Abstract
Purpose
People with tetraplegia face substantial physical and financial hardships. Although upper-extremity reconstruction has been advocated for people with tetraplegia, these procedures are markedly underutilized in the United States. Population-based preference evaluation of upper-extremity reconstruction is important to quantify the value of these reconstructive procedures. This study sought to establish the preferences for three health states: tetraplegia, tetraplegia with corrected pinch function, and tetraplegia with corrected elbow extension function.
Methods
A computer-based time trade-off survey was administered to a cohort of 81 able-bodied second-year medical students who served as a surrogate for “the general public.” This survey instrument has undergone pilot testing and has established face validity to evaluate the three health states of interest. Utilities were calculated based on an estimated 20 years of remaining life.
Results
The mean utility for the tetraplegic health state was low. On average, respondents gave up 10.8 ± 5.0 out of a hypothetical 20 years for perfect health, for a utility of tetraplegia equal to 0.46. For recovery of pinch function, respondents gave up an average of 6.5 ± 4.3 years, with a corresponding health utility of 0.68. For recovery of elbow extension function, respondents gave up an average of 7.6 ± 4.5 years, with a corresponding health utility of 0.74.
Conclusions
This study established the preferences for two upper-extremity surgical interventions: tetraplegia with pinch and tetraplegia with elbow extension. The findings from this study place a high value on upper limb reconstructive procedures with tetraplegia.
Keywords: Health utilities, upper extremity reconstruction, tetraplegia, economic model
In the United States, there are over 100,000 people living with tetraplegia (1, 2). Individuals with this condition cope with physical hardships that are often exacerbated by financial difficulties. The economic burden of tetraplegia is substantial; estimates of the direct lifetime cost for a person injured at age 25 ranges from $1.7–$3.0 million (2). Rehabilitation for people with tetraplegia focuses upon improving the patient’s ability to perform activities of daily living (ADL), which both enhances independence and lessens the cost-burden on society.
People with tetraplegia struggle to gain independence so an important goal for rehabilitation is to improve lost upper limb function (3). Tendon transfer procedures have been shown to restore basic upper limb movements (4); however, these procedures are markedly underutilized, and few patients actually receive optimum intervention (5). Although the majority of clinicians believe that upper extremity function is vital for this patient population, physician preconceptions and a lack of cross-specialty relationships appear to contribute to the underuse of these procedures (4, 6). The disparity in care has been shown for this vulnerable population, but one critical piece of information has been missing: How valuable is pinch and elbow extension function in the setting of tetraplegia?
To answer this question, preferences must be obtained and converted to discrete values using a health utility assessment. The utility score is measured as a single number that is expressed along a continuum extending from death (0.0) to perfect health (1.0) (7). It provides an aggregate value of the net change in health-related quality of life – the gains and losses of morbidity and mortality experienced with a particular intervention (8, 9). The utility measure has many advantages that make it a favorable econometric tool. First, it combines the positive and negative aspects of a health outcome into a single numerical value. Second, it reflects two important dimensions of a health state: duration and quality. These attributes allow the utility score to be expressed as an output known as quality-adjusted life years (QALYs), which can be incorporated into economic evaluations (10).
Until now, population-preferences for upper extremity reconstruction in individuals with tetraplegia were unknown. The aim of our study is to establish the health preferences for the essential upper limb movements, namely pinch and elbow extension by using utility measures. This will provide a quantifiable value for limb functions that can be used for comparison with other interventions such as improvement of bowel and bladder function. In addition, these values can be incorporated into economic analyses of different rehabilitative options for this patient population (8). Ultimately, this information can be weighed against utility values obtained for other health state interventions (for example, medically managing cirrhosis) to assist with prioritization of resources for this population’s complex rehabilitative needs.
Methods
Survey Design
The purpose of our survey was to determine the health utility scores for three health states in the tetraplegia condition. The first health state is the global tetraplegia state, which was described as a spinal cord injury that affects function of both arms and legs. The second health state is tetraplegia with corrected pinch function that would permit handling of items such as an ATM card or a fork. Finally, we asked about tetraplegia with corrected elbow extension function that would improve one’s ability to stabilize the arm in space to assist with eating, brushing hair, and reaching above the head. The questions were designed to represent the average results after upper extremity reconstructive procedures as demonstrated by a systematic review of the literature; we also solicited the viewpoint of an occupational therapist specializing in the care of people with tetraplegia to craft realistic scenarios for the utility survey (11).
To obtain utilities for these health states, we used the time trade-off method (TTO) (12). In this method, subjects express the number of years they would give up to live in a better health state. Because the TTO portrays scenarios without the consideration of gamble, the TTO utility is more of a value score and tends to be lower than the utility score obtained from ‘standard gamble’ for the same health state (13, 14). The first question involved choosing to live 20 years with tetraplegia with no function of all four limbs, or living fewer years with perfect health. The second question involved choosing to live 20 years with tetraplegia or choosing to live for a shorter period of time with surgically corrected pinch function. The third question involved choosing to live 20 years with tetraplegia or choosing to live for a shorter time with surgically corrected ability to extend the arm at the elbow.
Twenty years of life expectancy was chosen because we felt this represented the average life expectancy of the average person with tetraplegia. We arrived at the twenty years life expectancy after considering three factors. First, the average life expectancy for a person with tetraplegia after injury is about 35 years (15). Next, 40% of the U.S. population of individuals with spinal cord injuries is over the age of 45. Finally, many people with tetraplegia have long standing injuries, with 25% of this population more than 20 years out from his or her time of injury (16). Considering that this unique demographic is an older population with longstanding injuries and slightly shortened life expectancy, we decided that 20 years would be a close representation of the predicted life expectancy of the average person with tetraplegia in the US.
To establish the face validity and comprehension of the questionnaire, we pilot tested the survey on three heterogeneous groups of individuals: medical students, people with tetraplegia, and attending physicians. We had our respondents read the questions aloud using a concurrent think aloud technique to assure comprehension and then took feedback for content changes (17). Based upon the feedback from the pilot test, three rounds of major revisions were performed before the survey was deemed ready for administration.
The thirteen-item survey instrument was administered online via the ‘UM.Lessons’ survey engine, which was used in the past for establishing utilities for scaphoid fracture treatment (18). Computer based tools that use time trade-off to assess health states have been found to give comparable results as face-to-face interviews (19).
During the computer survey, we asked subjects demographic information and questions about general upper extremity health. Next, they completed a generic health-related quality of life measure, the Health Utility Index-3 (HUI-3) (20). The HUI-3 is a general health related quality of life measure that encompasses eight attributes (vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain). It has been extensively tested in the community and for a wide variety of health states (21). The HUI-3 ratings provide a value to each subject’s health status at the time of the survey and generate a reference for how this study population compares to the general community.
The time trade-off questions were administered in an iterative fashion and began with two practice questions to assure that the respondent comprehended the TTO technique. The first test question addressed binocular blindness and the second monocular blindness. Respondents who comprehend the survey should give up more time to cure blindness in both eyes than blindness in only one eye.
The final question of the survey addressed the inconvenience associated with post-operative casting. Our discussions with hand surgeons involved in tetraplegia reconstruction suggested that patients may be concerned about loss of independence with casting, which might contribute to the underutilization of these procedures.
Study Subjects
The Institutional Review board at the authors’ academic university approved the study protocol. The objective of the survey was to ascertain community-based preferences, as opposed to patient-based preferences, for a range of health states as recommended by The Panel on Cost Effectiveness in Health and Medicine (22, 23). A sample of 150 first- and second-year medical students was chosen for the study from a total of 350 students. A random sequence generator was used for selection of the participants. Initial recruitment began with an email briefly explaining participation and a $20 payment as a token for their time. Two additional email reminders were sent to the selected group with the informed consent document attached. Once interest was acknowledged and consent was obtained, the internet address for the survey engine was provided. The surveys were anonymous. One hundred eighteen medical students of the 150 emailed responded to our recruitment email and submitted a survey. Out of this 118, 81 subjects produced fully completed and logically sound surveys which were subsequently used for analysis. These data were used as a proxy for able-bodied preferences (18). The final sample was 81 medical students.
Data Analysis
Data were downloaded from the UM.Lessons survey engine and calculations were performed to determine utility scores, including the mean value for each scenario and standard deviations for each outcome studied.
Utility Calculations
The TTO method determines the utility of various health states by comparing living longer in less-than-perfect health versus a specified shorter but perfectly healthy life. For example, a respondent who feels that 6 years of life without tetraplegia (giving up 4 years) is equal to 10 years with tetraplegia, means the utility of the tetraplegia health state would be 0.6. (Below is the calculation for utility scores, Calculation 1).
Calculation 1
U = Utility
LE = Life expectancy with health state in question
Y = Number of years given up for perfect health
For the specific health states in tetraplegia regarding both grip and pinch function, both utilities were calculated and then averaged(Calculation 2).
Calculation 2
U(s) = Utility of tetraplegia with one particular upper extremity deficit surgically corrected
N = Number of years the subject is willing to trade for cure of the impairment
U(t) = Utility of the tetraplegic health state.
Results
Survey Response
A total of 118 of the 150 medical students submitted surveys. Of these 118 data sets, 37 were excluded due to missing data and logical inconsistencies. Therefore, 81 surveys were ultimately included in the final analysis. The final cohort consisted of 37 males (46%), 44 females (54%). The initial response rate was 78% with 69% of the returned surveys used in the final analysis. The age of respondents ranged from 21–30, with an average age being 23.2 years and standard deviation of 1.7. All respondents answered the practice questions concerning hypothetical monocular and binocular vision loss correctly, which gives confidence that all the responders understood the TTO strategy.
The mean summary score for the HUI-3 scores for this study sample was 0.9. According to the Institute of Medicine, the average HUI-3 for a healthy 20–29 year-old living in the United States was 0.91(22). Based on this standard, our participants had a very high health related quality of life (0.88 with 1.0 meaning perfect health) and thus represent a healthy control group (20).
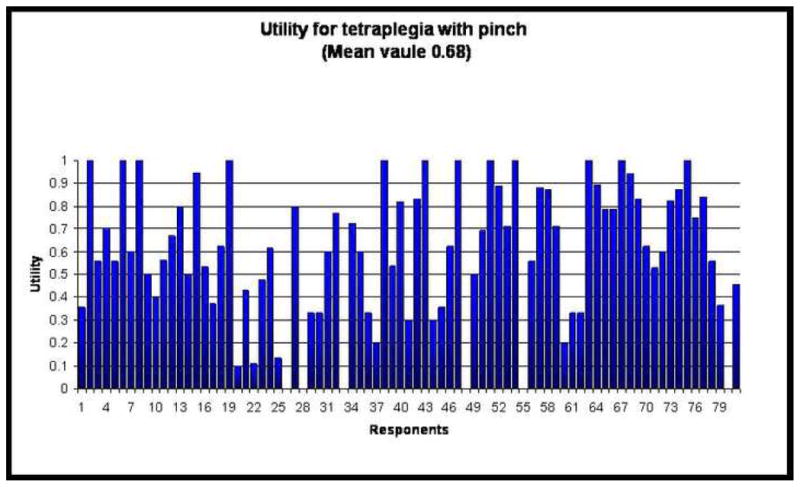
For the first health state, the utility of tetraplegia, the respondents traded a mean of 10.8 ± 5.0 years out of a hypothetical 20 years to gain perfect health. This means that the utility for tetraplegia was very low at 0.46. The utility scores for tetraplegia are presented in Figure 1. For restoration of pinch function, respondents gave up an average of 6.5 years ± 4.3, years, with a corresponding health utility of 0.68. Figure 2 graphs the utility scores for pinch. For elbow extension function, the respondents gave up an average of 7.6 years ± 4.5 years, with a corresponding health utility of 0.74. Figure 3 presents the utility scores for elbow extension. Blank spaces in our figures indicate a preference score of ‘0’ or death. In other words, some subjects felt that death is preferable to living with tetraplegia, in some cases, even with restored upper extremity function.
Figure 1.
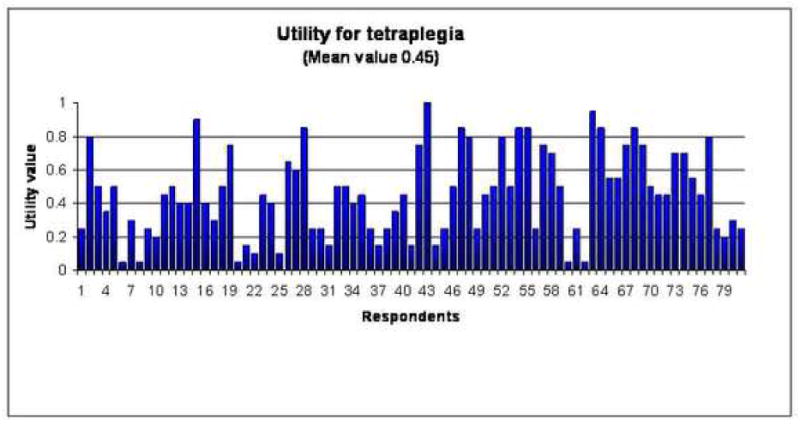
Health Preferences for Tetraplegia
Figure 2.
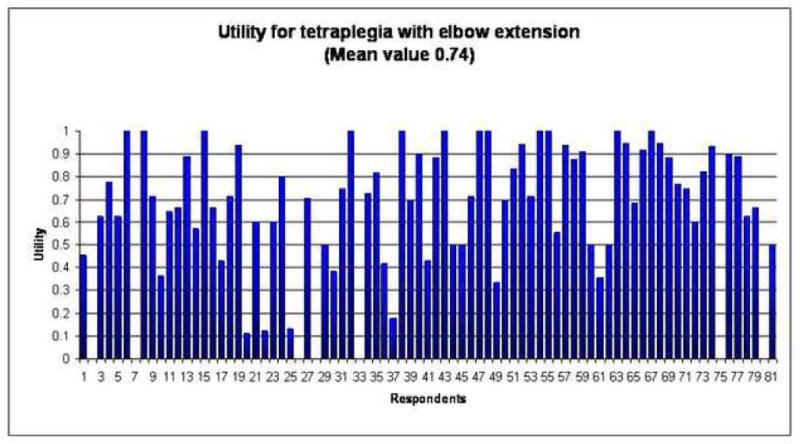
Health Preferences for Tetraplegia with Restored Grip
Figure 3.
Health Preferences for Tetraplegia with Restored Elbow Extension
Finally, we asked the survey respondents to indicate how many weeks they would tolerate in a cast after surgery to improve upper extremity function (from 0 weeks up to 8 weeks). Two participants preferred to decline surgery rather than be casted longer than four weeks; all others indicated that they would be willing to be casted for 8 weeks. In our study sample, time in cast did not appear to be a barrier to surgery.
Discussion
Utility measures are important for understanding health economics, healthcare utilization, and evaluation of healthcare priorities. Utilities have been calculated for many medical conditions, but as of yet, few upper limb health states preferences have been quantified (23). Utility scores provide information on patient preferences and are a particularly critical component of the health economic approach because they can be converted to quality adjusted life years (QALYs). This study calculated utilities for two critical basic upper limb states for people with tetraplegia: pinch function and elbow extension.
Utilities are such powerful tools because they allow for comparisons between very different health states. These comparisons can be used for the prioritization and rationing of care (24). For example, the Oregon Health Plan used health utilities in construction of their list of medical conditions and their treatments. The rank on this list was then to be used to determine what treatments the state insurance plan would cover (25). Currently, large databases such as the cost effectiveness analysis registry provide utility weights for a wide variety of diseases and their treatment (26). Table 1 provides a sampling of utility scores to establish some frame of reference for different health states. This table shows a wide range of responses for different health states and that the type of surveyed subjects impacts health preference values. For example, physicians tend to undervalue disease states and place a low utility for AIDS, which in contrast to patients who, in general, place higher utilities for their health states, as is demonstrated by the higher utility of the patient on dialysis (27).
Table 1.
Health Utility Index (HUI) – 3
| Mean Score | |
|---|---|
|
| |
| HUI summary score | 0.884 |
| Vision | 0.989 |
| Hearing | 1.0 |
| Speech | 0.999 |
| Ambulation | 1.0 |
| Dexterity | 1.0 |
| Emotion | 0.991 |
| Cognition | 0.998 |
| Pain | 0.937 |
This study found the utility of the tetraplegic condition to be 0.46, which is similar to the finding (0.52) of a previous patient-based study (28). A utility value of 0.46 is very low, and comparable to the utility assigned to a major stroke (0.2–0.5) (23). We found a large gain (utility gains of 0.22 to 0.28) simply with providing these critical functions through the surgical procedures to restore pinch and elbow extension. To put this change of health states into perspective, the differences between tetraplegia and tetraplegia with improvement in one upper limb function is comparable to the difference physicians see between compensated and uncompensated cirrhosis (29). These values suggest that our respondents would sacrifice roughly 25% of their remaining life expectancy for improvement in either pinch or elbow extension. The results of our study indicate a strong preference for treating a major upper-extremity deficit in those with tetraplegia.
The importance of the upper limb function in tetraplegia has been studied with other more traditional methodologies. A survey by Snoek et al. showed that 75% of people with tetraplegia found hand function to be very important for their independence and their quality of life (30); small gains in upper extremity function were found to be extremely beneficial (31, 32). In addition, case series on surgical reconstruction for tetraplegia have shown that these interventions improve patients’ abilities to groom, self-feed, self-catheterize, lift objects, write, swim, and drive (4, 33). This study further supports the conclusions drawn from previous studies, which indicate that the lack of upper limb function is a very concerning feature of tetraplegia, and correction of this deficit adds substantial value to the tetraplegic health state.
One controversy exists when establishing utilities for people with disability. Who should generate these health preferences, the people with the condition or the general population? We chose to survey medical students as proxies for the general population and not people with tetraplegia. This was based on recommendations generated by the Panel on Cost Effectiveness in Health and Medicine, which maintains that population-based preferences are preferable to patient-based preferences (34) (22). The rationale behind this is that utilities are a component of cost-effectiveness analyses, which compare interventions from a societal perspective. These analyses can direct allocation of limited funds within a system with competing needs. Given that utilities are used to determine what is cost-effective for the general public, these values should be based upon the general community’s values and not those of those who are experiencing the disease (35).
Yet, it is easy to imagine a case in which the general population fails to appreciate the true sense of daily life for individuals living with disabilities and subsequently undervalues a certain health state. Cost effective analyses lack compassion and this is a recognized limitation. Studies exploring this problem have found that patients adapt to their disability and indeed place a higher value on their health states than the general population (27, 36). Therefore, future work may compare the health preferences for upper extremity reconstruction between our estimates from medical students to those of people with tetraplegia.
Limitations to this study include the basic difficulties of obtaining utility scores. First our study population was medical students. Medical students are a unique group and likely have different attitudes towards medical conditions; these factors may limit the generalizability of our findings. However, many utilities have been generated using health professionals and our results can be used in comparison to these studies(23). Preferences generated in this study were based on a holistic approach with subjects imagining hypothetical health state scenarios and assigning values to different health outcomes. These scenarios emphasize the important aspects of the health condition of interest, and encourage the participant to reflect on the physical, psychological, and social consequences of real or imagined health states and outcomes. However, opinions vary widely among individuals, and subjective views are difficult to capture by generic utility scales such as the TTO. Alternative measuring scales exist, but we chose the time trade-off technique because other tools such as the rating scale and standard gamble have been shown to suffer measurement bias and be less reflective of individuals’ true health-state preferences, respectively (37, 38). An additional concern is that survey respondents can be heavily influenced by subtle variations in the questionnaire (39–41). To try to minimize this bias, our scenarios portrayed concrete outcomes that were representative of the results of upper extremity surgical reconstruction for tetraplegia (42).
This study establishes the value of two current upper-extremity functions in the setting of tetraplegia: pinch and elbow extension. The results indicate that subjects would give up a substantial amount of time for recovery of pinch and elbow extension and quantifies the value of these two health states.
Figure 4.
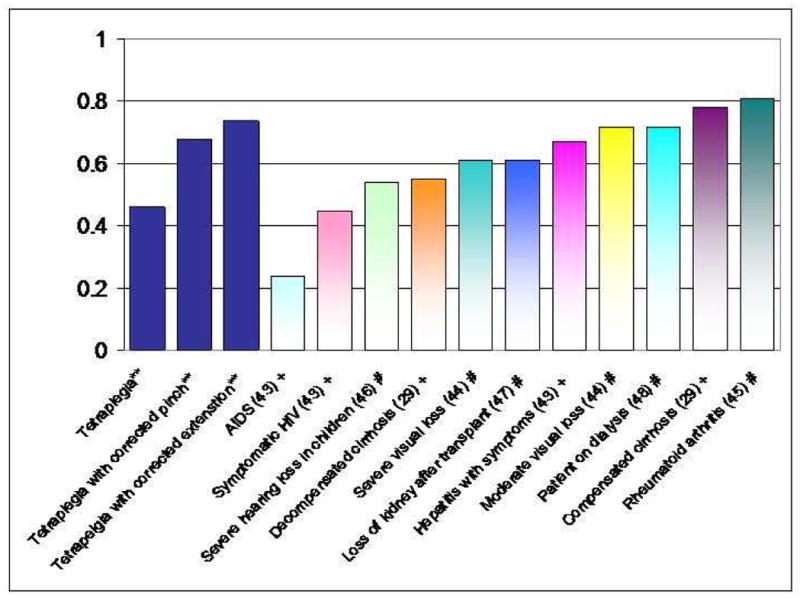
Comparison of Health Utility States
*Present study results
+ Physician perspective
# Patient Perspective
Acknowledgments
This project was supported in part by a VA Career Development Award (to Catherine Curtin) and Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Kevin C. Chung). The authors thank Allison Pushman for her help in formatting and organizing this manuscript.
Appendix 1
Sample TTO Question. Subject is asked to choose between Options A, B, or “Point of Indifference.”
References
- 1.Go BK, Devivo MJ, Richards JS. The Epidemiology of Spinal Cord Injury. In: Stover SL, Delisa JA, Whiteneck GG, editors. Spinal Cord injury Clinical OUtcomes from the Model Systems. Gaithersburg: Aspen Publishers; 1995. pp. 21–55. [Google Scholar]
- 2.National Spinal Cord Injury Statistical Center. Spinal Cord Injury: Facts and Figures at a Glance. J Spinal Cord Med. 2008;31:357–358. [PubMed] [Google Scholar]
- 3.Welraeds D, Ismail AA, Parent A. Functional reconstruction of the upper extremity in tetraplegia. Application of Moberg’s and Allieu’s procedures. Acta Orthop Belg. 2003 Dec;69(6):537–545. [PubMed] [Google Scholar]
- 4.Curtin CM, Hayward RA, Kim HM, Gater DR, Chung KC. Physician perceptions of upper extremity reconstruction for the person with tetraplegia. J Hand Surg [Am] 2005 Jan;30(1):87–93. doi: 10.1016/j.jhsa.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Curtin CM, Gater DR, Chung KC. Upper extremity reconstruction in the tetraplegic population, a national epidemiologic study. J Hand Surg [Am] 2005 Jan;30(1):94–99. doi: 10.1016/j.jhsa.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Curtin CM, Wagner JP, Gater DR, Chung KC. Opinions on the treatment of people with tetraplegia: contrasting perceptions of physiatrists and hand surgeons. J Spinal Cord Med. 2007;30(3):256–262. doi: 10.1080/10790268.2007.11753934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993 Apr 15;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 8.Feeny D. A utility approach to the assessment of health-related quality of life. Med Care. 2000 Sep;38(9 Suppl):II151–154. doi: 10.1097/00005650-200009002-00022. [DOI] [PubMed] [Google Scholar]
- 9.Lee JE, Fos PJ, Zuniga MA, Kastl PR, Sung JH. Assessing health-related quality of life in cataract patients: the relationship between utility and health-related quality of life measurement. Qual Life Res. 2000;9(10):1127–1135. doi: 10.1023/a:1016645523769. [DOI] [PubMed] [Google Scholar]
- 10.Feeny DH, Torrance GW. Incorporating utility-based quality-of-life assessment measures in clinical trials. Two examples. Med Care. 1989 Mar;27(3 Suppl):S190–204. doi: 10.1097/00005650-198903001-00016. [DOI] [PubMed] [Google Scholar]
- 11.Soegaard R, Bunger CE, Christiansen T, Hoy K, Eiskjaer SP, Christensen FB. Circumferential fusion is dominant over posterolateral fusion in a long-term perspective: cost-utility evaluation of a randomized controlled trial in severe, chronic low back pain. Spine. 2007 Oct 15;32(22):2405–2414. doi: 10.1097/BRS.0b013e3181573b2d. [DOI] [PubMed] [Google Scholar]
- 12.Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40(6):593–603. doi: 10.1016/0021-9681(87)90019-1. [DOI] [PubMed] [Google Scholar]
- 13.Johannesson M, Jonsson B, Karlsson G. Outcome measurement in economic evaluation. Health Econ. 1996 Jul-Aug;5(4):279–296. doi: 10.1002/(SICI)1099-1050(199607)5:4<279::AID-HEC218>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 14.Torrance GW, Feeny D, Furlong W. Visual analog scales: do they have a role in the measurement of preferences for health states? Med Decis Making. 2001 Jul-Aug;21(4):329–334. doi: 10.1177/0272989X0102100408. [DOI] [PubMed] [Google Scholar]
- 15.Strauss DJ, Devivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2006 Aug;87(8):1079–1085. doi: 10.1016/j.apmr.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 16.O’Leary Berkowitz M, Kruse DL. Spinal cord injury: an analysis of medical and social costs. Demos Medical Pub. 1998:18–20. [Google Scholar]
- 17.Dillman DA. Mail and Internet Surveys: The Tailored Design Method. New York: John Wiley and Sons; 2000. pp. 142–193. [Google Scholar]
- 18.Davis EN, Chung KC, Kotsis SV, Lau FH, Vijan S. A cost/utility analysis of open reduction and internal fixation versus cast immobilization for acute nondisplaced mid-waist scaphoid fractures. Plast Reconstr Surg. 2006 Apr;117(4):1223–1235. doi: 10.1097/01.prs.0000201461.71055.83. [DOI] [PubMed] [Google Scholar]
- 19.Sanders GD, Owens DK, Padian N, Cardinalli AB, Sullivan AN, Nease RF. A computer-based interview to identify HIV risk behaviors and to assess patient preferences for HIV-related health states. Proc Annu Symp Comput Appl Med Care; 1994; pp. 20–24. [PMC free article] [PubMed] [Google Scholar]
- 20.Feeny D, Furlong W, Boyle M, Torrance GW. Multi-attribute health status classification systems. Health Utilities Index. Pharmacoeconomics. 1995 Jun;7(6):490–502. doi: 10.2165/00019053-199507060-00004. [DOI] [PubMed] [Google Scholar]
- 21.Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. [Accessed June 30, 2009];Alternative approaches for estimating health-related quality of life impacts: Nonroad engine air emissions regulation case study Final report. 2005 Dec; http://www.iom.edu/Object.File/Master/31/440/EPA%20Case%20Study%20December%202005%20final.pdf.
- 23.Bell CM, Chapman RH, Stone PW, Sandberg EA, Neumann PJ. An off-the-shelf help list: a comprehensive catalog of preference scores from published cost-utility analyses. Med Decis Making. 2001 Jul-Aug;21(4):288–294. doi: 10.1177/0272989X0102100404. [DOI] [PubMed] [Google Scholar]
- 24.Floyd EJ. Healthcare reform through rationing. J Healthc Manag. 2003 Jul-Aug;48(4):233–241. [PubMed] [Google Scholar]
- 25.Dixon J, Welch HG. Priority setting: lessons from Oregon. Lancet. 1991 Apr 13;337(8746):891–894. doi: 10.1016/0140-6736(91)90213-9. [DOI] [PubMed] [Google Scholar]
- 26. [Accessed March 2009]; https://research.tufts-nemc.org/cear/Default.aspx.
- 27.Slevin ML, Stubbs L, Plant HJ, Wilson P, Gregory WM, Armes PJ, et al. Attitudes to chemotherapy: comparing views of patients with cancer with those of doctors, nurses, and general public. BMJ. 1990 Jun 2;300(6737):1458–1460. doi: 10.1136/bmj.300.6737.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snoek GJ, MJIJ, Post MW, Stiggelbout AM, Roach MJ, Zilvold G. Choice-based evaluation for the improvement of upper-extremity function compared with other impairments in tetraplegia. Arch Phys Med Rehabil. 2005 Aug;86(8):1623–1630. doi: 10.1016/j.apmr.2004.12.043. [DOI] [PubMed] [Google Scholar]
- 29.Wells CD, Murrill WB, Arguedas MR. Comparison of health-related quality of life preferences between physicians and cirrhotic patients: implications for cost-utility analyses in chronic liver disease. Dig Dis Sci. 2004 Mar;49(3):453–458. doi: 10.1023/b:ddas.0000020502.46886.c1. [DOI] [PubMed] [Google Scholar]
- 30.Snoek GJ, MJIJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord. 2004 Sep;42(9):526–532. doi: 10.1038/sj.sc.3101638. [DOI] [PubMed] [Google Scholar]
- 31.Hanson RW, Franklin MR. Sexual loss in relation to other functional losses for spinal cord injured males. Arch Phys Med Rehabil. 1976 Jun;57(6):291–293. [PubMed] [Google Scholar]
- 32.Manns PJ, Chad KE. Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res. 2001 Nov;11(6):795–811. doi: 10.1177/104973201129119541. [DOI] [PubMed] [Google Scholar]
- 33.Allieu Y, Benichou M, Ohanna F, Rabischong E, Benoit P. Functional surgery of the upper limbs in tetraplegic patients. Current trends after 10 years of experience at the Propara Center. Rev Chir Orthop Reparatrice Appar Mot. 1993;79(2):79–88. [PubMed] [Google Scholar]
- 34.Panel on Cost-Effectiveness in Health and Medicine. Summary recommendations. In: Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. pp. 304–311. [Google Scholar]
- 35.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172–1177. [PubMed] [Google Scholar]
- 36.Sackett DL, Torrance GW. The utility of different health states as perceived by the general public. J Chronic Dis. 1978;31(11):697–704. doi: 10.1016/0021-9681(78)90072-3. [DOI] [PubMed] [Google Scholar]
- 37.Drummond MOBB, Stoddart G, Torrance G. Methods for the Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005. pp. 150–157. [Google Scholar]
- 38.Bleichrodt H. A new explanation for the difference between time trade-off utilities and standard gamble utilities. Health Econ. 2002 Jul;11(5):447–456. doi: 10.1002/hec.688. [DOI] [PubMed] [Google Scholar]
- 39.Revicki DA, Kaplan RM. Relationship between psychometric and utility-based approaches to the measurement of health-related quality of life. Qual Life Res. 1993 Dec;2(6):477–487. doi: 10.1007/BF00422222. [DOI] [PubMed] [Google Scholar]
- 40.Revicki DA. Relationship between health utility and psychometric health status measures. Med Care. 1992 May;30(5 Suppl):MS274–282. doi: 10.1097/00005650-199205001-00027. [DOI] [PubMed] [Google Scholar]
- 41.Naylor D. Cost-effectiveness analysis: are the outputs worth the inputs? ACP J Club. 1996 Jan-Feb;124(1):A12–14. [PubMed] [Google Scholar]
- 42.Harmou C, Shah NR, DiPonio L, Curtin CM. Pinch and elbow extention restoration in people with tetraplegia: A Systematic Review of the Literature. J Hand Surg. doi: 10.1016/j.jhsa.2008.12.002. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Owens DK, Cardinalli AB, Nease RF., Jr Physicians’ assessments of the utility of health states associated with the human immunodeficiency virus (HIV) and hepatitis B virus (HBV) infection. Qual Life Res. 1997;6:77–86. doi: 10.1023/a:1026473613487. [DOI] [PubMed] [Google Scholar]
- 44.Brown MM, Brown GC, Sharma S, Busbee B. Quality of life associated with visual loss: A time tradeoff utility analysis comparison with medical health states. Ophthalmology. 2003;110(6):1076–1081. doi: 10.1016/S0161-6420(03)00254-9. [DOI] [PubMed] [Google Scholar]
- 45.Ariza-Ariza R, Hernández-Cruz B, Carmona L, Dolores Ruiz-Montesinos M, Ballina J, Navarro-Sarabia F the Costs and Quality of Life in Rheumatoid Arthritis Study Group. Assessing utility values in rheumatoid arthritis: A comparison between time trade-off and the EuroQol. Arthritis Rheum. 2006;55(5):751–756. doi: 10.1002/art.22226. [DOI] [PubMed] [Google Scholar]
- 46.Smith-Olinde L, Grosse SD, Olinde F, Martin PF, Tilford JM. Health state preference scores for children with permanent childhood hearing loss: a comparative analysis of the QWB and HUI3. Qual Life Res. 2008;17(6):943–953. doi: 10.1007/s11136-008-9358-x. [DOI] [PubMed] [Google Scholar]
- 47.Laupacis A, Keown P, Pus N, Krueger H, Ferguson B, Wong C, et al. A study of the quality of life and cost-utility of renal transplantation. Kidney Int. 1996;50(1):235–242. doi: 10.1038/ki.1996.307. [DOI] [PubMed] [Google Scholar]
- 48.Gorodetskaya I, Zenios S, McCulloch CE, Bostrom A, Hsu CY, Bindman AB, et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int. 2005;68(6):2801–2808. doi: 10.1111/j.1523-1755.2005.00752.x. [DOI] [PubMed] [Google Scholar]


