Abstract
Objective
Multicenter longitudinal outcome data for Fontan patients surviving into adulthood are lacking. The aim of this study was to better understand contemporary outcomes in Fontan survivors by collecting follow-up data in a previously well-characterized cohort.
Design
Baseline data from the Fontan Cross-Sectional Study (Fontan 1) were previously obtained in 546 Fontan survivors aged 11.9 ± 3.4 years. We assessed current transplant-free survival status in all subjects 6.8 ± 0.4 years after the Fontan 1 study. Anatomic, clinical, and surgical data were collected along with socioeconomic status and access to health care.
Results
Thirty subjects (5%) died or underwent transplantation since Fontan 1. Subjects with both an elevated (>21 pg/mL) brain natriuretic peptide and a low Child Health Questionnaire physical summary score (<44) measured at Fontan 1 were significantly more likely to die or undergo transplant than the remainder, with a hazard ratio of 6.2 (2.9–13.5). Among 516 Fontan survivors, 427 (83%) enrolled in this follow-up study (Fontan 2) at 18.4 ± 3.4 years of age. Although mean scores on functional health status questionnaires were lower than the general population, individual scores were within the normal range in 78% and 88% of subjects for the Child Health Questionnaire physical and psychosocial summary score, and 97% and 91% for the SF-36 physical and mental aggregate score, respectively. Since Fontan surgery, 119 (28%) had additional cardiac surgery; 55% of these (n = 66) in the interim between Fontan 1 and Fontan 2. A catheter intervention occurred in 242 (57%); 32% of these (n = 78) after Fontan 1. Arrhythmia requiring treatment developed in 118 (28%) after Fontan surgery; 58% of these (n = 68) since Fontan 1.
Conclusions
We found 95% interim transplant-free survival for Fontan survivors over an average of 7 years of follow-up. Continued longitudinal investigation into adulthood is necessary to better understand the determinants of long-term outcomes and to improve functional health status.
Introduction
The Fontan procedure results in near-normal systemic oxygen saturation in those born with a functional single ventricle, reducing the demands on the systemic ventricle and extending the lives of patients with even the most complex forms of congenital heart disease. Nevertheless, the resulting abnormal hemodynamic state is associated with a variety of late complications including decreased exercise performance, abnormal ventricular function, intracardiac and extracardiac thrombosis and embolic phenomena, arrhythmias and conduction system impairment, cirrhosis, and protein-losing enteropathy.1–4 As these patients age into adulthood, access to specialized health care may become limited as a result of insufficient insurance, lack of employment, and lack of education about the need for evaluation by adult congenital heart physicians.5,6 Therefore, although the survival of children and adolescents with the Fontan procedure continues to improve, survivors remain at increased risk for mortality and morbidities, as well as physiologic limitations that are likely to impact physical, psychological, and socioeconomic status.7,8
The Pediatric Heart Network Fontan Cross-Sectional Study (Fontan 1) characterized a multi-institutional cohort of 546 survivors after the Fontan procedure, with an age of 6 to 18 years at enrollment in 2003–2004.9 The design of Fontan 1 could not determine if observed differences between older and younger subjects were related to the length of time living with Fontan physiology or to changes in medical, catheter-based, or surgical management strategies. The primary objective of the current study (Fontan 2) was to better understand contemporary outcomes in Fontan survivors by collecting follow-up data involving assessment of vital status, repeat functional health status, collection of interim medical history, and access to health care at an average of 7 years after enrollment in Fontan 1.
Methods
Study Design and Patient Population
Vital and cardiac transplant status data were assessed in all 546 subjects enrolled in Fontan 1. From this original group, subjects who were alive with a Fontan circulation were approached for enrollment into the present study. Each center’s institutional review board approved the protocol. Written informed consent and assent were obtained according to local requirements. Anatomic, clinical, and surgical data were collected at enrollment (November 2009 to May 2011) using standardized forms. Structured interviews with the parent/guardian and/or subject were used to assess current clinical state, socioeconomic status, family functioning, and access to health care. Vital status was assessed by either contact or by search of the social security death index annually following enrollment.
Measures of Functional Health Status and Quality of Life
The Child Health Questionnaire (CHQ), which includes questionnaires for both the child and the parent, was used for subjects ≤18 years. In subjects aged ≥19 years, functional status was measured with the Short-Form Health Survey version 2 (SF-36).10 The Pediatric Quality of Life Inventory (Peds-QL) with a self-report and a parallel parent proxy report was used to assess quality of life.11,12 In addition, a cardiac disease-specific module of the Peds-QL was administered. Pediatric Quality of Life Inventory age group versions (8–12 years old, 13–18 years old, and 19–25 years old) have almost identical questions with minor differences in language. To preserve sample size and after consultation with experts (personal communication with J. Varni, MD, July, 2013), we combined these versions for analytic purposes.
Statistical Methods
The relationship between transplant-free survival and baseline (assessed at Fontan 1) covariates was examined using Cox proportional hazards regression modeling. Follow-up time was defined as the time from Fontan 1 medical record review until either death/transplant or the latest available assessment of vital/transplant status (at or after Fontan 2 enrollment). We report hazard ratios with 95% confidence intervals and P values associated with the Wald chi-square test. Statistical significance was considered using a two-sided critical value of P = .05. The proportional hazards assumption was evaluated using a supremum test for nonproportionality based on Martingale residuals, and interaction terms with time were considered as appropriate. Key results are illustrated using Kaplan–Meier survival plots.
Subsequent analyses compared prespecified subgroups defined by ventricular morphology, Fontan procedure type, and age at enrollment. Differences in patient outcomes by subgroup levels were assessed using a regression model adjusted for age, gender (if gender mix differed), and clinical site (for medical history variables and medication use). For continuous outcomes, mean values by subgroup were compared using a parametric analysis of variance-based test and an age- and gender-adjusted analysis of covariance. Additionally, median values by subgroup were compared using a nonparametric (Wilcoxon or Kruskal–Wallis) test. If any of these three tests was significant, Bonferroni corrections were calculated. For binary outcomes, frequencies in the subgroups were compared using Fisher’s exact test and a gender- and age-adjusted logistic regression model. For ordered categorical outcomes, the presence of a linear trend was assessed using Mantel-Haenszel test for trend, and a gender- and age-adjusted cumulative or multinomial logistic regression was used as appropriate. For interim medical history events, mean incidence rates of the event were compared by subgroup using Poisson regression. To explore differences related to age, we divided the study population into two groups (younger vs. older). For continuous variables and instruments validated across all ages, e.g. medical history and Peds-QL, 18 years was selected as a cutoff value. The cutoff of 18 was selected as this age is used frequently to define an adult and this provided similar sized groups for comparison. For instruments validated only in children (e.g., CHQ-PF50 and CHQ-CF87), 16 years was selected as a cutoff. Similarly, for forms validated only in adults (e.g., SF-36), the adult cohort (defined as ≥19 years) was divided into two roughly similar sized groups; those < or ≥22.5 years. All analyses were performed using SAS statistical software version 9.3 (SAS Institute, Inc., Cary, NC, USA).
Results
Patient Characteristics
From the original Fontan 1 cohort of 546 subjects, 29 (5%) either died (n = 16) or were transplanted (n = 13) prior to Fontan 2 enrollment and 1 subject died after enrollment. Additionally, one subject underwent a conversion to a two-ventricle circulation prior to Fontan 2 enrollment. The 516 surviving subjects with a Fontan circulation were considered eligible for the Fontan 2 study and 427 subjects (83%) enrolled. Thirteen subjects (2.5%) were lost to follow-up and 76 subjects (15%) did not give consent. The enrolled subjects were compared with the eligible but non-consenting subjects who either were lost to follow-up or refused consent. Enrolled subjects were younger (18.4 ± 3.4 vs. 19.6 ± 3.3 years, P = .002) and had a lower proportion of males (58% vs. 71%, P = .02). After adjustment for age and gender, enrollees came from households with a higher income level and higher level of maternal education (P < .001 for both). No differences were identified in any cardiac characteristics or laboratory measures from Fontan 1.
Died/Transplanted vs. Transplant-free Survivors
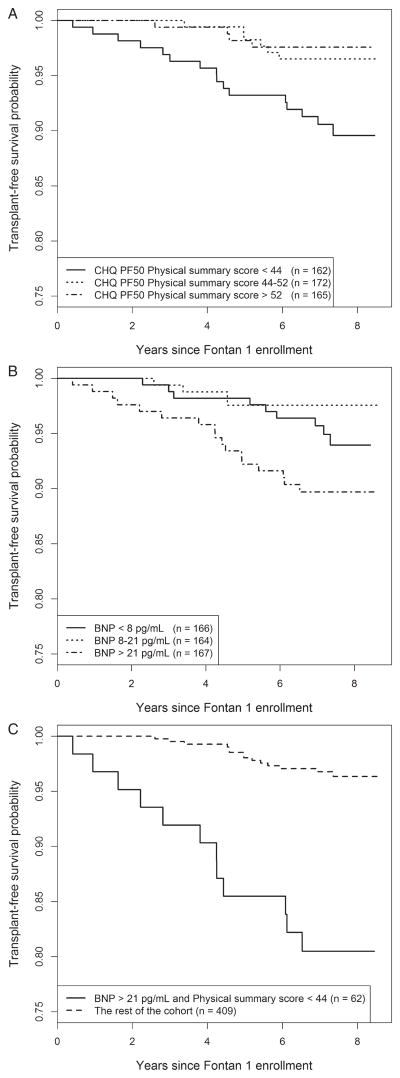
Vital status assessment data were collected on all of the original 546 subjects except the 13 who were lost to follow-up. The social security death index was searched for the 13 lost-to-follow-up subjects and none were reported to have died. The 502 transplant-free survivors through the end of follow-up were compared with the 30 who died or had heart transplants (1 subject died after enrolling in Fontan 2) (Figure 1). There were no differences in the risk of death/transplant based on age, dominant ventricular morphology, or type of Fontan procedure. On univariate analysis, the risk of death or transplant after Fontan 1 was significantly associated with the following measurements obtained at Fontan 1: a poorer CHQ-PF50 physical summary score (36.6 ± 13.6 vs. 45.8 ± 11.5, P < .01) (Figure 2A), increased end systolic and end diastolic volume z-scores (P < .02 for both), a higher brain natriuretic peptide (BNP) concentration value (P = .04) (Figure 2B), and inability to perform an exercise test (P < .05). The hazard of death/transplant for subjects with both an elevated BNP (>21 pg/mL) and a low physical summary score (<44) was 6.2 (2.9–13.5) times higher than for the rest of the cohort (Figure 2C).
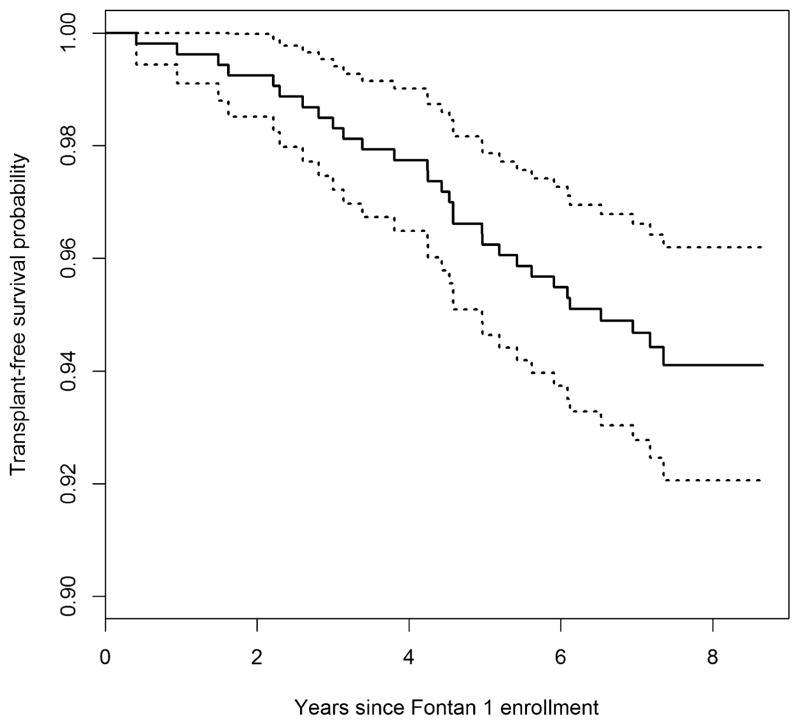
Figure 1.
Transplant-free survival since Fontan 1 (with 95% confidence intervals) in a cohort of 532 subjects with complete follow-up data. For improved resolution, the scale on the y-axis is limited to 0.9–1.0.
Figure 2.
Association of interim (between Fontan 1 and Fontan 2) transplant-free survival with CHQ-PF50 physical summary score (A); serum BNP level (B); and both (C). For improved resolution, the scale on the y-axis is limited to 0.75–1.0. BNP, brain natriuretic peptide; CHQ, Child Health Questionnaire.
Fontan 2 Cohort Characteristics
The 427 enrolled subjects were 18.4 ± 3.4 years old at Fontan 2 enrollment. The mean follow-up time was 6.8 ± 0.4 years from Fontan 1 and 15.2 ± 3.4 years after Fontan surgery. Since Fontan surgery, 119 subjects (28%) had additional cardiac surgery, with 55% of these (n = 66) occurring in the interim between Fontan 1 and Fontan 2. During the interim period, 10 subjects underwent a Fontan conversion. The most common surgical procedure performed since Fontan 1 involved placement or replacement of implantable electronic devices, which were currently in place in 13% (n = 56). A cardiac catheter intervention occurred in 242 subjects (57%); 32% of these (n = 78) took place after Fontan 1. Since the Fontan procedure, stroke was reported in 2%, seizures in 5%, thrombosis in 9%, cirrhosis in 4%, plastic bronchitis in 0.5%, and protein-losing enteropathy in 7%. Arrhythmia receiving treatment or intervention since the Fontan surgery occurred in 118 (28%) subjects; 58% of these (n = 68) happened since Fontan 1.
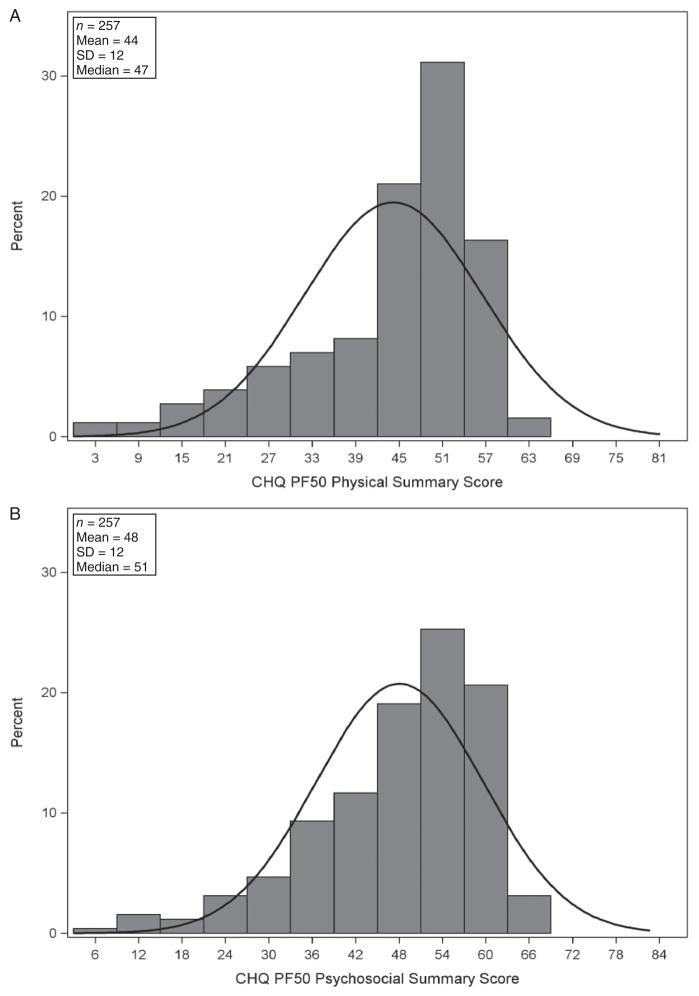
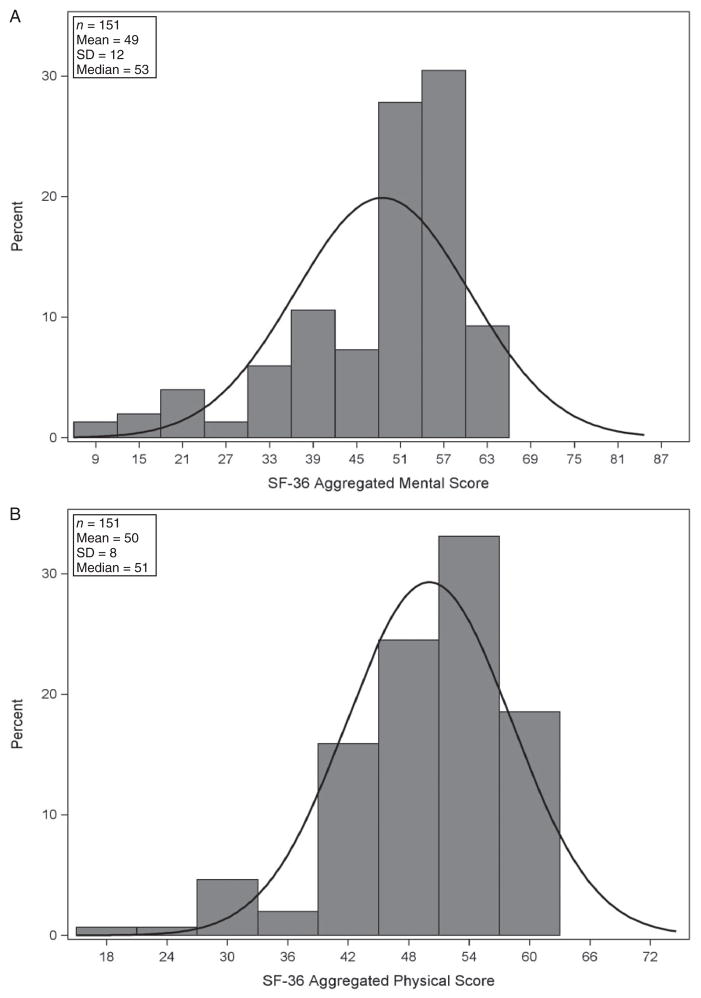
Mean CHQ-PF50 summary scores for the 264 subjects <19 years were significantly lower than those of historical, healthy, control subjects13 (44 ± 12 vs. 53 ± 9 for physical, and 48 ± 12 vs. 51 ± 9 for psychosocial summary scores, each P < .01). However, individual scores were within the 95th percentile confidence interval of the mean of historical healthy controls in 78% of subjects for the physical summary score and in 88% for the psychosocial summary score. (Figure 3) Mean summary scores among the 153 adult subjects completing the SF-36 were not different (P > .1) from those for healthy controls: the aggregate physical score was 50 ± 8; 97% of Fontan 2 subjects scored within the 95th percentile confidence interval for the mean of healthy control subjects. The aggregate mental score was 49 ± 12 with 91% of Fontan 2 subjects scoring within the 95th percentile confidence interval of the expected mean score of 50 (Figure 4).
Figure 3.
The distribution of Child Health Questionnaire-Parent Form (CHQ-PF50) physical (A) and psychosocial (B) summary scores from 257 children enrolled in the Fontan 2 Study. The line shows the normal distribution for the general population. SD, standard deviation.
Figure 4.
The distribution of Short Form 36 (SF-36) physical (A) and mental aggregate (B) scores from 153 adults enrolled in the Fontan 2 Study. The line shows the normal distribution for the general population. SD, standard deviation.
Association with Ventricular Dominance
The ventricular morphology was left dominant in 214, right dominant in 141, and mixed in 72 of the 427 enrolled subjects (Table 1). Subjects with a dominant right ventricle (RV) used a greater number of medicines. Those with a dominant RV were prescribed angiotensin-converting enzyme (ACE) inhibitors more frequently compared with the others, even after adjustments were made for differences by clinical center. Parents of subjects with a dominant RV reported a lower physical functioning domain score on the CHQ-PF50, although there was no difference in the analogous domain reported by the subjects themselves on the CHQ-CF87. Similarly, only a single domain on either the parent or subject, Peds-QL differed by ventricular dominance. Subjects (but not their parents) with a dominant RV reported a better “treatment” score compared with those with mixed ventricular morphology. Differences were observed in 8 of the 10 scales of the SF-36 among adult subjects with those with left ventricular morphology scoring better and those with mixed ventricular morphology scoring the poorest.
Table 1.
Patient Characteristics by Ventricular Dominance
| Total (n = 427) | Left (n = 214) | Right (n = 141) | Mixed (n = 72) | P value* | ||
|---|---|---|---|---|---|---|
| Age, years | Mean ± SD | 18.4 ± 3.4 | 18.7 ± 3.3 | 17.9 ± 3.3 | 18.5 ± 3.7 | .15† |
| Male | n (%) | 249 (58%) | 119 (56%) | 94 (67%) | 36 (50%) | .05‡ |
| Post-Fontan surgery medical review record | n | 426 | 214 | 140 | 72 | |
| Age, years | Mean ± SD | 18.6 ± 3.4 | 18.9 ± 3.4 | 18.1 ± 3.4 | 18.8 ± 3.7 | .14 |
| Follow-up time, years | Mean ± SD | 15.2 ± 3.4 | 15.5 ± 3.3 | 14.8 ± 3.4 | 15.1 ± 3.4 | .38 |
| Cardiac surgical procedure | n (%) | 119 (28%) | 70 (33%) | 36 (26%) | 13 (18%) | .04 |
| Cardiac cath intervention | n (%) | 242 (57%) | 118 (55%) | 84 (60%) | 40 (56%) | .51 |
| Stroke | n (%) | 10 (2%) | 5 (2%) | 5 (4%) | 0 (0%) | .07 |
| Seizure | n (%) | 23 (5%) | 11 (5%) | 11 (8%) | 1 (1%) | .05 |
| Thrombosis | n (%) | 39 (9%) | 24 (11%) | 11 (8%) | 4 (6%) | .47 |
| Arrhythmia | n (%) | 118 (28%) | 62 (29%) | 32 (23%) | 24 (33%) | .68 |
| Other important complications | n (%) | 215 (50%) | 98 (46%) | 73 (52%) | 44 (61%) | .25 |
| Protein-losing enteropathy | n (%) | 30 (7%) | 11 (5%) | 8 (6%) | 11 (15%) | .15 |
| Cirrhosis diagnosis | n (%) | 15 (4%) | 5 (2%) | 7 (5%) | 3 (4%) | .24 |
| Plastic bronchitis diagnosis | n (%) | 2 (0.5%) | 1 (0.5%) | 1 (1%) | 0 (0%) | .99 |
| IED in place | n (%) | 56 (13%) | 38 (18%) | 15 (11%) | 3 (4%) | .002 |
| Clinical assessment | ||||||
| Percentile height for age | Mean ± SD | 36.7 ± 30.9 | 37.5 ± 31.4 | 34.3 ± 30.2 | 39.7 ± 31.5 | .60 |
| Height-for-age z-score | Mean ± SD | −0.6 ± 1.4 | −0.6 ± 1.4 | −0.8 ± 1.5 | −0.4 ± 1.5 | .37 |
| Percentile weight for age | Mean ± SD | 45.1 ± 33.8 | 44.5 ± 33.5 | 44.4 ± 35.7 | 48.7 ± 30.5 | .81 |
| Weight-for-age z-score | Mean ± SD | −0.3 ± 1.6 | −0.3 ± 1.5 | −0.4 ± 1.7 | −0.1 ± 1.2 | .68 |
| BMI-for-age z-score | Mean ± SD | −0.0 ± 1.3 | 0.0 ± 1.2 | −0.1 ± 1.4 | 0.1 ± 1.1 | .95 |
| NYHA heart failure classification | .14 | |||||
| Class I | n (%) | 234 (55%) | 125 (58%) | 74 (53%) | 35 (49%) | |
| Class II | n (%) | 119 (28%) | 57 (27%) | 42 (30%) | 20 (28%) | |
| Class III | n (%) | 49 (12%) | 22 (10%) | 15 (11%) | 12 (17%) | |
| Class IV | n (%) | 24 (6%) | 10 (5%) | 9 (6%) | 5 (7%) | |
| Medications | ||||||
| Number of medications | n (%) | .002 | ||||
| 0 | n (%) | 45 (11%) | 27 (13%) | 7 (5%) | 11 (15%) | |
| 1 | n (%) | 99 (23%) | 60 (28%) | 25 (18%) | 14 (19%) | |
| ≥2 | n (%) | 282 (66%) | 127 (59%) | 108 (77%) | 47 (65%) | |
| Mean ± SD | 2.9 ± 2.6 | 2.5 ± 2.4 | 3.4 ± 2.9 | 2.8 ± 2.5 | <.001 | |
| ACE Inhibitors | n (%) | 226 (53%) | 92 (43%) | 102 (73%) | 32 (44%) | <.001 |
| CHQ-PF50—parent report | n | 264 | 124 | 98 | 42 | |
| Age, years | Mean ± SD | 16.3 ± 1.6 | 16.3 ± 1.6 | 16.3 ± 1.8 | 16.0 ± 1.4 | .48 |
| Physical summary score | Mean ± SD | 44 ± 12 | 43 ± 13 | 44 ± 12 | 47 ± 9 | .11 |
| Psychosocial summary score | Mean ± SD | 48 ± 12 | 49 ± 10 | 47 ± 12 | 48 ± 13 | .61 |
| Global health scale | Mean ± SD | 77 ± 21 | 77 ± 21 | 76 ± 21 | 83 ± 20 | .22 |
| Physical functioning scale | Mean ± SD | 81 ± 21 | 82 ± 21 | 78 ± 23 | 88 ± 13 | .01 |
| CHQ-CF87—child report | n | 255 | 121 | 93 | 41 | |
| Age, years | Mean ± SD | 16.3 ± 1.6 | 16.3 ± 1.5 | 16.3 ± 1.8 | 16.0 ± 1.4 | .46 |
| Global health scale | Mean ± SD | 76 ± 21 | 77 ± 20 | 75 ± 24 | 76 ± 21 | .52 |
| Physical functioning scale | Mean ± SD | 87 ± 14 | 88 ± 14 | 86 ± 16 | 90 ± 10 | .18 |
| Peds-QL—parent report | n | 262 | 123 | 97 | 42 | |
| Age, years | Mean ± SD | 16.2 ± 1.6 | 16.3 ± 1.6 | 16.2 ± 1.8 | 16.0 ± 1.4 | .48 |
| 4.0 generic core scales | ||||||
| Physical functioning score | Mean ± SD | 72 ± 21 | 72 ± 21 | 71 ± 22 | 75 ± 20 | .45 |
| Emotional functioning score | Mean ± SD | 72 ± 20 | 72 ± 20 | 71 ± 21 | 73 ± 19 | .70 |
| Social functioning score | Mean ± SD | 71 ± 25 | 73 ± 25 | 67 ± 25 | 74 ± 23 | .09 |
| School functioning score | Mean ± SD | 64 ± 21 | 64 ± 22 | 63 ± 21 | 67 ± 18 | .76 |
| Psychosocial health summary score | Mean ± SD | 69 ± 18 | 70 ± 18 | 67 ± 19 | 72 ± 17 | .27 |
| Physical health summary score | Mean ± SD | 72 ± 21 | 72 ± 21 | 71 ± 22 | 75 ± 20 | .45 |
| Total generic score of pediatric quality of life | Mean ± SD | 70 ± 18 | 71 ± 18 | 68 ± 18 | 73 ± 16 | .27 |
| 3.0 cardiac module | ||||||
| Heart problems and treatment score | Mean ± SD | 72 ± 19 | 70 ± 20 | 73 ± 19 | 75 ± 20 | .28 |
| Treatment score | Mean ± SD | 89 ± 13 | 90 ± 14 | 88 ± 13 | 90 ± 11 | .31 |
| Perceived physical appearance score | Mean ± SD | 78 ± 23 | 78 ± 23 | 77 ± 25 | 82 ± 19 | .31 |
| Treatment anxiety score | Mean ± SD | 76 ± 26 | 76 ± 27 | 76 ± 25 | 74 ± 28 | .99 |
| Cognitive problems score | Mean ± SD | 60 ± 26 | 62 ± 26 | 57 ± 27 | 64 ± 24 | .25 |
| Communication score | Mean ± SD | 71 ± 29 | 68 ± 32 | 73 ± 28 | 76 ± 23 | .22 |
| Peds-QL—child report | n | 408 | 206 | 132 | 70 | |
| Age, years | Mean ± SD | 18.5 ± 3.4 | 18.8 ± 3.4 | 18.1 ± 3.4 | 18.7 ± 3.7 | .23 |
| 4.0 generic core scales | ||||||
| Physical functioning score | Mean ± SD | 75 ± 18 | 76 ± 18 | 73 ± 18 | 74 ± 18 | .22 |
| Emotional functioning score | Mean ± SD | 74 ± 21 | 74 ± 20 | 74 ± 21 | 72 ± 22 | .68 |
| Social functioning score | Mean ± SD | 78 ± 20 | 80 ± 18 | 76 ± 23 | 78 ± 21 | .13 |
| Total (n = 427) | Left (n = 214) | Right (n = 141) | Mixed (n = 72) | P value* | ||
| School functioning score | Mean ± SD | 70 ± 20 | 71 ± 19 | 71 ± 22 | 68 ± 19 | .71 |
| Psychosocial health summary score | Mean ± SD | 74 ± 17 | 75 ± 15 | 73 ± 19 | 73 ± 17 | .46 |
| Physical health summary score | Mean ± SD | 75 ± 18 | 76 ± 18 | 73 ± 18 | 74 ± 18 | .22 |
| Total generic score of pediatric quality of life | Mean ± SD | 74 ± 16 | 75 ± 15 | 73 ± 18 | 73 ± 17 | .29 |
| 3.0 cardiac module | ||||||
| Heart problems and treatment score | Mean ± SD | 68 ± 19 | 68 ± 19 | 70 ± 20 | 67 ± 21 | .97 |
| Treatment score | Mean ± SD | 89 ± 13 | 89 ± 14 | 92 ± 9 | 84 ± 17 | .002 |
| Perceived physical appearance score | Mean ± SD | 77 ± 24 | 77 ± 24 | 78 ± 24 | 77 ± 23 | .90 |
| Treatment anxiety score | Mean ± SD | 81 ± 24 | 81 ± 24 | 83 ± 24 | 78 ± 24 | .74 |
| Cognitive problems score | Mean ± SD | 67 ± 23 | 69 ± 22 | 65 ± 24 | 66 ± 22 | .25 |
| Communication score | Mean ± SD | 73 ± 25 | 72 ± 24 | 74 ± 27 | 73 ± 25 | .96 |
| SF-36—adult | n | 153 | 85 | 39 | 29 | |
| Age, years | Mean ± SD | 22.4 ± 1.9 | 22.3 ± 1.8 | 22.4 ± 2.3 | 22.6 ± 1.9 | .81 |
| Aggregated physical score, norm based | Mean ± SD | 50 ± 8 | 51 ± 8 | 49 ± 9 | 48 ± 8 | .11 |
| Aggregated mental score, norm based | Mean ± SD | 49 ± 12 | 51 ± 11 | 49 ± 10 | 41 ± 14 | .001 |
| Physical functioning (transformed scale) | Mean ± SD | 80 ± 20 | 84 ± 19 | 77 ± 21 | 75 ± 20 | .04 |
| Role—physical (transformed scale) | Mean ± SD | 81 ± 24 | 86 ± 21 | 80 ± 25 | 68 ± 29 | .003 |
| Bodily pain (transformed scale) | Mean ± SD | 77 ± 23 | 82 ± 19 | 78 ± 23 | 63 ± 26 | <.001 |
| General health (transformed scale) | Mean ± SD | 63 ± 22 | 64 ± 22 | 63 ± 24 | 61 ± 21 | .78 |
| Vitality (transformed scale) | Mean ± SD | 62 ± 21 | 65 ± 19 | 60 ± 25 | 54 ± 19 | .03 |
| Social functioning (transformed scale) | Mean ± SD | 81 ± 24 | 86 ± 20 | 79 ± 22 | 66 ± 31 | <.001 |
| Role—emotional (transformed scale) | Mean ± SD | 82 ± 26 | 87 ± 23 | 84 ± 21 | 67 ± 33 | <.001 |
| Mental health (transformed scale) | Mean ± SD | 73 ± 20 | 77 ± 18 | 73 ± 19 | 62 ± 22 | .002 |
| Socioeconomic status | n | 420 | 211 | 139 | 70 | |
| Hollingshead Score | Mean ± SD | 44 ± 15 | 42 ± 14 | 45 ± 14 | 47 ± 16 | .04 |
ANCOVA for means; logistic regression for percentages; Poisson regression for incidence rates; adjusted for age and sex.
Medical review and medications are also adjusted for clinical site.
Adjusted for sex only.
Adjusted for age only.
ACE, angiotensin-converting enzyme; BMI, body mass index; cath, cardiac catheterization; CHQ-CF87, Child Report Child Health Questionnaire; CHQ-PF50, Parent Report Child Health Questionnaire; IED, implanted electronic device; NYHA, New York Heart Association Heart Failure Class; Peds-QL, The Pediatric Quality of Life Inventory; SD, standard deviation; SF-36, Short-Form Health Survey version 2. P values <0.05 noted in bold font.
Association with Age
Younger subjects (<18 years, n = 225) were less likely to have suffered from stroke both since their Fontan procedure and in the interim between Fontan 1 and Fontan 2. Interim development of thrombosis since Fontan 1 was more likely in the older (≥18 years, n = 202) cohort. Younger subjects were more likely to be prescribed ACE inhibitors. For the Peds-QL that included all ages, only the treatment scale differed, being better among the younger cohort.
Because the CHQ is validated only in children ≤19 years old, we compared results of these tests between a younger group of 120 subjects <16 years and an older group of 144 subjects 16–19 years old. The mental health, self-esteem, and general health perception scales were higher (better) among the younger group as reported by both the subjects and their parents. We also compared a younger adult group comprising 76 adult subjects 19 to <22.5 years with an older group of 77 subjects ≥22.5 years. No differences were seen in any of the 10 reported scales of the SF-36 (Table 2).
Table 2.
Associations with Age
| Younger (Age < 18) | Older (Age > 18) | P Value* | ||
|---|---|---|---|---|
| Medical review from Fontan 1 to Fontan 2 | n = 212 | n = 214 | ||
| Follow-up time, years | Mean ± SD | 6.8 ± 0.4 | 6.9 ± 0.5 | .32 |
| Cardiac surgical procedure | n (%) | 29 (14%) | 37 (17%) | .36 |
| Cardiac cath intervention | n (%) | 38 (18%) | 40 (19%) | .88 |
| Stroke | n (%) | 0 (0%) | 3 (1%) | .04 |
| Seizure | n (%) | 4 (2%) | 11 (5%) | .07 |
| Thrombosis | n (%) | 2 (1%) | 12 (6%) | .005 |
| Arrhythmia | n (%) | 26 (12%) | 42 (20%) | .06 |
| Other important complications | n (%) | 74 (35%) | 84 (39%) | .49 |
| On heart transplant waiting list | n (%) | 0 (0%) | 1 (1%) | .99 |
| IED in place | n (%) | 22 (10%) | 34 (16%) | .11 |
| Medical review since Fontan surgery | n = 212 | n = 214 | ||
| Follow-up time, years | Mean ± SD | 12.8 ± 1.7 | 17.8 ± 2.8 | <.001 |
| PLE | n (%) | 13 (6%) | 17 (8%) | .85 |
| Cirrhosis | n (%) | 3 (1%) | 12 (6%) | .07 |
| Plastic bronchitis | n (%) | 1 (0.5%) | 1 (0.5%) | .81 |
| Clinical assessment | n = 216 | n = 210 | ||
| Percentile height for age | Mean ± SD | 36 ± 31 | 40 ± 30 | .32 |
| Height-for-age z-score | Mean ± SD | −0.7 ± 1.5 | −0.5 ± 1.2 | .27 |
| Percentile weight for age | Mean ± SD | 45 ± 34 | 46 ± 34 | .72 |
| Weight-for-age z-score | Mean ± SD | −0.4 ± 1.6 | −0.2 ± 1.6 | .55 |
| BMI-for-age z-score | Mean ± SD | 0.0 ± 1.3 | 0.0 ± 1.3 | .94 |
| NYHA heart failure classification | n (%) | .25 | ||
| Class I | 123 (57%) | 111 (53%) | ||
| Class II | 63 (30%) | 56 (27%) | ||
| Class III | 22 (10%) | 27 (13%) | ||
| Class IV | 8 (4%) | 16 (7%) | ||
| Number of medications | n (%) | .22 | ||
| 0 | 18 (8%) | 27 (13%) | ||
| 1 | 55 (25%) | 44 (21%) | ||
| ≥2 | 145 (67%) | 137 (66%) | ||
| ACE inhibitors | n (%) | 127 (58%) | 99 (48%) | .03 |
| Peds-QL—subject report | n = 207 | n = 201 | ||
| 4.0 generic core scales | ||||
| Physical functioning score | Mean ± SD | 76 ± 17 | 73 ± 20 | .16 |
| Emotional functioning score | Mean ± SD | 74 ± 20 | 73 ± 21 | .51 |
| Social functioning score | Mean ± SD | 78 ± 20 | 78 ± 21 | .94 |
| School functioning score | Mean ± SD | 70 ± 19 | 71 ± 21 | .85 |
| Psychosocial health summary score | Mean ± SD | 74 ± 16 | 74 ± 18 | .74 |
| Physical health summary score | Mean ± SD | 76 ± 17 | 73 ± 20 | .16 |
| Total generic score of pediatric quality of life | Mean ± SD | 75 ± 15 | 74 ± 17 | .41 |
| 3.0 cardiac module | ||||
| Heart problems and treatment score | Mean ± SD | 70 ± 19 | 66 ± 20 | .06 |
| Treatment score | Mean ± SD | 91 ± 11 | 87 ± 15 | .001 |
| Perceived physical appearance score | Mean ± SD | 79 ± 22 | 75 ± 26 | .13 |
| Treatment anxiety score | Mean ± SD | 81 ± 24 | 81 ± 24 | .86 |
| Cognitive problems score | Mean ± SD | 69 ± 22 | 65 ± 24 | .08 |
| Communication score | Mean ± SD | 73 ± 24 | 72 ± 26 | .65 |
| Socioeconomic status | n = 214 | n = 206 | ||
| Hollingshead score | Mean ± SD | 45 ± 14 | 43 ± 15 | .19 |
| Median (IQR) | 47 (35, 56) | 45 (33, 55) | .19 | |
ANOVA for means; Fisher’s exact test for frequencies.
ACE, angiotensin-converting enzyme; BMI, body mass index; cath, cardiac catheterization; IED, implanted electronic device; IQR, interquartile range; NYHA, New York Heart Association Heart Failure Class; Peds-QL, The Pediatric Quality of Life Inventory; PLE, protein-losing enteropathy; SD, standard deviation. P values <0.05 noted in bold font.
Association with Fontan Type
Fontan procedure types included atriopulmonary connection (APC, n = 54), total cavopulmonary connection intracardiac lateral tunnel (LT, n = 251), and total cavopulmonary connection extracardiac conduit (ECC, n = 111). After adjustment for age, subjects with an APC were less likely to have had a cardiac catheter based intervention since the Fontan procedure (31% APC vs. 59% LT vs. 65% ECC), P = .004. However, catheter interventions since Fontan 1 were not different between groups, P = .4. The incidence of arrhythmia since the Fontan procedure was higher in APC subjects (44% APC vs. 28% LT vs. 19% ECC), but this was not significant after accounting for age, P = .4. However, the development of new arrhythmia requiring treatment in the interim period between Fontan 1 and Fontan 2 was significantly higher in APC subjects even after accounting for age (30% APC vs. 16% LT vs. 10% ECC), P = .049.
Characteristics of Health Care
There was a significant difference between sites for the frequency of a secondary source of insurance (P < .001). The rate was much higher for Canadian subjects (79%) than for those from US sites (10–26%). The vast majority of subjects (96%) have visited a cardiologist within the past 2 years. We compared 295 subjects with a visit frequency of ≤1 visit per year with 125 subjects with ≥2 visits per year. In multivariable modeling, the only associated factor for more frequent visits was clinical site (P < .001, R2 = 0.10). The most prevalent medical services reported by subjects were dental care (92%), ophthalmology (62%), educational support (36%), gynecology (32% of the females), mental health (19%), and dermatology and neurology (15% each) (Table 3).
Table 3.
Characteristics of Health Care
| n (%) | |
|---|---|
| Health insurance (n = 420) | |
| Yes | 406 (97%) |
| No | 14 (3%) |
| Primary insurance type (n = 406) | |
| Private | 214 (53%) |
| Public | 192 (47%) |
| Secondary source of health insurance (n = 405) | |
| Yes | 134 (33%) |
| No | 271 (67%) |
| Visited a cardiologist in the past 2 years (n = 420) | |
| Yes | 404 (96%) |
| No | 16 (4%) |
| Frequency of cardiologist visits (n = 404) | |
| Less than once a year | 41 (10%) |
| Once a year | 238 (59%) |
| Twice a year | 85 (21%) |
| More than twice a year | 40 (10%) |
| Visited an adult cardiologist in the past 2 years* (n = 284) | |
| Yes | 86 (30%) |
| No | 198 (70%) |
| Medical services received in the past 2 years (n = 420) | |
| Dental care | 385 (92%) |
| Ophthalmology | 261 (62%) |
| Education support | 150 (36%) |
| Obstetrician/gynecologist (n = 203)† | 64 (32%) |
| Mental health | 80 (19%) |
| Dermatology | 64 (15%) |
| Neurology | 61 (15%) |
| Orthopedic | 59 (14%) |
| Rehabilitation/physical therapy | 56 (13%) |
| Otolaryngology | 43 (10%) |
| Pulmonology | 42 (10%) |
| Occupational therapy | 37 (9%) |
| Speech therapy | 37 (9%) |
| Endocrine | 27 (6%) |
| Nutrition | 27 (6%) |
| Allergy services | 26 (6%) |
| Renal | 18 (4%) |
| Any other | 70 (17%) |
Question only asked of subjects ≥16 years.
Question only asked of female subjects.
Discussion
Longitudinal studies that involve children with chronic diseases transitioning to adulthood are uncommon. This is the largest report of a prospectively followed multicenter cohort of children with univentricular physiology palliated with a Fontan procedure. We found that only 2% were lost to follow-up and 83% of the original cohort were willing to participate. Older patients and males were less likely to agree to participate. This is consistent with challenges that are faced in the transition of clinical care from pediatric cardiologists to adult congenital heart disease specialists.14
We found 95% interim transplant-free survival over an average of 7 years of follow-up since enrollment in the Fontan 1 study. Those with poorer results during the baseline assessment at Fontan 1 were more likely to have died or be transplanted. Specifically, we found death or transplant to be associated with worse performance on previously administered CHQ-PF50 physical summary score, a more dilated ventricle as measured by echocardiography, and higher measured BNP assessed at Fontan 1. Previous studies examining vital status over time for Fontan survivors and predictors of death or transplant have been limited to single center reports that span large time periods (e.g., 25 years)15 or have included a much shorter length of follow-up (e.g., <2years).16 Our data show a slightly lower incidence of death and transplant than a previous study of 321 surviving Fontan subjects with a mean age of 21 years.16
There have been concerns that patients with a Fontan circulation are destined to have an increasing risk over time for death or heart transplantation17 as well as a decline in ventricular performance and health status.18 Rates of decline have been speculated to be greater among those with dominant RV morphology.19,20 We did not find RV dominant subjects to have a greater likelihood of death or transplant over the period of study. This is in contrast to a cohort of earlier era Fontan subjects born before 1985 and followed for a median of 12 years in whom a 10-fold risk of heart failure death was seen in those with a morphologic RV.15 We did find an increase in the use of ACE inhibitors in both younger subjects and those with a dominant RV. We speculate this is a difference in practice patterns that exists despite the lack of evidence to suggest benefit.21 Although no important differences in quality of life or functional health status were related to ventricular dominance among the children in our study, we did find higher (better) scores in 8 of 10 scales from the SF-36 among the adults with left ventricular dominance.
The strength of this current study is its uniform median follow-up period for all subjects. This allowed us to compare outcomes since the Fontan completion (median 15 ± 3.4 years) as well as in the interim since Fontan 1 (6.8 ± 0.4 years). Subjects with an APC type of Fontan had fewer interventional catheter procedures between Fontan completion and Fontan 1 assessment compared with other Fontan types, a difference that was not observed in the interim period since assessment at Fontan 1. This is likely due to a much higher rate of surgical fenestration in non-APC Fontan types with planned procedures to close these in the first year or so after Fontan surgery.22 We were able to confirm previous reports that ongoing risk of development of arrhythmia is greater among subjects with an APC compared with other Fontan types.23
Quality-of-life studies complement mortality and morbidity data by taking physical, psychological, and social factors into consideration.24 Although the mean CHQ-PF50 physical summary score was lower than those of healthy control subjects, a large majority of adolescent subjects (as reported by a parent) continue to score within the normal range. Comparisons among adults in our cohort evaluated by the SF-36 reveal even fewer differences compared with self-reported historic norms. These results may be explained by coping mechanisms in the adult subjects resulting in a higher appreciation of health status, which is exemplified by higher scores.25 This may also reflect the known discordance when comparing parent-completed surveys to subject-completed surveys.26
Because of the nature of this observational cohort, we cannot exclude the possibility that the lowest performing subjects are less likely to survive with a Fontan circulation into adulthood.
A significant limitation illustrated in our study is that instruments to study functional health outcomes are validated only for specific age groups. There is not a single instrument that includes the full age range of subjects who are transitioning from the teenage years to adulthood. The CHQ produces scores for 14 domains and two summary scores (physical functioning and psychosocial functioning). Our results for the mean physical summary score for Fontan subjects (44 ± 12) are similar to those subjects with asthma (48 ± 7), juvenile rheumatoid arthritis (42 ± 14), and epilepsy (48 ± 14). The same is true for the psychosocial summary scores, 48 ± 12 in our Fontan group, asthma (52 ± 8), epilepsy (47 ± 12), and attention deficit disorder (37 ± 11).13 The SF-36 is a multipurpose, 36-item adult health survey that yields an 8-scale profile of functional health and well-being scores as well as psychometrically based physical and mental health summary measures. The results of our cohort of adult subjects showed similar scores when compared with a recent study involving 54 Danish subjects with a Fontan circulation.27 A recent systematic review of quality-of-life studies in adult congenital heart disease patients suggests that, in general, quality of life is compromised in the physical domains compared with norms and less so in relation to psychosocial and environmental/occupational domains.28 These findings are supported by our results. Correlations are needed between individual instruments that assess functional health status and quality of life across the transition from child to adult.
The results of this study must be viewed in light of certain limitations. The original Fontan 1 cohort was by necessity a subset of Fontan survivors. The time frame between Fontan 1 and 2 may have been a period of relative clinical stability and too short to observe meaningful changes in functional health status and medical conditions. As stated previously, there are no measurements of functional health status, which are validated across the full age range of the subjects being studied. Comparisons between younger and older groups of subjects divided the cohort into similar-sized groups. If this separation was made in different ways, our findings related to age might be different. The present study was limited to assessment of functional health status and interim medical history. Our assessment was also restricted to the 85% of eligible Fontan 1 survivors who agreed to participate in this follow-up study. Repeat laboratory testing and comparisons of these measures over time, which were not assessed at Fontan 2, will be the subject of future research.
This is the largest report of a prospectively followed multicenter cohort of children with univentricular physiology palliated with a Fontan procedure and provides a contemporary overview of vital status, functional health status, and interim medical history in current survivors of the Fontan procedure. Incidence of death or transplantation is low and associated with prior poor functional health status and certain measures of ventricular performance. Functional health status was within normal range in the majority of subjects. Data from this study will permit useful comparisons with the data from single ventricle subjects being followed prospectively from birth in other studies. Continued longitudinal investigation into adulthood is necessary to better understand these patients and improve their long-term outcomes and functional health status.
Acknowledgments
The authors would like to thank the following:
National Heart, Lung, and Blood Institute: Gail Pearson, Mario Stylianou, Jonathan Kaltman, Victoria Pemberton
Data Coordinating Center: New England Research Institutes, Lynn Sleeper, Steven Colan, Dianne Gallagher, Victor Zak, Peter Shrader
Protocol Chair: Lynn Mahony, University of Texas Southwestern Medical Center
Clinical Site Investigators: Children’s Hospital Boston, Jane Newburger (Principal Investigator), Roger Breitbart, Carolyn Dunbar-Masterson, Jill Handisides, Lisa-Jean Buckley, Bethany Trainor; Children’s Hospital of New York, Wyman W. Lai (Principal Investigator), Rosalind Korsin; Children’s Hospital of Philadelphia, Robert Shaddy, J William Gaynor, Stephen M Paridon, (Principal Investigators), Kaitlyn Daniels, Tonia Morrison, Nicole Mirarchi*;Duke University, Jennifer S. Li (Principal Investigator), Piers Barker, Mingfen Xu; Medical University of South Carolina, J. Philip Saul (Principal Investigator), Andrew M. Atz, Patricia Infinger, Ann Harvey Frampton; Primary Children’s Medical Center, Salt Lake City, Utah, LuAnn Minich (Principal Investigator), Richard Williams, Linda Lambert; Hospital for Sick Children, Toronto, Brian McCrindle (Principal Investigator), Elizabeth Radojewski, Svetlana Khaikin, Patricia Walter; Cincinnati Children’s Medical Center, Bradley Marino, Karen Uzark*.
Protocol Review Committee: Michael Artman, Chair; Timothy Feltes, Julie Johnson*, Jeffrey Krischer, G. Paul Matherne, Nakela Cook*
Data and Safety Monitoring Board: John Kugler, Chair; David Gordon, David J. Driscoll, Mark Galantowicz, Sally A. Hunsberger, Holly Taylor, Thomas J. Knight, Catherine L. Webb*.
Funding: Supported by U01 grants from the National Heart, Lung, and Blood Institute (HL068269, HL068270, HL068279, HL068281, HL068285, HL068292, HL068290, HL068288).
Footnotes
No longer at the institution listed.
Authors’ Contributions
Andrew M. Atz, MD: Concept/design, data analysis/ interpretation, drafting article, critical revision of article, approval of article, data collection.
Victor Zak, PhD: Concept/design, data analysis/ interpretation, drafting article, statistics, critical revision of article, approval of article.
Lynn Mahony, MD: Concept/design, critical revision of article, approval of article.
Karen Uzark, PhD: Concept/design, data interpretation, critical revision of article, approval of article.
Peter Shrader, MA: Data analysis/interpretation, drafting article, statistics, critical revision of article, approval of article.
Dianne Gallagher, MS: Concept/design, data analysis/ interpretation, data collection, critical revision of article, approval of article.
Stephen M. Paridon, MD: Concept/design, data interpretation, critical revision of article, approval of article.
Richard V. Williams, MD: Concept/design, data interpretation, critical revision of article, approval of article.
Roger E. Breitbart, MD: Concept/design, data interpretation, critical revision of article, approval of article.
Steven D. Colan, MD: Concept/design, data analysis/ interpretation, critical revision of article, approval of article.
Jonathan R. Kaltman, MD: Concept/design, data analysis/ interpretation, critical revision of article, approval of article.
Renee Margossian, MD: Concept/design, data analysis/ interpretation, critical revision of article, approval of article.
Sara K. Pasquali, MD, MHS: Data analysis/interpretation, critical revision of article, approval of article.
Kerstin Allen, MS: Concept/design, data analysis/ interpretation, critical revision of article, approval of article.
Wyman W. Lai, MD, MPH: Concept/design, data interpretation, critical revision of article, approval of article.
Rosalind Korsin, RN: Concept/design, critical revision of article, data collection, approval of article.
Bradley S. Marino, MD: Concept/design, data analysis/ interpretation, critical revision of article, approval of article.
Nicole Mirarchi, RN: Concept/design, data collection, critical revision of article, approval of article.
Brian W. McCrindle, MD, MPH: Concept/design, data analysis/interpretation, drafting article, critical revision of article, approval of article.
Conflict of interest: None.
This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health/ National Heart, Lung, and Blood Institute.
Clinical Trials Registration number: NCT00132782
No relationship with industry exists.
References
- 1.Mahle WT, Wernovsky G, Bridges ND, Linton AB, Paridon SM. Impact of early ventricular unloading on exercise performance in preadolescents with single ventricle Fontan physiology. J Am Coll Cardiol. 1999;34 (5):1637–1643. doi: 10.1016/s0735-1097(99)00392-7. [DOI] [PubMed] [Google Scholar]
- 2.Rosenthal DN, Friedman AH, Kleinman CS, Kopf GS, Rosenfeld LE, Hellenbrand WE. Thromboembolic complications after Fontan operations. Circulation. 1995;92(9 Suppl):II287–II293. doi: 10.1161/01.cir.92.9.287. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch JC, Goldberg C, Bove EL, et al. Fontan operation in the current era: a 15-year single institution experience. Ann Surg. 2008;248 (3):402–410. doi: 10.1097/SLA.0b013e3181858286. [DOI] [PubMed] [Google Scholar]
- 4.Rychik J. Protein-losing enteropathy after Fontan operation. Congenit Heart Dis. 2007;2 (5):288–300. doi: 10.1111/j.1747-0803.2007.00116.x. [DOI] [PubMed] [Google Scholar]
- 5.Hellstedt LF. Insurability issues facing the adolescent and adult with congenital heart disease. Nurs Clin North Am. 1994;29 (2):331–343. [PubMed] [Google Scholar]
- 6.Reid GJ, Irvine MJ, McCrindle BW, et al. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113 (3 pt 1):e197–e205. doi: 10.1542/peds.113.3.e197. [DOI] [PubMed] [Google Scholar]
- 7.Marino BS. Outcomes after the Fontan procedure. Curr Opin Pediatr. 2002;14 (5):620–626. doi: 10.1097/00008480-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 8.McCrindle BW, Williams RV, Mitchell PD, et al. Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation. 2006;113 (8):1123–1129. doi: 10.1161/CIRCULATIONAHA.105.576660. [DOI] [PubMed] [Google Scholar]
- 9.Anderson PA, Sleeper LA, Mahony L, et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. J Am Coll Cardiol. 2008;52 (2):85–98. doi: 10.1016/j.jacc.2008.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner-Bowker DM, Bartley PJ, Ware JE. SF-36 Health Survey & SF Bibliography: Third Edition (1988–2000) Lincoln, RI: QualityMetric Incorporated; 2002. [Google Scholar]
- 11.Varni JW, Burwinkle TM, Rapoff MA, Kamps JL, Olson N. The PedsQL in pediatric asthma: reliability and validity of the Pediatric Quality of Life Inventory generic core scales and asthma module. J Behav Med. 2004;27 (3):297–318. doi: 10.1023/b:jobm.0000028500.53608.2c. [DOI] [PubMed] [Google Scholar]
- 12.Varni JW, Seid M, Knight TS, Uzark K, Szer IS. The PedsQL 4.0 Generic Core Scales: sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med. 2002;25 (2):175–193. doi: 10.1023/a:1014836921812. [DOI] [PubMed] [Google Scholar]
- 13.Landgraf JM, Abetz L, Ware JE. The CHQ User’s Manual. Second Printing. Boston, MA: Health Act; 1999. [Google Scholar]
- 14.Goossens E, Stephani I, Hilderson D, et al. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: an analysis of transfer destinations. J Am Coll Cardiol. 2011;57 (23):2368–2374. doi: 10.1016/j.jacc.2010.11.068. [DOI] [PubMed] [Google Scholar]
- 15.Khairy P, Fernandes SM, Mayer JE, Jr, et al. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation. 2008;117 (1):85–92. doi: 10.1161/CIRCULATIONAHA.107.738559. [DOI] [PubMed] [Google Scholar]
- 16.Diller GP, Giardini A, Dimopoulos K, et al. Predictors of morbidity and mortality in contemporary Fontan patients: results from a multicenter study including cardiopulmonary exercise testing in 321 patients. Eur Heart J. 2010;31 (24):3073–3083. doi: 10.1093/eurheartj/ehq356. [DOI] [PubMed] [Google Scholar]
- 17.D’Udekem Y, Iyengar AJ, Cochrane AD, et al. The Fontan procedure: contemporary techniques have improved long-term outcomes. Circulation. 2007;116 (11 Suppl):I157–I164. doi: 10.1161/CIRCULATIONAHA.106.676445. [DOI] [PubMed] [Google Scholar]
- 18.Paridon SM, Mitchell PD, Colan SD, et al. A cross-sectional study of exercise performance during the first 2 decades of life after the Fontan operation. J Am Coll Cardiol. 2008;52 (2):99–107. doi: 10.1016/j.jacc.2008.02.081. [DOI] [PubMed] [Google Scholar]
- 19.Giardini A, Hager A, Pace NC, Picchio FM. Natural history of exercise capacity after the Fontan operation: a longitudinal study. Ann Thorac Surg. 2008;85 (3):818–821. doi: 10.1016/j.athoracsur.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 20.Trojnarska O, Gwizdala A, Katarzynski S, et al. Evaluation of exercise capacity with cardiopulmonary exercise test and B-type natriuretic peptide in adults with congenital heart disease. Cardiol J. 2009;16 (2):133–141. [PubMed] [Google Scholar]
- 21.Anderson PA, Breitbart RE, McCrindle BW, et al. The Fontan patient: inconsistencies in medication therapy across seven pediatric heart network centers. Pediatr Cardiol. 2010;31 (8):1219–1228. doi: 10.1007/s00246-010-9807-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atz AM, Travison TG, McCrindle BW, et al. Late status of Fontan patients with persistent surgical fenestration. J Am Coll Cardiol. 2011;57 (24):2437–2443. doi: 10.1016/j.jacc.2011.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gatzoulis MA, Munk MD, Williams WG, Webb GD. Definitive palliation with cavopulmonary or aortopulmonary shunts for adults with single ventricle physiology. Heart. 2000;83 (1):51–57. doi: 10.1136/heart.83.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moons P, Van DK, De GS, Gewillig M, Budts W. Is the severity of congenital heart disease associated with the quality of life and perceived health of adult patients? Heart. 2005;91 (9):1193–1198. doi: 10.1136/hrt.2004.042234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fekkes M, Kamphuis RP, Ottenkamp J, et al. Health-related quality of life in young adults with minor congenital heart disease. Psychol Health. 2001;16:239–250. [Google Scholar]
- 26.Lambert LM, Minich LL, Newburger JW, et al. Parent- vs. child-reported functional health status after the Fontan procedure. Pediatrics. 2009;124 (5):e942–e949. doi: 10.1542/peds.2008-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Idorn L, Jensen AS, Juul K, et al. Quality of life and cognitive function in Fontan patients, a population-based study. Int J Cardiol. 2013;168 (4):3230–3235. doi: 10.1016/j.ijcard.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 28.Fteropoulli T, Stygall J, Cullen S, Deanfield J, Newman SP. Quality of life of adult congenital heart disease patients: a systematic review of the literature. Cardiol Young. 2013;23 (4):473–485. doi: 10.1017/S1047951112002351. [DOI] [PubMed] [Google Scholar]