Abstract
Objectives To determine the real world safety of dabigatran or rivaroxaban compared with warfarin in terms of gastrointestinal bleeding.
Design Retrospective cohort study.
Setting Large administrative database of commercially insured people in United States from 1 October 2010 through 31 March 2012.
Participants Enrollees with a prescription of warfarin, dabigatran, or rivaroxaban between 1 October 2010 and 31 March 2012, who were aged 18 years or older, had continuous enrollment and no oral anticoagulant use during the six months before the entry date, with known age and sex, and with no gastrointestinal bleeding for at least six months before the cohort entry date. The final study sample of 46 163 patients included 4907 using dabigatran, 1649 using rivaroxaban, and 39 607 using warfarin.
Main outcome measure Time to gastrointestinal bleeding. Hazard ratios were derived from Cox proportional hazard models with propensity score weighting and robust estimates of errors.
Results Dabigatran users tended to be older (dabigatran v rivaroxaban v warfarin: 62.0 v 57.6 v 57.4 years) and more likely to be male (69% v 49% v 53%). The rate of gastrointestinal bleeding was highest among dabigatran users and lowest among rivaroxaban users (dabigatran v rivaroxaban v warfarin: 9.01 v 3.41 v 7.02 cases per 100 person years). After adjustment for potentially confounding covariates, there was no evidence of a statistically significant difference in the risk of gastrointestinal bleeding between dabigatran and warfarin users (adjusted hazard ratio 1.21, 95% confidence interval 0.96 to 1.53) or between rivaroxaban and warfarin users (0.98, 0.36 to 2.69).
Conclusions Although rates of gastrointestinal bleeding seem to be similar in this commercially insured sample of adults in the United States, we cannot rule out as much as a 50% increase in the risk of gastrointestinal bleeding with dabigatran compared with warfarin or a more than twofold higher risk of bleeding with rivaroxaban compared with warfarin.
Introduction
Anticoagulants are widely prescribed in the United States, the United Kingdom, and around the world for various conditions including atrial fibrillation.1 Dabigatran and rivaroxaban are available as alternatives to warfarin for the prevention of stroke in atrial fibrillation. These drugs offer several advantages over warfarin, including simplified dosing, fewer drug interactions, and no requirement for monitoring. As the pharmacokinetic half life of novel anticoagulants is relatively brief, their pharmacologic effects are transient and disappear within a week.
Clinical trials have established the relative efficacy or non-inferiority of these agents compared with warfarin in selected patients.2 3 For example, in the Randomized Evaluation of Long-Term Anticoagulant Therapy (RE-LY) trial,4 dabigatran administered at a dose of 150 mg was associated with lower rates of stroke and systemic embolism (1.11% v 1.71%; P<0.001) compared with warfarin. In this trial, both drugs had similar rates of major hemorrhage (annual major bleeding risk 3.32% v 3.57% for dabigatran v warfarin; P=0.32). However, the rates of gastrointestinal bleeding were higher with dabigatran. The Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation (ROCKET-AF) trial showed that rivaroxaban at a 10 mg dose was non-inferior to warfarin for the outcome of stroke and systemic embolism.5 As with the RE-LY trial, no differences were seen in rates of major bleeding between warfarin and rivaroxaban in the ROCKET-AF trial, although rates of fatal bleeding were lower in the rivaroxaban arm.
Despite the insights that these trials provide, the real world safety of these novel oral anticoagulants compared with warfarin from limited observational studies is less clear.6 7 8 9 Such safety may diverge from the trial results for several reasons, including trials’ selective inclusion criteria as well as the limited duration of these investigations. Information on findings on gastrointestinal safety will allow clinicians to weigh the risks and benefits of these agents. Gastrointestinal bleeding carries substantial morbidity and mortality. In the United States in 2009, an estimated 140 000 or more hospital admissions had the principal diagnoses of gastrointestinal bleeding and their aggregate costs reached $1.15bn (£0.77bn; €1.06bn).10 The incidence of upper gastrointestinal bleeding in the United Kingdom was 103 cases per 100 000 adults per year.11 Among patients admitted to hospital with acute upper gastrointestinal bleeding in the United Kingdom in 2007, the overall mortality rate was 10%12; among UK patients with atrial fibrillation with warfarin induced gastrointestinal bleeding, 6% of such bleeds are fatal.13
Post-marketing reports have noted reports of major bleeding associated with dabigatran among older patients, those at the extremes of body weight, and those with impaired renal function. Such patients have been largely excluded from the trials.14 Approximately 25% of the bleeding events in post-marketing reports were associated with prescribing and dosing error. Concomitant use of antiplatelet drugs with dabigatran increases the risk of bleeding.15 The proportion of patients taking antiplatelet drugs is higher in the real world, making such patients susceptible to bleeding complications. Furthermore, in contrast to warfarin, no specific antidote for dabigatran exists and it is not dialyzable.
We did a retrospective cohort study using a large administrative claims database of commercially insured people to quantify the comparative safety of these novel anticoagulants relative to warfarin with respect to major gastrointestinal bleeding. We focused on gastrointestinal bleeding because of earlier signals in pivotal clinical trials suggesting an increase in gastrointestinal bleeding with dabigatran relative to warfarin. Additionally, these novel agents have been approved only recently and assessing the efficacy of long term outcomes such as stroke without incurring adequate follow-up would be premature.
Methods
Data
We used the IMS Health LifeLink Health Plan Claims Database. This database contains commercial health plan information from managed care plans and other sources (such as Medicare and Medicaid) throughout the United States, and it is generally representative of the national, commercially insured population in terms of age and sex.16 The database contains claims files and enrollment files. We used the claims files to derive information on inpatient and outpatient diagnoses documented as the ICD-9-CM (international classification of diseases, ninth revision, clinical modification) codes, procedures as the Current Procedural Terminology (CPT-4) codes or the Healthcare Procedural Coding System (HCPCS), prescriptions as National Drug Code (NDC), date of services, and days of the prescription supplied. We used the enrollment files to derive information about patients’ demographic characteristics (including year of birth and sex) and monthly medical/pharmacy enrollment indicators.
Study population
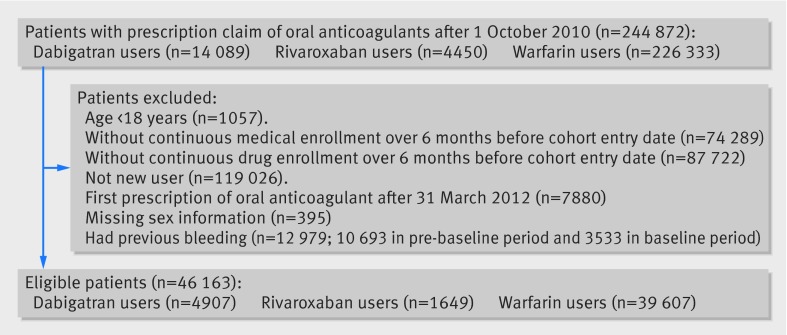
Our study population included 244 872 enrollees with a prescription of warfarin, dabigatran, or rivaroxaban between 1 October 2010 and 31 March 2012. We entered each person into the cohort at the date of his or her first prescription for any of the three study drugs after 1 October 2010. To be eligible for this study, we required people to be aged 18 years or older, have continuous medical and pharmacy enrollment in the six months before the entry date (the baseline period), have none of the three drugs prescribed in the baseline period (new user design), have the first prescription before 31 March 2012, have known age and sex, and not have a previous bleeding event. The final study sample of 46 163 patients included 4907 dabigatran users, 1649 rivaroxaban users, and 39 607 warfarin users (fig 1).
Fig 1 Flow chart of sample size
We defined a patient’s observation ending date as the earliest of five dates. The first of these was the last date of (continuous) exposure to the same drug. The last exposure date was the last day of continuous drug at hand plus 14 days; we used these 14 days to take into account the clearance of the drug. For example, if there was a gap of 14 days or less between two consecutive prescriptions of the same drug, we considered the exposure to be continuous. However, if a patient switched to another drug within the 14 day period of the previous exposure, we considered the day before the start of the second drug to be the last exposure date. The second date was the date of the loss of medical or pharmacy enrollment. The third was the end date of the study, which was 31 March 2012. The fourth was the date before the first date of hospital admission not related to gastrointestinal bleeding, because we did not have prescription information during hospital admission. The last date was the first date of gastrointestinal bleeding. If gastrointestinal bleeding occurred during hospital admission, we used the first date of admission as the bleeding date for patients admitted for gastrointestinal bleeding. We censored a patient if the observation ending date was not equal to the first bleeding date.
Outcome and independent variables
Our independent variable of interest was the type of drug exposure: warfarin, dabigatran, or rivaroxaban. We used control variables including demographics (age groups, sex, and region), three binary clinical conditions (having any diagnosis of renal failure, trauma, or Helicobacter pylori infection), three binary drug indicators (having any prescription of non-steroidal anti-inflammatory drugs, proton pump inhibitor, or steroid), and six levels of counts of Clinical Classification Software (CCS). The CCS is a tool, developed by the Agency for Healthcare Research and Quality, for clustering patients’ diagnoses and procedures into a manageable number of clinically meaningful categories17; the higher the CCS score, the higher the comorbidity. All variables were derived from claims data in the baseline period. We incorporated propensity scores into the models as a means of weighting the observations to account for potential confounding by the variables above. Our outcome of interest was gastrointestinal bleeding, which we identified using ICD-9 codes and CPT codes validated in a recent study (web appendix 1).18
Propensity score
To control for the differences in patients’ characteristics across warfarin, dabigatran, and rivaroxaban users, we developed two propensity scores: one to predict whether a person used dabigatran relative to warfarin among dabigatran and warfarin users (n=44 514) and another to predict use of rivaroxaban relative to warfarin among rivaroxaban and warfarin users (n=41 256). To develop these propensity scores, we included the aforementioned control variables; the only exception was that we entered CCS into the propensity score model as 285 mutually exclusive binary indicators.
Various methods have been proposed to apply propensity scores, including matching, inverse probability of treatment weighting, stratification, and regression covariates; each has its own advantages and disadvantages, and no single method consistently outperforms other approaches.19 20 21 We used propensity score weighting because we did not want to lose the observations of treated patients (compared with matching) and we wanted one interpretable overall treatment effect (compared with stratification). We applied the average treatment effect of the treated weighting because this allows us to estimate the average effect of treatment on patients who received the treatment; that is, we compared the hazards of gastrointestinal bleeding among dabigatran or rivaroxaban users with the hypothesized situation had they taken warfarin instead of the oral anticoagulant. This is particularly useful when the study sample is likely to differ systematically from the overall population.19 We compared the balance in baseline covariates before and after weighting by using the standardized difference; we considered a standardized difference less than 0.1 to be a negligible difference between treatment groups.19 After we applied average treatment effect of the treated weighting, standardized differences of all available covariates between dabigatran and warfarin users and between rivaroxaban and warfarin users were reduced to 0.05 or smaller, suggesting that the groups were well balanced (appendix 2).
Statistical analysis
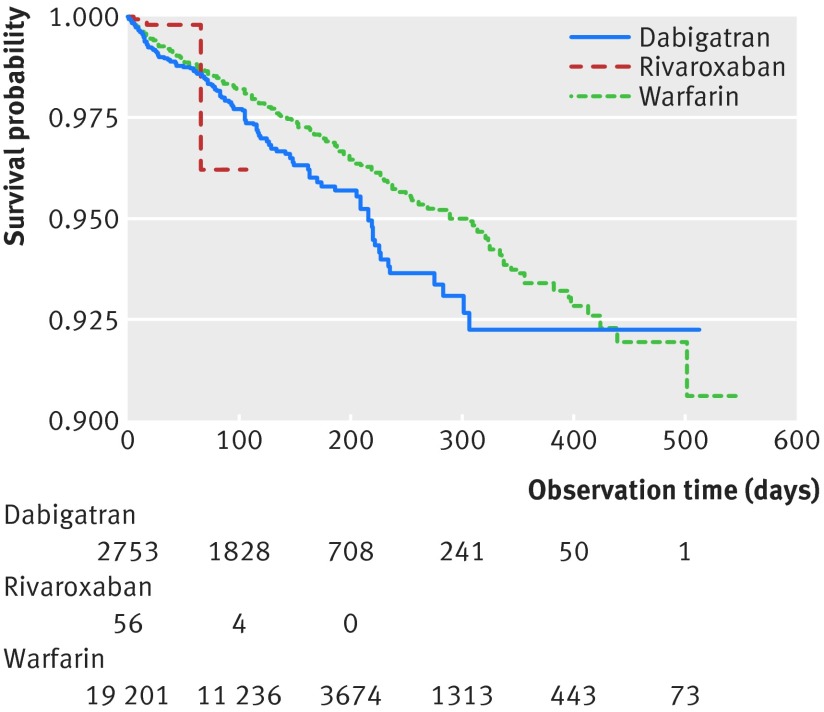
We used χ2 tests and analysis of variance/Kruskal-Wallis tests to examine whether patients’ characteristics were different across the three groups of drug users. We present Kaplan-Meier survival curves of having gastrointestinal bleeding stratified by the three different drug groups (fig 2). We created two separate Cox proportional hazard models with propensity score average treatment effect of the treated weighting to examine the association between anticoagulant exposure (“dabigatran v warfarin” and “rivaroxaban v warfarin”) and gastrointestinal bleeding, and we calculated robust estimates of standard errors for all variables in the model.22 Control variables could enter the model as either regression covariates or stratification factors; if a variable violated the proportional hazard assumption, this variable would enter the model as a stratification factor. We started with all control variables as regression covariates and examined whether the proportional hazard assumption was violated for any control variable at the P=0.1 level (Kolmogorov-type supremum test).23 Across two models, three variables reached that level—age groups, CCS categories, and having any use of non-steroidal anti-inflammatory drug in the baseline period; these were later included in the model as stratification factors. We re-checked the proportional hazard assumption and found that it was not violated with all remaining variables (P≥0.1). We also did a post hoc analysis stratifying our results for patients above and below the age of 65 years, using the same model as for the total sample. We used SAS version 9.2 for all analyses.
Fig 2 Survival function and number of patients at risk over time by drug use
Sensitivity analyses
We used several sensitivity analyses to examine whether our findings were robust. Firstly, we evaluated two additional models: one including all variables as regression covariates and another including all variables as stratification factors. Secondly, we varied the length of washout period from seven to 30 to 45 days to check the robustness of our results. Thirdly, we censored all inpatient records owing to the lack of the prescription information during hospital admission, as we wanted to examine whether such exclusion would affect our findings. Finally, we additionally included the HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly, drugs/alcohol concomitantly) bleeding risk score in the model to control for a patient’s risk of bleeding and examine whether our results would change.24 25 26 Given that we did not have laboratory data, we excluded the labile international normalized ratio from construction of this risk score.
Results
Among 46 163 patients included in the study, about 85.8% were warfarin users; fewer used dabigatran (10.6%) or rivaroxaban (3.6%) (table 1). Dabigatran users were the oldest (dabigatran v rivaroxaban v warfarin: 62.0 v 57.6 v 57.4 years) and most likely to be male (69% v 49% v 53%). Overall, the CCS score was lower in dabigatran and rivaroxaban users than in warfarin users (dabigatran v rivaroxaban v warfarin: 11.3 v 12.3 v 13.5). The number of cases of gastrointestinal bleeding among dabigatran users was 122 compared with only four among rivaroxaban users. The rate of gastrointestinal bleeding was highest among dabigatran users and lowest among rivaroxaban users (dabigatran v rivaroxaban v warfarin: 9.01 v 3.41 v 7.02 per 100 person years).
Table 1.
Characteristics of study sample. Values are percentages (numbers) unless stated otherwise
| Dabigatran (n=4907) | Rivaroxaban (n=1649) | Warfarin (n=39 607) | Total (n=46 163) | |
|---|---|---|---|---|
| Patients’ characteristics | ||||
| Mean (SD) age, years | 62.0 (12.0) | 57.6 (9.8) | 57.4 (13.5) | 57.6 (13.3) |
| Age group*: | ||||
| 18-44 | 6.0 (295) | 8.1 (133) | 14.9 (5909) | 13.7 (6337) |
| 45-64 | 16.9 (827) | 25.5 (420) | 22.6 (8962) | 22.1 (10 209) |
| 55-64 | 44.4 (2178) | 49.0 (808) | 40.1 (15 867) | 40.8 (18 853) |
| ≥65 | 32.8 (1607) | 17.5 (288) | 22.4 (8869) | 23.3 (10 764) |
| Female sex* | 30.9 (1514) | 51.5 (849) | 46.9 (18 568) | 45.3 (20 931) |
| Region*: | ||||
| East | 10.5 (515) | 3.9 (65) | 11.1 (4391) | 10.8 (4971) |
| Mid-West | 29.6 (1450) | 33.7 (555) | 37.0 (14 648) | 36.1 (16 653) |
| South | 49.5 (2431) | 55.4 (913) | 40.4 (15 982) | 41.9 (19 326) |
| West | 10.4 (511) | 7.0 (116) | 11.6 (4586) | 11.3 (5213) |
| Clinical/medication indicators from baseline period | ||||
| Renal failure* | 4.2 (207) | 2.1 (34) | 5.1 (2004) | 4.9 (2245) |
| Trauma* | 13.3 (653) | 27.7 (457) | 23.3 (9240) | 22.4 (10 350) |
| Helicobacter pylori infection | 0.2 (11) | 0.2 (3) | 0.1 (54) | 0.2 (68) |
| Mean (SD) CCS score | 11.3 (6.9) | 12.3 (5.6) | 13.5 (8.5) | 13.2 (8.2) |
| CCS category*: | ||||
| ≤5 | 18.60 (912) | 8.3 (136) | 14.9 (5917) | 15.1 (6965) |
| 6-10 | 33.5 (1642) | 30.2 (498) | 25.6 (10 147) | 26.6 (12 287) |
| 11-15 | 25.5 (1253) | 37.1 (612) | 25.8 (10 218) | 26.2 (12 083) |
| 16-20 | 13.0 (640) | 16.3 (268) | 16.5 (6532) | 16.1 (7440) |
| 21-25 | 5.2 (254) | 6.3 (103) | 8.4 (3332) | 8.0 (3689) |
| ≥26 | 4.2 (206) | 1.9 (32) | 8.7 (3461) | 8.0 (3699) |
| NSAID use* | 15.6 (764) | 43.7 (721) | 23.9 (9475) | 23.7 (10 960) |
| PPI use | 18.7 (916) | 19.2 (316) | 19.5 (7734) | 19.4 (8966) |
| Steroid use* | 12.5 (615) | 12.7 (209) | 15.3 (6074) | 14.9 (6898) |
| Outcome | ||||
| No with gastrointestinal bleeding* | 122 | 4 | 632 | 758 |
| Total person years | 1354.0 | 117.4 | 9007.1 | 10 478.5 |
| Rate of gastrointestinal bleeding (per 100 person years) | 9.01 | 3.41 | 7.02 | 7.23 |
| Median (IQR) observation time, days* | 70 (45-133) | 25 (18-30) | 47 (35-105) | 45 (33-105) |
Source: IMS Health LifeLink® Health Plan Claims Database, 2010-12.
CCS=Clinical Classification Software; NSAID=non-steroidal anti-inflammatory drug; PPI=proton pump inhibitor.
*P≤0.01.
Table 2 shows the unadjusted and adjusted results of the average treatment effect of the treated for the total sample and for patients under and over 65 years of age. Appendix 3 shows the results of the full model for the total sample.
Table 2.
Multivariable association between novel oral anticoagulant use and gastrointestinal bleeding
| Analysis | Dabigatran (reference group: warfarin) | Rivaroxaban (reference group: warfarin) |
|---|---|---|
| All patients: | (n=44 514) | (n=41 256) |
| Crude hazard ratio* (95% CI) | 1.20 (0.96 to 1.52) | 0.95 (0.31 to 2.94) |
| Adjusted hazard ratio† (95% CI) | 1.21 (0.96 to 1.53) | 0.98 (0.36 to 2.69) |
| Patients aged under 65 years: | (n=34 038) | (n=32 099) |
| Crude hazard ratio* (95% CI) | 1.33 (0.98 to 1.80) | 1.08 (0.27 to 4.41) |
| Adjusted hazard ratio† (95% CI) | 1.34 (0.98 to 1.83) | 1.03 (0.33 to 3.18) |
| Patients aged over 65 years: | (n=10 476) | (n=9157) |
| Crude hazard ratio* (95% CI) | 1.07 (0.75 to 1.52) | 0.69 (0.10 to 4.68) |
| Adjusted hazard ratio† (95% CI) | 1.07 (0.75 to 1.53) | 0.62 (0.18 to 2.08) |
Source: IMS Health LifeLink® Health Plan Claims Database, 2010-12.
*No control variables.
†Age groups, Clinical Classification Software categories, and non-steroidal anti-inflammatory drug use as stratification factors and others as regression covariates.
Without adjusting for any covariate, we found no statistically significant difference between dabigatran and warfarin in the risk of gastrointestinal bleeding; the crude hazard ratio was 1.20 (95% confidence interval 0.96 to 1.52). After adjustment for age groups, CCS categories, and non-steroidal anti-inflammatory drug use as stratification factors and for sex, regions, three binary clinical conditions (having any diagnosis of renal failure, trauma, or Helicobacter pylori infection), and two binary medication indicators (having any prescription of proton pump inhibitor or steroid) as regression covariates, the adjusted hazard ratio was 1.21 (0. 96 to 1.53).
Without adjusting for any covariate, we found no statistically significant difference between rivaroxaban and warfarin in the risk of gastrointestinal bleeding; the crude hazard ratio was 0.95 (0.31 to 2.94). After adjustment for age groups, CCS categories, and non-steroidal anti-inflammatory drug use as stratification factors and all other confounders as regression covariates, the adjusted hazard ratio was 0.98 (0.36 to 2.69).
Appendix 4 shows the sensitivity analyses with different covariate inclusion methods, and appendix 5 shows those with three different washout periods for warfarin users. Appendix 6 shows the results with censoring of inpatient gastrointestinal bleeding, and appendix 7 shows those including HAS-BLED risk score. Results from these sensitivity analyses were very similar, suggesting that our findings were robust.
We found no statistically significant differences (at the P=0.05 level) in the adjusted hazard ratios comparing dabigatran or rivaroxaban users with warfarin users among patients under or over the age of 65. However, when we compared dabigatran and warfarin users under 65, the adjusted hazard ratio was borderline significant (P<0.1) (adjusted hazard ratio 1.33, 0.98 to 1.83), suggesting a potentially increased risk associated with dabigatran.
Discussion
In this analysis of novel oral anticoagulant use among commercially insured people in the United States, neither dabigatran nor rivaroxaban was associated with a statistically significantly increased risk of gastrointestinal bleeding relative to warfarin. These findings are important given the global burden of thromboembolic disease, as well as the recent development of several novel oral anticoagulants of which the real world safety and effectiveness relative to warfarin remain unclear.
Comparison with previous studies
Our inability to detect a statistically significant difference in gastrointestinal bleeding between dabigatran and warfarin is noteworthy, given that several studies examining this outcome have identified such an association. For example, a meta-analysis of clinical trials reported a statistically significant increased risk of gastrointestinal bleeding with novel anticoagulants, with a relative risk of 1.45 (95% confidence interval 1.07 to 1.97). The odds ratio for dabigatran was 1.58 (1.29 to 1.93), and that for rivaroxaban was 1.48 (1.21 to 1.82).27 A recent study focusing on older US Medicare patients with non-valvular atrial fibrillation reported an increase in gastrointestinal bleeding with dabigatran compared with warfarin (hazard ratio 1.28, 1.14 to 1.44).28 These differences may be due to differences in the study populations; our study participants were relatively younger compared with the Medicare cohort. The excess hazard of dabigatran, relative to warfarin, may be age dependent and concentrated among very elderly people, a population that was not well represented in this sample of commercially insured patients. In contrast, our analysis showed that the risk of bleeding with dabigatran relative to warfarin was higher among patients under 65, although this was not significant (adjusted hazard ratio 1.33, 0.98 to 1.80). Major gastrointestinal bleeding events were statistically significantly higher with the 150 mg dose of dabigatran compared with warfarin in the RE-LY trial (relative risk 1.30, 1.08 to 1.56).29 However, the population was older than that in our study. Another small hospital based study reported no difference in the risk of gastrointestinal bleeding among dabigatran compared with rivaroxaban users (5.3% v 4.8%; P=0.82).9 Another database study reported no difference in the rates of gastrointestinal bleeding between rivaroxaban and warfarin users among patients with non-valvular atrial fibrillation.6
Other observational studies have similarly reported either very low rates of gastrointestinal bleeding or no difference in rates between warfarin and dabigatran in several European cohorts.7 8 However, these studies had several drawbacks including limited efforts in ensuring baseline balance across different exposure groups (propensity score matching based on up to three simple variables, or none26); not adopting a new user design so that previous exposure might affect the observed outcomes; focusing on prevalent instead of incident outcomes; basing the classification of exposure group on the first eligible claims; and not requiring continuous exposure. The different results observed from clinical trials and observational studies likely reflect differences in populations enrolled in these studies and the selection of participants to receive these drugs. It is important to note here that several of these European cohort studies reporting no difference in bleeding included the lower 110 mg dose of dabigatran, which is widely used in other countries. The US Food and Drug Administration has not allowed the use of 110 mg dabigatran in the United States, so our study did not include such users. A recent analysis of documents suggested that the plasma concentrations of the drug vary substantially across users. This variability in blood concentrations could also be associated with differences in rates of adverse effects such as gastrointestinal bleeding.30 31
Our results showing no evidence of a difference in the risk of gastrointestinal bleeding with rivaroxaban compared with warfarin are similar to a recent observational from the United Stated that reported no statistically significant difference in real world rates of bleeding between rivaroxaban and warfarin in patients with non-valvular atrial fibrillation (hazard ratio 1.06, 0.71 to 1.64).6
Strengths and weaknesses of study
Our study has several strengths. Firstly, we adopted a new user design, which allowed us to eliminate the residual effect of the previous exposure. Secondly, we focused on the incident cases to remove the effect of prevalent gastrointestinal bleeding, an important risk factor for subsequent bleeding. Thirdly, we used a validated algorithm to identify gastrointestinal bleeding cases. Fourthly, we included a wide range of potential confounders identified from the literature in constructing propensity scores. Fifthly, baseline balance between different exposure groups was achieved through the propensity score weighting and evaluated through the standardized difference to minimize confounding. Sixthly, we did several sensitivity analyses to evaluate the robustness of our results, including varying length of exposure washout periods and different methods of applying propensity scores.
Our study also has some limitations. Firstly, we did not have access to information about patients’ mortality or about laboratory tests such as prothrombin times. Secondly, we assumed that prescription fill data reflect actual patient usage. Thirdly, our inability to detect a significant difference between dabigatran and warfarin may have been a result of a low number of events resulting in inadequate statistical power. Fourthly, our outcome of interest, gastrointestinal bleeding, may not have been fully captured by the algorithm. However, we used an approach that has been validated with reasonable accuracy in a previous study.18 Fifthly, this study might underestimate bleeding associated with novel agents, as patients are more likely to report and seek treatment for bleeding associated with these agents than for warfarin. Sixthly, the short observation time might not allow us to explore other important long term bleeding effects. In addition, the length of observation was different across the three drug user groups, with the shortest observation period for rivaroxaban users. Seventhly, we have limited clinical information on patients excluded from the cohort. The generalizability of these findings to European cohorts and those taking lower doses of dabigatran 110 mg is unknown. Eighthly, the average treatment effect of the treated weighting results in effect estimates standardized to different populations (rivaroxaban users or dabigatran users). Given the substantial differences between the two groups, the effect estimates could not be directly compared. Finally, our findings may be subject to unmeasured confounding. For example, it is particularly difficult to capture aspirin, which is obtained over the counter and a significant risk factor for gastrointestinal bleeding. Selection bias whereby health professionals may have channeled patients at risk of gastrointestinal bleeding to one class of agents is always possible.
Priorities for future research
Our findings raise questions and opportunities for further investigation. For example, future studies should consider other designs, such as the self controlled case series, to control for time invariant, within person confounding.32 Such studies should also evaluate additional outcomes such as overall bleeding and benefits such as reduction in thromboembolic stroke. Another novel anticoagulant—apixaban—is now available and should also be evaluated as a comparator in future studies. In addition, given evidence suggesting variations in the risk of gastrointestinal hemorrhage with age, studies with adequate samples of older people are important to evaluate this association further. Finally, most of our study patients exited the cohort owing to loss of continuous drug exposure (46% for dabigatran users, and about 60% for rivaroxaban and warfarin users; see appendix 8). Many factors may contribute to this phenomenon, including the short length of washout period (for example, if the length was expanded to 45 days, the proportion would reduce to 27% for dabigatran users and about 40% for others), patients’ unwillingness to fill the prescription (due to side effects, costs, or other concerns), or information not recorded on claims data (patients might have obtained the drug but it was not recorded on claims—for example, by obtaining samples or paying cash). In a Chinese atrial fibrillation patient cohort prescribed dabigatran (n=467), 22% permanently discontinued dabigatran; the most common reason for discontinuation was dyspepsia (31%), followed by other adverse events (18%), such as minor bleeding (9%), major gastrointestinal bleeding (8%), and intracranial hemorrhage (1%); cost concerns accounted for 1%.33 Better understanding of the reasons behind discontinuation may help to increase patients’ adherence rates and help patients to increase the quality of medical care they receive.
Implications and conclusions
Our findings have clinical and policy implications. In the light of other studies that suggest an increased risk of gastrointestinal bleeding associated with dabigatran, our findings show a null effect in a relatively younger insured population. However, these findings are not inconsistent with previous studies and do not rule out a greater than 50% increased risk with dabigatran and more than twofold increased risk with rivaroxaban. Pharmacy benefit managers, insurers, and guideline makers may also use this information to make evidence based decisions about the group of patients who are eligible for therapy.
In this commercially insured database of adults in the United States, neither dabigatran nor rivaroxaban use was associated with a statistically significantly increased risk of gastrointestinal bleeding relative to warfarin. Evidence from observational studies such as ours should prove useful to clinicians in selecting the appropriate anticoagulant for patients after incorporating other information about the safety, efficacy, and effectiveness of these agents, as well as their cost and patients’ preferences regarding anticoagulant therapy.
What is already known on this topic
Most evidence on the increased risk of gastrointestinal bleeding for novel oral anticoagulants compared with warfarin comes from clinical trials providing limited duration of follow-up and selective inclusion criteria
Observational studies have been inconsistent on the association with gastrointestinal bleeding of dabigatran compared with warfarin
What this study adds
A 50% increase in the risk of gastrointestinal bleeding associated with dabigatran compared with warfarin cannot be ruled out
A more than twofold increased risk of bleeding with rivaroxaban compared with warfarin cannot be ruled out
The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from the following IMS Health Incorporated information service(s): IMS Health LifeLink LRx Database (2007-13), IMS Health Incorporated. All rights reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its affiliated or subsidiary entities.
Contributors: HC designed the study, managed data, did analyses, and drafted the manuscript. MZ managed data and drafted the manuscript. WT did analyses and drafted the manuscript. GCA provided critical comments and revised the manuscript. SS designed the study, secured data, and drafted the manuscript. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved of the final manuscript. HC and SS are the guarantors.
Funding: GCA is supported by the National Heart, Lung and Blood Institute (R01 HL107345). The funding source had no role in the design and conduct of the study, the analysis or interpretation of the data, or the preparation or final approval of the manuscript before publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: GCA is supported by the National Heart, Lung and Blood Institute (R01 HL107345); GCA is chair of the FDA’s Peripheral and Central Nervous System Advisory Committee, serves as a paid consultant to IMS Health, and serves on an IMS Health scientific advisory board; this arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The data source included de-identified information, and this project was deemed not to be human subjects research by the institutional review board of the Johns Hopkins Bloomberg School of Public Health; ethics review board approval for such studies is not required.
Data sharing: No additional data available.
Transparency: HC and SS affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Cite this as: BMJ 2015;350:h1585
Web Extra. Extra material supplied by the author
References
- 1.Kirley K, Qato DM, Kornfield R, et al. National trends in oral anticoagulant use in the United States, 2007 to 2011. Circ Cardiovasc Qual Outcomes 2012;5:615-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boehringer Ingelheim Pharmaceuticals. Pradaxa [package insert]. 2011.
- 3.Janssen Pharmaceuticals. Xarelto [package insert]. 2011.
- 4.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139-51. [DOI] [PubMed] [Google Scholar]
- 5.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 2011;365:883-91. [DOI] [PubMed] [Google Scholar]
- 6.Laliberte F, Cloutier M, Nelson WW, et al. Real-world comparative effectiveness and safety of rivaroxaban and warfarin in nonvalvular atrial fibrillation patients. Curr Med Res Opin 2014;30:1317-25. [DOI] [PubMed] [Google Scholar]
- 7.Larsen TB, Gorst-Rasmussen A, Rasmussen LH, et al. Bleeding events among new starters and switchers to dabigatran compared with warfarin in atrial fibrillation. Am J Med 2014;127:650-6. [DOI] [PubMed] [Google Scholar]
- 8.Sorensen R, Gislason G, Torp-Pedersen C, et al. Dabigatran use in Danish atrial fibrillation patients in 2011: a nationwide study. BMJ Open 2013;3:e002758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sherid M, Sifuentes H, Sulaiman S, et al. Risk of gastrointestinal bleeding with dabigatran: a head-to-head comparative study with rivaroxaban. Digestion 2014;90:137-46. [DOI] [PubMed] [Google Scholar]
- 10.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143:1179-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hopper AD, Sanders DS. Upper GI bleeding requires prompt investigation. Practitioner 2011;255:15-9. [PubMed] [Google Scholar]
- 12.Hearnshaw SA, Logan RF, Lowe D, et al. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut 2011;60:1327-35. [DOI] [PubMed] [Google Scholar]
- 13.Gallagher AM, van Staa TP, Murray-Thomas T, et al. Population-based cohort study of warfarin-treated patients with atrial fibrillation: incidence of cardiovascular and bleeding outcomes. BMJ Open 2014;4:e003839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harper P, Young L, Merriman E. Bleeding risk with dabigatran in the frail elderly. N Engl J Med 2012;366:864-6. [DOI] [PubMed] [Google Scholar]
- 15.Desai J, Kolb JM, Weitz JI, et al. Gastrointestinal bleeding with the new oral anticoagulants—defining the issues and the management strategies. Thromb Haemost 2013;110:205-12. [DOI] [PubMed] [Google Scholar]
- 16.IMS Health Incorporated or its affiliates. LifeLink® Health Plan claims data user guide & data dictionary. 2012.http://tri.uams.edu/wp-content/uploads/2011/10/LifeLink-Health-Plan-Claims-Data-Dictionary-June-2012.pdf.
- 17.Cowen ME, Dusseau DJ, Toth BG, et al. Casemix adjustment of managed care claims data using the clinical classification for health policy research method. Med Care 1998;36:1108-13. [DOI] [PubMed] [Google Scholar]
- 18.Abraham NS, Hartman C, Richardson P, et al. Risk of lower and upper gastrointestinal bleeding, transfusions, and hospitalizations with complex antithrombotic therapy in elderly patients. Circulation 2013;128:1869-77. [DOI] [PubMed] [Google Scholar]
- 19.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Methods 2010;15:234-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurth T, Walker AM, Glynn RJ, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol 2006;163:262-70. [DOI] [PubMed] [Google Scholar]
- 22.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Stat Assoc 1989;84:1074-8. [Google Scholar]
- 23.Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika 1993;80:557-72. [Google Scholar]
- 24.Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010;138:1093-100. [DOI] [PubMed] [Google Scholar]
- 25.Deitelzweig SB, Pinsky B, Buysman E, et al. Bleeding as an outcome among patients with nonvalvular atrial fibrillation in a large managed care population. Clin Ther 2013;35:1536-45. [DOI] [PubMed] [Google Scholar]
- 26.Hippisley-Cox J, Coupland C. Predicting risk of upper gastrointestinal bleed and intracranial bleed with anticoagulants: cohort study to derive and validate the QBleed scores. BMJ 2014;349:g4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holster IL, Valkhoff VE, Kuipers EJ, et al. New oral anticoagulants increase risk for gastrointestinal bleeding: a systematic review and meta-analysis. Gastroenterology 2013;145:105-12. [DOI] [PubMed] [Google Scholar]
- 28.Graham DJ, Reichman ME, Wernecke M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for non-valvular atrial fibrillation. Circulation 2015;131:157-64. [DOI] [PubMed] [Google Scholar]
- 29.Bytzer P, Connolly SJ, Yang S, et al. Analysis of upper gastrointestinal adverse events among patients given dabigatran in the RE-LY trial. Clin Gastroenterol Hepatol 2013;11:246-52. [DOI] [PubMed] [Google Scholar]
- 30.Moore TJ, Cohen MR, Mattison DR. Dabigatran, bleeding, and the regulators. BMJ 2014;349:g4517. [DOI] [PubMed] [Google Scholar]
- 31.Cohen D. Dabigatran: how the drug company withheld important analyses. BMJ 2014;349:g4670. [DOI] [PubMed] [Google Scholar]
- 32.Maclure M, Fireman B, Nelson JC, et al. When should case-only designs be used for safety monitoring of medical products? Pharmacoepidemiol Drug Saf 2012;21(suppl 1):50-61. [DOI] [PubMed] [Google Scholar]
- 33.Ho MH, Ho CW, Cheung E, et al. Continuation of dabigatran therapy in “real-world” practice in Hong Kong. PLoS One 2014;9:e101245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.