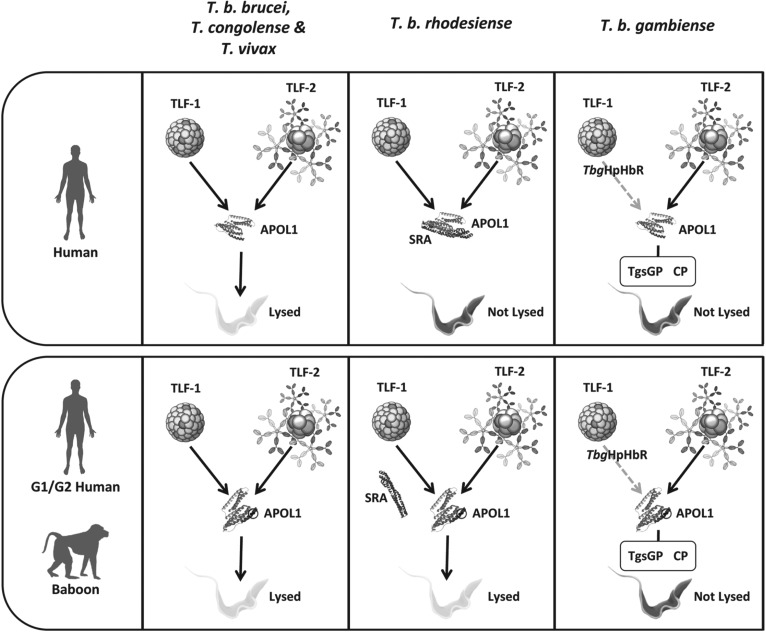
Although the mechanisms for how primates resist trypanosome infection and how some trypanosomes have overcome this resistance are becoming clearer, the evolutionary arms race between primates and trypanosomes continues. It is becoming apparent that mechanisms to combat infection of both T. b. rhodesiense and T. b. gambiense in primates have evolved and are continuing to evolve. Although trypanolytic APOL1 evolved in the ancestors of catarrhine primates, it appears to have diverged into two distinct lineages that exhibit differing efficacies of trypanosome lysis. APOL1 from the hominidae lineage (gorillas and humans) is effective against most trypanosomes (Seed and Sechelski, 1990; Lugli et al. 2004), except T. b. rhodesiense and T. b. gambiense while APOL1 from the cercopithecidae lineage (baboons and macaques) is also able to lyse T. b. rhodesiense (Seed and Sechelski, 1990; Kageruka et al. 1991; Thomson et al. 2009). Cercopithecidae lineage APOL1 is able to lyse T. b. rhodesiense due to a modification of the SRA interacting domain of APOL1 at the C-terminus of the protein (Fig. 4), which disrupts SRA binding after APOL1 has undergone conformational change (Lecordier et al. 2009; Thomson et al. 2009). Recombinant protein created by deleting this domain from human APOL1 is also able to lyse T. b. rhodesiense, suggesting that evolving a modification to this region of APOL1 would render humans resistant to T. b. rhodesiense (Lecordier et al. 2009). There is preliminary evidence that this may have occurred with the identification of selection for two specific APOL1 alleles (G1 and G2) in African Americans with ancestry in sub-Saharan Africa (Genovese et al. 2010). Both the G1 and G2 alleles of APOL1 show modification of the SRA binding region (Fig. 4) and recombinant versions of these alleles, particularly G2, are able to reduce the growth of T. b. rhodesiense parasites in vitro (Genovese et al. 2010). However, presence of these alleles also correlates with increased incidence of kidney disease, particularly in individuals homozygous for either allele (Freedman et al. 2010; Genovese et al. 2010; Tzur et al. 2010). The maintenance of a trait that is beneficial to heterozygotes but deleterious to homozygotes parallels the well-described co-evolutionary interplay between sickle-cell anaemia and Plasmodium (Williams et al. 2005). However, to date, no case-controlled study using natural populations has been undertaken to test the hypothesis that G1/G2 selection is due to pressure from trypanosomes. A study examining APOL1 selection across Africa found extremely low prevalence for G2, and G1 was only present in a population not exposed to T. b. rhodesiense (Ko et al. 2013). They did, however, find a much higher number of non-synonymous mutations in the SRA binding domain of APOL1 than would be expected by chance.
Fig. 4.
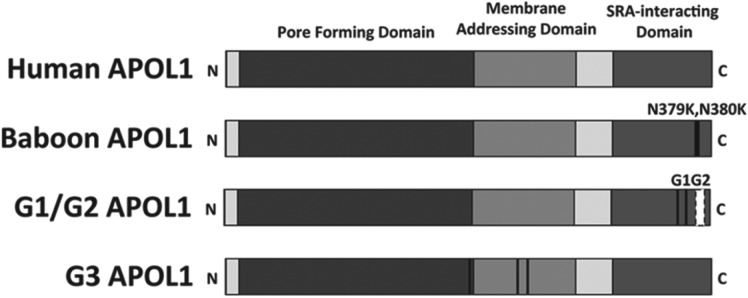
APOL1 variants. Several variants of APOL1 show differing lysis efficacy against trypanosomes. Wild-type human APOL1 can lyse T. congolense, T. vivax and T. b. brucei. Baboon APOL1 possesses two consecutive lysines rather than asparagines in the SRA-interacting domain of APOL1 (black lines). This reduces the binding affinity of SRA to APOL1, allowing the baboon protein to lyse T. b. rhodesiense. G1/G2 human alleles are under selection in populations of African descent and also possess modifications to the SRA-interacting domain of APOL1 (black lines, white box). Like baboon APOL1, these alleles demonstrate efficacy against T. b. rhodesiense. The G3 allele is under selection in populations exposed to T. b. gambiense but efficacy of this allele against trypanosome sub-species has not been assessed. Unlike G1/G2, G3 mutations lie within the pore-forming and membrane-addressing domains of APOL1 (black lines).
While less well studied than T. b. rhodesiense, it is also possible that there are primates or human populations that have evolved APOL1 alleles that protect against T. b. gambiense. The Bambuti people of the Mbomo region in the Democratic Republic of the Congo have long been believed to be less susceptible to African sleeping sickness (Frezil, 1983), although no controlled study has been performed to test this assumption or investigate their APOL1 alleles. It is also becoming increasingly apparent that infection by T. b. gambiense is not always fatal with the recent identification of asymptomatic and self-cure cases from Côte d'Ivoire (Ilboudo et al. 2012; Jamonneau et al. 2012). The APOL1 sequences from these individuals have not been assessed, although a recent study assessing APOL1 selection across Africa has identified an allele termed G3 that is under selection in the Fulani people of Cameroon, a region affected by T. b. gambiense African sleeping sickness (Ko et al. 2013). This particular allele differs from the G1/G2 variants that have a mutation in the SRA interacting domain and instead possesses a mutation in the membrane-addressing domain of APOL1 (Fig. 4). It is, as yet, unknown if this variant is protective against T. b. gambiense. Looking outside human populations and to the Cercopithecidae lineage of APOL1, the baboon species Papio papio appears to only be transiently infected by T. b. gambiense. This species range overlaps with that of T. b. gambiense, while the ranges of other Papio species that are not resistant to the disease do not overlap (Kageruka et al. 1991; Lecordier et al. 2009; Thomson et al. 2009). It is possible that this species of baboon has evolved an APOL1 variant that is able to lyse T. b. gambiense due to exposure to the disease. Finally, while the majority of effort has primarily concentrated on finding APOL1 variants toxic to human infective trypanosomes, other proteins may also contribute. For example, specific alleles of IL-6 and IL-10 have been associated with resistance to T. b. gambiense in humans (Courtin et al. 2006, 2007; Garcia et al. 2006). A recent study has also reported evidence that alleles containing a duplication of the parasite receptor ligand, HPR, are present at high frequency in Central and West African populations endemic to T. b. gambiense, relative to the global distribution. However, whether such duplication offers any protective effect against T. b. gambiense sleeping sickness has not yet been experimentally tested (Hardwick et al. 2014). There was no significant link between HPR duplication and the presentation of sleeping sickness in children in affected areas, although this may be due to the low power of the study. To discover other possible factors involved in genetic susceptibility to African sleeping sickness, large-scale genome-wide association studies should be undertaken.
DISCUSSION AND FUTURE DIRECTIONS
The co-evolutionary arms race between trypanosomes and primates is a fascinating case study in parasite and host interactions. As the mammalian adaptive immune system is rendered ineffective by the trypanosomes’ antigenic variation strategy, primates have evolved specific countermeasures to target trypanosomes utilizing the trypanolytic protein APOL1 bound to HDL (Summary: Fig. 5). By evolving a trypanolytic HDL, primates were able to exploit both the trypanosomes’ high lipid requirement necessary for fast turnover of the VSG coat to maintain antigenic variation and the lack of a haem production pathway in the parasite. However, two sub-species of T. brucei have evolved their own counters to overcome lysis by human serum and APOL1. Both resistance mechanisms appear to utilize a truncated VSG as an essential component, SRA in T. b. rhodesiense and TgsGP in T. b. gambiense. This highlights the evolutionary potential that the huge VSG repertoire provides this parasite. Although not covered during this review, there are also two other potential serum resistance mechanisms in T. brucei that do not utilize SRA or TgsGP. In East sub-Saharan Africa, a small number of human infective trypanosomes have been identified from T. b rhodesiense foci that do not possess the SRA gene (De Greef et al. 1989; Rifkin et al. 1994; Enyaru et al. 2006). In Western sub-Saharan Africa, sympatric with T. b gambiense, a further group of human infective trypanosomes has been identified. These are termed group 2 T. b. gambiense as they do not fit into the classical genetic profiles associated with the much more prevalent group 1 T. b. gambiense (Gibson, 1986). Unlike group 1, group 2 T. b. gambiense do not possess TgsGP and the resistance mechanism is variably expressed in a manner reminiscent of T. b. rhodesiense. The resistance mechanism does not appear to correlate with changes in expression site, however (Capewell et al. 2011). How non-SRA T. b. rhodesiense and group 2 T. b. gambiense are able to overcome APOL1 remains unclear, although it highlights the high potential for T. brucei to quickly evolve to infect new hosts and overcome innate immunity.
Fig. 5.
Summary of the co-evolutionary arms race between African trypanosomes and the primate host. Humans are protected from infection from the majority of Africa trypanosome species by two serum trypanolytic factors, TLF-1 and TLF-2, which exploit parasite nutrient scavenging pathways to take up and deliver lytic APOL1 protein to the lysosome. A conformational change in the low pH environment of the lysosome releases APOL1 and exposes domains that allow it to form anionic pores in the membrane, leading to osmotic imbalance and cell lysis. Two sub-species of T. brucei have evolved specific mechanisms to overcome this innate resistance. In T. b. rhodesiense, expression of the SRA gene, a truncated VSG, confers resistance to lysis by both TLF-1 and 2. Deletion of the VSG surface loops results, ultimately, in its trafficking through the endocytic pathway, where it is able to bind APOL1 and prevent pore-forming activity in the lysosome. In contrast, T. b. gambiense has evolved a complex, multi-component mechanism of HSR involving reduction in the binding affinity of TbgHpHbR for TLF-1, the expression of a T. b. gambiense specific truncated VSG (TgsGP) which conceivably increases resistance of the lysosomal membrane to APOL1 disruption and enhanced expression or activity of cysteine proteases (CP) that aid degradation of APOL1 within the endocytic pathway. Recently, the discovery of certain APOL1 variants has suggested the evolution of counter measures to at least one of these resistance mechanisms. APOL1 from a subset of primates of the cercopithecidae lineage are naturally resistant to T. b. rhodesiense but not T. b. gambiense infection as a result of mutations in the SRA interacting domain that impair SRA binding and restore APOL1 activity. In an example of convergent evolution, two haplotypes displaying similar mutations, termed G1 and G2, have been identified in a number of human populations of African origin.
It is becoming apparent that the evolutionary arms race between primates and T. brucei is continuing, with several human and primate populations displaying resistance to both T. b. rhodesiense and T. b gambiense. Understanding the complex co-evolution that has occurred between trypanosomes and primates may lead to prospective disease interventions. For example, inhibitors or antibodies that target the essential proteins involved in each sub-species’ resistance mechanism (SRA and TgsGP) would render these parasites susceptible to normal innate resistance and APOL1. An alternative approach is to identify APOL1 variants or other genes present in trypanosome-resistant human and primate populations that may serve as a universal therapy for all African trypanosomes. Once identified, these APOL1 variants must be targeted to trypanosomes as APOL1 uptake when not bound to a facilitating ligand is slow and inefficient (Vanhamme et al. 2003; Baral et al. 2006). One proposed solution involves the distribution of transgenic cows across Africa that express either recombinant baboon APOL1 (Thomson et al. 2009) or truncated human APOL1 (Lecordier et al. 2009). Mice models expressing these genes ectopically are unable to be infected by either T. b. brucei or T. b. rhodesiense, if expressed in concert with HPR and APOA1 (Thomson et al. 2009). An alternative proposed delivery mechanism is the conjugation of variant APOL1 to antibody fragments that target conserved motifs on parasite VSGs (Baral et al. 2006). A caveat to these proposed interventions is that the APOL1 variant used by each is not lytic to the most prevalent human infective trypanosome, T. b. gambiense (Lecordier et al. 2009; Thomson et al. 2009). It is possible that usage of such APOL1 variants would select for increased incidence of human disease by eradicating the competitor species such as Trypanosoma congolense, Trypanosoma vivax or Trypanosoma brucei. Nevertheless, it is clear that understanding the co-evolution of primates and African trypanosomes is a powerful tool in combating human trypanosomiasis.
FINANCIAL SUPPORT
The Wellcome Trust Centre for Molecular Parasitology is supported by core funding from the Wellcome Trust [085349]. PC, CC, AC, WW and AM are funded by a Wellcome Senior Fellowship Grant awarded to AM.
REFERENCES
- Balmer O., Beadell J. S., Gibson W. and Caccone A. (2001). Phylogeography and taxonomy of Trypanosoma brucei. PLoS Neglected Tropical Diseases 5(2), . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltz T., Giroud C., Ottones F., Coustou V., Dacheux D., Biteau N., Miezan B., Van Reet N., Carrington M. and Doua F. (2009). Murine models for Trypanosoma brucei gambiense disease progression – from silent to chronic infections and early brain tropism. PLOS Neglected Tropical Diseases 3, . doi: 10.1371/journal.pntd.0000509.t003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral T. N., Magez S., Stijlemans B., Conrath K., Vanhollebeke B., Pays E., Muyldermans S. and De Baetselier P. (2006). Experimental therapy of African trypanosomiasis with a nanobody-conjugated human trypanolytic factor. Nature Medicine 12, 580–584. doi: 10.1038/nm1395. [DOI] [PubMed] [Google Scholar]
- Barry J. D. and McCulloch R. (2001). Antigenic variation in trypanosomes: enhanced phenotypic variation in a eukaryotic parasite. Advances in Parasitology 49, 1–70. [DOI] [PubMed] [Google Scholar]
- Berberof M., Pérez-Morga D. and Pays E. (2001). A receptor-like flagellar pocket glycoprotein specific to Trypanosoma brucei gambiense. Molecular and Biochemical Parasitology 113, 127–138. [DOI] [PubMed] [Google Scholar]
- Berriman M. (2005). The genome of the African trypanosome Trypanosoma brucei. Science 309, 416–422. doi: 10.1126/science.1112642. [DOI] [PubMed] [Google Scholar]
- Bishop J. R., Shimamura M. and Hajduk S. L. (2001). Insight into the mechanism of trypanosome lytic factor-1 killing of Trypanosoma brucei brucei. Molecular and Biochemical Parasitology 118, 33–40. [DOI] [PubMed] [Google Scholar]
- Bullard W., Kieft R., Capewell P., Veitch N. J., Macleod A. and Hajduk S. (2012). Haptoglobin-hemoglobin receptor independent killing of African trypanosomes by human serum. Virulence 3, 72–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campillo N. and Carrington M. (2003). The origin of the serum resistance associated (SRA) gene and a model of the structure of the SRA polypeptide from Trypanosoma brucei rhodesiense. Molecular and Biochemical Parasitology 127, 79–84. doi: 10.1016/S0166-6851(02)00306-7. [DOI] [PubMed] [Google Scholar]
- Capewell P., Veitch N. J., Turner C. M. R., Raper J., Berriman M., Hajduk S. L. and Macleod A. (2011). Differences between Trypanosoma brucei gambiense groups 1 and 2 in their resistance to killing by trypanolytic factor 1. PLOS Neglected Tropical Diseases 5, . doi: 10.1371/journal.pntd.0001287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capewell P., Clucas C., DeJesus E., Kieft R. and Hajduk S. (2013). The TgsGP gene is essential for resistance to human serum in Trypanosoma brucei gambiense. PLOS Pathogens 9, . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtin D., Argiro L., Jamonneau V., N'dri L., N'guessan P., Abel L., Dessein A., Cot M., Laveissiere C. and Garcia A. (2006). Interest of tumor necrosis factor-alpha −308 G/A and interleukin-10 -592 C/A polymorphisms in human African trypanosomiasis. Infection, Genetics and Evolution 6, 123–129. doi: 10.1016/j.meegid.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Courtin D., Milet J., Jamonneau V., Yeminanga C. S., Kumeso V. K. B., Bilengue C. M. M., Betard C. and Garcia A. (2007). Association between human African trypanosomiasis and the IL6 gene in a Congolese population. Infection, Genetics and Evolution 7, 60–68. doi: 10.1016/j.meegid.2006.04.001. [DOI] [PubMed] [Google Scholar]
- De Greef C. and Hamers R. (1994). The serum resistance-associated (SRA) gene of Trypanosoma brucei rhodesiense encodes a variant surface glycoprotein-like protein. Molecular and Biochemical Parasitology 68, 277–284. [DOI] [PubMed] [Google Scholar]
- De Greef C., Imberechts H., Matthyssens G., Van Meirvenne N. and Hamers R. (1989). A gene expressed only in serum-resistant variants of Trypanosoma brucei rhodesiense. Molecular and Biochemical Parasitology 36, 169–176. doi: 10.1016/0166-6851(89)90189-8. [DOI] [PubMed] [Google Scholar]
- De Greef C., Chimfwembe E., Kihang'a Wabacha J., Bajyana Songa E. and Hamers R. (1992). Only the serum-resistant bloodstream forms of Trypanosoma brucei rhodesiense express the serum resistance associated (SRA) protein. Annales de la Société Belge de Médecine Tropicale 72 (Suppl. 1), 13–21. [PubMed] [Google Scholar]
- DeJesus E., Kieft R., Albright B., Stephens N. A. and Hajduk S. L. (2013). A single amino acid substitution in the Trypanosoma brucei gambiense haptoglobin-hemoglobin receptor abolishes TLF-1 binding. PLOS Pathogens 9(4), . doi: 10.1371/journal.ppat.1003317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drain J., Bishop J. R. and Hajduk S. L. (2001). Haptoglobin-related protein mediates trypanosome lytic factor binding to trypanosomes. Journal of Biological Chemistry 276, 30254–30260. doi: 10.1074/jbc.M010198200. [DOI] [PubMed] [Google Scholar]
- Duchateau P. N., Pullinger C. R., Orellana R. E., Kunitake S. T., Naya-Vigne J., O'Connor P. M., Malloy M. J. and Kane J. P. (1997). Apolipoprotein L, a new human high density lipoprotein apolipoprotein expressed by the pancreas. Identification, cloning, characterization, and plasma distribution of apolipoprotein L. Journal of Biological Chemistry 272, 25576–25582. [DOI] [PubMed] [Google Scholar]
- Duffy C. W., MacLean L., Sweeney L., Cooper A., Turner C. M. R., Tait A., Sternberg J., Morrison L. J. and Macleod A. (2013). Population genetics of Trypanosoma brucei rhodesiense: clonality and diversity within and between foci. PLOS Neglected Tropical Diseases 7, . doi: 10.1371/journal.pntd.0002526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enyaru J. C. K., Matovu E., Nerima B., Akol M. and Sebikali C. (2006). Detection of T.b. rhodesiense trypanosomes in humans and domestic animals in south east Uganda by amplification of serum resistance-associated gene. Annals of the New York Academy of Sciences 1081, 311–319. [DOI] [PubMed] [Google Scholar]
- Felgner P., Brinkmann U., Zillmann U. and Mehlitz D. (1981). Epidemiological studies on the animal reservoir of gambiense sleeping sickness. Part II. Parasitological and immunodiagnostic examination of the human population. Tropenmedizin und Parasitologie 32, 134–140. [PubMed] [Google Scholar]
- Felu C., Pasture J., Pays E. and Pérez-Morga D. (2007). Diagnostic potential of a conserved genomic rearrangement in the Trypanosoma brucei gambiense-specific TGSGP locus. American Journal of Tropical Medicine and Hygiene 76, 922–929. [PubMed] [Google Scholar]
- Fèvre E. M., Coleman P. G., Odiit M., Magona J. W., Welburn S. C. and Woolhouse M. E. (2001). The origins of a new Trypanosoma brucei rhodesiense sleeping sickness outbreak in eastern Uganda. Lancet 358, 625–628. [DOI] [PubMed] [Google Scholar]
- Fèvre E. M., Picozzi K., Fyfe J., Waiswa C., Odiit M., Coleman P. G. and Welburn S. C. (2005). A burgeoning epidemic of sleeping sickness in Uganda. Lancet 366, 745–747. [DOI] [PubMed] [Google Scholar]
- Freedman B. I., Kopp J. B., Langefeld C. D., Genovese G., Friedman D. J., Nelson G. W., Winkler C. A., Bowden D. W. and Pollak M. R. (2010). The apolipoprotein L1 (APOL1) gene and nondiabetic nephropathy in African Americans. Journal of the American Society of Nephrology 21, 1422–1426. doi: 10.1681/ASN.2010070730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frezil J. L. (1983). Human Trypanosomiasis in the Congo. ORSTOM, Paris, France. [Google Scholar]
- Garcia A., Courtin D., Solano P., Koffi M. and Jamonneau V. (2006). Human African trypanosomiasis: connecting parasite and host genetics. Trends in Parasitology 22, 405–409. doi: 10.1016/j.pt.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Genovese G., Friedman D. J., Ross M. D., Lecordier L., Uzureau P., Freedman B. I., Bowden D. W., Langefeld C. D., Oleksyk T. K., Uscinski Knob A. L., Bernhardy A. J., Hicks P. J., Nelson G. W., Vanhollebeke B., Winkler C. A., Kopp J. B., Pays E. and Pollak M. R. (2010). Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 329, 841–845. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson W. (1986). Will the real Trypanosoma b. gambiense please stand up. Parasitology Today 2, 255–257. [DOI] [PubMed] [Google Scholar]
- Gibson W. (2002). Will the real Trypanosoma brucei rhodesiense please step forward? Trends in Parasitology 18, 486–490. [DOI] [PubMed] [Google Scholar]
- Gibson W. (2005). The SRA gene: the key to understanding the nature of Trypanosoma brucei rhodesiense. Parasitology 131, 143. [DOI] [PubMed] [Google Scholar]
- Gibson W., Mehlitz D. and Lanham S. M. (1978). The identification of Trypanosoma brucei gambiense in Liberian pigs and dogs by isoenzymes and by resistance to human plasma. Tropenmedizin und Parasitologie 29, 335–345. [PubMed] [Google Scholar]
- Gibson W. C., Marshall T. F., Godfrey D. G., Lumsden W. H. R., Muller R. and Baker J. R. (1980). Numerical analysis of enzyme polymorphism: a new approach to the epidemiology and taxonomy of trypanosomes of the subgenus Trypanozoon. Advances in Parasitology 18, 175–246. [DOI] [PubMed] [Google Scholar]
- Gibson W., Backhouse T. and Griffiths A. (2002). The human serum resistance associated gene is ubiquitous and conserved in Trypanosoma brucei rhodesiense throughout East Africa. Infection, Genetics and Evolution: Journal of Molecular Epidemiology and Evolutionary Genetics in Infectious Diseases 1, 207–214. [DOI] [PubMed] [Google Scholar]
- Gibson W., Nemetschke L. and Ndung'u J. (2010). Conserved sequence of the TgsGP gene in Group 1 Trypanosoma brucei gambiense. Infection, Genetics and Evolution 10, 453–458. [DOI] [PubMed] [Google Scholar]
- Green H. P., Del Pilar Molina Portela M., St Jean E. N., Lugli E. B. and Raper J. (2002). Evidence for a Trypanosoma brucei lipoprotein scavenger receptor. Journal of Biological Chemistry 278, 422–427. doi: 10.1074/jbc.M207215200. [DOI] [PubMed] [Google Scholar]
- Hager K. M., Pierce M. A., Moore D. R., Tytler E. M., Esko J. D. and Hajduk S. L. (1994). Endocytosis of a cytotoxic human high density lipoprotein results in disruption of acidic intracellular vesicles and subsequent killing of African trypanosomes. Journal of Cell Biology 126, 155–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajduk S. L., Moore D. R., Vasudevacharya J., Siqueira H., Torri A. F., Tytler E. M. and Esko J. D. (1989). Lysis of Trypanosoma brucei by a toxic subspecies of human high density lipoprotein. Journal of Biological Chemistry 264, 5210–5217. [PubMed] [Google Scholar]
- Hardwick R. J., Ménard A., Sironi M., Milet J., Garcia A., Sese C., Yang F., Fu B., Courtin D. and Hollox E. J. (2014). Haptoglobin (HP) and haptoglobin-related protein (HPR) copy number variation, natural selection, and trypanosomiasis. Human Genetics 133, 69–83. doi: 10.1007/s00439-013-1352-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington J. M., Widener J., Stephens N., Johnson T., Francia M., Capewell P., Macleod A. and Hajduk S. L. (2010). The plasma membrane of bloodstream-form African trypanosomes confers susceptibility and specificity to killing by hydrophobic peptides. Journal of Biological Chemistry 285, 28659–28666. doi: 10.1074/jbc.M110.151886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hide G., Buchanan N., Welburn S., Maudlin I., Barry J. D. and Tait A. (1991). Trypanosoma brucei rhodesiense: Characterisation of stocks from Zambia, Kenya, and Uganda using repetitive DNA probes. Experimental Parasitology 72, 430–439. [DOI] [PubMed] [Google Scholar]
- Hide G., Welburn S. C., Tait A. and Maudlin I. (1994). Epidemiological relationships of Trypanosoma brucei stocks from south east Uganda: evidence for different population structures in human infective and non-human infective isolates. Parasitology 109, 95–111. [DOI] [PubMed] [Google Scholar]
- Higgins M. K., Tkachenko O. and Brown A. (2013). Structure of the trypanosome haptoglobin–hemoglobin receptor and implications for nutrient uptake and innate immunity. Proceedings of the National Academy of Sciences USA 110, 1905–1910. doi: 10.1073/pnas.1214943110/-/DCSupplemental. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilboudo H., Berthier D., Camara M. and Camara O. (2012). APOL1 expression is induced by Trypanosoma brucei gambiense infection but is not associated with differential susceptibility to sleeping sickness. Infection, Genetics and Evolution 12, 1519–1523. [DOI] [PubMed] [Google Scholar]
- Jackson A. P., Sanders M., Berry A., McQuillan J., Aslett M. A., Quail M. A., Chukualim B., Capewell P., MacLeod A. and Melville S. E. (2010). The genome sequence of Trypanosoma brucei gambiense, causative agent of chronic human African trypanosomiasis. PLOS Neglected Tropical Diseases 4, . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson A. P., Berriman M., Allison H. C., Barry J. D., Field M. C. and Hertz-Fowler C. (2013). A cell-surface phylome for African trypanosomes. PLOS Neglected Tropical Diseases 7, . doi: 10.1371/journal.pntd.0002121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamonneau V., Ilboudo H., Kaboré J., Kaba D., Koffi M., Solano P., Garcia A., Courtin D., Laveissiere C., Lingue K., Büscher P. and Bucheton B. (2012). Untreated human infections by Trypanosoma brucei gambiense are not 100% fatal. PLOS Neglected Tropical Diseases 6, . doi: 10.1371/journal.pntd.0001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kageruka P., Mangus E., Bajyana Songa E., Nantulya V., Jochems M., Hamers R. and Mortelmans J. (1991). Infectivity of Trypanosoma (Trypanozoon) brucei gambiense for baboons (Papio hamadryas, Papio papio). Annales de la Société Belge de Médecine Tropicale 71, 39–46. [PubMed] [Google Scholar]
- Kieft R., Capewell P., Turner C. M. R., Veitch N. J., Macleod A. and Hajduk S. (2010). Mechanism of Trypanosoma brucei gambiense (group 1) resistance to human trypanosome lytic factor. Proceedings of the National Academy of Sciences USA 107, 16137–16141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko W.-Y., Rajan P., Gomez F., Scheinfeldt L., Froment A., Nyambo T. B., Omar S. A., Wambebe C., Ranciaro A., Hirbo J. B. and Tishkoff S. A. (2013). Identifying Darwinian selection acting on different human APOL1 variants among diverse African populations. American Journal of Human Genetics 93, 54–66. doi: 10.1016/j.ajhg.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korený L., Lukeš J. and Oborník M. (2010). Evolution of the haem synthetic pathway in kinetoplastid flagellates: an essential pathway that is not essential after all? International Journal for Parasitology 40, 149–156. doi: 10.1016/j.ijpara.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Laveran A. and Mesnil F. (1912). Trypanosomes et Trypanosomiases In Trypanosomiase Humaine ou Maladie du Sommeil. Masson et Cie, Paris, France. [Google Scholar]
- Lecordier L., Vanhollebeke B., Poelvoorde P., Tebabi P., Paturiaux-Hanocq F., Andris F., Lins L. and Pays E. (2009). C-terminal mutants of Apolipoprotein L-I efficiently kill both Trypanosoma brucei brucei and Trypanosoma brucei rhodesiense. PLOS Pathogens 5, . doi: 10.1371/journal.ppat.1000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugli E. B., Pouliot M., Portela M. D. P. M., Loomis M. R. and Raper J. (2004). Characterization of primate trypanosome lytic factors. Molecular and Biochemical Parasitology 138, 9–20. doi: 10.1016/j.molbiopara.2004.07.004. [DOI] [PubMed] [Google Scholar]
- Lutz R. J. (2000). Role of the BH3 (Bcl-2 homology 3) domain in the regulation of apoptosis and Bcl-2-related proteins. Biochemical Society Transactions 28, 51–56. [DOI] [PubMed] [Google Scholar]
- MacLean L., Chisi J. E., Odiit M., Gibson W. C., Ferris V., Picozzi K. and Sternberg J. M. (2004). Severity of human African trypanosomiasis in East Africa is associated with geographic location, parasite genotype, and host inflammatory cytokine response profile. Infection and Immunity 72, 7040–7044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod A., Tweedie A., Welburn S. C., Maudlin I., Turner C. M. R. and Tait A. (2000). Minisatellite marker analysis of Trypanosoma brucei: reconciliation of clonal, panmictic, and epidemic population genetic structures. Proceedings of the National Academy of Sciences USA 97, 13442–13447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehlitz D. (1979). Trypanosome infections in domestic animals in Liberia. Tropenmedizin und Parasitologie 30, 212–219. [PubMed] [Google Scholar]
- Mehlitz D., Brinkmann U. and Haller L. (1981). Epidemiological studies on the animal reservoir of Gambiense sleeping sickness. Part I. Review of literature and description of the study areas. Tropenmedizin und Parasitologie 32, 129–133. [PubMed] [Google Scholar]
- Mehlitz D., Zillmann U. and Scott C. M. (1982). Epidemiological studies on the animal reservoir of Gambiense sleeping sickness. Part III. Characterization of trypanozoon stocks by isoenzymes and sensitivity to human serum. Tropenmedizin und Parasitologie 33, 113–118. [PubMed] [Google Scholar]
- Milner J. D. and Hajduk S. L. (1999). Expression and localization of serum resistance associated protein in Trypanosoma brucei rhodesiense. Molecular and Biochemical Parasitology 104, 271–283. [DOI] [PubMed] [Google Scholar]
- Mimmack M. L., Ryan M., Baba H., Navarro-Ruiz J., Iritani S., Faull R. L. M., McKenna P. J., Jones P. B., Arai H., Starkey M., Emson P. C. and Bahn S. (2002). Gene expression analysis in schizophrenia: reproducible up-regulation of several members of the apolipoprotein L family located in a high-susceptibility locus for schizophrenia on chromosome 22. Proceedings of the National Academy of Sciences USA 99, 4680–4685. doi: 10.1073/pnas.032069099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien T. C., Mackey Z. B., Fetter R. D., Choe Y., O'Donoghue A. J., Zhou M., Craik C. S., Caffrey C. R. and McKerrow J. H. (2008). A parasite cysteine protease is key to host protein degradation and iron acquisition. Journal of Biological Chemistry 283, 28934–28943. doi: 10.1074/jbc.M805824200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odiit M., Coleman P. G., Liu W.-C., McDermott J. J., Fèvre E. M., Welburn S. C. and Woolhouse M. E. J. (2005). Quantifying the level of under-detection of Trypanosoma brucei rhodesiense sleeping sickness cases. Tropical Medicine & International Health 10, 840–849. doi: 10.1111/j.1365-3156.2005.01470.x. [DOI] [PubMed] [Google Scholar]
- Oli M. W., Cotlin L. F., Shiflett A. M. and Hajduk S. L. (2006). Serum resistance-associated protein blocks lysosomal targeting of trypanosome lytic factor in Trypanosoma brucei. Eukaryotic Cell 5(1), 132–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pays E., Lips S., Nolan D., Vanhamme L. and Pérez-Morga D. (2001). The VSG expression sites of Trypanosoma brucei: multipurpose tools for the adaptation of the parasite to mammalian hosts. Molecular and Biochemical Parasitology 114, 1–16. [DOI] [PubMed] [Google Scholar]
- Pays E., Vanhollebeke B., Vanhamme L., Paturiaux-Hanocq F., Nolan D. P. and Pérez-Morga D. (2006). The trypanolytic factor of human serum. Nature Reviews. Microbiology 4, 477–486. doi: 10.1038/nrmicro1428. [DOI] [PubMed] [Google Scholar]
- Radwanska M., Chamekh M., Vanhamme L., Claes F., Magez S., Magnus E., de Baetselier P., Büscher P. and Pays E. (2002). The serum resistance-associated gene as a diagnostic tool for the detection of Trypanosoma brucei rhodesiense. American Journal of Tropical Medicine and Hygiene 67, 684–690. [DOI] [PubMed] [Google Scholar]
- Raper J., Nussenzweig V. and Tomlinson S. (1996). The main lytic factor of Trypanosoma brucei brucei in normal human serum is not high density lipoprotein. Journal of Experimental Medicine 183, 1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raper J., Portela M. P. M., Lugli E., Frevert U. and Tomlinson S. (2001). Trypanosome lytic factors: novel mediators of human innate immunity. Current Opinion in Microbiology 4, 402–408. [DOI] [PubMed] [Google Scholar]
- Rifkin M. R. (1978a). Identification of the trypanocidal factor in normal human serum: high density lipoprotein. Proceedings of the National Academy of Sciences USA 75, 3450–3454. doi: 10.1073/pnas.75.7.3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rifkin M. R. (1978b). Trypanosoma brucei: some properties of the cytotoxic reaction induced by normal human serum. Experimental Parasitology 46, 189–206. [DOI] [PubMed] [Google Scholar]
- Rifkin M. R., De Greef C., Jiwa A., Landsberger F. R. and Shapiro S. Z. (1994). Human serum-sensitive Trypanosoma brucei rhodesiense: a comparison with serologically identical human serum-resistant clones. Molecular and Biochemical Parasitology 66, 211–220. [DOI] [PubMed] [Google Scholar]
- Seed J. R. and Sechelski O. (1990). A survey for a trypanocidal factor in primate sera. Journal of Protozoology 37, 393–400. [DOI] [PubMed] [Google Scholar]
- Simarro P. P., Diarra A., Postigo J. A. R., Franco J. R. and Jannin J. G. (2011). The human African trypanosomiasis control and surveillance programme of the world health organization 2000–2009: the way forward. PLOS Neglected Tropical Diseases 5, . doi: 10.1371/journal.pntd.0001007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiflett A. M., Faulkner S. D., Cotlin L. F., Widener J., Stephens N. and Hajduk S. L. (2007). African Trypanosomes: intracellular trafficking of host defense molecules. Journal of Eukaryotic Microbiology 54, 18–21. [DOI] [PubMed] [Google Scholar]
- Smith E. E. and Malik H. S. (2009). The apolipoprotein L family of programmed cell death and immunity genes rapidly evolved in primates at discrete sites of host-pathogen interactions. Genome Research 19, 850–858. doi: 10.1101/gr.085647.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symula R. E., Beadell J. S. and Sistrom M. (2012). Trypanosoma brucei gambiense group 1 is distinguished by a unique amino acid substitution in the HpHb receptor implicated in human serum resistance. PLOS Neglected Tropical Diseases 6, . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson R., Molina-Portela P., Mott H., Carrington M. and Raper J. (2009). Hydrodynamic gene delivery of baboon trypanosome lytic factor eliminates both animal and human-infective African trypanosomes. Proceedings of the National Academy of Sciences USA 106, 19509–19514. doi: 10.1073/pnas.0905669106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson S., Jansen A. M., Koudinov A., Ghiso J. A., Choi-Miura N. H., Rifkin M. R., Ohtaki S. and Nussenzweig V. (1995). High-density-lipoprotein-independent killing of Trypanosoma brucei by human serum. Molecular and Biochemical Parasitology 70, 131–138. [DOI] [PubMed] [Google Scholar]
- Tzur S., Rosset S., Shemer R., Yudkovsky G., Selig S., Tarekegn A., Bekele E., Bradman N., Wasser W. G., Behar D. M. and Skorecki K. (2010). Missense mutations in the APOL1 gene are highly associated with end stage kidney disease risk previously attributed to the MYH9 gene. Human Genetics 128, 345–350. doi: 10.1007/s00439-010-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzureau P., Uzureau S., Lecordier L., Fontaine F., Tebabi P., Homblé F., Grélard A., Zhendre V., Nolan D. P., Lins L., Crowet J.-M., Pays A., Felu C., Poelvoorde P., Vanhollebeke B., Moestrup S. K., Lyngsø J., Pedersen J. S., Mottram J. C., Dufourc E. J., Pérez-Morga D. and Pays E. (2013). Mechanism of Trypanosoma brucei gambiense resistance to human serum. Nature 501, 430–434. doi: 10.1038/nature12516. [DOI] [PubMed] [Google Scholar]
- Van Meirvenne N., Magnus E. and Janssens P. G. (1976). The effect of normal human serum on trypanosomes of distinct antigenic type (ETat 1 to 12) isolated from a strain of Trypanosoma brucei rhodesiense. Annales de la Societe belge de medecine tropicale 56, 55–63. [PubMed] [Google Scholar]
- Vanhamme L. and Pays E. (2004). The trypanosome lytic factor of human serum and the molecular basis of sleeping sickness. International Journal for Parasitology 34, 887–898. [DOI] [PubMed] [Google Scholar]
- Vanhamme L., Van Den Abbeele J., Paturiaux-Hanocq F., Poelvoorde P., Nolan D. P., Lins L., Pays A., Tebabi P., Van Xong H., Jacquet A., Moguilevsky N., Dieu M., Kane J. P., De Baetselier P., Brasseur R. and Pays E. (2003). Apolipoprotein L-I is the trypanosome lytic factor of human serum. Nature 422, 83–87. doi: 10.1038/nature01461. [DOI] [PubMed] [Google Scholar]
- Vanhollebeke B. and Pays E. (2006). The function of apolipoproteins L. Cellular and Molecular Life Sciences 63, 1937–1944. doi: 10.1007/s00018-006-6091-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhollebeke B. and Pays E. (2010). The trypanolytic factor of human serum: many ways to enter the parasite, a single way to kill. Molecular Microbiology 76, 806–814. doi: 10.1111/j.1365-2958.2010.07156.x. [DOI] [PubMed] [Google Scholar]
- Vanhollebeke B., Nielsen M. J., Watanabe Y., Truc P., Vanhamme L., Nakajima K., Moestrup S. K. and Pays E. (2007). Distinct roles of haptoglobin-related protein and apolipoprotein LI in trypanolysis by human serum. Proceedings of the National Academy of Sciences USA 104, 4118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhollebeke B., De Muylder G., Nielsen M. J., Pays A., Tebabi P., Dieu M., Raes M., Moestrup S. K. and Pays E. (2008). A haptoglobin-hemoglobin receptor conveys innate immunity to Trypanosoma brucei in humans. Science 320, 677–681. doi: 10.1126/science.1156296. [DOI] [PubMed] [Google Scholar]
- Wan G., Zhaorigetu S., Liu Z., Kaini R., Jiang Z. and Hu C. A. A. (2008). Apolipoprotein L1, a novel Bcl-2 homology domain 3-only lipid-binding protein, induces autophagic cell death. Journal of Biological Chemistry 283, 21540–21549. doi: 10.1074/jbc.M800214200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welburn S., Picozzi K., Fevre E., Coleman P., Odiit M., Carrington M. and Maudlin I. (2001). Identification of human-infective trypanosomes in animal reservoir of sleeping sickness in Uganda by means of serum-resistance-associated (SRA) gene. Lancet 358, 2017–2019. [DOI] [PubMed] [Google Scholar]
- Widener J., Nielsen M. J., Shiflett A., Moestrup S. K. and Hajduk S. (2007). Hemoglobin is a co-factor of human trypanosome lytic factor. PLOS Pathogens 3, 1250–1261. doi: 10.1371/journal.ppat.0030129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams T. N., Mwangi T. W., Wambua S., Alexander N. D., Kortok M., Snow R. W. and Marsh K. (2005). Sickle cell trait and the risk of Plasmodium falciparum malaria and other childhood diseases. Journal of Infectious Diseases 192, 178–186. doi: 10.1086/430744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2006). Weekly epidemiological record: relevé épidémiologique hebdomadaire. WHO, Geneva, Switzerland.
- Xong H., Vanhamme L., Chamekh M., Chimfwembe C. E., Van Den Abbeele J., Pays A., Van Meirvenne N., Hamers R., De Baetselier P. and Pays E. (1998). A VSG expression site-associated gene confers resistance to human serum in Trypanosoma rhodesiense. Cell 95, 839–846. [DOI] [PubMed] [Google Scholar]
- Zhaorigetu S., Wan G., Kaini R., Jiang Z. and Hu C. A. A. (2008). ApoL1, a BH3-only lipid-binding protein, induces autophagic cell death. Autophagy 4, 1079–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zillmann U., Mehlitz D. and Sachs R. (1984). Identity of Trypanozoon stocks isolated from man and a domestic dog in Liberia. Tropenmedizin und Parasitologie 35, 105–108. [PubMed] [Google Scholar]