Abstract
Although economic evaluation has become more popular among medical professionals, its use in surgery is still lacking. Economic evaluation is used even less so in plastic surgery in which health-related quality of life is of particular importance. The purpose of this paper, part of a tutorial series on Evidence Based Medicine, will focus on the fundamental principles of conducting a surgery economic analysis.
We include the essential aspects of conducting a surgical cost-utility analysis by considering perspectives, costs, outcomes, and utilities. We also describe and give examples of how to conduct the analyses, including calculating quality-adjusted life years (QALYs) and discounting, how to interpret the results, and how to report the results.
Although economic analyses are not simple to conduct, a well-conducted one provides many rewards, such as recommending the adoption of a more effective treatment. For comparing and interpreting economic analysis publications, it is important that all studies use consistent methodology and report the results in a similar manner.
Keywords: Economic Analysis, Cost, Utility, Effectiveness, Evidence-based Medicine
Although economic evaluation has become more popular among medical professionals, its use in Surgery is still lacking. A review over a 6-year period of the number of studies employing utility measurements (used in cost-utility analyses) revealed 649 publications in the medical literature versus just 57 in the surgical literature.1 Chew et al. feel that “the lack of formal economic evaluation in the surgical literature likely stems from the complexity of the subject and (with few exceptions) the lack of surgeon training in clinical research methodology.”1 Within the plastic surgery literature, the use of economic analysis is even more dismal. A review of the plastic surgery literature over a 16-year period revealed that only 0.6% of outcomes studies involved economic analysis.2 Kerrigan et al. note that, “Health-related quality of life is of particular importance in plastic surgery, whose interventions significantly impact quality of life yet may have little impact on length of life.”3
This paper, part of a tutorial series on Evidence Based Medicine, will focus on the fundamental principles of conducting a surgical economic analysis. Although these principles can be applied to any field, we will use examples from the surgical literature. We will frequently reference recommendations made by “the Panel.” The Panel on Cost-Effectiveness in Health and Medicine is a nonfederal group of 13 scientists and scholars who were convened in 1993 by the US Public Health Service to develop recommendations to improve the quality and comparability of economic analysis studies.4
Getting Started
Why should you conduct an economic analysis? It is “a method for evaluating the health outcomes and resource costs of health interventions. Its central function is to show the relative value of alternative interventions for improving health.”4 As in all evidence-based medicine, there should be some uncertainty about the best clinical strategy for a patient in a given health state.5 There are 4 different types of economic evaluation: cost-minimization analysis, cost-effectiveness analysis, cost-utility analysis, and cost-benefit analysis. The definitions, metrics reported, advantages, and disadvantages of these 4 types of studies are shown in Table 1. Because of the advantage that cost-utility studies have in being able to compare treatments with different outcomes, we will focus on how to conduct a cost-utility analysis.
Table 1.
| Type of Study | Definition | Metric Reported | Advantages | Disadvantages |
|---|---|---|---|---|
| Cost-Minimization | Used when 2 or more interventions of equal effectiveness are being compared, but their costs are different. | Cost | Easier to conduct than full cost-effectiveness analysis. | Interventions must have equal effectiveness. |
| Cost-Effectiveness | Health outcomes are not valued but are reported in physical units such as life years gained or cases successfully treated. | Cost/Non-Quality Adjusted Outcome | May be quicker and easier to conduct than cost-utility analysis. | Difficult to compare studies with varying outcomes. Give little credit to interventions that primarily improve quality of life. Fail to account for adverse effects. |
| Cost-Utility | A type of cost-effectiveness study that typically measures health improvement in quality-adjusted life years (QALYs). | Cost/QALY (or other Quality Adjusted Outcome) | Useful when comparing alternative treatments that produce outcomes of different types. Useful when increased survival is bought at the expense of reduced quality of life. |
May bias in favor of those individuals with potentially more years to live in a good health state. |
| Cost-Benefit | Attaches a monetary value to the consequences (costs and effectiveness) of an intervention by asking health care consumers what they would be willing to pay for health services that achieve certain outcomes. | Cost | Allows comparison of medical and non-medical interventions (non- medical interventions typically use cost-benefit). Provides a more definitive endpoint than cost-effectiveness. |
May show bias towards interventions for the rich (if they are more willing to pay than the poor). Places a dollar value on human life. |
Perspective and Assumptions
Costs and outcomes can be evaluated from a number of different perspectives: patient, hospital, third-party payer, or society. However, it is impossible to assess the economic impact of various studies if the studies use different perspectives. Studies based on different perspectives are not comparable. The Panel recommends a societal perspective. By conducting a study using the societal perspective, “the analyst considers everyone affected by the intervention, and all health effects and costs that flow from it are counted, regardless of who would experience them. Health effects include both benefits and harms, even when these occur in people who are not the intended recipients of the intervention.”4
The reference (or base) case is defined by a standard set of methods and assumptions. It serves as a benchmark whereby others can evaluate the quality of a study and determine whether its results can be compared across studies.4 For example, a study should describe the mean or standard values for probabilities, utilities, costs, and discount rates that will be used for the reference case. As described later, these values can be varied in the sensitivity analysis to obtain best and worst case scenarios.
Costs
There are several sources for cost data: hospital, Medicare, and private sources. It is important to remember, especially if using hospital data, the difference between costs and charges. Costs are the actual expenditures incurred when providing a service and charges are list prices. As expected, charges are usually inflated and do not reflect the actual cost In most institutions, obtaining cost data can be difficult because a hospital will not want to divulge the cost structure for fear of losing its competitive edge and permitting insurance reimbursements to decrease if these cost structures are made public.
Costs, not charges, should be measured and they should be the costs in dollars of a fixed year. If cost data are from different years, inflation must be taken into consideration by either inflating the data from an earlier year than the fixed year or deflating the data from a later year.6 An inflation calculator is available from the Bureau of Labor Statistics website.7 If costs are not readily available, as is often the case, some studies employ a cost-to-charge ratio in order to calculate costs. The general formula for a cost-to-charge ratio is: charge for hospitalization x (amount reimbursed by third-party payer ÷ amount charged to third-party payer.8 For example, in a cost-utility analysis of breast reconstruction,9 International Classification of Diseases (ICD-9) codes for different procedures were determined and these were used to obtain mean hospitalization charges from the Healthcare Cost and Utilization Project (HCUP) data set. The Medicare Provider Analysis and Review (MedPAR) database was then used to determine the amount of reimbursement for each diagnosis-related group (DRG) code. A cost-to-charge ratio was calculated by dividing the amount of the DRG reimbursement by the amount of ICD-9 charge. This number was then multiplied by the mean charge from HCUP to calculate a cost.
Narrower perspectives, such as third-party payer, have been used in other surgical economic analyses.10, 11 However, it must be kept in mind that the third-party usually does not pay the full amount billed12 and the results will not be generalizable to studies with a societal perspective.
According to the Panel, the major categories that should be included as costs are, “costs of health care services; costs of patient time expended for the intervention; costs associated with caregiving (paid or unpaid); other costs associated with illness, such as child care and travel expenses; economic costs borne by employers, other employees, and the rest of society, including so-called friction costs associated with absenteeism and employee turnover; and costs associated with non-health impacts of the intervention, such as on the educational system, the criminal justice system, or the environment.”6
There is some controversy as to what should be included in the numerator (as cost) or in the denominator (as effectiveness). It is important not to double count by including, for example, costs of lost life-years when these are already included in the denominator as lost life-years. However, in order to have a true societal perspective, it is important to incorporate into quality adjusted life years (QALYs) anything that has been excluded as a cost. So, if lost wages from time off work will be included as costs, you may wish to include a statement in the utility assessment such as, “In answering this question, please assume that your financial circumstances would not be affected by the illness, as might be the case if you did not have to pay anything for health care and you received disability payments that completely replaced any lost earnings.”13 Similar statements have been used in other economic analyses.14, 15 Thus, the costs of time off work are not double-counted in the denominator by the respondent who may consider a loss of income during recovery. Respondents should be instructed to consider the loss of leisure activities. Lost wages should correspond to the age and gender composition of the target population.6 Such data can be obtained from the US Bureau of Labor Statistics.16 For those individuals not in the labor force, average age- and gender-specific wages should still be used.6
How long should costs be included? Again, there is some controversy. However, the Panel definitely recommends including (1) costs of related diseases in the original life span, (2) costs for intervention-related diseases that occur in added years of life, and (3) costs of an ongoing therapy throughout added years of life. Areas of debate surround including costs of disease unrelated to the intervention and ensuing as a result of added years of life. The Panel concludes that these may either be included or excluded from the reference case. They do not recommend including future non-health care costs (such as food, clothing, and shelter).6
Outcomes
It is essential to know the possible outcomes of the condition under study. Such outcomes may include the probability of surgical complications and what follow-up care, if any, is required from these complications. These data may come from published studies and/or your own clinical trial. If a meta-analysis or a systematic review of the outcomes of interest has not been conducted, you should essentially conduct your own by performing a literature search, critically evaluating the literature, and averaging the results from several quality studies. The studies do not necessarily have to be randomized controlled trials, but they should be of high quality. The goal is to obtain a range of reasonable probability estimates for each outcome. Although the range may come from different studies, it may be based on the 95% confidence interval from a single study17 if that is the only high quality study available. Tips on how to perform a systematic review or meta-analysis are published by Margaliot et al.18 and Chung et al.19 You must also determine how long you will assess outcomes. For surgical studies, one year may be sufficient to assess all possible surgical complications.
Utilities
Utilities can be viewed as the preferences that individuals or society may have for a particular health state.1 When measuring health states, a continuous scale of 0 to 1 is used in which 0 represents death and 1 represents perfect health. For example, in a study of breast hypertrophy, respondents assigned mild breast hypertrophy a utility of 0.93 and severe breast hypertrophy a utility of 0.70 using one type of utility assessment.20 If an intervention extends a patient’s life by 1 year in a 0.70 utility state, and another intervention extends a patient’s life by 2 years in a 0.35 utility state, the QALYs gained for the two interventions would be the same at 0.70.1 For permanent health states, QALYs are calculated by multiplying the utility of the health state by the patient’s expected number of remaining healthy life years. For temporary health states, when a time frame is specified, QALYs are calculated as shown in Table 2.
Table 2.
Example of Calculating QALYs for Temporary Health States
|
| |
| In a study of wrist arthrodesis with a superficial wound infection,29 QALYs were calculated as: . |
The Panel recommends using community preferences. The “community” should be representatives of the general population that contains people with disabilities or chronic illnesses in proportion to the prevalence of the condition under study. Community preferences are different from patient preferences which are values that people experiencing a particular condition will assign to their own health.4 However, it has been found that the general public underestimates the quality of life of certain conditions compared to patients with those conditions. For example, the general public estimated that the quality of life of chronic dialysis is 0.39 whereas dialysis patients rate the quality of life as 0.56.21 The general public seems to have difficulty assessing the quality of life associated with unfamiliar health conditions.22 One option, although time consuming, is to obtain both community and patient preferences. Any differences between the two groups can then be ascertained. Another option is to use members of the “general public” who are familiar with a particular health condition, such as physicians or patients with the same condition under study who have not received nor been evaluated for the treatment under study, for example, rheumatoid arthritis patients waiting for a general check-up if a researcher wants to evaluate a particular type of rheumatoid surgery. The assessment of the utility of colostomy is another example of the importance of choosing the appropriate subjects to measure preference. It was found that physicians with experience in the treatment of gastrointestinal malignancies provided similar utilities as patients treated for rectal cancer with the formation of a colostomy. On the other hand, patients treated for rectal cancer without a colostomy gave the lowest utilities, even lower than a group of healthy volunteers and a group of university science students.23
Several generic utility measurements have been developed such as the EuroQol,24 Health Utilities Index (HUI),25 and the Quality of Well Being (QWB) Scale.26 The choice of a utility tool should reflect the health domains that are important for the particular health problem being investigated.27 Because of the generic nature of these utility assessments, they may not be sensitive enough to capture attributes of a particular disease.1 For example, the EuroQol asks individuals to rate how good or bad various health states are that are related to six domains: mobility, self-care, main activity (e.g. work, study, housework), social relationships, pain, and mood.24 If such health states do not relate to your condition of study, you may have to create your own utility assessment. Surgical studies that have created their own utility assessments include carpal tunnel surgery,28 scaphoid fracture,15 treatment of rheumatoid wrist,29 hand transplantation,30 open tibial fractures,14 and breast hypertrophy.3, 20 There are various ways in which one can assess preferences: rating scale, time trade-off, and standard gamble. Descriptions, advantages, and disadvantages of each of these methods are shown in Table 3.
Table 3.
Methods to Assess Utilities
| Method | Description | Advantages | Disadvantages |
|---|---|---|---|
| Rating Scale | Asks the respondent to assign each health state to one number, usually on a scale of 0 (death) to 100 (perfect health), such as on a “feeling thermometer.”27 | Highly familiar to respondents, less cognitive burden.27 Accommodates states worse than death.27 |
People have difficulty assigning a number to feelings about health states.42 Extreme categories of a scale are often avoided, resulting in clustering of values.43 Need to specify that spacing between each point in the scale should be regarded as equivalent.12, 27 |
| Time Trade-Off | Asks the respondent to value living in a less desirable health state for a longer period of time (A) versus being in a more desirable state for a shorter period of time (B). The time in state B is decreased to a point where the respondent becomes indifferent between the alternatives.27 | May have an advantage because it measures effectiveness and value for a particular health state in the same metric.27 Accommodates states worse than death.27 |
May confound preferences because the years of life that are “sacrificed” come at the end of the life span and may be valued less because they are in the future.27 |
| Standard Gamble | Asks the respondent to consider a hypothetical choice between the certainty of continued life in a particular health state and a gamble. The gamble has 2 possible outcomes: a state of full health or death. The probabilities in the gamble are systematically altered until the respondent is indifferent between the choice of certain continued life in the particular health state and the gamble.27 | Accommodates states worse than death.27 | Usually results in numerically higher utility values due to the risk of gambling with death.27 May be difficult for respondents to comprehend probabilities.12 |
Analysis
To analyze the results, you should create a decision tree. Software such as TreeAge Pro (TreeAge Software Inc., Williamstown, MA) is available for this purpose. Each node or fork in the tree represents a purposeful or random choice.31 Each branch must have advantages and disadvantages32 and the probabilities of all branches must add up to 1 for that node. Cost, duration, utility, and probability are entered into the decision tree for each outcome. The software then calculates a cost and QALY for outcome. In Figure 1, the clinical question is how to best treat a patient with a unilateral hand amputation. The two treatment choices are: hand transplantation or no hand transplantation. From each of these treatment choices arises an outcome or a new choice. Utilities are assigned to the different choices (such as prosthesis versus no prosthesis) and probabilities are assigned to the chance events (such as the probability of surgical complication and subsequent graft loss after hand transplantation). Eventually each branch reaches a terminus, calculated as QALYs in Figure 1.33 We previously illustrated how to calculate QALYs for a single event. At chance events, QALYs are calculated as a weighted average of the QALYs of all possible outcomes resulting from the chance event, and the weighting factors are the probabilities of each element occurring.34 For example, in a cost-utility analysis of hand transplantation,30 there are 4 possible outcomes of treatment using unilateral hand transplantation: minor immunosuppressive complication, major immunosuppressive complication, graft failure, or death. The QALYs of unilateral hand transplantation are calculated as the total sum of each outcome’s QALYs multiplied by the probability of that outcome occurring (Table 4).
Figure 1.
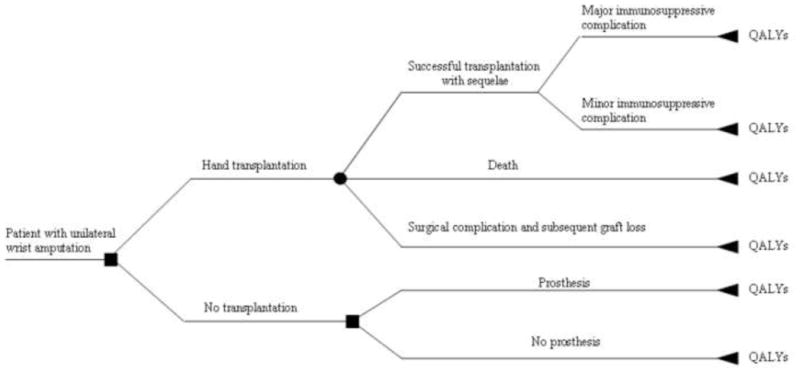
Example of a decision tree for treatment of unilateral hand amputation: amputation versus no amputation33
Table 4.
Calculation of Expected QALYs for Unilateral Hand Transplantation30
|
| |
|
|
The outcomes of an economic analysis are shown in Table 5. As shaded in dark gray, strategies that are less costly and more effective should definitely be adopted. Likewise, strategies that are more costly and less effective should definitely be rejected. All other areas generally fall into “grey zones” that need to be further evaluated or are only weakly accepted or rejected.
Table 5.
Possible Outcomes of Economic Analysis
| Incremental cost | Incremental effectiveness | |||
| More | Same | Less | ||
| More | Need ICER | Weakly reject | Reject | |
| Same | Weakly accept | Neutral | Weakly reject | |
| Less | Accept | Weakly accept | Need ICER | |
ICER=Incremental Cost-Effectiveness Ratio
Adapted from published table12
As shown in Table 5, there are certain instances in which you will need to calculate an incremental cost-effectiveness ratio (ICER). ICER is the cost difference between the two therapies under study divided by the difference in effectiveness between the two therapies ([CostA-CostB]÷[OutcomeA-OutcomeB]). The use of an ICER will be increasingly important, as one of the current healthcare agendas is to compare the cost-effectiveness of interventions in a head-to-head comparison. For example, the ICER for a cost-utility study comparing double hand transplantation versus double prostheses after double hand amputation is $318,961/QALY.30 Typically, ICERs of $50,000 per QALY are considered an acceptable threshold for adopting a particular intervention and those $100,000 or more are considered unaffordable. Thus, for the hand amputation study, hand transplantation was considered to be more effective but exceeds the cost-effectiveness threshold for adoption as the standard therapy. This cutoff appears to have originated in 1982 US dollars and $50,000 was the approximate cost of dialysis for a patient in renal failure (renal dialysis is a federal entitlement to all US citizens under Medicare).35 This ICER is used in the US and may not be applicable in other countries that vary in their willingness to pay for health and health care.36 Although some have proposed raising this threshold,35 there is no other “standard” at this time.
Discounting is the valuation of costs and consequences over time. Money spent or saved in the future should not be weighed as heavily as dollars spent or saved today.12 Discounting is unnecessary in studies with durations of less than 1 year.37 However, it is essential when interventions have costs occurring at differing times over the remaining life of the patient. This was shown in a cost-utility analysis14 of amputation versus salvage for open tibial fractures. Amputation involves the long-term expenses of ongoing prosthetics. Long-term costs are influenced more substantially by discounting and long-term expenses have more impact for younger patients. The Panel recommends using both 3% and 5% as discount rates. Before discounting, all costs should be adjusted for inflation.6 The discounting formula12 shown in Table 6 also gives an example of how to perform discounting. Future QALYs should be discounted in a similar manner with the same rate used to discount cost.
Table 6.
Example of Discount Calculation
| |
|
*If costs all occur at the beginning of each year, the above formula should be used. Thus, year 1 costs are not discounted and year 2 costs are discounted by one year, etc.12 | |
| If costs all occur at the end of each year, the following formula should be used: | |
| Hypothetical Cost and Discounted Cost (3% Discount) of a Cohort of 1,000 Patients Over a Four-Year Period+^: |
| Column 1 | Column 2 | Column 3 | Column 4 | Column 5 |
|---|---|---|---|---|
| Year | Number Surviving | Cost per Person | Total Cost (Column 2 x Column 3) | Discounted Cost (Column 4/1.03Column 1) |
| 1 | 1,000 | $5,000 | $5,000,000 | $4,854,368 |
| 2 | 990 | $4,500 | $4,455,000 | $4,199,265 |
| 3 | 910 | $3,000 | $2,730,000 | $2,498,337 |
| 4 | 840 | $6,500 | $5,460,000 | $4,851,139 |
| Total | $17,645,000 | $16,403,109 |
Adapted from published example8
Assuming all costs occurred at the end of each year
Sensitivity Analysis
A sensitivity analysis should also be performed in order to assess the degree of uncertainty with the result (similar to statistical hypothesis testing).34 Conclusions are not as strong if they change when subjected to the extreme values of the variables.31 One-way sensitivity analysis varies one variable at a time, usually over their entire range. In two- and three-way sensitivity analysis, two or three variables are varied at a time. Although there is no rule as to which variables should be evaluated in multi-way analysis, those that appear to be important in one-way sensitivity analysis should be further studied in multi-way analysis.34 The Panel recommends varying the discount rate from 0 to 7% in the sensitivity analysis.
More sophisticated analyses include Markov models and Monte Carlo simulation. Markov models are useful when there is a problem that involves a risk that is ongoing over time (such as the risk of mortality of a healthy or sick person) and when a given event may occur more than once (such as a hemorrhage after surgery). These scenarios are difficult to represent in a simple tree model.38 Unlike a regular decision tree, future states are independent of past states. A hypothetical cohort of subjects is entered into the model and subjects encounter a number of different probabilities. The process is repeated hundreds or thousands of times until a distribution of cost or effectiveness values are reached.8 For example, in a study comparing implants versus transverse rectus abdominis musculocutaneous (TRAM) flap breast reconstruction, a Markov model was used because there is the possibility of both immediate and late surgical complications.9 Outcomes were modeled for both the implant and TRAM for the remaining life expectancy of the average 48-year old woman. A Markov cycle tree may be evaluated as a Monte Carlo simulation. Monte Carlo simulation uses a large number of trials to determine a distribution of survival values, including statistical measures such as variance and standard deviation of the expected utility.38 We recommend further reading38 and the assistance of a health economist in order to incorporate these sophisticated analyses.
Reporting Results
Reference case results should include: total costs and effectiveness, incremental costs and effectiveness, and ICERs. Both un-discounted and discounted ICERs should be reported. When reporting the results of your economic analysis, it is important to state all assumptions that were used. It is also important to keep in mind the generalizability of your results. Data from economic analyses are not often considered to be generalizable because of differences in the availability of health care resources, clinical practice patterns, and relative prices.39 Recommendations for designing, conducting, and reporting the results of an economic evaluation alongside a randomized trial as well as a checklist for assessing the generalizability of trial-based studies are available in papers by Ramsey et al.40 and Drummond et al.39 General reporting guidelines are also available in Siegel et al.41
Conclusions
Although economic analyses are not simple to conduct, a well-conducted one provides many rewards. Evidence for the adoption of a more effective treatment is one such reward. The fundamental principles offered in this paper provide a basis for conducting a surgery cost-utility study. However, even the best economic analysis is limited by the quality of data available to calculate costs, outcome probabilities, and utilities. In order to compare outcomes of cost and effectiveness across economic analyses and in order to interpret the results of a single economic analysis, it is important that all economic analyses use consistent methodology and report the results in a similar manner. One should understand that the conclusion from an economic analysis project gives recommendations based on the societal perspective to design health policy strategies. However, a physician has the ethical duty and the professional right to consider the need of an individual patient when considering the best treatment decision.
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
References
- 1.Chew RT, Sprague S, Thoma A. A systematic review of utility measurements in the surgical literature. J Am Coll Surg. 2005;200:954–964. doi: 10.1016/j.jamcollsurg.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 2.Davis Sears E, Burns PB, Chung KC. The outcomes of outcome studies in plastic surgery: a systematic review of 17 years of plastic surgery research. Plast Reconstr Surg. 2007;120:2059–2065. doi: 10.1097/01.prs.0000287385.91868.33. [DOI] [PubMed] [Google Scholar]
- 3.Kerrigan CL, Collins ED, Kneeland TS, et al. Measuring health state preferences in women with breast hypertrophy. Plast Reconstr Surg. 2000;106:280–288. doi: 10.1097/00006534-200008000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172–1177. [PubMed] [Google Scholar]
- 5.Detsky AS, Naglie G, Krahn MD, Naimark D, Redelmeier DA. Primer on medical decision analysis: Part 1--Getting started. Med Decis Making. 1997;17:123–125. doi: 10.1177/0272989X9701700201. [DOI] [PubMed] [Google Scholar]
- 6.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1253–1258. [PubMed] [Google Scholar]
- 7.United States Department of Labor. Bureau of Labor Statistics. [Accessed September 17, 2009];CPI Inflation Calculator. Available at: http://www.bls.gov/data/inflation_calculator.htm.
- 8.Muennig P. Designing and Conducting Cost-Effectiveness Analyses in Medicine and Health Care. San Francisco: Josey-Bass; 2002. [Google Scholar]
- 9.Preminger BA, Pusic AL, McCarthy CM, Verma N, Worku A, Cordeiro PG. How should quality-of-life data be incorporated into a cost analysis of breast reconstruction? A consideration of implant versus free TRAM flap procedures. Plast Reconstr Surg. 2008;121:1075–1082. doi: 10.1097/01.prs.0000304246.66477.cd. [DOI] [PubMed] [Google Scholar]
- 10.Kerrigan CL, Stanwix MG. Using evidence to minimize the cost of trigger finger care. J Hand Surg Am. 2009;34:997–1005. doi: 10.1016/j.jhsa.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 11.Thoma A, Khuthaila D, Rockwell G, Veltri K. Cost-utility analysis comparing free and pedicled TRAM flap for breast reconstruction. Microsurgery. 2003;23:287–295. doi: 10.1002/micr.10138. [DOI] [PubMed] [Google Scholar]
- 12.Drummond M, O’Brien B, Stoddart G, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. New York: Oxford University Press; 1997. [Google Scholar]
- 13.Meltzer D, Johannesson M. Inconsistencies in the “societal perspective” on costs of the Panel on Cost-Effectiveness in Health and Medicine. Med Decis Making. 1999;19:371–377. doi: 10.1177/0272989X9901900401. [DOI] [PubMed] [Google Scholar]
- 14.Chung KC, Saddawi-Konefka D, Haase SC, Kaul G. A cost-utility analysis of amputation versus salvage for Gustilo IIIB and C open tibial fractures. Plast Reconstr Surg. doi: 10.1097/PRS.0b013e3181bcf156. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis EN, Chung KC, Kotsis SV, Lau FH, Vijan S. A cost/utility analysis of open reduction and internal fixation versus cast immobilization for acute nondisplaced mid-waist scaphoid fractures. Plast Reconstr Surg. 2006;117:1223–1235. doi: 10.1097/01.prs.0000201461.71055.83. [DOI] [PubMed] [Google Scholar]
- 16.United States Department of Labor. Bureau of Labor Statistics. [Accessed September 10, 2009]; Available at: http://www.bls.gov.
- 17.Naglie G, Krahn MD, Naimark D, Redelmeier DA, Detsky AS. Primer on medical decision analysis: Part 3--Estimating probabilities and utilities. Med Decis Making. 1997;17:136–141. doi: 10.1177/0272989X9701700203. [DOI] [PubMed] [Google Scholar]
- 18.Margaliot Z, Chung KC. Systematic reviews: a primer for plastic surgery research. Plast Reconstr Surg. 2007;120:1834–1841. doi: 10.1097/01.prs.0000295984.24890.2f. [DOI] [PubMed] [Google Scholar]
- 19.Chung KC, Burns PB, Kim HM. A practical guide to meta-analysis. J Hand Surg. 2006;31A:1671–1678. doi: 10.1016/j.jhsa.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Chang WT, Collins ED, Kerrigan CL. An Internet-based utility assessment of breast hypertrophy. Plast Reconstr Surg. 2001;108:370–377. doi: 10.1097/00006534-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Sackett DL, Torrance GW. The utility of different health states as perceived by the general public. J Chronic Dis. 1978;31(11):697–704. doi: 10.1016/0021-9681(78)90072-3. [DOI] [PubMed] [Google Scholar]
- 22.Ubel PA, Loewenstein G, Hershey J, et al. Do nonpatients underestimate the quality of life associated with chronic health conditions because of a focusing illusion? Med Decis Making. 2001;21:190–199. doi: 10.1177/0272989X0102100304. [DOI] [PubMed] [Google Scholar]
- 23.Boyd NF, Sutherland HJ, Heasman KZ, Tritchler DL, Cummings BJ. Whose utilities for decision analysis? Med Decis Making. 1990;10:58–67. doi: 10.1177/0272989X9001000109. [DOI] [PubMed] [Google Scholar]
- 24.EuroQol--a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 25.Feeny D, Furlong W, Torrance GW, et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002;40:113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Kaplan R, Bush J. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1:61–80. [Google Scholar]
- 27.Gold M, Siegel J, Russell LW, MC . Cost-Effectiveness in Health and Medicine. New York: Oxford University Press, Inc; 1996. [Google Scholar]
- 28.Chung KC, Walters MR, Greenfield ML, Chernew ME. Endoscopic versus open carpal tunnel release: a cost-effectiveness analysis. Plast Reconstr Surg. 1998;102:1089–1099. doi: 10.1097/00006534-199809040-00026. [DOI] [PubMed] [Google Scholar]
- 29.Cavaliere CM, Chung KC. Total wrist arthroplasty and total wrist arthrodesis in rheumatoid arthritis: a decision analysis from the hand surgeons’ perspective. J Hand Surg. 2008;33A:1744–1755. doi: 10.1016/j.jhsa.2008.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chung KC, Oda T, Saddawi-Konefka D, Shauver M. An economic analysis of hand transplantation in the United States. Plast Reconstr Surg. doi: 10.1097/PRS.0b013e3181c82eb6. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mastracci TM, Thoma A, Farrokhyar F, Tandan VR, Cina CS. Users’ guide to the surgical literature: how to use a decision analysis. Can J Surg. 2007;50:403–409. [PMC free article] [PubMed] [Google Scholar]
- 32.Detsky AS, Naglie G, Krahn MD, Redelmeier DA, Naimark D. Primer on medical decision analysis: Part 2--Building a tree. Med Decis Making. 1997;17:126–135. doi: 10.1177/0272989X9701700202. [DOI] [PubMed] [Google Scholar]
- 33.Chen NC, Shauver MJ, Chung KC. A primer on use of decision analysis methodology in hand surgery. J Hand Surg. 2009;34A:983–990. doi: 10.1016/j.jhsa.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Krahn MD, Naglie G, Naimark D, Redelmeier DA, Detsky AS. Primer on medical decision analysis: Part 4--Analyzing the model and interpreting the results. Med Decis Making. 1997;17:142–151. doi: 10.1177/0272989X9701700204. [DOI] [PubMed] [Google Scholar]
- 35.Ubel PA, Hirth RA, Chernew ME, Fendrick AM. What is the price of life and why doesn’t it increase at the rate of inflation? Arch Intern Med. 2003;163:1637–1641. doi: 10.1001/archinte.163.14.1637. [DOI] [PubMed] [Google Scholar]
- 36.O’Brien BJ, Heyland D, Richardson WS, Levine M, Drummond MF. Users’ guides to the medical literature. XIII. How to use an article on economic analysis of clinical practice. B. What are the results and will they help me in caring for my patients? Evidence-Based Medicine Working Group. JAMA. 1997;277:1802–1806. doi: 10.1001/jama.277.22.1802. [DOI] [PubMed] [Google Scholar]
- 37.Thoma A, Sprague S, Tandan V. Users’ guide to the surgical literature: how to use an article on economic analysis. Can J Surg. 2001;44:347–354. [PMC free article] [PubMed] [Google Scholar]
- 38.Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making. 1993;13:322–338. doi: 10.1177/0272989X9301300409. [DOI] [PubMed] [Google Scholar]
- 39.Drummond M, Manca A, Sculpher M. Increasing the generalizability of economic evaluations: recommendations for the design, analysis, and reporting of studies. Int J Technol Assess Health Care. 2005;21:165–171. [PubMed] [Google Scholar]
- 40.Ramsey S, Willke R, Briggs A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health. 2005;8:521–533. doi: 10.1111/j.1524-4733.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- 41.Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1339–1341. doi: 10.1001/jama.276.16.1339. [DOI] [PubMed] [Google Scholar]
- 42.Patrick DL, Starks HE, Cain KC, Uhlmann RF, Pearlman RA. Measuring preferences for health states worse than death. Med Decis Making. 1994;14:9–18. doi: 10.1177/0272989X9401400102. [DOI] [PubMed] [Google Scholar]
- 43.Streiner D, Norman G. Healht Measurement Scales. A Practical Guide to their Development and Use. New York: Oxford University Press; 1989. [Google Scholar]


