Abstract
Background
Migrants from Eastern Europe constitute more than 5% of Germany's population. Since population health in their countries of origin is poor their health status upon arrival may be worse than that of the native-born German population (hypothesis H1). As a minority, they may be socio-economically disadvantaged (H2), and their health status may deteriorate quickly (H3).
Methods
We compared data from 1995 and 2000 for immigrants from Eastern Europe (n = 353) and a random sample of age-matched Germans (n = 2, 824) from the German Socioeconomic Panel. We tested H1-3 using health satisfaction, as a proxy for health status, and socioeconomic indicators. We compared changes over time within groups, and between immigrants and Germans. We assessed effects of socio-economic status and being a migrant on declining health satisfaction in a regression model.
Results
In 1995, immigrants under 55 years had a significantly higher health satisfaction than Germans. Above age 54, health satisfaction did not differ. By 2000, immigrants' health satisfaction had declined to German levels. Whereas in 1995 immigrants had a significantly lower SES, differences five years later had declined. In the regression model, immigrant status was much stronger associated with declining health satisfaction than low SES.
Conclusion
In contrast to H1, younger immigrants had an initial health advantage. Immigrants were initially socio-economically disadvantaged (H2), but their SES improved over time. The decrease in health satisfaction was much steeper in immigrants and this was not associated with differences in SES (H3). Immigrants from Eastern Europe have a high risk of deteriorating health, in spite of socio-economic improvements.
Background
The breakdown of the "Iron Curtain" at the end of the 1980s and the opening of borders between Eastern and Western Europe marked the beginning of a large migration process affecting Europe as a whole. In the 1990s, an average of about 600,000 people migrated annually from the former Communist states to Western Europe [1]. Germany was one of the main countries of destination. Between 1989 and 2002, almost 2.9 million persons of ethnic German origin, so called "Aussiedler" (resettlers), mainly from the former Soviet Union, Poland and Romania, arrived in the country[2]. In addition, 1.7 million people with a citizenship of an Eastern European country reside in Germany. Together, these two groups today constitute more than 5% of Germany's population[3].
Thus far, hardly any data on the health status of these immigrants are available. However, it might differ from that of the native German population due to two influencing factors. Firstly, population health status in the immigrants' countries of origin is worse than in Germany. Since the 1970s, the gap in mortality rates between Eastern and Western Europe has steadily widened, with an additional worsening during and after the transition period[4]. Today, Eastern Europe and especially the states of the former Soviet Union report some of the highest mortality rates worldwide, with a large number of premature deaths due to cardiovascular and other chronic diseases as well as external causes[5,6]. The reasons for this dramatic development are not fully understood, but it is assumed that a broad range of behavioural, environmental and societal risk factors contribute[4]. Not only objective health indicators differ; the perceived health status in Eastern Europe is also on average 25% lower than in Western Europe[7]. Since immigrants were exposed to the described poor health conditions before leaving their respective countries of origin, it can be hypothesised that their health status upon arrival in Germany is worse than that of native Germans of the same age and sex (hypothesis H1). This hypothesis is based on an explanatory model for the health of migrants which focuses not merely on selection effects at the time of migration, but also on differences in the progression of the health transition between countries of origin and host countries[8]. The model contrasts with the frequently postulated "healthy migrant effect", which explains an initially better health status in immigrants through selective migration of healthy people[8,9]. An explanation only based on selective migration, however, disregards the health status of the immigrants' population of origin which might have a strong effect on health status after migration[8]. A second major factor influencing health is the socioeconomic status (SES). It is well established that there is an inverse association between SES and health status; the underlying pathways are only partly understood[10,11]. As a minority, immigrants from Eastern Europe might be socio-economically disadvantaged relative to the native German population (hypothesis H2). Given the combination of low SES and poor health and risk factor profile, such as a high prevalence of smoking or hypercholesterolemia, which will result in the onset of disease years after exposure[12,13], the immigrants' health status might rapidly deteriorate in the years after migration (hypothesis H3). Stress during migration and adaptation are other possible contributors to a deterioration.
The aim of the present study was to test the hypotheses H1-3 on longitudinal changes of the SES and the health status among immigrants from Eastern Europe, relative to those of the native-born German population.
Methods
Data source and comparison groups
The analysis uses data from the German Socio-Economic Panel (GSOEP)[14], a longitudinal survey of currently about 12,000 households in Germany which started in 1984. Every year, household members above 16 years are asked questions on a broad range of socio-economic, and also some health-related, indicators. In addition, heads of households are asked about the situation of the whole household (e.g. size of housing). Since 1994/95, the panel includes households whose head had immigrated to Germany from Eastern Europe after 1984. The representativeness for German households and the longitudinal stability of the sample have been confirmed in several studies [14-16].
The two comparison groups, referred to as "immigrants" and "native Germans", were defined as follows. In a first step, GSOEP participants were selected who were aged 16 to 74 years in 1995 and stated either an Eastern European country or Germany as their country of origin. Selection was done on an individual basis independently from the origin of the household head, e.g. a person of Eastern European origin living in a household with a German head was categorised as immigrant and vice versa. Since the aim of the study was to observe changes over time, only persons who participated in both the 1995 and 2000 surveys and answered the question on health satisfaction were included. For each immigrant, eight native Germans of the same age and sex were randomly selected to avoid residual confounding by age after stratification into three age bands (16–34, 35–54 and 55–74 years in 1995). Drop-out rates (participants who could not be followed up in 2000 divided by participants who met the inclusion criteria in 1995) by age, were 42.5%, 36.3%, and 38.2% for immigrants and 42.4%, 27.9% and 31.9% for native Germans.
Variables
To test H1 and H3, information on self-rated health, expressed as health satisfaction, was used. The corresponding question in the GSOEP is: "How satisfied are you with your health?". It is measured on a scale from 0 ("not at all satisfied") to 10 ("completely satisfied"). Although this is a subjective health indicator, numerous studies including one using GSOEP data have shown measures of self-rated and self-perceived health to correlate well with objective outcomes such as mortality [17-19], to be reliable[20] and to be valid in different ethnic groups[21].
To test H2, SES was assessed in 1995 and 2000 based on income, size of housing, welfare dependency and unemployment. A standardised per capita income was calculated by dividing total household income by the number of household members to the power of 0.73 (equivalence scale)[22]. The size of housing was calculated by dividing the total available living space by the number of household members. Welfare dependency, which refers to the question if any household member was dependent on welfare, and unemployment are dichotomous variables. In order to better reflect relative socio-economic deprivation, the continuous variables income and size of housing were also dichotomised; participants were regarded as socioeconomically disadvantaged if the respective value was in the lowest quartile. The cut-off values for income were 1,300 German Marks in 1995 and 1,526.67 German Marks in 2000; the cut-off values for size of housing were 22 and 25 square meters, respectively. To account for a potential loss of power, income and size of housing in the respective years were also compared as continuous variables with a non-parametric Wilcoxon test.
Statistical methods
Health satisfaction of immigrants in 1995 (the earliest year data was available) was compared to that of native Germans using a t-test for unpaired observations (H1). The odds of socioeconomic disadvantage among immigrants, relative to those of native Germans, were estimated by calculating prevalence odds ratios for the four socioeconomic variables (H2). The comparison of the odds ratios for 1995 and 2000 allows to assess longitudinal changes in the immigrants' odds of being socioeconomically disadvantaged.
H3 was tested in two different ways. Firstly, in a cross-sectional analysis, health satisfaction among immigrants and native Germans was also compared in 2000. Secondly, in a longitudinal analysis, changes in health satisfaction between 1995 and 2000 within groups were assessed using a t-test for paired observations.
To assess the effect of socioeconomic factors on health satisfaction, logistic regression modelling was used. The outcome was defined as a decline in health satisfaction by at least two points between 1995 and 2000. This corresponds to the highest quartile of all observed values of the five-year difference in health satisfaction in the overall study population. In a sensitivity analysis, declines by one point and by three points were also examined. Independent variables were the socioeconomic indicators, assessed in 1995 and expressed in quartiles, and the migration status (native German – immigrant arrived before 1990 – immigrant arrived between 1990 and 1994). ORs were first obtained crude and then adjusted for age, sex, marital status, number of household members (potential confounders) and for all other variables in the model. SAS release 8.02 was used for all statistical analyses[23]
Results
A total of 353 immigrants and 2,824 native Germans were enrolled. Table 1 shows demographic details of the immigrants. The age and sex distribution of the native Germans is identical due to the sampling procedure.
Table 1.
Demographic data of the immigrant group at baseline in 1995
| Age group | Number | Percent |
| 16–34 | 134 | 38.0 |
| 35–54 | 156 | 44.2 |
| 55–74 | 63 | 17.8 |
| total | 353 | 100.0 |
| Sex | Number | Percent |
| male | 177 | 50.1 |
| female | 176 | 49.9 |
| total | 353 | 100.0 |
| Country of origin | Number | Percent |
| Poland | 134 | 38.0 |
| Russia | 73 | 20.7 |
| Kazakhstan | 66 | 18.7 |
| Romania | 53 | 15.0 |
| other Eastern Europe | 27 | 7.7 |
| total | 353 | 100.0 |
| Arrival in Germany | ||
| <1989 | 154 | 43.6 |
| 1990–1994 | 195 | 55.2 |
| no information | 4 | 1.2 |
| total | 353 | 100.0 |
Health status and its change over time (hypotheses H1 and H3)
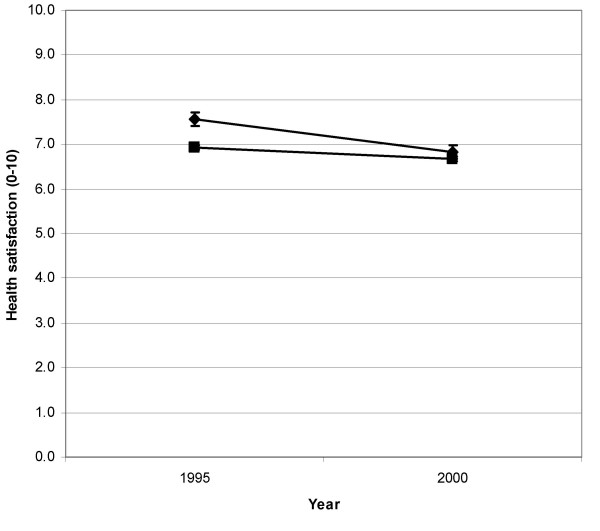
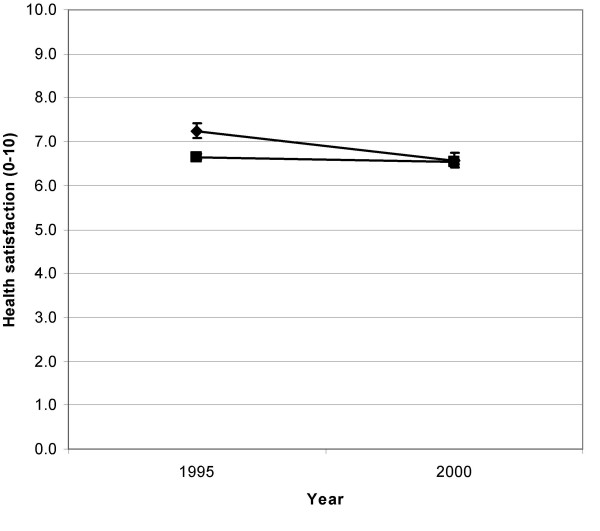
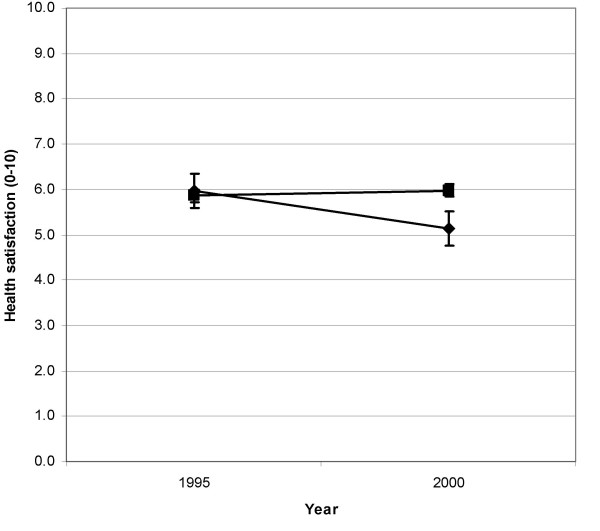
Mean values and 95% confidence intervals of health satisfaction among immigrants and native Germans in 1995 and 2000 are displayed in figures 1 and 2. In 1995, immigrants had a significantly higher health satisfaction (both sexes combined: p < 0.01). Five years later, differences were no longer significant. Separate analyses of the different age strata yielded similar results (data not shown). Men in the age group 55–74 years were an exception: In 1995, immigrants had a higher health satisfaction than native Germans, but the difference was not statistically significant; in 2000, their health satisfaction was significantly lower than that of native Germans (figure 3). Women of this age group had an initially lower health satisfaction than native German women of the same age, but this finding was not significant.
Figure 1.
Health satisfaction (scale 0–10) for males, all age groups combined immigrants (◆) and native Germans (■) in 1995 and 2000
Figure 2.
Health satisfaction (scale 0–10) for females, all age groups combined immigrants (◆) and native Germans (■) in 1995 and 2000
Figure 3.
Health satisfaction (scale 0–10) for males, aged 55–74 in 1995 immigrants (◆) and native Germans (■) in 1995 and 2000
Between 1995 and 2000, mean health satisfaction within the immigrant group declined significantly, by 0.73 points (p < 0.005) for men and 0.67 points (p < 0.005) for women. The respective values for native Germans were 0.24 (p < 0.005) and 0.11 points (p = 0.07). An age-stratified analysis revealed few exceptions. The average health satisfaction of female immigrants in the age group 55–74 slightly increased over time, but this subsample was small. In addition, the decrease of health satisfaction in both male and female native Germans of the oldest age group was not significant.
Socioeconomic disadvantage of immigrants (hypothesis H2)
Table 2 shows the comparison of socioeconomic parameters for immigrants and native Germans. In 1995, the immigrant group had significantly higher odds for all indicators for socioeconomic disadvantage than the native Germans. Five years later, the point estimates of the odds ratios for all indicators had declined; odds ratios were no longer significant for welfare dependency, and for unemployment among women. In other words, socioeconomic disadvantages of immigrants compared to native Germans has diminished between 1995 and 2000. Analyses of income and size of housing as continuous variables did not yield different results, with income and size of housing being significantly lower in the immigrant group for both sexes and in both years and with mean differences between the two groups being smaller in 2000 (not shown in table 2). Age-stratified analyses of all socio-economic variables gave similar results, with the exceptions of no difference in the prevalence of unemployment in 1995 for men aged 55–74 and women aged 16–34 years.
Table 2.
Prevalence odds ratios (ORs) with 95% confidence intervals (CIs)
| 1995 | ||||||||
| male | female | |||||||
| immigrants number (%) |
native Germans number (%) | OR | 95%-CI | immigrants number (%) |
native Germans number (%) | OR | 95%-CI | |
| lowest income quartile | 73 (42.2) | 285 (21.14) | 2.72 | [1.96;3.78] | 79 (46.2) | 326 (24.22) | 2.69 | [1.94;3.72] |
| welfare dependency | 30 (16.95) | 29 (2.05) | 9.73 | [5.68;15.67] | 28 (15.91) | 40 (2.84) | 6.47 | [3.88;10.79] |
| unemployed | 22 (12.43) | 83 (5.92) | 2.26 | [1.37;3.72] | 36 (20.45) | 149 (10.71) | 2.14 | [1.43;3.21] |
| lowest quartile size of housing | 91 (51.41) | 322 (23.23) | 3.50 | [2.54;4.82] | 87 (49.43) | 289 (20.85) | 3.71 | [2.69;5.12] |
| 2000 | ||||||||
| male | female | |||||||
| immigrants number (%) |
native Germans number (%) | OR | 95%-CI | immigrants number (%) |
native Germans number (%) | OR | 95%-CI | |
| lowest income quartile | 65 (38.01) | 293 (21.43) | 2.25 | [1.61;3.14] | 75 (43.6) | 329 (24.23) | 2.42 | [1.75;3.35] |
| welfare dependency | 5 (2.82) | 19 (1.34) | 2.13 | [0.78;5.78] | 5 (2.84) | 35 (2.49) | 1.14 | [0.44;2.96] |
| unemployed | 21 (11.86) | 94 (6.64) | 1.89 | [1.15;3.13] | 16 (9.09) | 113 (8.03) | 1.15 | [0.66;1.98] |
| lowest quartile size of housing | 85 (48.57) | 337 (23.99) | 2.99 | [2.17;4.12] | 83 (47.7) | 320 (23.01) | 3.05 | [2.21;4.21] |
Multivariate regression model
Table 3 displays the associations between a decline in health satisfaction and the socioeconomic factors as well as migration status. In the unadjusted analysis, immigrants, especially those who arrived between 1990 and 1994, have significantly higher odds of a decline in health satisfaction than native Germans. Welfare dependency and unemployment were significantly associated with the outcome. The same holds for income, but the effect was only significant for being in the second-lowest quartile. Housing size, in contrast, was not associated with declining health satisfaction. After adjustment for all socioeconomic factors and marital status, the effects of welfare dependency and unemployment diminished and lost significance. Housing size became even positively associated with declining health satisfaction. However, the effect of migration status remained unchanged; it still showed the strongest association in the model. Before including immigrants and native Germans in the same model, separate models for the two groups were calculated. Since the results showed no large differences, both groups were included into a single model. In sensitivity analyses, the cut-off point for the outcome "decline in health satisfaction" was lowered to one point and increased to three points. This did not appreciably change the results. Diagnostic statistics did not show any important multicollinearity in the model.
Table 3.
Odds ratios (ORs) and 95% confidence intervals for a decline in health satisfaction
| Crude OR (95% CI) | Multivariate-adjusted OR* (95% CI) | |
| Migration status | ||
| Native German† | 1 | 1 |
| Immigrant arrived before 1990 | 1.57 (1.11–2.24) | 1.58 (1.10–2.29) |
| Immigrant arrived 1990–1994 | 2.22 (1.64–3.01) | 2.18 (1.54–3.08) |
| Dependency on social welfare | ||
| no† | 1 | 1 |
| yes | 1.61 (1.10–2.36) | 1.00 (0.64–1.58) |
| Unemployment | ||
| no† | 1 | 1 |
| yes | 1.32 (1.00–1.73) | 1.20 (0.88–1.62) |
| Standardised per capita income | ||
| highest quartile† | 1 | 1 |
| second-highest quartile | 1.05 (0.82–1.35) | 1.08 (0.83–1.42) |
| second-lowest quartile | 1.38 (1.08–1.75) | 1.43 (1.09–1.88) |
| lowest quartile | 1.23 (0.97–1.57) | 1.23 (0.92–1.64) |
| Standardised per capita size of housing | ||
| highest quartile† | 1 | 1 |
| second-highest quartile | 0.81 (0.63–1.03) | 0.74 (0.56–0.97) |
| second-lowest quartile | 0.95 (0.76–1.20) | 0.80 (0.60–1.07) |
| lowest quartile | 1.00 (0.80–1.26) | 0.73 (0.53–1.01) |
*adjusted for age in years, sex, marital status, number of household members and all other variables in the model †reference category
Discussion
Findings
The main finding of this study is that the health status of immigrants from Eastern Europe, expressed by their health satisfaction, deteriorated to a much larger degree than that of native Germans, in spite of substantial improvements in all indicators of SES that the immigrants experienced.
Hypotheses H2 and H3 were supported by the findings. Immigrants were socioeconomically disadvantaged relative to native Germans, although this gap became smaller over time. Nevertheless, the decline in health satisfaction among the immigrants was much steeper than among native Germans over the same time period. The regression model shows that after multivariate adjustment, this decline is primarily associated with being an immigrant, and not with socioeconomic status. This finding possibly reflects the unfavourable health conditions and high prevalence levels of risk factors the immigrants were exposed to in Eastern Europe. These might include a high prevalence of smoking, hypertension, deficiencies in antioxidants due to a low consumption of fruits and vegetables or frequent binge drinking, which all have been discussed as determinants of the mortality crisis in Eastern Europe[4]. Some immigrants might have already had subclinical disease upon arrival in Germany which only after some time became apparent and caused their health satisfaction to deteriorate. Immigrants who arrived after 1990 had an even higher risk of deteriorating health satisfaction, in line with the increasingly deteriorating health conditions in their countries of origin after the breakdown of the Iron Curtain in 1989[4]. Alternatively, the observed decline could be due to factors associated with immigrant status but not reflected by standard socioeconomic indicators. Examples are psychological stress, discrimination, or a lack of informal support networks.
In contrast, hypothesis H1, postulating an initially lower health satisfaction among immigrants, was not supported by the findings. At the beginning of the observation period, younger immigrants even had a higher health satisfaction than native Germans; older immigrants had values similar to those of Germans. This phenomenon is known as "healthy migrant effect". One explanation is a selection effect at the time of migration[8]. Recent explanatory models postulate a second effect, the so-called "late-entry-bias". This implies that immigrants with a poor health status may remain excluded from studies that start enrolling participants only years after the time of immigration[24].
Selection effects may have played a role especially in young people who migrated for economical reasons. This may cause a selection towards people who are part of the working force, who is normally healthier than the general population[25]. Among older people of ethnic German origin, however, even those with poorer health status may have decided to migrate. Common motives are an affinity to Germany, seen as the original home country, and negative feelings towards Eastern European countries, experienced as oppressors during the Communist regime[26]. This could explain the finding that initially there was no better health satisfaction in the oldest age groups.
Late-entry-bias could have played a role, too: Most of the participants had immigrated some years before recruitment into the GSOEP. Finally, the perceived health satisfaction in young people may still be high in spite of a high prevalence of risk factors because for many chronic diseases there is a long time lag between exposure and onset[12,13]. In all probability, the initially higher health satisfaction among younger immigrants is caused by an interplay of the factors discussed.
The findings are in line with results from a previous study, which also used the GSOEP and looked into morbidity measures of Germans and migrants from Southern Europe with longitudinal comparisons between 1984 and 1991[9]. The study found for two out of three measures a lower morbidity among migrants in 1984, but the increase in morbidity was faster among migrants than Germans. Initial morbidity among migrants was higher in women than in men, but the magnitude of the increase in morbidity was higher in male migrants. This sex-specific pattern was similar to the one found in the present study. One possible explanation are sex-specific differences in the perception of health[27].
The results of the present study are also supported by findings from Israel, a country which has experienced an immigration of 775,000 Jews from the former Soviet Union since 1989. Two cross-sectional surveys performed in 1998 found lower self-reported health among immigrants compared to veteran Israelis[28,29]. In both studies, lower self-reported health was associated with a more frequent reporting of chronic disease. Adjustment for socio-economic variables did not change these results. One of the studies showed that more recent immigrants had a significantly higher risk of reporting sub-optimal health and having at least one disease. Earlier immigrants, in contrast, did not show differences in the prevalence of disease compared to veterans. This might be explained by a strong selection which caused the migration of more healthy people in the beginning of this big migration wave to Israel[28].
Limitations
This study has some limitations. Although the GSOEP is representative of the population in Germany [13-16], this may not have been the case for the study population. The GSOEP provides weighting factors which allow adjustment for disproportionate sampling when using the complete GSOEP dataset. However, due to the inclusion criteria of the study, weighting was not possible.
Another drawback is that persons living in institutional settings, such as housing facilities for immigrants, are underrepresented in the GSOEP[30]. Immigrants of ethnic German origin stay in such facilities for an average period of 1.5 years after arrival in Germany[31]. These facilities are regarded as "foci of social problems" [31], so an under-representation of their inhabitants in the GSOEP might lead to an overestimation of health and socioeconomic status of the immigrant population in our study.
Excluding the GSOEP participants who did not answer the question on health satisfaction both in 1995 and 2000, or who dropped out of the panel, may also have introduced a bias. Persons with poor health status are probably underrepresented since they have a higher probability to be lost to follow-up[32]. Drop-out rates in the immigrant group are higher, especially in older age groups. The selection bias that might possibly result, however, would not change our conclusions since it would lead to an underestimation of the decline in health satisfaction in the immigrant group.
Finally, health satisfaction is a subjective indicator, so its appropriateness as a proxy for the actual health status needs to be discussed. A review of twenty-seven studies in different cultural settings has shown measures of self-rated health, based on questions with different wording and using different scales, to be valid predictors of mortality[17]. These findings were confirmed in a German national health survey[19] and for the GSOEP[18]. Self-rated health measures have been shown to have a high reliability [20] and to provide valid results in different ethnic groups[21]. Nevertheless, it cannot be completely excluded that answers to the question on health satisfaction are influenced by the differing cultural backgrounds of immigrants and native Germans. The adaptation to a new environment which immigrants have to undergo may influence health satisfaction even though it doesn't affect health in an objectively measurable way. For example, differences between the image the immigrants had of Germany before arriving and the reality they experience afterwards could cause a general disappointment which could be expressed through deteriorating health satisfaction. Even poor knowledge of the German language could bias the results in the immigrant group towards higher or lower values. Nevertheless, there are convincing arguments for using self-rated health as an outcome. It can provide a more holistic view of health which may not be reflected by "objective" health measures such as quantifiable medical diagnoses[17].
It is not entirely clear which magnitude a decline in health satisfaction on a scale from 0 to 10 has to have in order to reflect a relevant deterioration in perceived health. The cut-off point for the regression model was chosen using the highest quartile of all values of deterioration reported in the study population. It is also not clear if a decline of a given magnitude has the same meaning independently of the absolute values of health satisfaction. Finally, a period of five years between the two measurements might also be too short to draw conclusions from changes in reported health satisfaction. A Swedish study, however, demonstrated a significantly higher mortality in men who had reported a deterioration of two or more points on a 7-point scale of self-perceived health over a period of seven years[33]. This suggests that the degree of deterioration measured in the present study and the time interval are sufficiently large to mirror relevant changes in self-perceived health.
Conclusions
The rapidly deteriorating health status of immigrants from Eastern Europe, occurring independently of improvements in their socioeconomic status, should be of concern to public health and health policy in Germany. Other European countries may experience similar challenges: The International Organisation for Migration (IOM) predicts that 3–5 million more people will immigrate from the new EU member states in Eastern Europe alone[34]. Future research needs to validate the findings of the present study with objective outcome indicators such as morbidity or cause-specific mortality. Also, the presumably high prevalence of risk factors, which could not be measured in this study, needs to be confirmed. In addition, a deeper insight into the immigrants' life situation is needed to identify disadvantages specific to this group which may reach beyond financial and employment issues. Once more data are available, immigrants from Eastern Europe need to be a target group of public health interventions to prevent the rapid deterioration in their health status.
Competing interests
None declared.
Authors' contributions
UR did the statistical analyses and drafted the paper. OR developed the hypotheses, conceived of the study, participated in its design and coordination and provided statistical advice. Both authors read and approved the final manuscript.
Acknowledgments
Acknowledgements
The data of the German Socio-Economic Panel (SOEP) used in this publication were provided by the Deutsches Institut für Wirtschaftsforschung (DIW), Berlin. Ulrich Ronellenfitsch is supported by a Ph.D. grant from Deutsche Forschungsgemeinschaft (GK 793: Epidemiology of communicable and chronic non-communicable diseases and their interrelationships).
Contributor Information
Ulrich Ronellenfitsch, Email: Ulrich.Ronellenfitsch@urz.uni-heidelberg.de.
Oliver Razum, Email: Oliver.Razum@urz.uni-heidelberg.de.
References
- Münz R. Woher? Wohin? Europäische Integrationsmuster 1950 - 2000. In: Bade KJ and Münz R, editor. Migration in Europa. Hannover, Niedersächsische Landeszentrale für politische Bildung; 2001. pp. 21–40. [Google Scholar]
- Bundeszentrale für politische Bildung, editor. Aussiedler. München, Franzis' print &media GmbH; 2000. (Informationen zur politischen Bildung, vol 267). Bundeszentrale für politische Bildung. [Google Scholar]
- Bevölkerung nach Staatsangehörigkeit. 2003. http://www.destatis.de/basis/d/bevoe/bevoetab10.htm
- Bobak M, Marmot M. East-West mortality divide and its potential explanations: proposed research agenda. BMJ. 1996;312:421–425. doi: 10.1136/bmj.312.7028.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Health for All Mortality Database. Copenhagen, WHO Regional Office for Europe; 2004. [Google Scholar]
- Men T, Brennan P, Boffetta P, Zaridze D. Russian mortality trends for 1991-2001: analysis by cause and region. BMJ. 2003;327:964. doi: 10.1136/bmj.327.7421.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson P. Self-perceived health in East and West Europe: another European health divide. Soc Sci Med. 1998;46:1355–1366. doi: 10.1016/S0277-9536(97)10093-4. [DOI] [PubMed] [Google Scholar]
- Razum O, Twardella D. Time travel with Oliver Twist--towards an explanation for a paradoxically low mortality among recent immigrants. Trop Med Int Health. 2002;7:4–10. doi: 10.1046/j.1365-3156.2002.00833.x. [DOI] [PubMed] [Google Scholar]
- Lechner I, Mielck A. [Decrease in the "healthy migrant effect": trends in the morbidity of foreign and German participants in the 1984-1992 Socioeconomic Panel] Gesundheitswesen. 1998;60:715–720. [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Marmot M, Ryff CD, Bumpass LL, Shipley M, Marks NF. Social inequalities in health: next questions and converging evidence. Soc Sci Med. 1997;44:901–910. doi: 10.1016/S0277-9536(96)00194-3. [DOI] [PubMed] [Google Scholar]
- Rose G. Incubation period of coronary heart disease. Br Med J (Clin Res Ed) 1982;284:1600–1601. doi: 10.1136/bmj.284.6329.1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law M, Wald N. Why heart disease mortality is low in France: the time lag explanation. BMJ. 1999;318:1471–1476. doi: 10.1136/bmj.318.7196.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SOEP Group. The German Socio-Economic Panel (GSOEP) after more than 15 years - Overview. In: HolstE, LillardDR and DiPreteA, editor. Proceedings of the 2000 Fourth International Conference of German Socio-Economic Panel Study Users (GSOEP2000), Berlin, Duncker & Humblot; 2001. pp. 7–14. (Vierteljahrshefte zur Wirtschaftsforschung;). [Google Scholar]
- Wagner G. Kennziffern zur Charakterisierung der Stabilität von Panel-Erhebungen - Das Beispiel des SOEP. Berlin: Deutsches Institut für Wirtschaftsforschung; 1991. (DIW Discussion Papers, vol 27). Deutsches Institut für Wirtschaftsforschung. [Google Scholar]
- Rendtel U. Über die Repräsentativität von Panelstichproben. Eine Analyse der feldbedingten Ausfälle im Sozio-oekonomischen Panel. Berlin: Deutsches Institut für Wirtschaftsforschung; 1993. (DIW Discussion Papers, vol 70). Deutsches Institut für Wirtschaftsforschung. [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- Schwarze J, Andersen HH, Anger S. Self-rated health and changes in self-rated health as predictors of mortality - First evidence from German panel data. 2000. (DIW Discussion Papers).
- Helmert U. [Perceived general health and mortality] Gesundheitswesen. 2003;65:47–54. doi: 10.1055/s-2003-36913. [DOI] [PubMed] [Google Scholar]
- Martikainen P, Aromaa A, Heliovaara M, Klaukka T, Knekt P, Maatela J, Lahelma E. Reliability of perceived health by sex and age. Soc Sci Med. 1999;48:1117–1122. doi: 10.1016/S0277-9536(98)00416-X. [DOI] [PubMed] [Google Scholar]
- Chandola T, Jenkinson C. Validating self-rated health in different ethnic groups. Ethn Health. 2000;5:151–159. doi: 10.1080/713667451. [DOI] [PubMed] [Google Scholar]
- Buhmann B, Rainwater L, Schmaus G, Smeeding TM. Equivalence scales, well-being, inequality and poverty: sensitivity estimates across ten countries using the Luxembourg Income Study (LIS) database. Review of Income & Wealth. 1988;34:115–142. [Google Scholar]
- The SAS system, release 8.02. Cary, NC, SAS Institute Inc.; 2001. [Google Scholar]
- Razum O, Rohrmann S. [The healthy migrant effect: role of selection and late entry bias] Gesundheitswesen. 2002;64:82–88. doi: 10.1055/s-2002-20271. [DOI] [PubMed] [Google Scholar]
- Li CY, Sung FC. A review of the healthy worker effect in occupational epidemiology. Occup Med (Lond) 1999;49:225–229. doi: 10.1093/occmed/49.4.225. [DOI] [PubMed] [Google Scholar]
- Mammey U. Zur Situation der Aussiedler in der Bundesrepublik Deutschland: Werkstattbericht zum Projekt des Bundesinstituts für Bevölkerungsforschung. Raumforschung und Raumordnung. 1993;51:265–275. [Google Scholar]
- Gijsbers van Wijk CM, van Vliet KP, Kolk AM, Everaerd WT. Symptom sensitivity and sex differences in physical morbidity: a review of health surveys in the United States and The Netherlands. Women Health. 1991;17:91–124. doi: 10.1300/J013v17n01_06. [DOI] [PubMed] [Google Scholar]
- Baron-Epel O, Kaplan G. Self-reported health status of immigrants from the former Soviet Union in Israel. Isr Med Assoc J. 2001;3:940–946. [PubMed] [Google Scholar]
- Gross R, Brammli-Greenberg S, Remennick L. Self-rated health status and health care utilization among immigrant and non-immigrant Israeli Jewish women. Women Health. 2001;34:53–69. doi: 10.1300/J013v34n03_04. [DOI] [PubMed] [Google Scholar]
- Haisken-DeNewJP and FrickJR, editor. Desktop Companion to the German Socio-Economic Panel Study (GSOEP), Version 5.0. Berlin, Deutsches Institut für Wirtschaftsforschung; 2001. [Google Scholar]
- Hülskemper M. Integrationschancen von Aussiedlern. Eine Einschätzung ihrer sozialen Situation in der Bundesrepublik. Informationsdienst zur Ausländerarbeit. pp. 48–53.
- Heller G, Schnell R. The Choir Invisible. In: Helmert U, editor. Müssen Arme früher sterben. Weinheim, Juventa-Verlag; 2000. pp. 115–134. [Google Scholar]
- Svardsudd K, Tibblin G. Is quality of life affecting survival? The study of men born in 1913. Scand J Prim Health Care Suppl. 1990;1:55–60. [PubMed] [Google Scholar]
- Baker M. Eastern Europe: German Bank Study Foresees High Outward Migration For 50 Years. 2003. http://www.rferl.org/nca/features/2003/08/06082003160751.asp